Abstract
Study Design
A retrospective, propensity score, multivariate analysis of the National Trauma Data Bank (NTDB) between 2008 and2011.
Objective
The aim of this study was to determine the relationship between insurance status and rates of surgery for acute spinal fractures with and without spinal cord injury (SCI).
Summary of Background Data
The decision for surgery in patients with spinal fractures is often based on fracture pattern and stability, associated SCI, and the presence of ligamentous and other associated injuries. It is poorly understood how nonclinical factors, such as insurance status, influence the decision for surgical intervention in patients sustaining spinal trauma.
Methods
Using NTDB admission years 2008 to 2011, we included patients 18 to 64 years old who sustained a fracture of the cervical or thoracolumbar spine. Patients were excluded if they sustained polytrauma (Injury Severity Score >=27) or a major injury (Abbreviated Injury Scale severity >=3) to the head, thorax, or abdomen. Our main outcome measure was surgical versus nonsurgical treatment for spinal injury; our main predictor was insurance status. Hierarchical multivariate regression analysis and propensity scores were used to determine the relationship between insurance status and surgical treatment, controlling for other factors. We calculated adjusted odds ratios (ORs) for rates of surgery.
Results
Our propensity score multivariate analysis demonstrated significantly higher rates of surgery in patients with SCI (OR = 11.76, P < 0.001), insurance (OR = 1.27, P < 0.001), white (OR = 1.21, P = 0.018) versus black race, blunt trauma (OR = 5.63, P < 0.001), shock (OR = 1.62, P < 0.001), higher Glasgow Coma Scale (GCS) score (OR = 1.02, P = 0.002), transfer from lower acuity hospital (OR = 1.51, P < 0.001), and treatment at teaching hospitals (OR = 1.49, P < 0.001). Multivariable subgroup analysis of SCI patients similarly revealed higher surgical rates for insured patients (OR = 1.46, P < 0.001) than those without insurance.
Conclusion
Patients with traumatic spine fractures were more likely to receive surgery if they were insured, regardless of the presence of SCI.
Fractures of the spinal column are common, with an estimated annual incidence of 64 per 100,000 population or approximately 200,000 new cases each year in the United States.1 Traumatic spinal fractures with spinal cord injury (SCI) account for some of the most devastating injuries in this group and result in significant morbidity, mortality, and cost.2–4 Fractures to the spinal column, especially those with SCI, are frequently treated surgically. The decision to proceed with surgical intervention is based on many factors, including fracture pattern and stability, the presence of ligamentous and other associated injuries, and the occurrence of neurological deficits. Scoring systems have been developed to aid surgeons in deciding on the need for surgical intervention. These scoring systems recognize patient neurologic status as a vital component of the decision for surgery.5,6
Universal access to health care does not exist in the United States. As a result, significant disparities in the delivery of health care services persist.7 Despite recent political efforts to establish universal health care and provide insurance for the uninsured, the number of Americans without health insurance remains significant. In 2010, the US Census Bureau reported that 49.9 million Americans (16.3%) were uninsured, up from 45.7 million (15.3%) in 2007.8 Because of discrepancies in access, uninsured adults in the United States are less likely to receive necessary medical care.9,10 Furthermore, morbidity and mortality is higher in uninsured patients, specifically those sustaining traumatic injuries.11–13 The etiology of this finding is undoubtedly multifactorial. Possible underlying mechanisms may include treatment delay, undiagnosed and untreated pre-existing comorbidities, decreased health literacy, or differential treatment based on provider disincentives.9,11–13
It is poorly understood how nonclinical factors, such as insurance status, influence the decision for surgical intervention in patients sustaining spinal trauma. This study aims to determine the influence of insurance coverage on the rate of surgical intervention for acute cervical and thoracolumbar spine fractures with and without SCI.
MATERIALS AND METHODS
Data Source
We obtained data from the National Trauma Data Bank (NTDB) for admission years 2008 to 2011. The NTDB is maintained by the American College of Surgeons and represents the largest and most complete repository of trauma data in the United States.14 For admission years 2008 to 2011, a total of 831 trauma centers voluntarily contributed over 9.3 million trauma records to the NTDB. Each record contains information characterizing the patient (eg, age, sex, race, comorbidities, insurance status), their injuries (eg, ICD-9 diagnosis codes, indicators of anatomic and physiologic injury severity), treatment rendered (ICD-9 procedure codes), and outcomes (eg, mortality, length of stay, ventilator days, complications, discharge disposition).
Selection Criteria
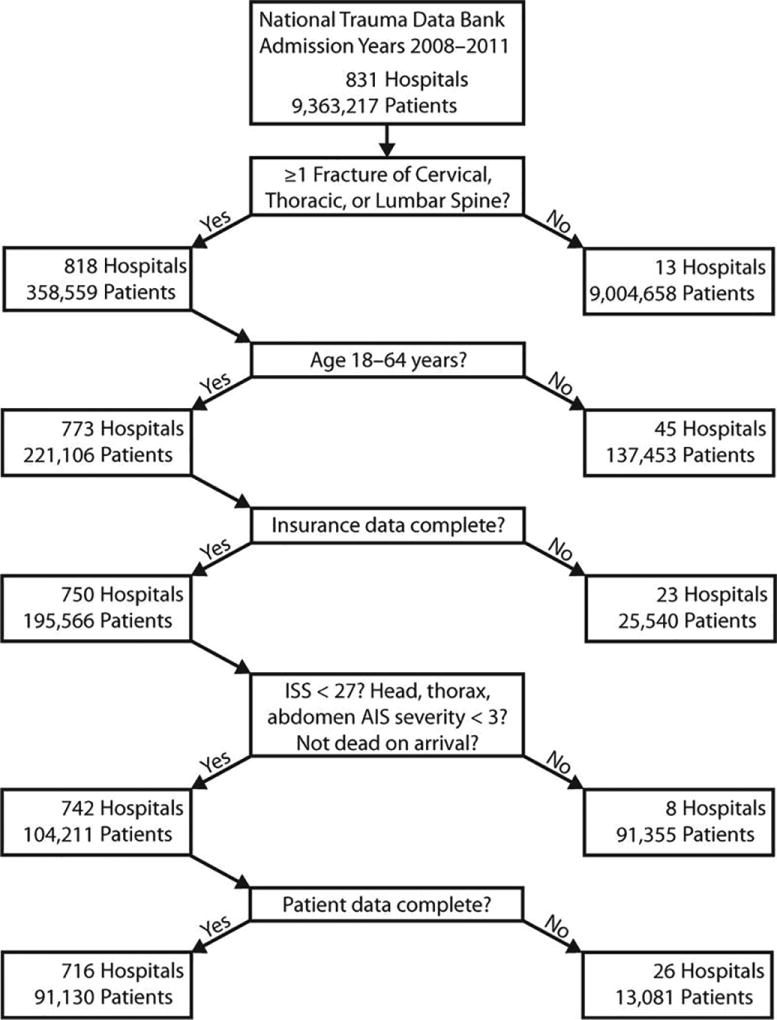
In total, 91,130 patients met selection criteria and were included in our analysis (Figure 1). We included all patients 18 to 64 years of age treated at a participating trauma facility after sustaining a fracture of the cervical or thoracolumbar spine with or without SCI according to ICD-9 diagnosis codes (see Text, Supplementary Digital Content 1, http://links.lww.com/BRS/B28).
To capture patients with similar likelihood of having insurance, we limited patient age from 18 to 64, as pediatric (<=17 years of age) and older (>=65 years of age) patients were assumed to have a higher likelihood of government-sponsored insurance. As insurance is our primary predictor, we excluded patients if they had incomplete insurance data. Patients were also excluded if they were dead on arrival or died in the emergency department (ED); if they sustained major polytrauma (Injury Severity Score [ISS] >=27)15 or a major injury (Abbreviated Injury Scale [AIS] severity score >=3)16,17 to the head, thorax, or abdomen; or if they had incomplete data for baseline variables (patient demographics, injury characteristics, hospital factors) used as covariates in our multivariable analysis.
Data Elements
For all trauma incidents meeting selection criteria, we abstracted information for our main outcome (surgery), main predictor (insurance status), and other covariates, including age, gender, race, pre-existing comorbidities, fracture location (cervical, thoracolumbar, or multilevel [>=1 cervical and >=1 thoracolumbar fracture]), presence of SCI, type of injury (blunt or penetrating), mechanism of injury (eg, motor vehicle traffic, fall, firearm, struck by/against), injury intent (unintentional, assault, self-inflicted), presence of shock in the ED, total Glasgow Coma Scale (GCS) score in the ED, transfer status, hospital nonprofit status, and hospital teaching status.
Serious comorbidities are correlated with poor outcomes and may hinder initial clinical assessment and patient response to resuscitation following major trauma,18 which in turn may influence the decision for surgery and confound our analysis. To account for comorbid status, we used the Deyo–Charlson comorbidity index (DCI)19—a modification of the original Charlson comorbidity index proposed by Deyo et al19 for use with administrative databases. We dichotomized DCI into 0 and at least 1 reported comorbidities for each traumatic incident in the NTDB.
Our main outcome measure was surgical treatment of the patient's spinal injury based on ICD-9 procedure codes for treatments rendered during their initial hospitalization (see Text, Supplementary Digital Content 2, http://links.lww.com/BRS/B28). Insurance status was categorized as uninsured (self-pay; no charge) or insured (private/commercial; Blue Cross/Blue Shield; no fault/automobile; Government [Medicaid, Medicare, worker's compensation, other government]; Other) according to the definitions and guidelines of the National Healthcare Cost and Utilization Project.20
Statistical Methods
We analyzed baseline variables using bivariate statistics (t test and Chi-square) for our unadjusted comparisons. Bivariate analysis was first performed between insured and uninsured patients to discover unadjusted differences in rates of surgery as well as unadjusted differences in clinical factors (age, gender, race, pre-existing comorbidities, fracture location, SCI, injury type, injury mechanism, injury intent, shock, and GCS in the ED) and nonclinical factors (transfer status, hospital nonprofit status, and hospital teaching status).
We performed multiple logistic regression analyses to control for observed confounders in our adjusted comparisons. We used hierarchical modeling to account for clustering by hospital facility. Propensity scores were used to standardize (and provide an unbiased estimate of) the effect of having insurance coverage on the basis of measured baseline covariates in the analysis of surgical treatment. We performed a propensity-controlled multiple logistic regression as well as a propensity-matched analysis controlling for other covariates to standardize and match on the likelihood of having insurance. Because our propensity-controlled and propensity score matched analyses yielded similar results, we present only our propensity-controlled analysis.
Using the propensity-controlled, hierarchical multivariable logistic regression model, we determined adjusted odds ratios (ORs) for likelihood of having surgery, controlling for insurance status, clinical factors, and nonclinical factors (as delineated above). All statistical significance tests were 2-tailed; statistical significance was defined as P value less than 0.05 (SAS 9.3; SAS Institute, Cary, NC).
RESULTS
We identified 91,130 spine fracture patients who met selection criteria (Figure 1). There were 62,427 men (69%) and 28,703 women (31%) with mean age 40 years. Most patients were white (78%), insured (79%), and lacked any serious pre-existing comorbidities (91%). The majority of patients suffered unintentional injuries (96%) secondary to blunt trauma (98%), usually in the setting of motor vehicle traffic accidents (51%) or falls (31%). Fractures of the thoracolumbar spine (62%) occurred approximately twice as often as cervical spine fractures. A total of 5562 (6%) sustained a SCI (Table 1).
| Variable | Neurological Status | Insurance Status | |||||
|---|---|---|---|---|---|---|---|
| Total (N = 91,130) |
SCI (n = 5562) |
No SCI (n = 85,568) |
P | Insured (n = 71,938) |
Uninsured (n = 19,192) |
P | |
| Patient characteristics | |||||||
| Mean age | 40.9 ± 14 | 39.9 ± 14 | 42.0 ± 14 | <0.001 | 41.8 ± 14 | 37.5 ± 12 | <0.001 |
| Male (%) | 62,427 (69) | 4292 (77) | 58,135 (68) | <0.001 | 47,864 (67) | 14,563 (76) | <0.001 |
| Race/Ethnicity (%) | <0.001 | <0.001 | |||||
| White | 70,546 (78) | 4069 (73) | 66,477 (78) | 57,957 (80) | 12,589 (65) | ||
| Black | 10,318 (11) | 906 (16) | 9412 (11) | 7119 (10) | 3199 (17) | ||
| Hispanic | 10,266 (11) | 587 (11) | 9679 (11) | 6862 (10) | 3404 (18) | ||
| ≥1 comorbidity* (%) | 7358 (8) | 404 (7) | 6954 (8) | 0.022 | 6372 (9) | 986 (5) | <0.001 |
| Insured (%) | 71,938 (79) | 4480 (81) | 67,458 (79) | 0.002 | NA | NA | NA |
| Injury characteristics | |||||||
| SCI (%) | 5562 (6) | NA | NA | NA | 4480 (6) | 1082 (6) | 0.002 |
| Fracture (%) | <0.001 | <0.001 | |||||
| Cervical | 27,985 (31) | 2857 (51) | 25,128 (29) | 21,770 (30) | 6215 (33) | ||
| Thoracolumbar | 56,163 (62) | 2217 (40) | 53,946 (63) | 44,615 (62) | 11548 (60) | ||
| Multilevel | 6982 (8) | 488 (9) | 6494 (8) | 5553 (8) | 1429 (7) | ||
| Injury Type (%) | <0.001 | <0.001 | |||||
| Blunt | 89,450 (98) | 5214 (94) | 84,236 (98) | 70,986 (99) | 18464 (96) | ||
| Penetrating | 1680 (2) | 348 (6) | 1332 (2) | 952 (1) | 728 (4) | ||
| Injury intent (%) | <0.001 | <0.001 | |||||
| Unintentional | 87,291 (96) | 5100 (92) | 82,191 (96) | 69,559 (97) | 17,732 (92) | ||
| Assault | 2890 (3) | 367 (7) | 2523 (3) | 1687 (2) | 1203 (6) | ||
| Self-inflicted | 736 (1) | 58 (1) | 678 (1) | 552 (1) | 184 (1) | ||
| Injury mechanism (%) | <0.001 | <0.001 | |||||
| MVT | 46,686 (51) | 2172 (39) | 44,514 (52) | 36,893 (51) | 9793 (51) | ||
| Fall | 27,997 (31) | 2118 (38) | 25,879 (30) | 22,404 (31) | 5593 (29) | ||
| Transport, other | 8956 (10) | 517 (9) | 8439 (10) | 7196 (10) | 1760 (9) | ||
| Struck by/against | 3766 (4) | 266 (5) | 3500 (4) | 2790 (4) | 976 (5) | ||
| Firearm | 1407 (2) | 325 (6) | 1082 (1) | 792 (1) | 615 (3) | ||
| Shock† | 1569 (2) | 261 (5) | 627 (2) | <0.001 | 1265 (2) | 304 (2) | 0.10 |
| Mean CCS | 14.6 ± 2 | 14.3 ± 2 | 14.6 ± 2 | <0.001 | 14.6 ± 2 | 14.5 ± 2 | <0.001 |
| Hospital care | |||||||
| Transferred‡ (%) | 28,866 (32) | 1861 (34) | 27,005 (32) | 0.003 | 23,063 (32) | 5803 (30) | <0.001 |
| Nonprofit hospital (%) | 84,170 (92) | 5057 (91) | 79,113 (92) | <0.001 | 66,579 (93) | 17,591 (92) | <0.00l |
| Teaching hospital (%) | 45,833 (50) | 2918 (52) | 42,915 (50) | 0.027 | 35,251 (49) | 10,582 (55) | <0.001 |
Percentages may not add to 100% due to rounding or due to exclusion of variable categories with negligible frequency. Continuous variables expressed as mean ± standard deviation or median (IQR); Categorical variables expressed as number of trauma incidents (%). Cervical indicates ≥1 cervical fracture; GCS, Glasgow Coma Scale in the Emergency Department; multilevel, ≥1 cervical fracture and ≥1 thoracolumbar fracture; MVT, motor vehicle traffic; NA, not applicable; SCI, spinal cord injury; thoracolumbar, ≥1 thoracolumbar fracture.
Comorbidity categorized using the Deyo–Charlson Comorbidity Index (see text for details).
Shock is defined as systolic blood pressure <90 mm Hg in the Emergency Department.
“Transferred” indicates patients transferred in from an outside acute care facility.
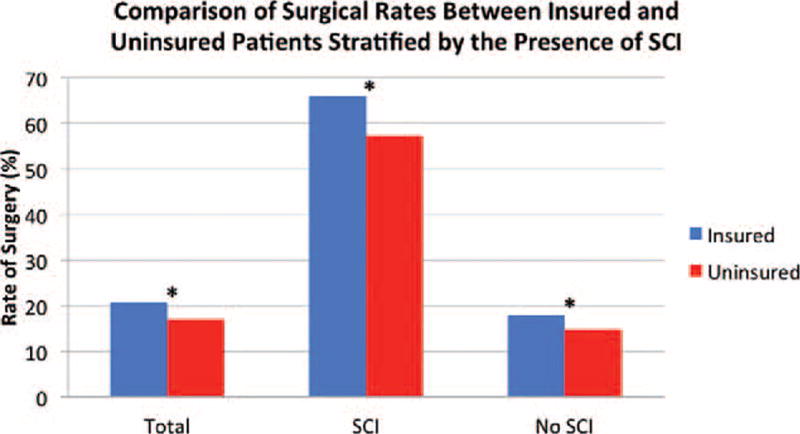
Overall, 20% (18,656/91,130) of patients received surgical treatment for their spinal injury. Surgical rates were higher in insured (21%) than in uninsured (17%) patients and in patients who sustained SCI (66%) relative to those who did not (17%). In our unadjusted bivariate comparisons, surgery was significantly associated with insurance (P < 0.001), race (P < 0.001), SCI (P < 0.001), and fracture location (P < 0.001) (Table 2).
| Variable | N | Rate of Surgery (%) | OR (95% CI) | P |
|---|---|---|---|---|
| Total cohort | 91,130 | 18,656 (20.5%) | ||
| Patient characteristics | ||||
| Mean age | NA | NA | 0.9990 (0.998–0.999) | 0.005 |
| Gender | ||||
| Male | 62,427 | 12,938 (20.7%) | 1.05 (1.01–1.09) | 0.005 |
| Female | 28,703 | 5718 (19.9%) | 1 | |
| Rate/Ethnicity | <0.001 | |||
| White | 70,546 | 14,694 (20.8%) | 1 | |
| Black | 10,318 | 1950 (18.9%) | 0.89 (0.84–0.93) | <0.001 |
| Hispanic | 10,266 | 2012 (19.6%) | 0.93 (0.88–0.98) | 0.004 |
| ≥1 comorbidity* | ||||
| Yes | 7358 | 1475 (20.0%) | 0.97 (0.92–1.03) | 0.35 |
| No | 83,772 | 17,181 (20.5%) | 1 | |
| Insurance status | ||||
| Insured | 71,938 | 15,253 (21.2%) | 1.25 (1.20–1.30) | <0.001 |
| Uninsured | 19,192 | 3403 (17.7%) | 1 | |
| Injury characteristics | ||||
| Neurological status | ||||
| SCI | 5562 | 3686 (66.3%) | 9.27 (8.74–9.83) | <0.001 |
| No SCI | 85,568 | 14,970 (17.5%) | 1 | |
| Fracture Location | <0.001 | |||
| Cervical | 27,985 | 6336 (22.7%) | 1 | |
| Thoracolumbar | 56,163 | 10,714 (19.1%) | 0.81 (0.78–0.83) | <0.001 |
| Multilevel | 6982 | 1606 (23.0%) | 1.02 (0.96–1.09) | 0.52 |
| Injury type | ||||
| Blunt | 89,450 | 18,498 (20.7%) | 2.51 (2.13–2.98) | <0.001 |
| Penetrating | 1680 | 158 (9.4%) | 1 | |
| Injury intent | <0.001 | |||
| Unintentional | 87,291 | 18,138 (20.8%) | 1 | |
| Assault | 2890 | 266 (9.2%) | 0.39 (0.34–0.44) | <0.001 |
| Self-inflicted | 736 | 207 (27.9%) | 1.49 (1.26–1.76) | <0.001 |
| Mechanism of injury | <0.001 | |||
| MVT | 46,686 | 8881 (19.0%) | 1 | |
| Fall | 27,997 | 6578 (23.5%) | 1.31 (1.26–1.36) | <0.001 |
| Transport, other | 8956 | 1924 (21.5%) | 1.16 (1.10–1.23) | <0.001 |
| Struck by/against | 3766 | 692 (18.4%) | 0.96 (0.88–1.04) | 0.33 |
| Firearm | 1407 | 138 (9.8%) | 0.46 (0.38–0.55) | <0.001 |
| Hemodynamic status† | ||||
| Shock | 1569 | 490 (31.2%) | 1.78 (1.60–1.99) | <0.001 |
| No shock | 89,561 | 18,166 (20.3%) | 1 | |
| Mean GCS | NA | NA | 0.9956 (0.990–1.001) | 0.10 |
| Hospital care | ||||
| Transfer status‡ | ||||
| Transferred | 28,866 | 7647 (26.5%) | 1.68 (1.62–1.73) | <0.001 |
| Not transferred | 62,264 | 11,009 (17.7%) | 1 | |
| Hospital nonprofit status | ||||
| For profit | 6960 | 1548 (22.2%) | 1.12 (1.06–1.19) | <0.001 |
| Nonprofit | 84,170 | 17,108 (20.3%) | 1 | |
| Hospital teaching status | ||||
| Teaching | 45,833 | 10,291 (22.5%) | 1.28 (1.24–1.32) | <0.001 |
| Non-teaching | 45,297 | 8365 (18.5%) | 1 | |
Note: Percentages may not add to 100% due to rounding or due to exclusion of variable categories with negligible frequency. Cervical indicates ≥1 cervical fracture; GCS, Glasgow Coma Scale in the Emergency Department; multilevel, ≥1 cervical fracture and ≥1 thoracolumbar fracture; MVT, motor vehicle traffic; NA, not applicable; OR, unadjusted odds ratio representing relative likelihood of having surgery; SCI, spinal cord injury; thoracolumbar, ≥1 thoracolumbar fracture.
Comorbidity categorized using the Deyo–Charlson Comorbidity Index (see text for details).
Shock is defined as systolic blood pressure <90 mm Hg in the Emergency Department.
“Transferred” indicates patients transferred in from an outside acute care facility.
Our multivariate propensity score regression analysis, after accounting for hospital clustering, demonstrated significantly higher rates of surgery in patients with SCI (OR 11.76, P < 0.001) and insurance (OR 1.27, P < 0.001), among other variables. Age, gender, comorbidity, fracture location, and hospital nonprofit status were not significantly associated with surgical rates (Table 3).
| Variable | OR (95% CI) | P |
|---|---|---|
| Propensity score | 0.398 (0.102–1.551) | 0.18 |
| Age | 1.000(0.996–1.005) | 0.96 |
| Gender | 0.30 | |
| Male | 0.953 (0.371–1.044) | |
| Female | 1 | |
| Race/Ethnicity | 0.033 | |
| White | 1 | |
| Black | 0.825 (0.703–0.967) | 0.018 |
| Hispanic | 0.863 (0.718–1.037) | 0.12 |
| ≥1 comorbidity* | 0.32 | |
| No | 1 | |
| Yes | 1.052 (0.953–1.162) | |
| Insurance status | <0.001 | |
| Insured | 1.269 (1.211–1.330) | |
| Uninsured | 1 | |
| Fracture location | 0.06 | |
| Cervical | 1 | |
| Thoracolumbar | 1.007 (0.964–1.052) | 0.74 |
| Multilevel | 1.083 (1.010–1.161) | 0.025 |
| Spinal cord injury | <0.001 | |
| Yes | 11.759(10.785–12.821) | |
| No | 1 | |
| Injury type | <0.001 | |
| Blunt | 5.626 (4.407–7.181) | |
| Penetrating | 1 | |
| Shock† | <0.001 | |
| Yes | 1.617(1.424–1.837) | |
| No | 1 | |
| GCS | 1.018(1.007–1.030) | 0.002 |
| Transferred‡ | <0.001 | |
| Yes | 1.513 (1.455–1.574) | |
| No | 1 | |
| Hospital teaching status | <0.001 | |
| Teaching | 1.490 (1.264–1.756) | |
| Nonteaching | 1 | |
| Hospital nonprofit status | 0.31 | |
| Nonprofit | 1 | |
| For-profit | 0.891 (0.691–1.150) |
OR, adjusted odds ratio representing relative likelihood of having surgery controlling for covariates (see text). Cervical indicates ≥1 cervical fracture; ED, Emergency Department; GCS, Glasgow Coma Scale; Multilevel, ≥ 1 cervical fracture and ≥ 1 thoracolumbar fracture; Thoracolumbar, ≥ 1 thoracolumbar fracture.
Comorbidity categorized using the Deyo-Charlson Comorbiclity Index (see text for details).
Shock is defined as systolic blood pressure <90mm Hg in the Emergency Department.
“Transferred” indicates patients transferred in from an outside acute care facility.
Subgroup analysis of patients with and without SCI demonstrated higher surgical rates in insured patients. In patients without SCI, surgical rates were higher in insured (18%) than in uninsured (15%) patients (bivariate unadjusted OR, 1.22; 95% confidence interval [95% CI], 1.16–1.27; P < 0.001). In patients with SCI, we found a similar but more pronounced disparity in surgical rates—insured patients with SCI had a surgical rate of 68% compared with 57% in the uninsured (bivariate unadjusted OR, 1.59; 95% CI, 1.38–1.82; P < 0.001) (Figure 2). Multivariate, propensity-controlled subgroup analysis of the 5562 SCI patients demonstrated significantly higher rates of surgery in patients with insurance (OR, 1.46; 95% CI, 1.23–1.72; P < 0.001) (Table 4).
| Variable | OR (95% CI) | P |
|---|---|---|
| Propensity score | 0.175 (0.002–18.812) | 0.46 |
| Age | 0.983 (0.970–0.997) | 0.020 |
| Gender | 0.97 | |
| Male | 1.005 (0.752–1.344) | |
| Female | 1 | |
| Race/Ethnicity | 0.23 | |
| White | 1 | |
| Black | 0.690 (0.419–1.135) | 0.14 |
| Hispanic | 0.776 (0.433–1.388) | 0.39 |
| ≥ 1 comorbidity‡ | 0.93 | |
| No | 1 | |
| Yes | 1.016 (0.721–1.431) | |
| Insurance status | <0.001 | |
| Insured | 1.455 (1.233–1.716) | |
| Uninsured | 1 | |
| Fracture location | 0.010 | |
| Cervical | 1 | |
| Thoracolumbar | 0.930 [0.801–1.081) | 0.51 |
| Multilevel | 0.703 (0.560–0.882) | 0.010 |
| Type of injury | <0.001 | |
| Blunt | 11.397 (5.995–21.668) | |
| Penetrating | 1 | |
| Shock* | 0.032 | |
| Yes | 1.443 (1.033–2.016) | |
| No | 1 | |
| GCS | 1.049 (1.018–1.081) | 0.002 |
| Transferred† | 0.010 | |
| Yes | 1.215 (1.049–1.408) | |
| No | 1 | |
| Hospital teaching status | 0.010 | |
| Teaching | 1.603(1.163–2.210) | |
| Non-teaching | 1 | |
| Hospital nonprofit status | 0.78 | |
| Nonprofit | 1 | |
| For-profit | 0.937 (0.384–2.289) |
OR, adjusted odds ratio representing relative likelihood of having surgery controlling for covariates (see text). Cervical indicates ≥ 1 cervical fracture; ED, Emergency Department; GCS, Glasgow Coma Scale; Multilevel, ≥1 cervical fracture and ≥1 thoracolumbar fracture; Thoracolumbar, ≥1 thoracolumbar fracture.
Shock is defined as systolic blood pressure <90 mmHg in the Emergency Department.
“Transferred” indicates patients transferred in from an outside acute care facility.
Comorbidity categorized using the Deyo-Charhon Comorbidity Index (See text for details).
DISCUSSION
Spinal column fractures are common and account for significant morbidity and cost. The decision for surgery is usually based on important clinical factors such as fracture pattern or stability, and the presence of neurological impairment. The role of insurance coverage in influencing the decision for surgery is less well known. In this study, we aimed to assess the relationship between insurance status and surgical treatment among subjects with acute spinal fractures using the NTDB. Using a propensity-controlled multivariable analysis, we found that insured patients were significantly more likely to receive surgery than their uninsured counterparts. In addition, we even found that in the spinal cord injured patient subgroup, patients with insurance were more likely to receive surgical treatment than uninsured patients. These findings suggest that insurance status influences the utilization of urgent surgical services in patients with acute spinal fractures, regardless of the presence of SCI.
Disparities in musculoskeletal health and other health care disciplines are being reported with increasing frequency.21,22 A recent systematic review identified several reports of discrepancies in surgical rates for elective orthopedic procedures based on insurance status.23 Dunlop et al24 reported lower rates of total joint arthroplasty (OR, 0.45; 95% CI, [0.22–0.90]) in patients with Medicare coverage only (without supplemental insurance). In a study by Hanchate et al,25 the authors demonstrated lower rates of total knee arthroplasty in uninsured patients (OR, 0.61; 95% CI, 0.40–0.92) than those holding private insurance. McWilliams et al26 found that, compared with those who were continuously insured, patients without prior insurance had higher rates of total joint arthroplasty after receiving Medicare coverage (OR, 0.45; 95% CI, 0.22–0.90, P = 0.006). These studies suggest that rates of certain elective, nonemergent surgical procedures depend on insurance coverage, with a higher likelihood of receiving surgery if a patient has insurance. Given that the United States’ current healthcare reimbursement structure remains predominantly fee-for-service, such discrepancies in surgical rates might depend on insurance status due to financial incentives and/or disincentives, especially for elective nonemergent procedures wherein out-of-pocket expense may be prohibitively high for the uninsured. What is more difficult to understand and explain, however, are insurance status-based disparities in outcomes (eg, mortality) and health service utilization (eg, rates of surgery, use of diagnostic tests, transfers) in the setting of acute traumatic injury, wherein emergent treatment may be immediately necessary to reduce morbidity and mortality and wherein disparities based on payer status should not exist.
Previous reports have used the NTDB to examine disparities in trauma care.12,13,27–34 Several studies have used the NTDB to identify an association between insurance status and mortality in the setting of traumatic injury.12,13,27–29 In a study of general acute trauma patients, Haider et al13 found that both race and insurance status independently predict mortality following trauma and noted that racial disparities could not simply be explained by differences in insurance status. In this same study, the odds of mortality was 46% higher for uninsured trauma patients than for insured trauma patients.13 In an attempt to reduce the effect of medical comorbidities, Downing et al27 similarly noted a significant difference in risk of death in young trauma patients (ages 19–30 years) who were uninsured. Insurance status was a stronger predictor of mortality than gender or race.27 Furthermore, in the pediatric trauma population (17 years or younger), higher mortality has been noted in uninsured children or those with Medicaid than those who are commercially insured.12 Stratifying broadly by injury mechanism, Greene et al28 found that in both penetrating and blunt trauma, uninsured patients had a higher mortality than insured patients. Further delineating this effect, Crandall et al29 studied a single injury type (ie, lower extremity vascular injuries) and noted that after stratifying by mechanism of injury, mortality differences as a function of race or insurance status were only seen for penetrating trauma and not blunt trauma. The authors proposed that potential explanations for these findings included both genetic differences in the response to penetrating trauma and biases in providing care for those with violent penetrating injuries.29
The studies outlined above suggest that, even in the setting of acute traumatic injury, there may be significant disparities in outcomes and the provision of emergent health care services based on patient insurance status. Similarly, the present study demonstrates a significant disparity in the delivery of emergent surgical services—in a cohort drawn of more than 5500 patients with traumatic spinal fractures associated with SCI, those with insurance coverage were more likely to undergo surgery than the uninsured. How can we eliminate this disparity? Our understanding of the underlying causes of this disparity is currently incomplete, making it difficult to assert full confidence in any proposed solutions. However, we feel that specialized SCI centers, either with supplemental funding or offset by a more diverse payer mix, might eventually play a role in providing more equitable surgical care.
The management of patients suffering from acute SCI is complex, requiring the collaboration of a wide range of specialists including the spine surgeon, physical therapist, occupational therapist, psychologist, nurse coordinator, physiatrist, and social worker. Coordinating the care of these patients, from the acute treatment period through rehabilitation and long-term social/vocational re-integration is therefore challenging. Specialized SCI centers, first established in the US by Donald Munro in the 1930s 35 and in the UK by Sir Ludwig Guttman in the 1940s,36 have been developed to facilitate a comprehensive multidisciplinary approach and to improve the neurological recovery of patients with acute SCI.3,35,36 A systematic review by Parent et al3 identified several retrospective studies examining the effect of specialized SCI tertiary care centers on outcomes. On the basis of the best available evidence, the authors concluded that early transfer to specialized SCI centers decreases overall length of stay and mortality.3 In addition to improving outcomes in patients with acute SCI, do specialized SCI centers also help allocate health care services more equitably? If so, increasing the percentage of patients treated initially at, or transferred early to, specialized SCI centers may alleviate insurance-based disparities in surgical rates. Further studies exploring this or similar hypotheses may be warranted.
We recognize several limitations to our study. First, as contributing trauma centers voluntarily report data, the NTDB represents a convenience sample that may not be representative of all US trauma centers.11,12 Although this makes the NTDB susceptible to selection bias,37 this limitation may be at least partially mitigated by the NTDB's tremendous size and the fact that most Level 1 trauma centers do receive government funding for the care of uninsured patients, thus potentially underestimating differences in the provision of care for uninsured patients.14 Second, poor or inconsistent charting and data abstraction may limit NTDB data quality and reliability.38 However, the ACS has taken definitive steps to address data quality, most notably through its adoption of the National Trauma Data Standard (NTDS) in 2007, which created national standards for inclusion criteria, data coding, and submission.39 Therefore, to ensure that we were working with the highest quality data available, we based our analysis exclusively on data collected after 2007. Third, due to the inherent lack of specificity in ICD-9 diagnosis codes, it was not possible to further classify each spine fracture according to more clinically accepted classification systems (eg, compression, burst, seat-belt-type, fracture-dislocation).40
Our analysis of over 91 100 traumatic spinal fractures suggests that insurance status is a more important determinant of treatment than previously recognized. Among those who sustained cervical or thoracolumbar injuries, patients with health insurance coverage were significantly more likely to receive surgery than patients without medical insurance. Moreover, when compared with their uninsured counterparts, insured patients with traumatic spine fractures were more likely to receive surgery even in the presence of SCI. These findings suggest that discrepancies exist in the standard of care for these injuries based on payer status. Further studies are needed to explore the provision of care for patients sustaining spinal fractures to identify potentially modifiable factors influencing the decision for surgery and improve disparities in the delivery of health care services.
Supplementary Material
Key Points.
-
*
After excluding those with polytrauma (ISS >=27) or major injury (AIS severity >=3) to the head, thorax, or abdomen, we identified 91,130 adult patients (18–64 years old) with traumatic spine fracture—6% sustained associated SCI; 79% had insurance.
-
*
In the complete cohort of 91,130 patients, there were higher rates of surgery in those with associated SCI (OR 11.76, P < 0.001), insurance (OR 1.27, P < 0.001), white (OR 1.21, P = 0.018) versus black race, blunt trauma (OR 5.63, P < 0.001), shock (OR 1.62, P < 0.001), higher GCS score (OR 1.02, P = 0.002), transfer from lower acuity hospital (OR 1.51, P < 0.001), and treatment at teaching hospitals (OR 1.49, P < 0.001).
-
*
In the subset of 5562 patients with traumatic spine fracture and associated SCI, we found higher rates of surgery in patients with insurance (OR 1.46, P < 0.001) than those without insurance.
-
*
Our analysis of over 91,100 traumatic spinal fractures suggests that insurance status is a more important determinant of treatment than previously recognized.
Acknowledgments
No funds were received in support of this work.
Footnotes
The manuscript submitted does not contain information about medical device(s)/drug(s).
Relevant financial activities outside the submitted work: board membership, consultancy, expert testimony, royalties, payment for development of educational presentations, stocks.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.spinejournal.com).
References
- 1.Hu R, Mustard CA, Burns C. Epidemiology of incident spinal fracture in a complete population. Spine (Phila Pa 1976) 1996;21:492–499. doi: 10.1097/00007632-199602150-00016. [DOI] [PubMed] [Google Scholar]
- 2.Sekhon LH, Fehlings MG. Epidemiology demographics and pathophysiology of acute spinal cord injury. Spine (Phila Pa 1976) 2001;26(Suppl 24):S2–S12. doi: 10.1097/00007632-200112151-00002. [DOI] [PubMed] [Google Scholar]
- 3.Parent S, Barchi S, LeBreton M, et al. The impact of specialized centers of care for spinal cord injury on length of stay, complications, and mortality: a systematic review of the literature. J Neurotrauma. 2011;28:1363–1370. doi: 10.1089/neu.2009.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spinal Cord Injury Facts and Figures at a Glance [Internet] National Spinal Cord Injury Statistical Center; Birmingham, Alabama: 2013. [accessed November 1, 2015]. [cited January 29, 2014]. Available at: https://www.nscisc.uab.edu/PublicDocuments/fact_figures_docs/Facts%202013.pdf. [Google Scholar]
- 5.Vaccaro AR, Lehman RA, Hurlbert RJ, et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976) 2005;30:2325–2333. doi: 10.1097/01.brs.0000182986.43345.cb. [DOI] [PubMed] [Google Scholar]
- 6.Vaccaro AR, Hulbert RJ, Patel AA, et al. Spine Trauma Study Group. The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976) 2007;32:2365–2374. doi: 10.1097/BRS.0b013e3181557b92. [DOI] [PubMed] [Google Scholar]
- 7.National Research Council. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press; 2001. Committee on Quality of Health Care in America, Institute of Medicine. [Google Scholar]
- 8.DeNavas-Walt C, Proctor BD. [accessed November 1, 2015];Smith JC US Census Bureau Current Population Reports (P60-239): Income, Poverty, and Health Insurance Coverage in the United States. 2010 Issued September 2011. Available at: http://www.census.gov/prod/2011pubs/p60-239.pdf.
- 9.Ayanian JZ, Weissman JS, Schneider EC, et al. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061–2069. doi: 10.1001/jama.284.16.2061. [DOI] [PubMed] [Google Scholar]
- 10.Richardson LC, Tangka FK. Ambulatory care for cancer in the United States: results from two national surveys comparing visits to physicians’ offices and hospital outpatient departments. J Natl Med Assoc. 2007;99:1350–1358. [PMC free article] [PubMed] [Google Scholar]
- 11.Rosen H, Saleh F, Lipsitz S, et al. Downwardly mobile: the accidental cost of being uninsured. Arch Surg. 2009;144:1006–1011. doi: 10.1001/archsurg.2009.195. [DOI] [PubMed] [Google Scholar]
- 12.Rosen H, Saleh F, Lipsitz SR, et al. Lack of insurance negatively affects trauma mortality in US children. J Pediatr Surg. 2009;44:1952–1957. doi: 10.1016/j.jpedsurg.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 13.Haider AH, Chang DC, Efron DT, et al. Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143:945–949. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 14.Haider AH, Saleem T, Leow JJ, et al. Influence of the National Trauma Data Bank on the study of trauma outcomes: is it time to set research best practices to further enhance its impact? J Am Coll Surg. 2012;214:756–768. doi: 10.1016/j.jamcollsurg.2011.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McLain RF, Benson DR. Urgent surgical stabilization of spinal fractures in polytrauma patients. Spine (Phila Pa 1976) 1999;24:1646–1654. doi: 10.1097/00007632-199908150-00005. [DOI] [PubMed] [Google Scholar]
- 16.Greenspan L, McLellan BA, Greig H. Abbreviated Injury Scale and Injury Severity Score: a scoring chart. J Trauma. 1985;25:60–64. doi: 10.1097/00005373-198501000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Baker SP, O’Neill B, Haddon W, et al. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- 18.Wardle TD. Co-morbid factors in trauma patients. Br Med Bull. 1999;55:744–756. doi: 10.1258/0007142991902754. [DOI] [PubMed] [Google Scholar]
- 19.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 20.Stranges, E. (Thomson Reuters), Kowlessar, N. (Thomson Reuters) and Davis, P.H. (Agency for Healthcare Research and Quality). Uninsured Hospitalizations, 2008. HCUP Statistical Brief #108. April 2011. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb108.pdf
- 21.Groman R, Ginsburg J American College of Physicians. Racial and ethnic disparities in health care: a position paper of the American College of Physicians. Ann Intern Med. 2004;141:226–232. doi: 10.7326/0003-4819-141-3-200408030-00015. [DOI] [PubMed] [Google Scholar]
- 22.Nelson CL. Disparities in orthopaedic surgical intervention. J Am Acad Orthop Surg. 2007;15(Suppl 1):S13–S17. doi: 10.5435/00124635-200700001-00005. [DOI] [PubMed] [Google Scholar]
- 23.Bederman SS, Rosen CD, Bhatia NN, et al. Drivers of surgery for the degenerative hip, knee, and spine: a systematic review. Clin Orthop Relat Res. 2012;470:1090–1105. doi: 10.1007/s11999-011-2004-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dunlop DD, Song J, Manheim LM, et al. Racial disparities in joint replacement use among older adults. Med Care. 2003;41:288–298. doi: 10.1097/01.MLR.0000044908.25275.E1. [DOI] [PubMed] [Google Scholar]
- 25.Hanchate AD, Zhang Y, Felson DT, et al. Exploring the determinants of racial and ethnic disparities in total knee arthroplasty: health insurance, income, and assets. Med Care. 2008;46:481–488. doi: 10.1097/MLR.0b013e3181621e9c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McWilliams JM, Meara E, Zaslavsky AM, et al. Medicare spending for previously uninsured adults. Ann Intern Med. 2009;151:757–766. doi: 10.7326/0003-4819-151-11-200912010-00149. [DOI] [PubMed] [Google Scholar]
- 27.Downing SR, Oyetunji TA, Greene WR, et al. The impact of insurance status on actuarial survival in hospitalized trauma patients: when do they die? J Trauma. 2011;70:130–134. doi: 10.1097/TA.0b013e3182032b34. [DOI] [PubMed] [Google Scholar]
- 28.Greene WR, Oyetunji TA, Bowers U, et al. Insurance status is a potent predictor of outcomes in both blunt and penetrating trauma. Am J Surg Elsevier Inc. 2010;199:554–557. doi: 10.1016/j.amjsurg.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 29.Crandall M, Sharp D, Brasel K, et al. Lower extremity vascular injuries: increased mortality for minorities and the uninsured? Surgery. 2011;150:656–664. doi: 10.1016/j.surg.2011.07.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bolorunduro OB, Haider AH, Oyetunji TA, et al. Disparities in trauma care: are fewer diagnostic tests conducted for uninsured patients with pelvic fracture? Am J Surg. 2013;205:365–370. doi: 10.1016/j.amjsurg.2012.10.026. [DOI] [PubMed] [Google Scholar]
- 31.Bjurlin MA, Zhao LC, Goble SM, et al. Race and insurance status are risk factors for orchiectomy due to testicular trauma. J Urol. 2012;187:931–935. doi: 10.1016/j.juro.2011.10.152. [DOI] [PubMed] [Google Scholar]
- 32.Pickham DM, Callcut RA, Maggio PM, et al. Payer status is associated with the use of prophylactic inferior vena cava filter in high-risk trauma patients. Surgery. 2012;152:232–237. doi: 10.1016/j.surg.2012.05.041. [DOI] [PubMed] [Google Scholar]
- 33.Babu MA, Nahed BV, Demoya MA, et al. Is trauma transfer influenced by factors other than medical need? An examination of insurance status and transfer in patients with mild head injury. Neurosurgery. 2011;69:659–667. doi: 10.1227/NEU.0b013e31821bc667. [DOI] [PubMed] [Google Scholar]
- 34.Parks J, Gentilello LM, Shafi S. Financial triage in transfer of trauma patients: a myth or a reality? Am J Surg. 2009;198:e35–e38. doi: 10.1016/j.amjsurg.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 35.Donovan WH. Donald Munro Lecture. Spinal cord injury - past, present, and future. J Spinal Cord Med. 2007;30:85–100. doi: 10.1080/10790268.2007.11753918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Frankel HL. The Sir Ludwig Guttmann lecture 2012: the contribution of Stoke Mandeville Hospital to spinal cord injuries. Spinal Cord. 2012;50:790–796. doi: 10.1038/sc.2012.109. [DOI] [PubMed] [Google Scholar]
- 37.Glance LG, Osler TM, Dick A, et al. The relation between trauma center outcome and volume in the National Trauma Databank. J Trauma. 2004;56:682–690. doi: 10.1097/01.ta.0000053469.92142.40. [DOI] [PubMed] [Google Scholar]
- 38.Crompton JG, Pollack KM, Oyetunji T, et al. Racial disparities in motorcycle-related mortality: an analysis of the National Trauma Data Bank. Am J Surg. 2010;200:191–196. doi: 10.1016/j.amjsurg.2009.07.047. [DOI] [PubMed] [Google Scholar]
- 39. [cited August 16, 2012];National Trauma Data Standard Data Dictionary 2012 Admissions [Internet] 2012 Available at: http://www.ntdsdictionary.org/dataElements/documents/NTDS2012_xsd_Final_102011.pdf.
- 40.Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 1983;8:817–831. doi: 10.1097/00007632-198311000-00003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


