Abstract
Setting
Academic medical center ED.
Design
Retrospective electronic record review.
Participants
Individuals aged 65 and older seen from 1/1/2013– 9/30/2015
Measurements
We evaluated the utility of routinely collected Hendrich II fall risk scores in predicting ED visits for a fall within 6 months of an all-cause index ED visit.
Results
Among in-network patient visits resulting in discharge with a completed Hendrich II score (N = 4366), the return rate for fall within 6 months was 8.3%. The area under the ROC curve (AUC) when using the score to predict return visits for falls was 0.64. In a univariate model, the OR for returning with a fall in 6 months was 1.23 (95%CI 1.19–1.28) for a one point increase in Hendrich II score. When included in a model with other potential confounders or predictors of fall, the Hendrich II score remains a significant predictor of return visit for fall (aOR 1.15, 95%CI 1.10–1.20). The area under the ROC curve (AUC) for this model was 0.75.
Conclusion
Routinely collected Hendrich II scores demonstrated correlation with outpatient falls, but would likely have little utility as a stand-alone fall risk screen. When combined with easily extractable covariates, the screen performs much better. These results highlight the potential for secondary use of EHR data for risk stratification of ED patients. Using data already routinely collected, patients at high risk of falls after discharge could be identified for referral without requiring additional screening resources to be employed.
Keywords: Falls, Screening, Electronic Health Record, Emergency Medicine
Introduction
Falls among older adults are a major public health concern, with significant morbidity and mortality. Despite guidelines1 and quality measures,2 screening for fall risk remains inconsistent in the primary care setting.3,4 The Emergency Department (ED), where patients are generally at higher risk of outpatient falls than the general population,5–7 offers an ideal additional site to identify high risk patients. While multi-specialty guidelines recommend screening for fall risk in the ED,1,8 guideline adherence to falls screening is generally inadequate in ED settings.9 Interventions to screen ED patients prior to discharge for risk of outpatient falls have not been widely implemented and are an identified research priority within the field of geriatric emergency medicine.10,11
ED-based screening tests have been advocated, and in many cases implemented through regulatory requirements, for many other conditions such as alcohol abuse,12 domestic violence,13 suicide risk,14 and low literacy.15 Given the competing demands to deliver acute illness care, there is little enthusiasm from providers for adding additional screening for non-emergent conditions to the ED workflow.10 Furthermore, despite previous efforts at improving ED-based fall prevention, no existing interventions satisfy the need for a scalable, adaptable, and measurable model suitable for wide dissemination and implementation.16
Many ED patients, however, are screened for inpatient falls, due to the financial penalties on hospitals with high inpatient fall rates.17,18 Numerous screens exist for inpatient fall risk including the Hendrich II instrument,19 which includes several questions similar to those used in validated outpatient fall screens. Although widely implemented,17 to our knowledge, this instrument has not been studied with regard to its ability to predict outpatient falls after an ED visit.6
The objective of this study was to evaluate the utility of routinely collected Hendrich II fall scores in predicting returns to the ED for falls within 6 months. We hypothesized that the Hendrich II instrument would have predictive utility in screening for outpatient fall risk.
Methods
Study Design and Setting
We performed a retrospective observational study using patient Electronic Health Record (EHR) data at a single academic medical center ED with level 1 trauma center accreditation and approximately 60,000 patient visits per year. The study was designed in accordance with the STROBE (STrengthening the Reporting of OBservational studies in Epidemiology) statement and was IRB-approved.20 Our outcome of interest was a fall visit to the ED within 6 months of an index visit. We chose ED visits for fall (as opposed to any fall) both due to data availability and the relevance of an ED-specific fall outcome to those considering implementing screeing in the ED.
Population
Subjects were included in the study if they presented to the University of Wisconsin-University Hospital ED, were discharged, and were aged 65 years or older (the recommended age at which the CDC recommends routine, outpatient fall risk screening).21 We limited our analysis to discharged patients who had a PCP in our health system, minimizing the effect of the inpatient stay and maximizing the quality of collected comorbidity data and probability that subjects would return to our ED for care. Data were collected from 1/1/2013– 9/30/2015, during which time all patient visits were coded using ICD-9 codes.
Measurements
At all ED visits during the study time period, nurses completed a triage screening process. This consisted of an electronic flowsheet including the Hendrich II instrument (Supplementary Table S1). Nurses were instructed to fill out this flowsheet for all patients, but the EHR system did not include a “hard stop” forcing completion. The Hendrich II Score as implemented includes questions regarding confusion/disorientation/impulsiveness, depression, altered elimination, dizziness, gender, administration of high risk medications, and a “rising from chair” test.. As this was a retrospective study, no intervention or education surrounding fall risk was provided to the nursing staff. After all elements of the Hendrich II Score are entered, the flowsheet calculates the total score and flags a patient as high risk for inpatient fall if the score is greater than 4. All elements of the score were extracted from the EHR for analysis.
Based on our prior work,22 we defined fall visits as those in which patients presented with a chief complaint indicating a fall, or had a mechanism of injury code which specifically indicated a fall mechanism. In addition to the Hendrich II Scores and our fall outcome, we extracted patient demographics (age, gender, race/ethnicity, and insurance status) and factors affecting mode of presentation to the ED (arrival mode and Emergency Severity Index (ESI) triage category). The ESI is a widely-used triage system for ED patients, which categorizes patients into five levels, from 1 for the most acute to 5 for the least acute, and has been validated for use in the geriatric population.23 We also report the Center for Medicare and Medicaid Services’ hierarchical condition categories (HCC) scores, which are used for baseline risk adjustment.24
Data Analysis
Data were extracted from the EHR and analyzed using Stata® 13.1 (StataCorp, College Station, TX). In the main analysis, we excluded all visits in which any component of the Hendrich II score was missing. We estimated two logistic regression models to evaluate the association between Hendrich II score assigned at an index visit and return for fall within 6 months. The first model evaluated the Hendrich II score alone, and the second included other variables preselected based on the potential for additional predictive value or confounding. These variables were age, gender, insurance status, mode of arrival, triage ESI acuity score, HCC score, and presence of Fall at the index visit. Both of these models were created censoring cases with missing Hendrich II data.
After completing our primary analysis, for robustness, we recreated the above logistic models using a multiple imputation approach which uses the full dataset and imputes values for observations missing data. We used STATA25 to perform a chained equation multiple imputation model. We created 10 imputed datasets using predictive mean matching with five nearest neighbors to generate Hendrich II scores based on the above control variables. After creation of imputed datasets, logistic regression was performed on each imputed dataset and results were generated by averaging over the estimated results.
To test for selection bias, we investigated the association between missing scores at index visit and returns for fall within 6 months. Here we again created two logistic regression models: one including only presence of a score at an index visit, and one controlling for the same list of potential confounders used in the main result analysis as above.
RESULTS
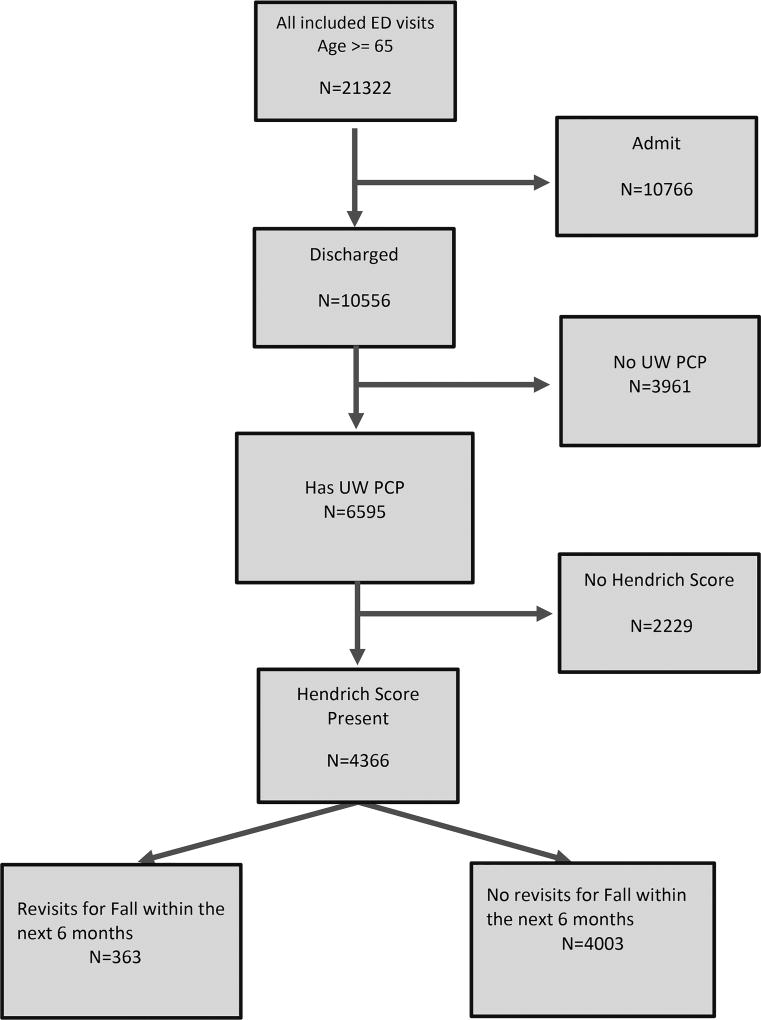
We had 21,322 visits to the ED during the study period, of which 6,595 were both discharged and had a PCP in our network, making up our study population (Figure 2). Among all patient visits with an in-network PCP presenting to the ED (both admitted and discharged, N = 13,062), 15.7 percent were fall related. Among this group of fall patients, 37.5% had been seen in the ED within the prior 6 months. Among discharged patients who had a PCP, 4,366 (66.2%) had a Hendrich II Score completely recorded (Table 1). Patients were predominant older, female, and white, with Medicare insurance and two-thirds had an ESI acuity score of 3. Among visits with a completed Hendrich II Score (N = 4366), the return rate for fall within 6 months was 8.3%.
Table 1. Characteristics of ED Patient Visits According to Whether They Received a Hendrich II Score and Fall Visit Variables by Outcome.
Characteristics of ED patient visits according to whether the received a Hendrich II score and fall Visit Variables by Outcome: All numbers are displayed as Proportion(standard deviation) with the exception of Age and HCC, which are displayed as Mean(standard deviation).
| All Older Adult ED Visits With UW PCP With Discharge |
All Older adults discharged who have a HII score |
Discharged Pts with a Hendrich II score and no return |
Discharged Pts with a Hendrich II who Do return |
|
|---|---|---|---|---|
| N (%) | 6595 (100%) | 4366 (66.2%) | 4003 | 363 |
| Age | 76.1 (8.4) | 75.5 (8.2) | 75.3 (8.1) | 78.3 (8.3) |
| Gen (% Female) | 61.0 (0.5) | 60.8 (0.5) | 60.2 (0.5) | 67.5 (0.5) |
| Race | ||||
| White | 92.8 (0.3) | 92.5 (0.3) | 92.5 (0.3) | 91.7 (0.3) |
| Nonwhite | 7.2 (0.3) | 7.5 (0.3) | 7.5 (0.3) | 8.3 (0.3) |
| Insurance Status | ||||
| Medicaid/BadgerCare | 0.3 (0.1) | 0.3 (0.1) | 0.3 (0.1) | 0.3 (0.1) |
| Medicare | 85.6 (0.4) | 86.4 (0.3) | 86.6 (0.3) | 83.8 (0.4) |
| Commercial/Worker’s Comp | 12.7 (0.3) | 12.4 (0.3) | 12.1 (0.3) | 15.7 (0.4) |
| Unknown | 1.3 (0.1) | 0.9 (0.1) | 0.95 (0.1) | 0.28 (0.1) |
| Mode of Arrival | ||||
| Family or Self | 67.5 (0.5) | 76.4 (0.4) | 78.4 (0.4) | 54.5 (0.5) |
| EMS | 32.3 (0.5) | 23.4 (0.4) | 21.4 (0.4) | 44.9 (0.5) |
| Police | 0.2 (0.0) | 0.2 (0.0) | 0.2 (0.0) | 0.6 (0.1) |
| ESI Triage Acuity Score | ||||
| 1 | 0.0(0.0) | N/A | N/A | N/A |
| 2 | 19.7 (0.4) | 19.5 (0.4) | 19.8 (0.4) | 16.5 (0.4) |
| 3 | 69.3 (0.5) | 68.9 (0.5) | 68.6 (0.5) | 71.6 (0.5) |
| 4 | 10.6 (0.3) | 11.2 (0.3) | 11.2 (0.3) | 11.3 (0.3) |
| 5 | 0.4(0.1) | 0.4 (0.1) | 0.4 (0.1) | 0.6 (0.1) |
| Mean HCC score | 1.45 (1.3) | 1.40 (1.2) | 1.35 (1.2) | 1.95 (1.4) |
| Fall at index visit | 16.3(0.4) | 14.0 (0.3) | 12.6 (0.3) | 28.9 (0.5) |
| Rate of Return for Fall at 180 days | 9.6(0.3) | 8.4 (0.3) | N/A | N/A |
Among visits with a completed Hendrich II score, the area under the ROC curve (AUC) for Hendrich II score as a predictor of return visit for fall was was 0.64 (Figure in Supplementary Figure S2). Table 2 shows test characteristics among the study population based on various cutoffs of the Hendrich II score. In a univariate model, each additional point on the Hendrich II score had an OR of 1.23(95%CI 1.19–1.28) on returning for a fall within 6 months. When included in a model with other potential confounders or predictors of fall, the Hendrich II score remains a significant predictor of return visit for fall (aOR 1.15, 95%CI 1.10–1.20). This more inclusive model had more predictive value for falls, with an AUC of 0.75 (Supplementary Figure S2). Please see Supplementary Table S3 for full regression results from the main analysis.
Table 2. Hendrich Score Performance.
Hendrich Score Cutoffs and test characteristics. Sensitivity, Specificity, Likelihood Ratios (LRs), observed rates and classification reported within test population. Predicted chance of return if above cutoffs calculated using STATA postestimation margins for the univariate regression model with Hendrich II score for fall within 180 days.
| Hendrich II Score Cutoff |
Sensitivity | Specificity | LR(+) | LR(−) | Observed Rate of fall if above cutoff |
Correctly Classified |
Predicted Rate of of fall if Above Cutoff |
|---|---|---|---|---|---|---|---|
| ≥0 | 100.0% | 0.0% | 1 | 8.4% | 8.36% | 8.3(7.5–9.1) | |
| ≥1 | 80.6% | 29.3% | 1.14 | 0.66 | 9.4% | 33.62% | 9.3(8.3–10.3) |
| ≥2 | 57.8% | 64.8% | 1.65 | 0.65 | 13.1% | 64.27% | 12.9(11.3 –14.5) |
| ≥3 | 46.6% | 78.1% | 2.12 | 0.68 | 16.2% | 75.42% | 16.1(13.9–18.4) |
| ≥4 | 39.7% | 83.6% | 2.42 | 0.72 | 18.1% | 79.94% | 18.0(15.3–20.6) |
| ≥5 | 23.8% | 90.0% | 2.39 | 0.85 | 17.9% | 84.49% | 17.9(14.5–21.3) |
| ≥6 | 15.6% | 94.5% | 2.85 | 0.89 | 20.7% | 87.93% | 20.7(15.9–25.4) |
| ≥7 | 12.6% | 96.0% | 3.13 | 0.91 | 22.2% | 89.01% | 22.2(16.6–27.9) |
| ≥8 | 10.4% | 96.9% | 3.33 | 0.92 | 23.5% | 89.67% | 23.5(16.9–30.0) |
| ≥9 | 6.9% | 98.3% | 3.91 | 0.95 | 26.3% | 90.61% | 26.3(17.5–35.2) |
| ≥10 | 3.3% | 99.4% | 5.26 | 0.97 | 32.4% | 91.34% | 32.4(17.3–47.5) |
| ≥11 | 1.1% | 99.7% | 3.13 | 0.99 | 22.2% | 91.41% | 22.2(3.0–41.4) |
| ≥12 | 0.8% | 99.9% | 5.48 | 0.99 | 33.3% | 91.57% | 33.3(2.5–64.1) |
| ≥13 | 0.3% | 99.9% | 2.74 | 0.99 | 20.0% | 91.57% | 20.0(−15.0–55.1) |
| >13 | 0.0% | 100.0% | 1 | N/A (No Obs) | 91.64% | N/A (No Obs) |
Among discharged patients who had a PCP, 4,366 (33.8%) had at least one element of the Hendrich II Score missing and were excluded from analysis. Among those visits with a missing Hendrich II Score, the “rising from chair” variable was left unfilled in 90.5% of cases, with rates of missingness for other variables ranging from 46–51%. The score sheet was completely unfilled in 15% of cases. Supplementary Table S1 lists individual score elements including missing variables for all patients. Results of regression in the multiple imputation models were similar overall to those in the censored regression model, with AUC for the Hendrich II score alone of 0.62, and for the Hendrich II Model along with covariates of 0.74. Supplementary Table S3 presents the full results of this analysis.
We also investigated whether the presence of missing values themselves had an effect on return visits for fall. In a univariate logistic regression model, the presence of a complete Hendrich II Score was associated with a lower rate of return for falls (OR 0.66, 95%CI 0.55–0.75). When included in a model along with potential confounders, however, there was no significant effect on return rates (aOR 0.96, 95%CI 0.8–1.15). For full regression results of the missing value analysis, please see Supplementary Table S4.
DISCUSSION
We performed an analysis of the Hendrich II, an existing, widely adopted inpatient fall screening instrument, to evaluate its usefulness in screening for outpatient fall risk. We showed that increasing scores on the Hendrich II instrument have a strong association with future visits for fall. Unfortunately, given the sensitivity and specificity at each score cutoff, it is likely insufficient as a standalone instrument for risk stratifying ED patients for fall risk beyond their hospital stay. When combined with other variables easily extracted from the EHR, however, we demonstrated improved prediction for falls, with an AUC of 0.75. This result suggests promise for risk stratifying adults for outpatient falls without adding to existing ED workflows using routinely collected EHR data.
Our approach of repurposing the Hendrich II instrument for outpatient falls has several advantages when compared to improving or creating a new standalone risk screening instrument. It is already widely used to screen for fall risk within hospitals and the data are already collected, meaning that there is no additional time or resource cost incurred using the results when examining outpatient fall risk. A gap currently exists between fall screening guidelines and interventions which are suitable for widespread adoption;16 automating the screening process has the potential to address numerous potential barriers to implementation by reducing cost in terms of resources, time, and behavioral change.26
There are some disadvantages to implementing the Hendrich II score in the ED setting. Specifically, the rising from chair test may not be feasible for all patients in all ED’s. Alternative instruments have been reported: Carpenter et al. developed a screen of 4 independent factors, reporting a 4% probability of falling in their lowest risk group and 42% among the highest,5 and Tiedemann et al. developed and externally validated a screening instrument with an AUC of 0.70.7 Both of these instruments require additional staff time for in-person screeining implementation.
Regardless of which instrument is used, the need for falls screening and intervention is clear: Nearly 15% of our ED visits among patients age 65 and older were fall related, highlighting the significant burden of disease for falls. 37.5% of patients with ED visits for falls in our study population had been seen in our ED within the previous 6 months, suggesting that the ED is an ideal site to capture high risk patients and intervene to modify risk.
Improved fall screening can only modify fall risk when coupled with an effective intervention for patients at risk, and both screening and lack of effective interventions have been implicated as barriers to improved ED based fall care.27 Multidisciplinary fall interevntions have been proven to reduce risk of falls in some settings: the Prevention of Falls in the Elderly (PROFET) trial enrolled ED patients after an initial fall, and demonstrated that ED based referral for multidisciplinary fall prevention programs reduced future fall rates.28
Our study has several limitations. The single site design may limit the generalizeability of our results. We know that falls are underreported by older adults,3 and likely the true burden of falls is higher than that captured by our outcome of ED visits for fall. However, we have no reason to believe that falls are differentially reported based on a screening score, thus this effect is unlikely to significantly alter our findings. Given our secondary use of a clinically obtained dataset, our study was likely subject to some selection bias.29 Specifically our decision to include only those patient who had a PCP may have created a sub-population with better access to care. In this case the specificity of our test would be artificially increased with little effect on sensitivity, when comparing our results to a more general population.30
In our sample, Hendrich II Scores were only completed for 66% of visits. Completion of the score was not independently associated with a change in fall rate, however the scores were filled out in a subset of our population less likely to return for falls. We would not expect scores themselves to influence fall rates, as no attempt was made to lower outpatient fall risk among those who had high scores. Likely patients who arrived by ambulance represented a sicker subpopulation both more likely to fall in the future, and less likely to receive a fall score. In ambulance arrivals nursing staff are more focused on initiating patient care than filling out screening instruments, likely explaining the association we observed. Our multiple imputation analysis suggests that this process difference had little effect on our primary results. Future screening efforts may be able to increase completion rates using other EHR data points such as those collected in our study to reserve nursing screening questions for further risk stratification among only those patients who are at somewhat increased risk based on age, presenting complaint, or other factors.
CONCLUSIONS
In this analysis, we examined the effectiveness of a widely adopted inpatient fall screening instrument for the prediction of serious outpatient falls. We found that the instrument had an AUC of 0.64, but given the sensitivity and specificity at each particular cutoff value, would likely not be useful as a stand-alone fall risk screen. However, when combined with easily extractable covariates, the screen performs much better, with an AUC of 0.75 for return visits. These results highlight the potential for secondary use of EHR data for risk stratification of ED patients. Using data already routinely collected, patients at high risk of future falls after discharge could be identified for referral to fall reduction programs or other follow-up measures without requiring additional screening resources to be employed, overcoming a major barrier to falls prevention from the ED setting.
Supplementary Material
Supplementary Table S1: Hendrich II Fall Risk Score As Implemented
Supplementary Table S3: Regression Results, Main Analysis
Supplementary Table S4: Regression Results for Missing Value Sensitivity Analysis
Supplementary Figure S2: ROC curve: Hendrich II score alone for outcome of return visit for fall within 6 months (left) and Hendrich II score along with EHR derived variables for outcome of return visit for fall within 6 months (right).
Figure 1.
Patient flow in the study.
IMPACT.
We certify that this research is novel. We found relatively poor performance of the Hendrich II instrument when used alone, but improved performance when combined with data already available in the EHR. These results highlight the potential for secondary use of EHR data for risk stratification of ED patients.
Acknowledgments
This project was supported by grant numbers K08HS024558 and 1K24AG054560 from the Agency for Healthcare Research and Quality and K08DK111234 from the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality nor the National Institutes of Health.
Footnotes
Prior Presentations: None
Conflict of Interest: None
Author Contributions: Patterson: study concept and design, data acquisition, analysis and interpretation, drafting and revision of manuscript. Repplinger: data analysis and interpretation, revision of manuscript. Pulia: data analysis and interpretation, revision of manuscript. Batt: data analysis including multiple imputation Svenson: data analysis and interpretation. Trinh: data analysis, revision and formatting of manuscript. Mendonça: data analysis and interpretation, revision of manuscript. Smith: study design, data acquisition, analysis and interpretation, revision of manuscript. Hamedani: analysis and interpretation, revision of manuscript. Shah: Study design, data analysis and interpretation, revision of manuscript.
References
- 1.Kenny R, Rubenstein LZ, Tinetti ME, Brewer K, Cameron KA, Capezuti EA, John DP, Lamb S, Martin F, Rockey PH, Suther M, Peterson E, Susskind O, Radcliff S, Addleman K, Drootin M, Ickowicz E, Lunderbjerg N. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. Journal of the American Geriatrics Society. 2011;59:148–57. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Medicare & Medicaid Services. 2016 Physician Quality Reporting System (PQRS) Measures Groups Specifications Manual. 2016 [Google Scholar]
- 3.Phelan EA, Mahoney JE, Voit JC, Stevens JA. Assessment and management of fall risk in primary care settings. Med Clin North Am. 2015;99:281–93. doi: 10.1016/j.mcna.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Landis SE, Galvin SL. Implementation and assessment of a fall screening program in primary care practices. J Am Geriatr Soc. 2016;62:2408–14. doi: 10.1111/jgs.13137. [DOI] [PubMed] [Google Scholar]
- 5.Carpenter C, Scheatzle M, D'Antonio J, Ricci P, Coben J. Identification of fall risk factors in older adult emergency department patients. Acad Emerg Med. 2009;16:211–9. doi: 10.1111/j.1553-2712.2009.00351.x. [DOI] [PubMed] [Google Scholar]
- 6.Carpenter CR, Avidan MS, Wildes T, Stark S, Fowler SA, Lo AX. Predicting geriatric falls following an episode of emergency department care: a systematic review. Acad Emerg Med. 2014;21:1069–82. doi: 10.1111/acem.12488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tiedemann A, Sherrington C, Orr T, et al. Identifying older people at high risk of future falls: Development and validation of a screening tool for use in emergency departments. Emergency medicine journal : EMJ. 2013;30:918–22. doi: 10.1136/emermed-2012-201783. [DOI] [PubMed] [Google Scholar]
- 8.Rosenberg M, Carpenter CR, Bromley M, Caterino JM, Chun A, Gerson L, Greenspan J, Hwang U, John DP, Lichtman J, Lynos WL, Mortensen B, Platts-Mills TF, Ragsdale LC, Rispoli J, Seaberg DC, Wilber ST. Geriatric emergency department guidelines. Annals of emergency medicine. 2014;63:e7–25. doi: 10.1016/j.annemergmed.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 9.Tirrell G, Sri-on J, Lipsitz LA, Camargo CA, Jr, Kabrhel C, Liu SW. Evaluation of older adult patients with falls in the emergency department: discordance with national guidelines. Acad Emerg Med. 2015;22:461–7. doi: 10.1111/acem.12634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carpenter CR, Griffey RT, Stark S, Coopersmith CM, Gage BF. Physician and nurse acceptance of technicians to screen for geriatric syndromes in the emergency department. West J Emerg Med. 2011;12:489–95. doi: 10.5811/westjem.2011.1.1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carpenter CR, Shah MN, Hustey FM, Heard K, Gerson LW, Miller DK. High Yield Research Opportunities in Geriatric Emergency Medicine: Prehospital Care, Delirium, Adverse Drug Events, and Falls. J Gerontol A Biol Sci Med Sci. 2011;66A:775–83. doi: 10.1093/gerona/glr040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.D'Onofrio G, Degutis Linda C. Preventive care in the emergency department: Screening and brief intervention for alcohol problems in the emergency department: A systematic review. Acad Emerg Med. 2016;9:627–38. doi: 10.1111/j.1553-2712.2002.tb02304.x. [DOI] [PubMed] [Google Scholar]
- 13.Feldhaus KM, Koziol-McLain J, Amsbury HL, Norton lM, Lowenstein SR, Abbott JT. Accuracy of 3 brief screening questions for detecting partner violence in the emergency department. Jama. 2016;277:1357–61. [PubMed] [Google Scholar]
- 14.Allen MH, Abar BW, McCormick M, et al. Screening for suicidal ideation and attempts among emergency department medical patients: Instrument and results from the psychiatric emergency research collaboration. Suicide Life Threat Behav. 2016;43:313–23. doi: 10.1111/sltb.12018. [DOI] [PubMed] [Google Scholar]
- 15.Carpenter CR, Kaphingst KA, Goodman MS, Lin MJ, Melson AT, Griffey RT. Feasibility and diagnostic accuracy of brief health literacy and numeracy screening instruments in an urban emergency department. Acad Emerg Med. 2016;21:137–46. doi: 10.1111/acem.12315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carpenter CR, Lo AX. Falling behind? Understanding implementation science in future emergency department management strategies for geriatric fall prevention. Acad Emerg Med. 2015;22:478–80. doi: 10.1111/acem.12628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Williams T, Szekendi M, Thomas S. An analysis of patient falls and fall prevention programs across academic medical centers. Journal of nursing care quality. 2014;29:19–29. doi: 10.1097/NCQ.0b013e3182a0cd19. [DOI] [PubMed] [Google Scholar]
- 18.Rosenthal MB. Nonpayment for performance? Medicare's new reimbursement rule. The New England journal of medicine. 2007;357:1573–5. doi: 10.1056/NEJMp078184. [DOI] [PubMed] [Google Scholar]
- 19.Hendrich AL, Bender PS, Nyhuis A. Validation of the Hendrich II fall risk model: A large concurrent case/control study of hospitalized patients. Applied nursing research : ANR. 2003;16:9–21. doi: 10.1053/apnr.2003.YAPNR2. [DOI] [PubMed] [Google Scholar]
- 20.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–7. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 21. [Accessed 2/1/2016];STEADI Initiative for Health Care Providers | STEADI - Older Adult Fall Prevention | CDC Injury Center. 2016 (at http://www.cdc.gov/steadi/.)
- 22.Patterson BW, Smith MA, Repplinger MD, et al. Using Chief Complaint in Addition to Diagnosis Codes to Identify Falls in the Emergency Department. J Am Geriatr Soc. 2017 doi: 10.1111/jgs.14982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baumann MR, Strout TD. Triage of geriatric patients in the emergency department: validity and survival with the Emergency Severity Index. Annals of emergency medicine. 2007;49:234–40. doi: 10.1016/j.annemergmed.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 24.Pope GC, Kautter J, Ellis RP, et al. Risk adjustment of Medicare capitation payments using the CMS-HCC model. Health care financing review. 2004;25:119–41. [PMC free article] [PubMed] [Google Scholar]
- 25.Royston P, White IR. Multiple Imputation by Chained Equations (MICE): Implementation in Stata. Journal of Statistical Software. 2011;45:17. [Google Scholar]
- 26.Neta G, Glasgow RE, Carpenter CR, et al. A Framework for Enhancing the Value of Research for Dissemination and Implementation. Am J Public Health. 2015;105:49–57. doi: 10.2105/AJPH.2014.302206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shankar KN, Treadway NJ, Taylor AA, Breaud AH, Peterson EW, Howland J. Older adult falls prevention behaviors 60 days post-discharge from an urban emergency department after treatment for a fall. Inj Epidemiol. 2017;4 doi: 10.1186/s40621-017-0114-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET): A randomised controlled trial. Lancet (London, England) 1999;353:93–7. doi: 10.1016/S0140-6736(98)06119-4. [DOI] [PubMed] [Google Scholar]
- 29.Botsis T, Hartvigsen G, Chen F, Weng C. Secondary Use of EHR: Data Quality Issues and Informatics Opportunities. Summit on Translat Bioinforma. 2010;2010:1–5. [PMC free article] [PubMed] [Google Scholar]
- 30.Kohn MA, Carpenter CR, Newman TB. Understanding the direction of bias in studies of diagnostic test accuracy. Acad Emerg Med. 2013;20:1194–206. doi: 10.1111/acem.12255. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: Hendrich II Fall Risk Score As Implemented
Supplementary Table S3: Regression Results, Main Analysis
Supplementary Table S4: Regression Results for Missing Value Sensitivity Analysis
Supplementary Figure S2: ROC curve: Hendrich II score alone for outcome of return visit for fall within 6 months (left) and Hendrich II score along with EHR derived variables for outcome of return visit for fall within 6 months (right).