Abstract
Background and Aims
Adolescents and young adults increasingly view cannabis as a relatively safe drug. Perception of risk associated with cannabis use is negatively correlated with the prevalence of use, but the causal nature of this association is debated. The aim of this study is to quantitate the reciprocal associations between cannabis use and risk perception in a longitudinal panel of emerging adults.
Design
Observational study of longitudinal data from the Monitoring the Future longitudinal study using auto-regressive cross-lagged panel analyses to investigate reciprocal associations between cannabis risk perception and frequency of past year cannabis use.
Setting
Surveys administered to 12th grade students from the United States general population.
Participants
9,929 12th grade students (95% ages 17–18) who were initially surveyed during the years 2000–2005 and follow-up data through 6 years (3 waves; N=9,929).
Measurements
Perception of risk association with cannabis use and frequency of past-year cannabis use.
Results
At baseline, 33% of the 12th graders used cannabis in the past year versus 28% by the third follow-up; 83% believed that smoking cannabis regularly carried moderate or great risk versus 78% by the third follow-up. All cross-lagged paths in both directions were statistically significant (all p<0.001), consistent with reciprocal influences between cannabis use and risk perception. The negative association between past-year cannabis use and subsequent risk-perception (standardized coefficient range −0.21 to −0.27) was stronger than that between risk perception and subsequent use (standardized coefficient range −0.08 to −0.11; confidence intervals did not overlap with those for the coefficients reported above). Similar results were obtained when the analysis was limited to those who had never used cannabis prior to baseline.
Conclusions
Longitudinal associations between cannabis use and perception of risks from cannabis use are reciprocal in nature, with a stronger association between cannabis use and lower subsequent risk perception.
Keywords: Cannabis use, Cannabis, Hashish, Risk perception, perceived harm, Longitudinal
Introduction
Cannabis is the most commonly used federally proscribed drug in the U.S; 2014 estimates suggest 22.2 million Americans use cannabis in any given 30 day period (1). Cannabis is particularly popular among youth, with nearly a quarter of U.S. adolescents aged 13–18 reporting past-30 day use (2). While the long-term health effects of cannabis use are an area of active research, the Institute of Medicine recently evaluated existing evidence on consequences of cannabis use. Their report concludes that there is substantial evidence that cannabis use increases risk for motor vehicle accidents, may contribute to development or exacerbation of schizophrenia and other psychotic disorders among vulnerable individuals, cause respiratory symptoms and increase frequency of chronic bronchitis episode, and lead to lower birth weight among offspring of mothers who smoke cannabis during pregnancy (3).
There has been a gradual decline in recent years in the percentage of adolescents and adults who perceive cannabis use as risky. Results from 2002 to 2014 U.S. national surveys show that the proportion of adults who believe that there is at least moderate risk associated with using cannabis once or twice a week decreased from 50.4% to 33.3% (4). As with other drugs, risk perception has been consistently found to be negatively correlated with cannabis use (5–7). This association is often interpreted by drug prevention advocates as being causal and unidirectional; i.e., that decreases in the perception of risk lead to increases in use (8). The logical implication of this interpretation is that drug prevention programs maintain high risk perceptions will lead to decrease prevalence of use (9).
However, most studies of associations between risk perceptions and cannabis use have relied on data from cross-sectional surveys and therefore have not been able to address the potentially reciprocal associations between risk perception and cannabis use. That is, the association between risk perception and use may arise in part because those who do not experience adverse consequences from cannabis use are likely to modify their risk perception. In fact, results from qualitative studies have shown that the perceived risk of cannabis use is reportedly inferred, to a large extent, from individual experience with use (10,11). That is, if the experience is generally positive, cannabis is regarded as a low-risk drug. Conversely, if the user experiences negative consequences from his/her use, they are more likely to perceived it as a high-risk behavior and avoid it. Thus, these findings offer a compelling argument for studying whether there is a reverse causation between cannabis use and risk perception.
One longitudinal study of 318 participants suggested reciprocal associations: that risk perception was associated with subsequent cannabis use and that cannabis use was associated with subsequent risk perception (12). However, not all reciprocal associations were significant and the relatively wide confidence intervals precluded comparison of effect magnitudes (i.e., risk perception to use vs. use to risk perception). Aside from this relatively small study, there remains a paucity of empirical evidence for the direction of association between these two variables. Hence, in the present report, we describe longitudinal analyses of whether association patterns between risk perception and cannabis use are consistent with the interpretation that risk perception is a cause of cannabis use, whether temporal associations might suggest reverse-causation, or both. To accomplish this, we assembled data from the Monitoring the Future (MTF) longitudinal panel, which consists of a subset of the annual 12th grade sample who are followed into adulthood. This design allowed us to assemble a large sample of individuals for whom cannabis use and risk perceptions were assessed at multiple points in time. We estimated a full cross-lagged panel analysis using path analysis of data from Monitoring the Future (MTF) longitudinal panel, enabling us to examine the degree to which risk perception predicts subsequent cannabis use and vice versa.
Methods
Participants
We used participant data from the MTF longitudinal panel. MTF is an ongoing annual survey of adolescents in 8th, 10th, and 12th grades selected to be representative of students throughout the coterminous U.S. A three stage sampling procedure is used for student selection including geographic area, one or more schools within each geographic area, and students within each school. Each year, a sample of approximately 2,400 participants from the 13,000–19,000 12th graders participating in the cross-sectional survey is selected for longitudinal follow-up. Those reporting heavy cannabis use or any use of other illicit drugs are selected for the longitudinal panel with higher probability; thus differential weighting is used for analyses to account for differential sampling probabilities. Students selected for the longitudinal study are asked to complete follow-up surveys every other year after they graduate until approximately 11 or 12 years beyond high school (i.e., age 29 or 30). Half of the chosen sample from each cohort is followed on even years and half on odd-numbered years (13,14).
We used participant data from panel members who were given the baseline 12th grade survey in 2000–2005 (T0) and included three additional follow-up surveys (T1, T2, T3) until approximately age 23 to 24 years and who completed survey forms containing questions about both cannabis use and cannabis risk perceptions (weighted N=9,929 panel members).
Measures
Perceptions of regular cannabis use were assessed at baseline and at each follow-up using the question “How much do you think people risk harming themselves (physically or in other ways) if they smoke marijuana regularly?” Likert scales response options included (1) No risk, (2) Slight risk, (3) Moderate risk, or (4) Great risk. We used the natural log of this scale for purposes of analysis in our models described below.
Cannabis use in the past year was assessed at baseline and at each follow-up using the question “On how many occasions (if any) have you used marijuana (weed, pot) or hashish (hash, hash oil) during the last 12 months?” Similarly, cannabis use in the past month was assessed at baseline and at each follow-up with the item “On how many occasions (if any) have you used marijuana (weed, pot) or hashish (hash, hash oil) during the last 30 days?”. Response options for both cannabis use items included 0 occasions, 1–2 occasions, 3–5 occasions, 6–9 occasions, 10–19 occasions, 20–39 occasions, and 40 or more occasions. These responses were recoded into a continuous scale: 0 occasions, 1.5 occasions, 4 occasions, 7.5 occasions, 14.5 occasions, 29.5 occasions, 40 occasions. In our models described below, we used the natural log of this continuous scale (after adding one to all values to avoid taking the log of zero which is not defined).
Demographic characteristics of participants were assessed at baseline, including gender (male/female), race/ethnicity (White/Caucasian, Black/African American, Hispanic, Other), age, parents’ education level (dichotomized as ≤high school/≥some college), number of parents that lived in the home (0, 1, 2), and whether the student lived in a metropolitan statistical area (large MSA, other MSA, non-MSA).
Statistical analysis
We performed full cross-lagged panel models using path analysis to investigate the lagged associations between cannabis risk perception and cannabis use. This type of model allowed for the examination of whether risk perceptions are associated with subsequent cannabis use or vice versa, assessing both directional hypotheses in the same model (15). The linear regression model included cross-lagged effects of cannabis risk perceptions and cannabis use (i.e., prior observed risk perceptions influence subsequent cannabis use, and prior observed cannabis use influences subsequent risk perceptions) while also incorporating autoregressive effects (i.e., prior observed risk perceptions are associated with subsequent risk perceptions, and prior observed cannabis use are associated with subsequent cannabis use). Risk-perception and cannabis use measures were log-transformed and treated as continuous predictors/outcomes in the model. Primary models focused on past past-year use cannabis use with secondary analyses employing past-month use in lieu of past-year use. Models included gender and race as predictors of risk perceptions and cannabis use at baseline. We ran additional models further adjusting for parents’ education level, whether the participant lived in a two-parent household, and whether the student lived in a metropolitan statistical area. Results from these models were virtually identical to models adjusting for gender and race; therefore, for brevity, we present models adjusting for gender and race only. In order to contrast the results from our analyses of cannabis use with other substances, we analyzed the data for tobacco and alcohol use in the same sample (see Supplementary Material).
To examine whether reciprocal trajectories for cannabis use and risk perception differ after initiation of cannabis use, we also conducted the cross-lagged panel analyses on the two sub-samples defined by ever having used cannabis at index. For never-users, we omitted the time 0 cannabis use term since there is no variation on this variable. Other than that modification, the model was specified as above.
To determine the relative importance of each type of cross-lagged effect to model fit, we also estimated three other models to compare to the full cross-lagged model described above: (A) autoregressive effects only, (B) model A plus risk perception predicting subsequent use, (C) model A plus use predicting subsequent risk perception. All models also included demographic characteristics (gender, race) as predictors of risk perceptions and cannabis use at baseline (T0). Fit of the nested models was compared using Akaike Information Criterion (AIC) and the Bayesian Information Criterion (BIC) (16,17). These statistics are parsimony-adjusted goodness-of-fit measures and are derived from log-likelihood values with adjustment for the number of parameters in the model. The BIC weights model parsimony more heavily than the AIC and is the preferred statistic for large samples (18). In addition, each model was compared to model involving only autoregressive effects using the Satorra-Bentler scaled chi-square difference test This test is commonly used in path analysis and structural equations modeling and is a variation of the chi-square likelihood-ratio test that is robust to deviations from normality (19,20).
SAS version 9.4 for Windows (SAS Institute, Inc., Cary, NC) was used for descriptive statistics, employing survey procedures to apply MTF panel survey weights. MPlus version 7.4 was used for the above-described models of observed variables, and survey weights were applied (20). The Maximum likelihood estimation with robust standard errors (MLR) was used. MLR uses a full information maximum likelihood (FIML) approach, which uses likelihood information from all cases in the sample regardless of whether their data is complete; thus, parameter estimates are based on all available data (20). Standardized regression coefficients, 95% confidence intervals, and p values are presented.
Although models used all available data, participants who did not have any follow-up data beyond baseline differed from those who did respond to follow-up surveys. Those who did not respond to any follow-up surveys were more likely to have used cannabis in the past year (37.3% vs 32.2%, p<0.001) or in the past month (23.1% vs 18.1%, p<0.001) in the 12th grade and to believe that regular cannabis use was not or only slightly risky in the 12th grade (21.9% vs 16.1%, p<0.001). To address any potential bias for data not missing at random, we additionally ran two types of models as a sensitivity analysis: a) including only those who had complete data for variables of interest at all time points, and b) using the Diggle-Kenward selection model, which addresses data not missing at random by including dropout indicators after each time point that are regressed on the outcome at the prior time point and the outcome at the current time point (21). Results from these models are presented in the Supplementary Material.
Results
Characteristics of participants in the sample are shown in Table 1 and generally reflect the demographic composition of U.S. 12th graders during the baseline period. Table 2 presents the past –year and past-month cannabis use and risk perceptions for regular cannabis use at baseline (T0) and at each of the three follow-ups (T1, T2, T3) among those in our sample. At baseline in the 12th grade, 33% used cannabis in the past year and 19% used in the past month. By the third follow-up, 28% reported using cannabis in the past year and 15% in the past month. At baseline 83% believed that smoking cannabis regularly carried moderate to great risk; by the third follow-up, this percentage was 78%.
Table 1.
Baseline demographic characteristics of participants with at least one follow-up (weighted N=9929 unless otherwise noted)
| Demographic Characteristic | Weighted n (%) |
|---|---|
| Gender | |
| Male | 4578 (46) |
| Female | 5351 (54) |
| Race/Ethnicity (n=9728) | |
| White/Caucasian | 6700 (69) |
| Black/African American | 1104 (11) |
| Hispanic | 1081 (11) |
| Other | 844 (9) |
| Age at baseline mean (SE) | 18 (0.005) |
| Father’s educational level (n=9162) | |
| High school or less | 4002 (44) |
| Some college or more | 5159 (56) |
| Mother attended college (n=9461) | |
| High school or less | 3761 (40) |
| Some college or more | 5700 (60) |
| Number of parents in household (n=9854) | |
| Two | 7035 (71) |
| One | 2292 (23) |
| None | 527 (5) |
| Metropolitan Statistical Area (MSA) | |
| Large MSA | 2916 (29) |
| Other MSA | 4596 (46) |
| Non-MSA | 2416 (24) |
| Year of baseline survey administration | |
| 2000 | 1669 (17) |
| 2001 | 1633 (16) |
| 2002 | 1623 (16) |
| 2003 | 1671 (17) |
| 2004 | 1655 (17) |
| 2005 | 1678 (17) |
Table 2.
Marijuana use and risk perceptions among participants over time
| T0: Baseline | T1: 1st follow-up | T2: 2nd follow-up | T3: 3rd follow-up | |
|---|---|---|---|---|
|
| ||||
| Weighted n (%) | Weighted n (%) | Weighted n (%) | Weighted n (%) | |
|
| ||||
| Frequency used marijuana in the past year | N=9738 | N=5654 | N=5326 | N=4919 |
| 0 occasions | 6499 (67) | 3816 (67) | 3709 (70) | 3559 (72) |
| 1–2 occasions | 918 (9) | 564 (10) | 507 (10) | 407 (8) |
| 3–5 occasions | 534 (5) | 286 (5) | 233 (4) | 189 (4) |
| 6–9 occasions | 386 (4) | 192 (3) | 150 (3) | 122 (2) |
| 10–19 occasions | 381 (4) | 204 (4) | 164 (3) | 134 (3) |
| 20–39 occasions | 280 (3) | 150 (3) | 111 (2) | 104 (2) |
| ≥40 occasions | 739 (8) | 442 (8) | 452 (8) | 403 (8) |
|
| ||||
| Frequency used marijuana in the past month | N=9742 | N=5648 | N=5323 | N=4916 |
| 0 occasions | 7882 (81) | 4643 (82) | 4448 (84) | 4165 (85) |
| 1–2 occasions | 648 (7) | 343 (6) | 278 (5) | 239 (5) |
| 3–5 occasions | 314 (3) | 168 (3) | 117 (2) | 105 (2) |
| 6–9 occasions | 200 (2) | 101 (2) | 107 (2) | 71 (1) |
| 10–19 occasions | 223 (2) | 118 (2) | 130 (2) | 99 (2) |
| 20–39 occasions | 209 (2) | 138 (2) | 117 (2) | 103 (2) |
| ≥40 occasions | 266 (3) | 138 (2) | 126 (2) | 135 (3) |
|
| ||||
| Perceived risk from regular marijuana use | N=9521 | N=5583 | N=5271 | N=4847 |
| No risk | 567 (6) | 192 (3) | 231 (4) | 234 (5) |
| Slight risk | 1075 (11) | 728 (13) | 744 (14) | 813 (17) |
| Moderate risk | 2153 (23) | 1380 (25) | 1429 (27) | 1313 (27) |
| Great risk | 5727 (60) | 3283 (59) | 2866 (54) | 2487 (51) |
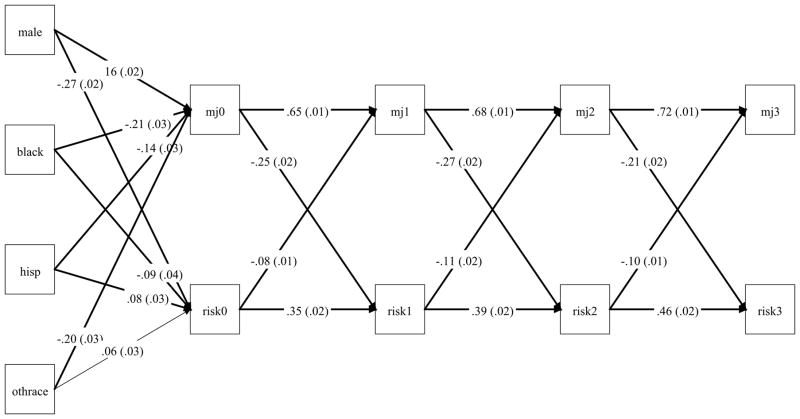
Figure 1 presents results from the cross-lagged model of log-transformed past-year cannabis use and log-transformed risk perceptions, with standardized regression coefficients and standard errors reported; standardized regression coefficients and 95% confidence intervals are enumerated in Table 3 (Model A). All cross-lagged paths in both directions were statistically significant (all p<0.001). Greater belief that regular cannabis use poses risk was associated with lower frequency of cannabis use at subsequent time points, with standardized coefficients ranging from −0.08 to −0.11. Similarly, greater frequency of past year cannabis use was associated with decreased belief that regular cannabis use is risky at subsequent time points; notably, these effects were over twice as large as the effects of risk perception on use (standardized coefficients ranged from −0.21 to −0.27 and confidence intervals did not overlap with those for risk perception). All autoregressive effects for both cannabis use and risk perceptions were positive and significant (all p<0.001). The effects of prior use on subsequent use (coefficients ranged from 0.65 to 0.72) were stronger than the effects of prior risk perceptions on subsequent risk perceptions (coefficients ranged from 0.35 to 0.46), indicating that cannabis use patterns are more stable over time than risk perceptions. Results of models using alternative approaches to missing data differed minimally from those described here. (See Supplementary Material, Table S1). Results from a model using frequency of past-month cannabis use rather than past-year use are shown in Table 3, Model B. These results were similar to those when using past-year cannabis use.
Figure 1.
Cross-lagged model of past year cannabis use (mjt) and risk perception (riskt). Standardized regression coefficients are presented with standard errors in parentheses.
Table 3.
Cross-lagged models of log-transformed frequency of Cannabis use and log-transformed perceptions of risk from regular Cannabis use
| Model results | Model A: (Past-year use + risk perception) Standardized β(95% CI) |
Model B: (Past-month use + risk perceptions) Standardized β (95% CI) |
Model C: (Model A for T0 Never Users) Standardized β (95% CI) |
Model D: (Model A for T0 Ever Users) Standardized β (95% CI) |
|---|---|---|---|---|
| Risk perception at T0 on: | ||||
| Male vs female | −0.27 (−0.31, −0.24) | −0.27 (−0.31, −0.24) | −0.20 (−0.25, −0.15) | −0.29 (−0.34, −0.24) |
| Black vs White | −0.09 (−0.16, −0.02) | −0.09 (−0.16, −0.02)** | −0.21 (−0.32, −0.11) | −0.05 (−0.16, 0.05)ns |
| Hispanic vs White | 0.08 (0.02, 0.14)** | 0.08 (0.03, 0.14)** | −0.10 (−0.20, 0.01)ns | 0.24 (0.16, 0.31) |
| Other race vs White | 0.06 (−0.03, 0.13)* | 0.06 (0.00, 0.13)* | −0.09 (−0.20, 0.01)ns | 0.10 (0.00, 0.20) * |
| Risk perception at T1 on | ||||
| Risk perception at T0 | 0.35 (0.32, 0.39) | 0.38 (0.34, 0.41) | 0.33 (0.27, 0.39) | 0.34 (0.29, 0.39) |
| Cannabis use at T0 | −0.25 (−0.29, −0.22) | −0.22 (−0.25, −0.19) | --------------- | −0.23 (−0.27, −0.18) |
| Risk perception at T2 on | ||||
| Risk perception at T1 | 0.39 (0.35, 0.43) | 0.41 (0.37, 0.45) | 0.35 (0.29, 0.41) | 0.43 (0.37, 0.48) |
| Cannabis use at T1 | −0.26 (−0.30, −0.23) | −0.24 (−0.28, −0.21) | −0.23 (−0.29, −0.17) | −0.22 (−0.27, −0.17) |
| Risk perception at T3 on | ||||
| Risk perception at T2 | 0.46 (0.42, 0.49) | 0.48 (0.44, 0.52) | 0.45 (0.40, 0.51) | 0.45 (0.40, 0.50) |
| Cannabis use at T2 | −0.21 (−0.24, −0.17) | −0.18 (−0.21, −0.14) | −0.14 (−0.19, −0.09) | −0.21 (−0.25, −0.16) |
| Cannabis use at T0/T11 on | ||||
| Male vs female | 0.16 (0.13, 0.20) | 0.19 (0.16, 0.22) | 0.09 (0.02, 0.15)* | 0.19 (0.14, 0.24) |
| Black vs White | −0.21 (−0.26, −0.16) | −0.09 (−0.14, −0.04) | 0.01 (−0.12, 0.13) | −0.30 (−0.38, −0.21) |
| Hispanic vs White | −0.14 (−0.19, −0.09) | −0.14 (−0.16, −0.07) | −0.16 (−0.25, −0.06)ns | −0.25 (−0.33, −0.17) |
| Other race vs White | −0.20 (−0.25, −0.14) | −0.16 (−0.20, −0.11) | −0.08 (−0.18, 0.02) ns | −0.17 (−0.27, −0.06) |
| Cannabis use at T1 on | ||||
| Cannabis use at T0 | 0.65 (0.63, 0.676) | 0.60 (0.57, 0.63) | --------------- | 0.55 (0.52, 0.58) |
| Risk perception at T0 | −0.08 (−0.11, −0.056) | −0.10 (−0.13, −0.07) | −0.13 (−0.18, −0.08) | −0.06 (−0.10, −0.02) |
| Cannabis use at T2 on | ||||
| Cannabis use at T1 | 0.68 (0.66, 0.71) | 0.65 (0.61, 0.68) | 0.54 (0.48, 0.60) | 0.64 (0.60, 0.67) |
| Risk perception at T1 | −0.11 (−0.14, −0.08) | −0.10 (−0.14, −0.07) | −0.11 (−0.15, −0.06) | −0.13 (−0.17, −0.09) |
| Cannabis use at T3 on | ||||
| Cannabis use at T2 | 0.72 (0.69, 0.74) | 0.67 (0.64, 0.70) | 0.61 (0.56, 0.67) | 0.70 (0.67, 0.73) |
| Risk perception at T2 | −0.10 (−0.12, −0.07) | −0.09 (−0.12, −0.06) | −0.10 (−0.14, −0.05) | −0.11 (−0.14, −0.07) |
Note: All p < .001 unless otherwise inidcaterd;
p<=.05,
p<.01,
p>.05.
Because T0 cannabis use was omitted from Model C, T1 use was regressed on demographic variables.
Because individuals without prior cannabis use experience may differ from ever-users with respect to the development of risk-perception, we also estimated the primary model on the sub-sample of individuals who had never used cannabis at T0 (omitting cannabis use at time 0 as a predictor, see Figure S1). We also estimated the model for those who had used cannabis prior to index. Coefficient estimates from these models are listed in the rightmost two columns of Table 3. There were few notable differences in the parameters of interest between these two populations. One possible exception is that for ever-users, risk perception at time 0 was a relatively weak predictor of use at time 1 (b=−.06, 95% CI: −0.10, −0.02). However, the overall picture was similar as for the other analyses: The use to risk perception pathways remained about twice as strong as the risk perception to use pathways and parameter estimates were similar to for the two subsamples.
To examine the relative contribution of each set of cross-lagged effects to the overall model fit, we examined a series of nested models, starting with the most basic model (A) that included auto autoregressive effects only, followed by a second model (B) which added risk perception at each time point predicting use at the subsequent time point. Model (C) comprised the baseline model (A) with the addition of use as a predictor of subsequent risk perception; Model (D) included both cross-lagged effects (i.e., the model presented in Figure 1). Model fit indices for each of the four models estimated are presented in Table 4 for the model using past-year cannabis use and in Supplementary Material (Table S2) for past-month cannabis use. Each model was a significantly better fit than the baseline model (A), as indicated by significant Satorra-Bentler scaled chi-square difference tests. Compared to all reduced models (Models A, B and C), the full model (D) had the lowest AIC and BIC values indicating the best parsimony-adjusted model fit. Notably, reduced model C had better fit than reduced model B, indicating that the a model including only risk perception to use pathways would be preferable to a model including only use to risk perception pathways. Similar analyses for binge drinking and cigarette smoking are provided in the Supplementary Material (Tables S3–S6 and Figures S1–S2). For the cigarette model, path coefficients were generally weaker, and risk perception to smoking pathways were not significant at the follow-up time points. For binge drinking, the two types of reciprocal associations (risk perception to binge drinking and vice-versa) were approximately equal in magnitude.
Table 4.
Model fit comparison of nested path analysis models for past-year marijuana use and perceptions of risk from regular marijuana use
| AIC (difference from Model A) | BIC (difference from Model A) | Log Likelihood | Scaling correction factor | Number of parameters | Test Statistic (Td) a | df a | P value a | |
|---|---|---|---|---|---|---|---|---|
| Model A: Autoregressive effects only | 105,309 | 105,538 | −52,624 | 1.6858 | 31 | - | - | - |
| Model B: Model A and risk perception to use | 104,964 (−345) |
105,215 (−323) |
−52,448 | 1.6776 | 34 | 220.6 | 3 | <0.001 |
| Model C: Model A and use to risk perception | 104,146 (−1163) |
104,397 (−1141) |
−52,039 | 1.6909 | 34 | 670.5 | 3 | <0.001 |
| Model D: Full model | 103,910 (−1399) |
104,183 (−1355) |
−51,918 | 1.6806 | 37 | 853.5 | 6 | <0.001 |
Statistics from Satorra-Bentler scaled chi-square difference based on log-likelihood values (Each model compared to Model A)
Discussion
In this study, we explored the reciprocal associations between cannabis use and risk perception in a sample of emerging adults beginning in 12th grade and extending through 3 biannual follow-ups. We found statistically significant negative associations in both directions across all time points: Cannabis use predicted decreased likelihood of perceiving cannabis as risky at the next follow-up, while beliefs about cannabis being risky predicted decreased likelihood of cannabis use at the next time-point. Notably, the effect of use predicting subsequent risk perception was found to be twice as strong as the effect of risk perception predicting use; this observation held even when the sample was restricted to those who had never used cannabis at baseline. For binge drinking, associations were approximately equal in both directions. For cigarettes use the associations were weaker overall but most consistently statistically significant in the use to risk perception paths (see Supplementary Material). To our knowledge, this is the first large-sample study to examine such reciprocal associations.
Our findings are consistent with other lines of research that suggest that prior experience with cannabis is a component of risk perception formation. Using a qualitative research approach, Wilkinson and colleagues interviewed a group of 31 veterans treated for substance use disorders (including cannabis use disorder) about their attitudes toward cannabis. Semi-structured interviews revealed that these participants emphasized the role of individual experience on the formation of cannabis risk perception (11). Other factors, such as information-based programs, medical professionals and the popular media seem to bear less influence on attitude formation. Most participants reported a positive experience of cannabis use, with limited behavioral effects and generally did not believe that cannabis was addicting. Furthermore, they were skeptical about other users having negative experiences with cannabis. Users who did experience negative effects as a result, such as interpersonal and social problems as well as poorer occupational performance, were more likely to perceive cannabis use as risky. In both groups, however, respondents believed that their experience shaped risk perception rather than vice-versa. Similarly, another study of current and ex-cannabis users used a qualitative inductive approach to find that users infer the particular risk-benefit ratio of the drug primarily from direct experience with using it, whereas prior to initiation, factors such as peer attitudes, prevention programs and media messages are relevant (10). These findings reinforce the idea that, at least among those who have initiated cannabis use, risk perception is substantially shaped by the quality of individual experiences with cannabis.
Perceptions of harm may be weighted heavily by immediate and/or short-term favorable effects of the drug, as opposed to slowly developing long-term harmful effects such as dependence (22,23). Cannabis users are likely aware of studies of expert-opinion comparing harms associated with cannabis use with those from other licit and illicit drugs. Results of these studies, which were widely publicized on the internet and in lay media, placed cannabis relatively low on the harm spectrum—much lower than alcohol, which was viewed as the most harmful drug across a spectrum of personal and social consequences (24,25). In light of these observations, it is important to consider whether prevention messages that solely emphasize the long-term harms associated with cannabis are sufficient to change the behavior of those who have initiated use and may be skeptical of such messages. Our results are consistent with a trajectory in cannabis which leads to lower perceptions of harm, potentially creating a disconnect between a user’s risk perception and information communicated in public health campaigns. Although there is still much to be learned about the formation of risk-perception, it seems that more research is needed on how receptive users at various stages of cannabis use to prevention messages that are primarily aimed altering users’ perception of cannabis-related harms
Our findings also confirm that higher risk-perception is associated with lower risk of subsequent use, and so interventional efforts in the form of awareness campaigns still constitute a reasonable strategy for primary prevention. But, as has been emphasized elsewhere, it is important that such programs provide balanced and up-to-date evidence-based material for risks associated with cannabis use, with accurate severities and probabilities of occurrence and without exaggerated risks (26).
The results of our study must be interpreted within the context of certain limitations. First, our cohort does not include adolescents younger than the age of 18. This limited our ability to examine the changes in risk perception and cannabis use as a function of age specific developmental stages. Therefore, the results shown here may not be generalizable to younger age groups. Second, the data from the MTF panel captures only general risk perception without accounting specifically for perceived risk on one’s self. The two variables sometimes may diverge when a user, while being well informed about the general risks attributed to the drug, does not appreciate these same risks onto oneself. Attrition between index and follow-up results in a non-random sample, however, results differed little across three missing data approaches. Finally, in order to estimate a full reciprocal effects model, it was necessary to use a single variable (frequency of cannabis use) to describe the association between cannabis use and risk perception. To accomplish this, we grouped never-users with those who did not use during a given survey period, and assumes a linear relationship between the various levels of that variable and risk perception. This reduction is partially supported by the robustness of our results when stratifying the sample by cannabis use status, but in reality it seems likely that the transition from never-user to ever-user might have more of an impact on risk perception than an escalation in frequency of use.
A strength of our study is that, by incorporating auto-regressive effects, our analyses focused on within-person covariation between risk-perception and cannabis use (27). However, unobserved time-varying confounding variables may still influence the reciprocal associations between the variables of interest.
Conclusion
Results from the present study indicate a bidirectional association between risk perception and future cannabis use and vice versa, with a stronger association between cannabis use and lower subsequent risk perception. The degree to which experience with cannabis use may influence risk perception should be considered when interpreting trends in risk perception. It may also be important for prevention scientists to consider the degree to which risk perception may be influenced by prior use rather than by public health messaging, and whether prevention messages that emphasize cannabis-related harms may have differential effects on those who have initiated use versus those who have not.
Supplementary Material
Acknowledgments
This work was funded by the National Institute of Health/National Institute on Drug Abuse, grants DA04041 (AA/RAG); DA042195 (RAG) DA32573; DA23668 (AA); DA036583 (LJB). The funding agency had no role in the design, conduct, collection, management, analysis or interpretation of data, or the preparation, review or approval of this paper. We are grateful to Monitoring the Future investigators for making the data available, to Timothy Perry (University of Michigan) for executing the analyses and, to Prof. Joshua Jackson and Dr. Sarah Hartz(Washington University) and Prof. Robert Krueger (University of Minnesota) for helpful advice.
Footnotes
Competing interest: NCS and MJK have no competing interests. AA has previously received peer –reviewed grant funding and reimbursement for travel from ABMRF/Foundation for Alcohol Research and National Institutes of Health. LJB is a consultant for the FDA Tobacco Products Scientific Advisory Committee, a member of the Advisory Board for the National Comprehensive Cancer Network Smoking Cessation Panel, and a member of the National Advisory Council on Drug Abuse. LJB is a member of the Speaker’s Bureau for Imedex. LJB is listed as an inventor on issued U.S. patent 8,080,371, “Markers for Addiction,” covering the use of certain SNPs in determining the diagnosis, prognosis, and treatment of addiction. RAG has received honoraria for peer-reviewed grant funding from National Institutes of Health.
References
- 1.Center for Behavioral Health Statistics and Quality. Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health. 2015. (HHS Publication No. SMA 15-4927, NSDUH Series H-50) [Google Scholar]
- 2.Kann L, Kinchen S, Shanklin SL, Flint KH, Kawkins J, Harris WA, et al. Youth risk behavior surveillance--United States, 2013. MMWR Suppl. 2014 Jun 13;63(4):1–168. [PubMed] [Google Scholar]
- 3.The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research [Internet] Washington, D.C: National Academies Press; 2017. Committee on the Health Effects of Marijuana: An Evidence Review and Research Agenda, Board on Population Health and Public Health Practice, Health and Medicine Division, National Academies of Sciences, Engineering, and Medicine. Available from: https://www.nap.edu/catalog/24625. Archived at http://www.webcitation.org/6tTuHHOIV on Sept 14, 2017. [PubMed] [Google Scholar]
- 4.Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States: 1991–1992 and 2001–2002. JAMA. 2004 May 5;291(17):2114–21. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- 5.Cohn A, Johnson A, Ehlke S, Villanti AC. Characterizing substance use and mental health profiles of cigar, blunt, and non-blunt marijuana users from the National Survey of Drug Use and Health. Drug Alcohol Depend. 2016 Mar;160:105–11. doi: 10.1016/j.drugalcdep.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 6.Lopez-Quintero C, Neumark Y. Effects of risk perception of marijuana use on marijuana use and intentions to use among adolescents in Bogotá, Colombia. Drug Alcohol Depend. 2010 Jun 1;109(1–3):65–72. doi: 10.1016/j.drugalcdep.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 7.Kilmer JR, Hunt SB, Lee CM, Neighbors C. Marijuana use, risk perception, and consequences: Is perceived risk congruent with reality? Addict Behav. 2007 Dec;32(12):3026–33. doi: 10.1016/j.addbeh.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 8.Nelson S. Key Anti-Pot Argument Torched? Teen Use Flat as Risk Perception Plunges. US News & World Report [Internet] 2015 Dec 16; Available from: https://www.usnews.com/news/articles/2015-12-16/key-anti-pot-argument-torched-teen-use-flat-as-risk-perception-plunges. Archived at http://www.webcitation.org/6tTuwtrz6 on Sept 14, 2017.
- 9.McBride N. A systematic review of school drug education. Health Educ Res. 2003 Dec 1;18(6):729–42. doi: 10.1093/her/cyf050. [DOI] [PubMed] [Google Scholar]
- 10.Shukla RK, Kelley MS. Investigating How Decisions to Use Marijuana Change Over Time. Subst Use Misuse. 2007 Jan;42(9):1401–25. doi: 10.1080/10826080701212485. [DOI] [PubMed] [Google Scholar]
- 11.Wilkinson ST, van Schalkwyk GI, Davidson L, D’Souza DC. The Formation of Marijuana Risk Perception in a Population of Substance Abusing Patients. Psychiatr Q. 2016 Mar;87(1):177–87. doi: 10.1007/s11126-015-9369-z. [DOI] [PubMed] [Google Scholar]
- 12.Grevenstein D, Nagy E, Kroeninger-Jungaberle H. Development of risk perception and substance use of tobacco, alcohol and cannabis among adolescents and emerging adults: evidence of directional influences. Subst Use Misuse. 2015;50(3):376–386. doi: 10.3109/10826084.2014.984847. [DOI] [PubMed] [Google Scholar]
- 13.Bachman JG, Johnston LD, O’Malley PM, Schulenberg JE, Miech RA. The Monitoring the Future project after four decades: Design and procedures. Ann Arbor, MI: Institute for Social Research, University of Michigan; 2015. p. 93. Report No.: (Occasional Paper No. 82) [Google Scholar]
- 14.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975–2010. Ann Arbor, MI: Institute for Social Research, University of Michigan; 2011. p. 744. [Google Scholar]
- 15.Newsom JT. Longitudinal structural equation modeling: A comprehensive introduction. New York: Routledge; 2015. [Google Scholar]
- 16.Akaike H. A new look at the statistical model identification. Autom Control IEEE Trans On. 1974;19(6):716–23. [Google Scholar]
- 17.Schwarz G. Estimating the dimension of a model. Ann Stat. 1978;6(2):461–4. [Google Scholar]
- 18.Dziak JJ, Coffman DL, Lanza ST, Li R. Sensitivity and specificity of information criteria. State College, PA: The Methodology Center, The Pennsylvania State University; 2012. (Technical Report Series). Report No.: #12-119. [Google Scholar]
- 19.Satorra A, Bentler PM. Ensuring Positiveness of the Scaled Difference Chi-square Test Statistic. Psychometrika. 2010 Jun;75(2):243–8. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muthén L, Muthén B. Mplus User’s Guide: Seventh Edition. Los Angeles, CA: Muthén & Muthén; 1998. [Google Scholar]
- 21.Diggle P, Kenward MG. Informative Drop-Out in Longitudinal Data Analysis. Appl Stat. 1994;43(1):49. [Google Scholar]
- 22.Sussman S, Earleywine M, Wills T, Cody C, Biglan T, Dent CW, et al. The Motivation, Skills, and Decision-Making Model of “Drug Abuse” Prevention. Subst Use Misuse. 2004 Jan;39(10–12):1971–2016. doi: 10.1081/ja-200034769. [DOI] [PubMed] [Google Scholar]
- 23.Coomber R, Oliver M, Morris C. Using Cannabis Therapeutically in the UK: A Qualitative Analysis. J Drug Issues. 2003 Apr;33(2):325–56. [Google Scholar]
- 24.Nutt DJ, King LA, Phillips LD. Drug harms in the UK: a multicriteria decision analysis. The Lancet. 2010;376(9752):1558–65. doi: 10.1016/S0140-6736(10)61462-6. [DOI] [PubMed] [Google Scholar]
- 25.Nutt D, King LA, Saulsbury W, Blakemore C. Development of a rational scale to assess the harm of drugs of potential misuse. The Lancet. 2007 Mar;369(9566):1047–53. doi: 10.1016/S0140-6736(07)60464-4. [DOI] [PubMed] [Google Scholar]
- 26.Cermak TL, Banys P. Prevention of Youthful Marijuana Use. J Psychoactive Drugs. 2016 Jan;48(1):21–3. doi: 10.1080/02791072.2015.1117689. [DOI] [PubMed] [Google Scholar]
- 27.Allison PD. Quantitative applications in the social sciences, 07-160. Los Angeles: SAGE publications; 2009. Fixed effects regression models. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.