Abstract
Breastfeeding in patients with chronic myeloid leukaemia (CML) during tyrosine kinase inhibitors (TKIs) therapy is not recommended but interruption of TKI treatment may cause the loss of remission. We studied the 3 cases of pregnancy and breastfeeding in women with CML and observed that stopping treatment without major molecular response may end in haematological relapse. The concentrations of nilotinib and imatinib in maternal milk were measured and nilotinib distribution in human breast milk was demonstrated for the first time. The estimated maximal doses of imatinib and nilotinib which an infant may ingest with the maternal milk were less than the therapeutical doses. However, the unknown impact of the low dose chronic exposure to these TKIs in infants imposes the limitations on their use during breastfeeding. Breastfeeding without TKI treatment may be safe with molecular monitoring, but preferably in those patients with CML who have durable deep molecular response.
Keywords: Chronic myeloid leukaemia, Pregnancy, Breastfeeding, milk, Breast milk, Imatinib, Nilotinib, Dasatinib, Molecular response
Introduction
Currently, patients with chronic myeloid leukaemia (CML) who achieve an optimal response being treated by tyrosine kinase inhibitors (TKIs) have a high life expectancy, and therefore planning a family is a significant issue for them.1,2 However, the TKIs used for CML treatment have been classified as Category D by the US Food and Drug Administration (FDA) due to their potential teratogenicity and the use during pregnancy is not recommended unless treatment benefits overweigh potential risks.3–5
It has been proved that the first-generation TKI imatinib is distributed into breast milk.6–10 It is reasonable to suggest that the second and third generation of TKIs used for CML treatment (nilotinib, dasatinib, bosutinib, ponatinib and radotinib) also distribute into maternal milk, but at the present time it has never been demonstrated in humans, as of our knowledge. According to the calculations made from the experimental data, the dose of imatinib which a child may ingest with the maternal milk is considerably lower than the therapeutic drug dose, since it corresponds to the plasmatic level.7 However, the effects that even low doses of TKIs may cause on infants in the first months of life are unknown. Therefore, breastfeeding for women who use these drugs is not recommended. On the other hand, if a woman insists on breastfeeding, a delay in resuming TKI after labour may lead to loss of response to treatment. We aimed to describe the course of the disease in women with CML who were off-treatment during the breastfeeding period and to measure the concentrations of TKIs in breast milk when available.
Materials and Methods
Three women with Ph+ positive CML in chronic phase (CP) were observed during the years 2014 to 2017. Two patients interrupted imatinib in order to conceive without TKI, one of them had an in vitro fertilization. One woman conceived while taking nilotinib and stopped the drug immediately after pregnancy confirmation. The haematological and the molecular response of the patients were assessed every 4–6 weeks during the off-treatment period or more often if required. The definitions of the haematological and molecular response were in accordance with the European LeukaemiaNet (ELN) recommendations.11 One patient resumed imatinib in the second trimester due to the loss of complete haematological response (CHR) and 2 patients were off-treatment until labour (Table 1). The pregnancy ended in childbirth in all 3 patients, all 3 babies were healthy. The women insisted on breastfeeding their children and were observed without treatment during the breastfeeding period.
Table 1.
Management of chronic myeloid leukaemia and treatment response in accordance with pregnancy and breastfeeding periods.
| № of case | Molecular and hematologic response | Treatment of CML | Follow-up | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Before pregnancy | During pregnancy | During breastfeeding period | Before pregnancy | During pregnancy | During breastfeeding period | Time of observation after labour, months | Treatment | Response at last follow-up | |
| 1 | DMR, CHR | DMR, CHR | DMR, CHR | NIL 800 mg | No treatment since 4th week of pregnancy | No treatment | 28 | No | DMR, CHR |
| 2 | DMR, CHR | Loss of MMR, CHR | Loss of MR2, CHR | IM 400 mg, no treatment at conception | No treatment | No treatment | 24 | IM 400 mg | DMR, CHR |
| 3 | no MR2, CHR | Loss of MR2, loss of CHR CHR restored when IM was resumed |
no MR2, CHR | IN 400 mg, no treatment at conception | IM 400 mg was resumed since 16th week of gestation | No treatment | 19 | IM 600 mg for 6 months, then switched to NIL 800 mg | MMR, CHR |
CML- chronic myeloid leukaemia, TKI- tyrosine kinase inhibitor, CHR- complete haematological response, MR2- molecular response with the level of BCR-ABL≤1%, MMR - major molecular response with the level of BCR-ABL<0,1%, DMR –molecular response with the level of BCR-ABL≤0,01% including undetectable level, IM- imatinib, NIL – nilotinib.
When the breastfeeding period came to an end, the patients were asked to collect breast milk samples after TKI intake. The patients took the same TKI they had before pregnancy and avoided breastfeeding during the sampling day. The time points for the milk sample collection were established as 1, 2, 4, 6, 8, 12 and 24 hours after the drug intake. The samples were stored at -20°C until evaluation. Quantitative detection of drug concentrations was done by high-performance liquid chromatography-tandem mass spectrometry (HPLC-MS/MS). All patients signed an appropriate informed consent for analysis of their biological samples and clinical data.
Results
Molecular monitoring of BCR-ABL levels during pregnancy and breastfeeding
The molecular response and management of CML differed in each case (Table 1). In order to provide the details, we present a brief description of these cases.
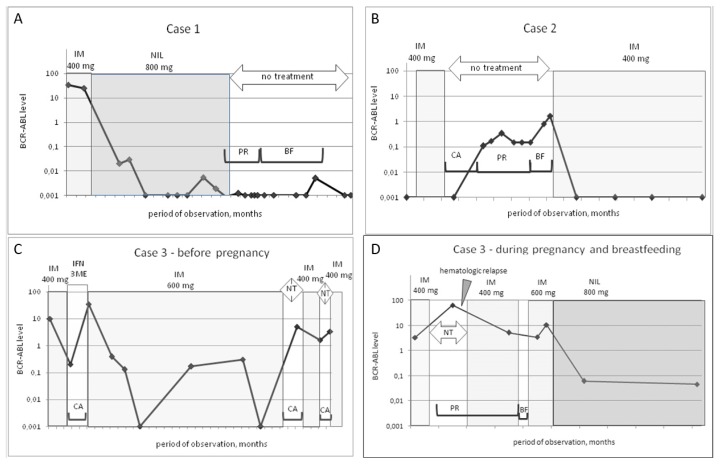
Case 1
A 32-year old woman with CML CP and low Sokal score had achieved a CHR but no cytogenetic response after 6 months on imatinib 400 mg and was switched to nilotinib at a dose of 800 mg. The patient conceived after 3.8 years of nilotinib therapy and stopped the drug from the fourth week of gestation. The patient had a stable DMR for 2 years before pregnancy and during whole pregnancy with BCR-ABL levels less than 0.0032%. Median (Me) time interval between subsequent molecular tests during pregnancy was 7 weeks (from 5 to 9 weeks). The treatment-free period was prolonged in order to breastfeed and it lasted for 19 months with no loss of DMR. Me time interval of molecular monitoring during breastfeeding period was 12 weeks (from 3 to 33 weeks). On the day when the breastfeeding was ended, the patient took 400 mg nilotinib and samples of breast milk were collected. After that, the patient did not restart nilotinib and continued treatment-free observation with molecular monitoring. Molecular tests were done every 3–6 months. The DMR was maintained (Figure 1a). Her total treatment-free period at the last follow-up was 37 months. The follow-up of the child for more than 2 years showed no developmental delay.
Figure 1.
Levels of BCR-ABL in patients with chronic myeloid leukaemia in accordance with pregnancy and breastfeeding periods. IM- imatinib, NIL- nilotinib, IFN- interferon alpha, CA- conceiving attempt, PR- pregnancy, BF –breastfeeding. NT- no treatment. Observation is shown with 3- month time intervals.
Case 2
A 30-year-old woman with CML CP and low Sokal score had been receiving treatment with imatinib at a dose of 400 mg for 7 years. A DMR was achieved which was stable for more than 6 years, and the BCR-ABL level was undetectable with the sensitivity of the PCR method of > 4.5 lg. The patient wished to become pregnant and stopped the drug intake. A pregnancy occurred after 5 months. At the onset of the pregnancy, the major molecular response (MMR) was lost and the level of BCR-ABL was 0.11%. Further tests during pregnancy showed fluctuations of BCR-ABL levels between 0.1% and 0.35%. Me time interval between molecular tests during pregnancy was 6 weeks (from 3 to 9 weeks). The patient insisted on breastfeeding. The treatment-free period was extended. Two molecular tests were done during breastfeeding period with time interval of 10 and 5 weeks. The last test showed the BCR-ABL level was 1.65% after nearly 3 months of breastfeeding. The breastfeeding was terminated, treatment with imatinib at a dose of 400 mg was resumed. The total duration of the treatment-free period for conception, pregnancy and breastfeeding was 18 months. The DMR was restored 4 months after restarting imatinib and remained stable for the following 2 years of follow-up. Molecular monitoring was done every 6 months after treatment resuming (Figure 1b). The child met the milestones of development during 2.5 years of follow-up.
Case 3
A 33-year old woman with CML CP and low Sokal score had received imatinib treatment before pregnancy for nearly 9 years. A first attempt to conceive was made after 1 year of imatinib 400 mg, when no MMR was achieved and only BCR-ABL level<1% was observed. The patient stopped taking imatinib and was switched to interferon alpha (IFN). No pregnancy took place, the BCR-ABL level increased to 35%, and the patient restarted treatment with imatinib. The dose of imatinib was increased to 600 mg and the patient continued this treatment for 6 years. A DMR was reached but it was not stable and long-lasting. Two more attempts to conceive with imatinib interruption for 3–7 months were made by the patient. The DMR was lost, the BCR-ABL level raised to 3%, and again no pregnancy occurred. The patient restarted treatment with imatinib at a dose of 400 mg (Figure 1c).
The last attempt to stop taking imatinib and to conceive with the help of in vitro fertilization was successful. The off-treatment period for conception lasted for 1 month and it was prolonged after pregnancy confirmation. The molecular test which was done at the 10th week of gestation (2.5 months after treatment was stopped) showed a BCR-ABL level of 65%. The haematological relapse of CML which was reflected by the loss of CHR was observed after 1 month. The whole treatment-free period during conception/pregnancy lasted for 5 months. Imatinib at 400 mg was resumed in the second trimester after the 16th week of gestation as imatinib was a drug with a high efficacy in this patient and has a low placental transfer.12 The CHR was restored in 3 weeks. The next molecular test during pregnancy was done 3 months after the administration of imatinib. The level of BCR-ABL was 5,16%. It was strongly recommended to the patient that she should continue imatinib after labour. However, the patient interrupted treatment to breastfeed and resumed imatinib at a dose of 600 mg after 1 month. She maintained CHR, but nearly 3 months after delivery the level of BCR-ABL increased to 10%. No BCR-ABL mutations were found. The patient was switched to nilotinib at a dose of 800 mg and the MMR was achieved in 3 months. (Figure 1d). The MMR remained stable during further observation. The recommended frequency of molecular monitoring every 3 months was not followed properly by the patent. The follow-up of the child for nearly 3 years showed no developmental delay and no growth retardation.
Concentration of imatinib and nilotinib in maternal breast milk
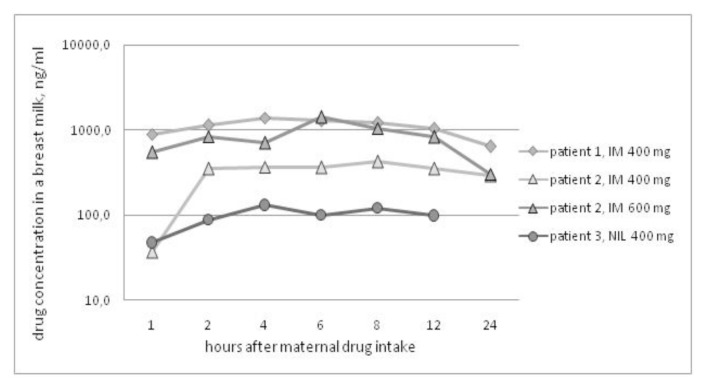
Four series of samples were analysed (Figure 2). In case 1, the patient received nilotinib at 400 mg; in case 2, the patient received imatinib at 400 mg; and in case 3, the patient received imatinib at 400 mg on day 1 and imatinib at 600 mg on the second day of milk-sample collection. One sample after 24 hours of nilotinib intake was missed, and other samples were collected according to the schedule.
Figure 2.
Concentration of nilotinib and imatinib in breast milk.
The maximum concentration (Cmax) of nilotinib in breast milk was 129 ng/ml after 4 hours of the drug intake in case 1. The Cmax of imatinib in breast milk at a dose of 400 mg was 1402 ng/ml after 4 hours of the drug intake and 420 ng/ml after 8 hours in cases 2 and case 3, respectively. The Cmax of imatinib after a dose of 600 mg was 1411 ng/ml after 6 hours of the drug intake in case 3.
Discussion
Lactation and breastfeeding are biological mechanisms that have been established in mammals, including humans, during years of evolution. Besides nutrition, the benefits of breastfeeding for the child include supporting the immune system and protection from infectious, autoimmune and other diseases.13 The emotional perception of women regarding breastfeeding may be connected with psychological, social and cultural factors.14 Mothers with CML may also ask whether they are permitted to breastfeed their children
It has been found that imatinib distributes to maternal milk as well as its active metabolite N-desmethyl derivative (or CGP74588) (Table 2). The milk/plasma ratio for CGP74588 was higher than for imatinib: 0.9–3 vs 0,5.7,9 The calculated maximal dose of imatinib plus CGP74588 that a child could take daily with the maternal milk was less than 3 mg. This dose corresponds to 0.75% of the standard maternal dose of 400 mg and it is much lower than the lowest paediatric dose of imatinib of 260 mg/m2 recommended for children with CML.15 However, experience of imatinib use in the first year of an infant’s life is very rare as the median age of paediatric CML patients is nearly 12 years.16 Some studies have reported impaired bone growth, growth hormone synthesis and vitamin D metabolism resulting in growth retardation in children with CML who received imatinib.17,18 Nilotinib has been just recently approved for use in children with CML and no extensive data can be taken from the pediatric population today.
Table 2.
Data from the literature regarding imatinib concentration in human breast milk and breastfeeding
| № | Literature source | Main observation | IM concentration in breast milk, | IM metabolite N-desmethyl derivative (CGP74588) concentration in milk | Time after IM maternal dose, hours | Calculated ratio of concentrations of IM and IM metabolite | Calculated daily dose of IM for an infant | Conclusion |
|---|---|---|---|---|---|---|---|---|
| 1 | Russel et al [6] | IM and its metabolite were found in breast milk in high concentrations in a single point measurement | 596 ng/ml | 1513 ng/ml | 15 | - | From 1,2 to 2 mg | The risk to an infant consuming the drug at the levels observed in breast milk is probably small. The long-term side effects of IM exposure and the neonatal pharmacokinetics of IM metabolism are not established |
| 2 | Gambacorti-Passerini et al [7] | IM and its metabolite were found in breast milk at several time points, IM plasma blood levels were analysed in parallel | 3–3,2 μg/ml | 0.8–11 μg/ml | 1, 2, 3, 4 and 9 | Milk/plasma ratio 0.5 for IM and 0.9 for CGP 74588. | < 3mg | The expected exposure for infant is about 10% of a therapeutic dose. The effects of low-dose, chronic exposure of infants to IM are not known |
| 3 | Ali et al [8] | IM was found in breast milk in a series of measurements from 7th to 16th day postpartum | From 1430 to 2623 ng/ml | - | From 10 to 16 | - | - | Breast feeding during IM therapy seems to be safe; but, the effects of chronic infant exposure to IM are not known. Breastfeeding is not advisable |
| 4 | Kronenberg el al [9] | IM and its metabolite were found in breast milk at several time points, IM blood levels were analysed in parallel. The accumulation of a CGP 74588 in milk was observed | From 751 to 1153 ng/ml | From 409 to 1052 ng/ml | 3, 27, 51, 171 | Milk/plasma ratio nearly 0.5 for IM and nearly 3 for CGP 74588. CGP 74588/IM ratio in milk from 54% to 132% |
- | Breastfeeding cannot be recommended during treatment with IM |
| 5 | Burwick et al [10] | IM and its metabolite were found in breast milk. IM blood levels were analysed in parallel. The accumulation of a CGP 74588 in milk was observed | 18.9 ng/ml | 658 ng/ml | 99 | - | - | Breastfeeding is discouraged. IM and its metabolite concentrate in breast milk. Longer period of drug cessation would be recommended if mother got IM before breastfeeding. |
Our concentration measurements of imatinib in maternal breast milk correspond with the drug levels described earlier (Table 2) and demonstrate the inter-individual and dose-depending variations (Figure 2). The concentration measurements of nilotinib in maternal milk described here are, to the best of our knowledge, the first in a woman with a single dose of nilotinib 400 mg once a day. Nilotinib penetration into human breast milk is evident. Based on our data, the estimated maximum daily dose which an infant may take is nearly 1 mg for imatinib and 0,1 mg for nilotinib since the maximum daily milk intake is considered as being 1000 ml. Therefore, we deduce that the calculated doses of these TKIs which an infant may ingest with the maternal milk are less than the therapeutical doses. However, the unknown effects of the low-dose chronic exposure to imatinib in infants in the first year of life and no data of nilotinib durable impact on infants’ development are the main concerns limiting the use of these TKIs during breastfeeding.
The key issue for treatment interruption during pregnancy or breastfeeding in patients with CML is the risk of disease progression. It has been demonstrated that treatment-free remission is safe in CML patients with stable and long-lasting DMR with a 40%-60% probability of maintaining an MMR without treatment.19,20 Our case series represents different situations of the leukaemic cells kinetics in CML patients without treatment ranging from stable DMR to haematological relapse. Stopping treatment during breastfeeding may be dangerous in patients without DMR/MMR and lead to further insufficient treatment response. A close molecular monitoring is needed for the patients who extend the off-treatment period for the breastfeeding. If the MMR loss after treatment cessation is confirmed breastfeeding needs to be terminated and TKI treatment should be restarted. We consider that recommendation to use a bottle feeding is the safe choice. The recommendation to avoid TKIs and to give breastfeeding for the short period of the first 2–5 days after labour to give the child colostrum5 may be acceptable as well.
The women with CML who plan pregnancy should be aware of the risks of taking TKIs during breastfeeding as well as the risks of remission loss if the treatment is discontinued.
Footnotes
Competing interests: The authors have declared that no competing interests exist.
References
- 1.Sasaki K, Kantarjian HM, Jain P, et al. Conditional survival in patients with chronic myeloid leukemia in chronic phase in the era of tyrosine kinase inhibitors. Cancer. 2016;122(2):238–248. doi: 10.1002/cncr.29745. https://doi.org/10.1002/cncr.29745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Law AD, Dong Hwan Kim D, Lipton JH. Pregnancy: part of life in chronic myelogenous leukemia. Leuk Lymphoma. 2017;58(2):280–287. doi: 10.1080/10428194.2016.1201571. https://doi.org/10.1080/10428194.2016.1201571. [DOI] [PubMed] [Google Scholar]
- 3.Cortes JE, Abruzzese E, Chelysheva E, Guha M, Wallis N, Apperley JF. The impact of dasatinib on pregnancy outcomes. Am J Hematol. 2015;90(12):1111–1115. doi: 10.1002/ajh.24186. https://doi.org/10.1002/ajh.24186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Palani R, Milojkovic D, Apperley JF. Managing pregnancy in chronic myeloid leukemia. Ann Hematol. 2015;94(2):S167–S176. doi: 10.1007/s00277-015-2317-z. https://doi.org/10.1007/s00277-015-2317-z. [DOI] [PubMed] [Google Scholar]
- 5.Abruzzese E, Trawinska MM, Perrotti AP, De Fabritiis P. Tyrosine Kinase Inhibitors and Pregnancy. Mediterr J Hematol Infect Dis. 2014 Apr 7;6(1):e2014028. doi: 10.4084/MJHID.2014.028. https://doi.org/10.4084/mjhid.2014.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Russel MA, Carpenter MW, Akhtar MS, Lagattuta TF, Egorin MJ. Imatinib mesylate and metabolite concentration in maternal blood, umbilical cord blood, placenta and breast milk. J Perinatol. 2007;27(4):241–243. doi: 10.1038/sj.jp.7211665. https://doi.org/10.1038/sj.jp.7211665. [DOI] [PubMed] [Google Scholar]
- 7.Gambacorti-Passerini CB, Tornaghi L, Marangon E, Franceschino A, Enrico M, Pogliani EM, D’Incalci M, Zucchetti M. Imatinib concentrations in human milk. Blood. 2007;109:1790. doi: 10.1182/blood-2006-08-039545. https://doi.org/10.1182/blood-2006-08-039545. [DOI] [PubMed] [Google Scholar]
- 8.Ali R, Ozkalemkas F, Kimya Y, Koksal N, Ozkocaman V, Gulten T, Yorulmaz H, Tunali A. Imatinib use during pregnancy and breast feeding: a case report and review of the literature. Arch Gynecol Obstet. 2009;280:169–175. doi: 10.1007/s00404-008-0861-7. https://doi.org/10.1007/s00404-008-0861-7. [DOI] [PubMed] [Google Scholar]
- 9.Kronenberger R, Schleyer E, Bornhäuser M, Ehninger G, Gattermann N, Blum S. Imatinib in breast milk. Ann Hematol. 2009;88:1265–1266. doi: 10.1007/s00277-009-0754-2. https://doi.org/10.1007/s00277-009-0754-2. [DOI] [PubMed] [Google Scholar]
- 10.Burwick RM, Kuo K, Brewer D, Druker BJ. Maternal, fetal, and neonatal imatinib levels with treatment of chronic myeloid leukemia in pregnancy. Obstet Gynecol. 2017;129:831–4. doi: 10.1097/AOG.0000000000001972. https://doi.org/10.1097/AOG.0000000000001972. [DOI] [PubMed] [Google Scholar]
- 11.Baccarani M, Deininger MW, Rosti G, et al. European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood. 2013;122(6):872–84. doi: 10.1182/blood-2013-05-501569. https://doi.org/10.1182/blood-2013-05-501569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chelysheva E, Turkina A, Polushkina E, et al. Placental transfer of tyrosine kinase inhibitors used for chronic myeloid leukemia treatment. Leuk Lymphoma. 2018 Mar;59(3):733–738. doi: 10.1080/10428194.2017.1347929. https://doi.org/10.1080/10428194.2017.1347929. [DOI] [PubMed] [Google Scholar]
- 13.Brahm P, Valdés V. The benefits of breastfeeding and risks associated with not breastfeeding. Rev Chil Pediatr. 2017;88(1):15–21. doi: 10.4067/S0370-41062017000100001. https://doi.org/10.4067/S0370-41062017000100001. [DOI] [PubMed] [Google Scholar]
- 14.Shepherd L, Walbey C, Lovell B. The role of social-cognitive and emotional factors on exclusive breastfeeding duration. Journal of Human Lactation. 2017;33(3):606–613. doi: 10.1177/0890334417708187. https://doi.org/10.1177/0890334417708187. [DOI] [PubMed] [Google Scholar]
- 15.De la Fuente J, Baruchel A, Biondi A, et al. International BFM Group (iBFM] Study Group Chronic Myeloid Leukaemia Committee. Managing children with chronic myeloid leukaemia (CML): recommendations for the management of CML in children and young people up to the age of 18 years. Br J Haematol. 2014;167:33–47. doi: 10.1111/bjh.12977. https://doi.org/10.1111/bjh.12977. [DOI] [PubMed] [Google Scholar]
- 16.Millot F, Guilhot J, Suttorp M, et al. Prognostic discrimination based on the EUTOS long-term survival score within the International for Chronic Myeloid Leukemia in children and adolescents Registry. Haematologica. 2017 Oct;102(10):1704–1708. doi: 10.3324/haematol.2017.170035. https://doi.org/10.3324/haematol.2017.170035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Millot F, Guilhot J, Baruchel A, et al. Growth deceleration in children treated with imatinib for chronic myeloid leukaemia. Eur J Cancer. 2014 Dec;50(18):3206–11. doi: 10.1016/j.ejca.2014.10.007. https://doi.org/10.1016/j.ejca.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 18.Rastogi MV, Stork L, Druker B, et al. Imatinib mesylate causes growth deceleration in pediatric patients with chronic myelogenous leukemia. Pediatr Blood Cancer. 2012 Nov;59(5):840–5. doi: 10.1002/pbc.24121. https://doi.org/10.1002/pbc.24121. [DOI] [PubMed] [Google Scholar]
- 19.Saussele S, Richter J, Hochhaus A, Mahon FX. The concept of treatment-free remission in chronic myeloid leukemia. Leukemia. 2016;30(8):1638–1647. doi: 10.1038/leu.2016.115. https://doi.org/10.1038/leu.2016.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hughes TP, Ross DM. Moving treatment-free remission into mainstream clinical practice of CML. Blood. 2016;128:17–23. doi: 10.1182/blood-2016-01-694265. https://doi.org/10.1182/blood-2016-01-694265. [DOI] [PubMed] [Google Scholar]