Abstract
Study Objective
To assess the effects of the Seventeen Days interactive video on young women’s perceived self-efficacy for using condoms 6 months after being offered the intervention, relative to a control.
Design
Multisite randomized controlled trial.
Setting
Twenty participating health clinics and county health departments in Ohio, Pennsylvania, and West Virginia.
Participants
Sexually active female adolescents ages 14 to 19 years.
Interventions
Seventeen Days (treatment intervention; sex education) vs Driving Skills for Life (control intervention; driving education).
Main Outcome Measures
Perceived self-efficacy for condom use.
Results
Participants in the Seventeen Days group reported higher perceived condom acquisition self-efficacy after 6 months than those in the driving group. This finding held after controlling for baseline self-efficacy scores and other covariates.
Conclusion
The Seventeen Days program shows promise to improve perceived self-efficacy to acquire condoms among sexually active female adolescents—an important precursor to behavior change.
Keywords: Pregnancy prevention, Self-efficacy, Condoms
Introduction
Although teen birth rates in the United States have decreased 61% since 1991 and 8% since 2014,1,2 they remain the highest among industrialized countries.3,4 Nearly 750,000 teen pregnancies occur annually, most unintended (mistimed, unplanned, or unwanted).1,4 A review of relevant literature reveals how challenging it is to intervene successfully in adolescent sexual behavior with only a few dozen programs showing promise for preventing teen pregnancy.5
The Teen Pregnancy Prevention (TPP) Evidence Review commissioned by the US Department of Health and Human Services (DHHS) in 2009 with findings later updated in 2012 reviewed 452 program evaluations conducted between 1989 and 2011 on programs attempting to affect teen pregnancy, sexually transmitted infections (STIs), or other associated sexual risk behaviors.5 The review identified just 31 programs that had shown evidence of favorable effect with a moderate or high-quality evaluation design. Only 5 showed a reduction in STIs.
In an effort to increase evidence-based teen pregnancy prevention programming, in 2010 the US DHHS began funding evaluations of large-scale replications of programs that have shown promise in research trials as part of the Teen Pregnancy Prevention Program. The failure of past replications has prompted pessimism about the viability of all behavioral interventions.6,7 Replication of an intervention in “the real world” with fidelity is a challenge, especially when it requires trained, motivated personnel—a common feature of most interventions with success in clinical trials.5 In fact, nearly all of the successful interventions identified by the review deliver their content through group discussion sessions that are facilitated by instructors or other trained personnel. Such programs are expensive and are vulnerable to reduced fidelity as they scale up because of less closely supervised personnel and implementation. Replications often fail to reproduce promising results because of poor fidelity, with many of the problems arising from low adherence and inconsistent delivery by personnel.8–10
One way to improve fidelity is to standardize as much of an intervention as possible. High-quality, user-friendly media technology now allows presentation of interactive material consistently to wide audiences with low distribution costs after the initial investment has been made in their creation.11,12 Computer-based HIV prevention programs have been reported to have efficacy similar to in-person interventions.13,14 Even before digital video made accessibility and interactivity trivial, video interventions were reported to be particularly effective in changing knowledge and attitudes about sexual risk15 and other precursors to behavior change.16 More generally, video has been reported to be effective in changing a variety of behaviors, especially ones requiring modeling of new behavior.17
In the domain of sexual health, interventions incorporating video have been reported to increase intentions to use female condoms,18 proximal behaviors such as condom coupon redemption, and HIV testing,19,20 longer-term behaviors including self-reported condom use several months after initial intervention,21–23 and clinical outcomes.24,25 However, even these interventions typically incorporate video as part of facilitator-led group sessions, leaving them vulnerable to the challenges of cost and fidelity.26
One of the 31 programs identified by the TPP Evidence Review for its promising findings was our 1990s video-based intervention, “What Could You Do?” (WCYD). WCYD was designed for use on a self-contained platform to promote ease and fidelity in field implementation. It focused on increasing young women’s self-protective decision-making about sex to reduce STIs. In a randomized controlled trial (RCT), participants assigned to view the video reported increased abstinence and reduced condom failures and STI diagnoses post-intervention compared with participants in 2 comparison groups—one that received a print version of the intervention and one that received equivalent topics from printed materials.27 The video group outperformed the equivalent print group, suggesting a unique effect of video as the medium for delivery.
WCYD targeted STI prevention by focusing on behaviors that are also effective for preventing pregnancy. After identification by the TPP Evidence Review as promising for teen pregnancy prevention, WCYD was funded for update and large-scale evaluation in 2010 by the Office of Adolescent Health. The characters and production value were updated, the content was expanded to include pregnancy prevention material, and the program underwent medical accuracy review in 2011 to create a new interactive video, “Seventeen Days.”
This article reports the results of an individual-level RCT across multiple clinical sites evaluating the effect of Seventeen Days on perceived condom use self-efficacy. We hypothesized that the experimental intervention, Seventeen Days, would increase perceived condom use self-efficacy 6 months post-intervention relative to a control, the interactive video intervention. “Driving Skills for Life.”
Materials and Methods
Participants
The sample included female adolescents at high risk for pregnancy—primarily patients from 20 urban, suburban, and rural health clinics in Ohio, Pennsylvania, and West Virginia between June 2012 and December 2014. Sites included hospital-affiliated adolescent health clinics, county health clinics, and nonprofit family planning clinics. Participants met 5 eligibility criteria: (1) female sex; (2) age 14–19 years; (3) reported sexual activity (participant-defined) in the previous 6 months; (4) not married; and (5) not currently pregnant.
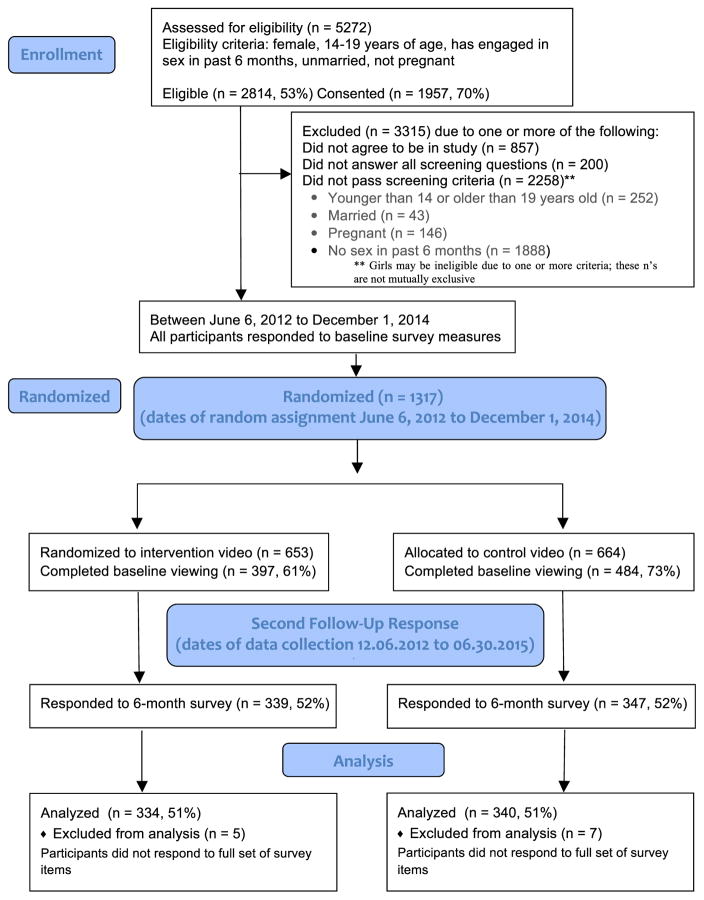
Power calculations revealed that we would require 1628 participants for 90% power to detect a difference in our behavioral outcome measure. Of the 5272 young women screened, 2814 were eligible for the study, of whom 1957 consented to participate and 1317 completed the baseline measures and were randomized to a group. There was an even distribution (P = .983), with 653 in the Seventeen Days group and 664 in the driving group. Despite efforts to maximize participant enrollment, fewer clients than expected were available and eligible to participate in the study. Additionally, attrition rates were higher than anticipated, but within DHHS standards. Recruitment was extended longer than originally planned, but was halted to accommodate all necessary follow-up windows before the end of the funding period. This analysis reports on results from the 674 participants who completed the 6-month outcome survey. The Consolidated Standards of Reporting Trials diagram in Fig. 1 shows recruitment and follow-up information.
Fig. 1.
Consolidated Standards of Reporting Trials flow diagram.
Research Design
The research design is a multicenter individual RCT (Clinical Trials NCT02049710). Institutional review board approval was obtained from Carnegie Mellon University, West Virginia University, University of Pittsburgh, and Nationwide Children’s Hospital of Columbus, Ohio. Consent was obtained for participation, including assent from minors and consent by their parents. A waiver of parental consent was obtained for minors who had no parent or guardian accompanying them at the clinic.
Immediately after a baseline survey was completed, an automated computer program provided the individual randomization of the participant to group, stratified according to clinic site. Participants were then routed to the appropriate video. Study personnel were blind to participants’ assignment.28 Because of a programming glitch in an early version of the evaluation software, 3 participants in the sample were inadvertently rerandomized 3 months after baseline and shown a portion of the video from the alternate group. For analysis, all participants were retained in their originally assigned group.
Data Collection Procedures
Upon enrollment, all participants in both groups were given access to the study site at teenvideostudy.com, where they completed all survey materials via Qualtrics online surveys and watched their assigned video. Participants were provided with an electronic tablet in clinic and were able to complete surveys and watch videos anywhere with Internet access by logging into the site. (Unfortunately, videos would not play on iPhones or iPads because of the site’s use of the Adobe Flash Player.)
Data were collected at baseline and 3 and 6 months after randomization. Surveys required 30–40 minutes to complete. Participants were paid $25 to complete the baseline survey and watch the “core dosage” of their assigned video—the portion of the video covering the key content for instruction (see Interventions). They received $25 for completing the 3-month and $25 for the 6-month follow-up measures, plus a $20 bonus for completing all measures. Follow-up measures could be completed online from anywhere, and participant reminders included a link for easy, direct access. Reminders were sent when milestones were approaching, due, and overdue, starting with the participant’s primary communication method, which was overwhelmingly text messaging. If the participant did not respond, additional reminders were sent by e-mail, voice call, postal mail, and eventually certified letter.
Measures
Survey items included questions on participants’ demographic characteristics, self-reported behavior, and perceived self-efficacy about condom use, knowledge about sex, and correct use of condoms. Data on measures were collected at baseline and again 6 months after randomization.
Self-Efficacy for Condom Use Scale
This analysis focused on participant responses to 7 questions pertaining to condom use self-efficacy.29 Responses ranged from 1 to 5, with higher numbers indicating greater self-efficacy. Factor analyses (see Appendix A) revealed 2 factors: condom negotiation and condom acquisition, each containing 3 items, with 1 item not loading onto either factor (Table 1). Subscales were created by adding the item scores, creating ranges from 3 (lowest self-efficacy) to 15 (highest self-efficacy).
Table 1.
Questions Assessing Self-efficacy for Condom Use
| Indicate How Sure You are that You Would be Able to Perform Each of the Following: | Mean (SD) at Baseline | Factor Loading Negotiation | Factor Loading Acquisition |
|---|---|---|---|
| Item not loading onto either factor | |||
| 1. Use a condom correctly | 4.52 (0.89) | 0.303 | 0.424 |
| Negotiation of condom use (Cronbach α= 0.87) | |||
| 2. Use a condom every time you have sexual intercourse | 3.82 (1.31) | 0.773 | |
| 3. Insist on using a condom during sex, even if your partner does not want to use a condom | 4.08 (1.24) | 0.899 | |
| 4. Refuse to have sex if your partner will not use a condom | 3.83 (1.35) | 0.791 | |
| Acquisition of condoms Cronbach α = 0.72) | |||
| 5. Get the money needed to buy condoms | 4.24 (1.16) | 0.737 | |
| 6. Walk into a store and buy condoms | 4.12 (1.28) | 0.780 | |
| 7. Find a place to get condoms for free | 3.89 (1.48) | 0.525 | |
n = 674. Items answered on a 5-point scale from 1 (“not at all sure”) to 5 (“very sure”).
From overall models that significantly predicted both self-efficacy subscales at 6 months—F6,667 = 34.43, P < .001, for negotiation and F6,666 = 44.04, P < .001, for condom acquisition—we found that scores were relatively stable from baseline to 6 months, with baseline values significantly predicting 6-month values in the regression for negotiation (b = 0.487, P < .001), as well as acquisition, (b = 0.458, P < .001). Acquisition scores tended to increase with each year of participant age (b = 0.297, P < .001), but negotiation scores did not (b = 0.130, P = .111). Means of both subscales were high at baseline, with 371 of 674 (55%) of participants at ceiling for at least 1 subscale (36%—or 134 out of 371—for just one and 19%—or 70 out of 371— for both subscales). However, there was still sufficient variability to predict behavior; a logistic regression revealed that self-efficacy of condom negotiation was a significant positive predictor of self-reported baseline condom use (β = 0.317, P < .001) but self-efficacy of condom acquisition was not (β = −0.052, P = .153).
Interventions
The Seventeen Days as well as Driving Skills for Life interventions were stand-alone interactive videos that were self-administered via electronic tablet and tracked viewer choices and content exposure. Participants could continue watching their intervention online outside the clinic.
The core program dosage of both interventions lasted approximately 35 minutes and could be watched in multiple sessions. Participants were then given additional content and encouraged monthly to watch more material online. The core dosage was required before additional material as well as for receiving compensation (as an incentive for completion). Unfortunately, in both groups some participants did not complete the baseline dosage (Fig. 1). Consistent with our intent-to-treat approach, all who completed the 6-month survey were included in analysis, irrespective of whether they had completed the core dosage.
Seventeen Days Intervention
Seventeen Days retains the original WCYD intervention’s key benefits, including adherence to research findings with the target population,27 use of narrative for risk-reduction strategies, and realistic decision-making,30 and the high fidelity of video delivery.31 Using high-definition Web streaming, it features a more ethnically and racially diverse cast and adds content on birth control and the risk of unintended pregnancy. Like the original, it retains the focus on correct, consistent condom use.
The intervention was developed through our formative research using the mental models methodology—a behavioral decision science approach—to investigate adolescent girls’ decisions about sex and relationships.27,30–38 In a series of in-depth mental models interviews, we identified aspects of adolescents’ sexual decisions that could lead to high-risk behavior or undermine attempts to reduce risk. On the basis of the findings from that research, the curriculum uses well established psychological tools, including behavioral modeling,39 cognitive rehearsal,40 and cognitive bias mitigation41 to improve sexual decision-making and reduce risky behavior as described in more detail below.
The primary mechanism by which Seventeen Days aims to reduce risky sexual behaviors is by encouraging young women to think about their decisions more systematically and acquire the necessary psychosocial tools to carry out their planned decisions. One of these psychosocial tools is perceived self-efficacy: the belief in one’s capacity to execute desired behaviors.42,43 Self-efficacy for condom use is a reliable predictor of actual condom use (with a medium effect size documented in meta-analysis44), suggesting that improving self-efficacy should reduce adolescents’ risk for unintended pregnancies and STIs.
Seventeen Days focuses on improving viewers’ condom use self-efficacy, including young women’s ability to acquire condoms, negotiate their use with a partner, and apply them correctly and consistently. Improvements in self-efficacy should lead to immediate increased condom use (and potential reinforcement through successful condom use) thereby reducing teen pregnancy and STIs in the long term. The intervention uses 2 major techniques to improve condom use self-efficacy:
Prompting viewers to engage in cognitive rehearsal while following vignettes of female characters in which they negotiate condom use; and
Increasing viewers’ knowledge about condom acquisition, correct use, and effectiveness using a condom demonstration scene.
Seventeen Days uses a “choose your own adventure” format in which viewers select from different stories as they encounter decisions that arise in potential sexual relationships. When a character faces a decision, the story pauses and the video presents a menu offering 3 paths the character could pursue with 2 of the paths modeling strategies for reducing risk behavior. Each option is presented as a video showing a different response and viewers choose how the story continues. Although these brief clips do not show the choice playing out to conclusion, it is clear from the character’s behavior whether she is encouraging or halting progression of the sexual situation.
When the viewer chooses a story path leading to lower risk, she is invited to engage in cognitive rehearsal—to mentally practice how she would respond in similar situations.39,45 This concept is demonstrated early in the film so viewers know what is being asked with questions like, “What could you do if you didn’t want to go off alone with a guy? Think about it, and practice it in your head.” The intervention also includes a condom demonstration scene and “mini-documentaries”—informational segments to correct misperceptions and increase knowledge about anatomy, contraception, visiting a gynecologist, STIs, and relative behavioral risks.
The core dosage of Seventeen Days consists of: (1) an introduction to the intervention’s core components of empowerment to make choices in sexual situations and cognitive rehearsal of safe choices; (2) a step-by-step demonstration of correct condom usage to increase condom use self-efficacy with background information about how and why condoms reduce risk; and (3) choice of one vignette on sexual negotiation that reinforces the key concept of empowered choices through cognitive rehearsal.
In addition to the core dosage, more than 2 hours of additional interactive material take the form of character vignettes and 4 mini-documentaries: (1) “Know Your Body,” covering female reproductive anatomy and function; (2) “I Got Birth Control and So Can You,” depicting experiences of young women obtaining birth control and an interactive feature on contraceptive methods; (3) “Going to the Gynecologist,” modeling interactions with a health care provider, including getting long-acting reversible contraception and requesting further services; and (4) “Watch Out for STIs,” featuring information explaining the risks of sexual behaviors, differences between viral and bacterial infections, the importance of regular screenings, and health consequences and treatment options for various STIs. (See the diagram in Appendix Fig. 1, screenshots in Appendix Fig. 2, or www.seventeendays.org for excerpts.).
Counterfactual
The control intervention, Driving Skills for Life, aimed to reduce vehicle crashes. We chose this focus because of its high incidence and morbidity in the adolescent population and negligible applicability to sexual behavior. It was a stand-alone interactive video produced by and used with permission from Ford Motor Company. Online delivery was identical to the intervention group.
The core dosage was matched in length to that of the experimental video—approximately 35 minutes. As with Seventeen Days, the Driving Skills for Life intervention could span multiple viewings. Although the optional content in this intervention included interactivity, the core dosage was a video that would play straight through if the participant did not close their browser. Thus, participants who started in this group and left the video running were inadvertently counted as having completed the core dosage.
In addition to the core dosage, Driving Skills for Life contains more than an hour’s worth of additional interactive material, including hazard recognition, car handling, speed management, space management, and distracted and impaired driving, including texting while driving. It also includes interactive games (for example, merging onto a busy highway). More information and excerpts of the intervention can be viewed at the drivingskillsforlife.com Web site.
Statistical Analyses
Analyses were conducted with SPSS statistical software (version 23; IBM Corp., Armonk, New York). For perceptions of condom negotiation and acquisition self-efficacy, 2 repeated measures analyses of covariance compared self-efficacy scores at baseline and 6 months between those in the Seventeen Days group and those in the driving group, controlling for covariates, which included age, race, and safer sexual behavior at baseline (defined as always using condoms correctly, or no sexual activity at all) Because of the previously mentioned missing values, we used the overall sample mean in place of missing values (because there were not sufficient other meaningful data to impute individual values) and also performed the analyses omitting the safer sex behavioral covariate. The mean value of this baseline covariate was identical for the 2 groups. Results of the 2 analyses were extremely similar; the results reported in this article exclude the safer sex behavioral covariate. The analysis reported in Results was conducted on the 674 participants who completed the 6-month outcome survey. See Fig. 1 for recruitment and follow-up.
Results
Baseline Equivalence
As reported in Table 2 for the final analytic sample, participants in the Seventeen Days and driving groups were not significantly different on demographic or behavioral characteristics at baseline (all P > .20), but those assigned to the Seventeen Days group scored slightly higher on their baseline measure of condom negotiation self-efficacy beliefs.
Table 2.
Baseline Demographic and Clinical Characteristics for Each Group
| Seventeen Days Intervention (n = 334)* | Driving Skills for Life Control (n = 340)* | P | |
|---|---|---|---|
| Race† | |||
| Black/African American, not Hispanic | 32.6% | 32.1% | .808 |
| White, no other categories checked | 52.7% | 54.1% | .960 |
| Hispanic | 5.7% | 5.0% | .691 |
| Other race or more than 1 category checked, not Hispanic | 9.0% | ||
| Mean age, years | 17.18 | 17.25 | .653 |
| Ever been pregnant | |||
| Yes | 9.9% | 12.1% | .366 |
| Self-efficacy for condom use at baseline | |||
| Condom acquisition (scaled from 3 to 15) | 12.23 (SE, 0.12) | 12.19 (SE, 0.32) | .801 |
| Condom negotiation (scaled from 3 to 15) | 11.79 (SE, 0.14) | 11.45 (SE, 0.14) | .084 |
SE, standard error.
Group n is identical across all variables other than safer sex, as noted.
Participants were permitted to check more than one racial category. This table specifies mutually exclusive categories.
Dosage
In the Seventeen Days group, 61% (or 204 of 334) of participants completed the core dosage, and 37% (or 124 of 334) watched additional video material beyond the core dosage—primarily watching additional character narratives. Of participants assigned to the control intervention, 73% (or 248 of 340) completed the core dosage and 38% (or 129 of 340) watched additional video material beyond the core dosage.
Hypothesis Testing
For condom negotiation self-efficacy beliefs, there was an overall main effect of group across both time points (baseline, 6 months; F1,668 = 8.40, P = .004), reflecting scores that started out higher among those assigned to Seventeen Days and stayed higher. However, there was no interaction with the repeated measure (F1,668 = 0.02, P = .881), indicating no relative improvement according to group.
In contrast, for condom acquisition self-efficacy beliefs an interaction emerged between treatment group and the repeated measure (F1,667 = 5.06, P = .025, partial η2 = .008), revealing that participants in the Seventeen Days group reported a greater gain at 6 months compared with those in the driving group, after controlling for age and race (Fig. 2). These results held when demographic characteristics were excluding from the model (F1,671 = 4.93, P = .027, partial η2 = 0.007).
Fig. 2.
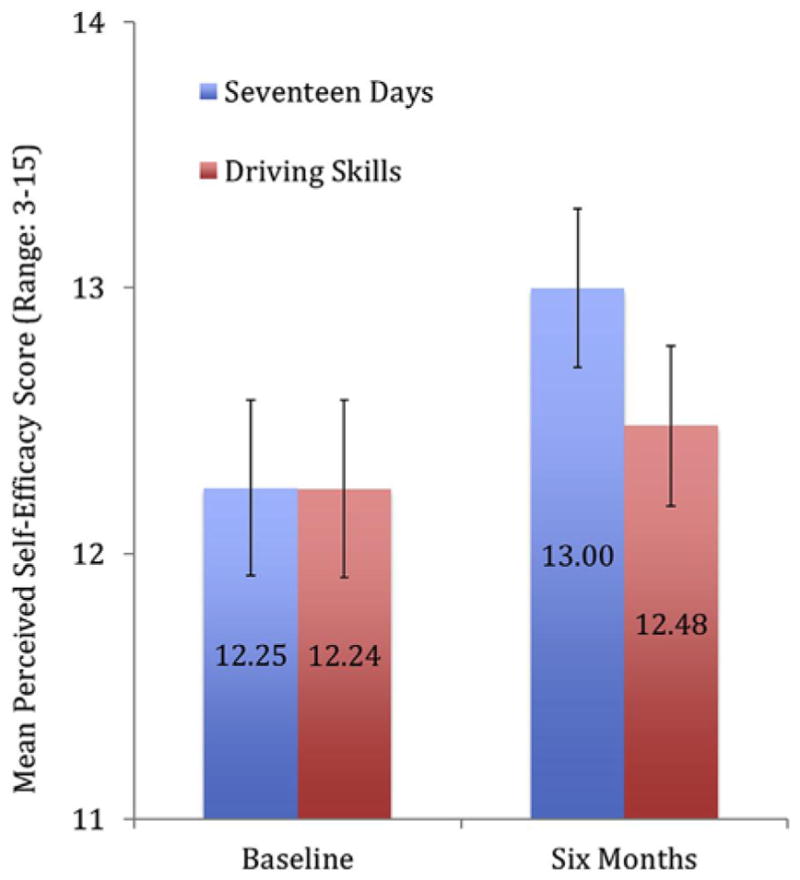
Improvement in perceptions of self-efficacy for condom acquisition after randomization to Seventeen Days video intervention. Estimated marginal means are plotted, controlling for age and race. Error bars represent each mean’s 95% confidence interval. Self-efficacy scores increased more over 6 months after randomization for the Seventeen Days group relative to the Driving Skills for Life control group (P = .025).
Discussion
The results of this rigorous multisite RCT indicate that the interactive video behavioral intervention Seventeen Days has a small but positive effect on perceived self-efficacy for condom acquisition, but no effect on corresponding beliefs about condom negotiation. Although the effect is small, it is an important contribution to teen pregnancy and STI prevention research. Many existing sexual health interventions are not evaluated, and many that are evaluated fail to show improvements in psychological mediators of behavior change. This report adds to our existing knowledge by presenting the effects of a stand-alone video intervention on a psychological outcome that should affect behavior change. Unplanned pregnancy and STIs have negative consequences on the social, economic, physical, and emotional well-being of American adolescents. A behavioral intervention that could decrease unplanned pregnancies and STIs by altering relationships and sexual decisions might be an important step in the direction of winning these public health battles. The Seventeen Days intervention shows promise in increasing teenagers’ perceived condom use self-efficacy, an important precursor to these behavior changes.
This study includes some important limitations. Because this intervention was a pregnancy prevention strategy, we recruited participants at risk for pregnancy (ie, female adolescents with recent sexual activity) and presented content targeted at heterosexual sexual behavior. Therefore, these findings are, by design, not generalizable to adolescent women having sex only with other women or to male adolescents. Furthermore, high overall attrition rates before as well as after randomization might limit generalizability of the findings. We took many steps throughout the study to reduce attrition, including:
Progressive reminders of study appointments at designated intervals using participants’ preferred contact method (text message reminders were the overwhelming preference);
Gathering updated contact information at study appointments to use when contacting participants with future study reminders;
Allowing participants to access the intervention material and survey questions at a time and from a location of their convenience;
Offering additional incentives to girls who completed study appointments (eg, “bonus” gift cards for completing all appointments; regular raffle drawings using a lottery system in which a small number of participants won prizes such as a $300 Visa gift card or a new Samsung Galaxy tablet for completing all study appointments);
Equipping study recruiters with gift cards while they were at clinic sites so they could provide incentives immediately to girls who completed baseline or study follow-up appointments in person;
Researching and suggesting addresses of local community sites with free computer or Internet access for girls with limited access; and
Scheduling study staff to meet girls at clinics sites so they could complete study appointments using our equipment and internet access.
Allowing participants to complete their follow-up surveys online from their own homes was originally conceived as a strategy to make compliance easier and, thus, boost retention rates. This design introduced a number of factors that might have contributed to low survey completion rates, however, especially because of teens’ increasing reliance on cell phones and the unexpectedly high rate at which their cell phone numbers change. This made it difficult to keep in touch with participants and remind them about their follow-up surveys. The teens at highest risk for negative sexual outcomes might be the hardest to successfully follow-up with for long-term monitoring. In addition, not having a specific appointment time allowed participants to put off their participation repeatedly, eventually leading many of them to miss the window of opportunity. Future research should consider the balance between allowing participants flexibility to complete the intervention and evaluation measures at their own convenience vs maintaining accountability for study completion. More intensive involvement (or relationship-building) is needed by program or clinic staff to ensure completion of intervention material and follow-up surveys.
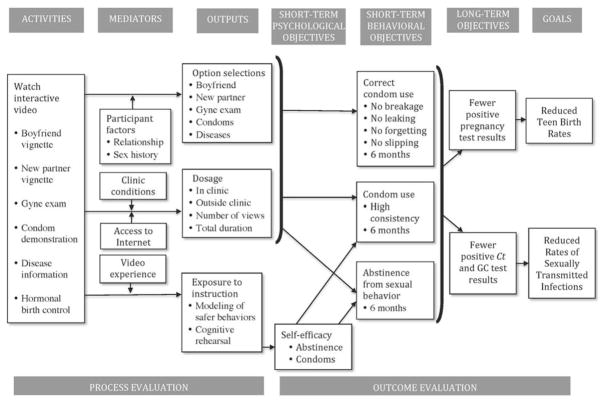
Despite challenges and limitations, the results suggest that the Seventeen Days intervention, as implemented in a wide variety of clinic settings, can improve an important psychological mediator to risky sexual behavior. Condom acquisition is highlighted early in the intervention materials, with condom negotiation following in later sections and increasing with additional, optional dosage. Because of the low dosage experienced by this sample overall, it is possible that increasing exposure to the material would give the intervention a better chance at increasing self-efficacy for condom negotiation. Self-efficacy is an important precursor to behavior change and a key theoretical component of the logic model that underlies the program (Appendix Fig. 3). These changes in self-efficacy beliefs are an encouraging indication of the potential of the video intervention to affect sexual decision-making in this population.
Acknowledgments
This research was supported by grant 1TP1AH0000400 from the Office of Adolescent Health.
We are greatly indebted to Nicole Bennett, Jean Knab, and Amy Margolis for their guidance on this project and to Mousumi Banikya-Leaseburg, Ashley Baskin, Amber Brown, Cory Campbell, Laura Clark, Karin Daniels, Alexandra De-Mand, Rachel Edelman, Robin Exline, Marz Holtzworth, Reesha Jackson, Mandy Lanyon, Shelly Layman, Laura Oliver, Mallory Rowell, Ore Shenbanjo, Catherine Spence, Molly Spurlock, Brenda Sullivan, Nancy Sutter, and Vanessa Veltre for their assistance with recruiting and managing the study.
This study is registered at ClinicalTrials.gov: NCT 02049710.
Appendix A. Factor Analysis Results
Separate parallel analysis and exploratory factor analysis were conducted on baseline and 6-month self-efficacy data to determine if the results are consistent across both time points. In general, the results are comparable. Parallel analysis results indicate that the optimal solution is a 2-factor solution. In exploratory factor analysis, using maximum likelihood extraction and varimax rotation, we found 2 factors (eigenvalues = 2.99 and 1.54, accounting for 65% of the total variance for the baseline measures). Items 2, 3, and 4 loaded on 1 factor whereas items 5,6, and 7 loaded on the second factor. These 2 factors are referred to as “condom negotiation” and “condom acquisition,” respectively. Item 1 on the self-efficacy scale had fairly low loadings on both factors at the baseline, but loaded substantially (0.497) on the negotiation factor at 6 months. It had substantial loading (0.497) on the condom correct use factor at 6 months. For the sake of consistency, it is not included in either subscale.
Appendix Fig. 1.
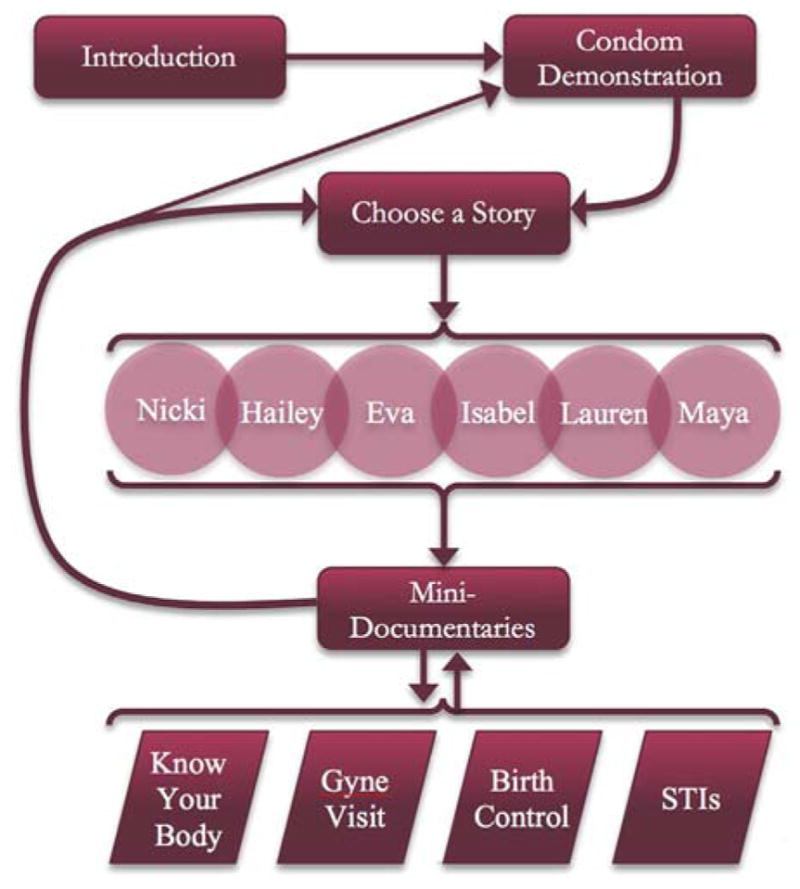
Site map for content of Seventeen Days intervention.
Appendix Fig. 2.
Images from the Seventeen Days intervention. (A) Screenshot from behavioral modeling preceding interactive choice. (B) Screenshot from he cognitive rehearsal animation. (C) Screenshot from modeling of correct condom usage.
Appendix Fig. 3.
Logic model for Seventeen Days. Ct, Chlamydia; GC, Gonorrhea.
Footnotes
The authors indicate no conflicts of interest.
References
- 1.Kost K, Henshaw S. U.S. Teenage Pregnancies, Births, and Abortions 2010: National and State Trends by Age, Race, and Ethnicity. Washington, DC: Guttmacher Institute; 2014. [Google Scholar]
- 2.Martin JA, Hamilton BE, Osterman MJ, et al. Births: final data for 2015. Natl Vital Stat Rep. 2017;64:1. [PubMed] [Google Scholar]
- 3.Sedgh G, Finer LB, Bankole A, et al. Adolescent pregnancy, birth, and abortion rates across countries: levels and recent trends. J Adolesc Health. 2015;56:223. doi: 10.1016/j.jadohealth.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84:478. doi: 10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goesling B, Colman S, Trenholm C, et al. Programs to reduce teen pregnancy, sexually transmitted infections, and associated sexual risk behaviors: a systematic review. J Adolesc Health. 2014;54:499. doi: 10.1016/j.jadohealth.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 6.Aral SO. Utility and delivery of behavioral interventions to prevent sexually transmitted infections. Sex Transm Infect. 2011;87(suppl 2):ii31. doi: 10.1136/sextrans-2011-050181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aral SO, Blanchard J, Lipshutz J. STD/HIV prevention intervention: efficacy, effectiveness and population impact. Sex Transm Infect. 2008;84(suppl 2):ii1. doi: 10.1136/sti.2008.033613. [DOI] [PubMed] [Google Scholar]
- 8.Durlak JA, DuPre EP. Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Community Psychol. 2008;41:327. doi: 10.1007/s10464-008-9165-0. [DOI] [PubMed] [Google Scholar]
- 9.Carroll C, Patterson M, Wood S, et al. A conceptual framework for implementation fidelity. Implement Sci. 2007;2:40. doi: 10.1186/1748-5908-2-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Valdiserri RO. Accomplishments in HIV prevention science: implications for stemming the epidemic. Nat Med. 2003;9:881. doi: 10.1038/nm0703-881. [DOI] [PubMed] [Google Scholar]
- 11.Delgado HM, Austin SB. Can media promote responsible sexual behaviors among adolescents and young adults? Curr Opin Pediatr. 2007;19:405. doi: 10.1097/MOP.0b013e32823ed008. [DOI] [PubMed] [Google Scholar]
- 12.Noar SM. Computer technology-based interventions in HIV prevention: state of the evidence and future directions for research. AIDS Care. 2011;23:525. doi: 10.1080/09540121.2010.516349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bailey JV, Murray E, Rait G, et al. Computer-based interventions for sexual health promotion: systematic review and meta-analyses. Int J STD AIDS. 2012;23:408. doi: 10.1258/ijsa.2011.011221. [DOI] [PubMed] [Google Scholar]
- 14.Noar SM, Black HG, Pierce LB. Efficacy of computer technology-based HlV prevention interventions: a meta-analysis. AIDS. 2009;23:107. doi: 10.1097/QAD.0b013e32831c5500. [DOI] [PubMed] [Google Scholar]
- 15.Healton CG, Messeri P. The effect of video interventions on improving knowledge and treatment compliance in the sexually transmitted disease clinic setting. Sex Transm Dis. 1993;20:70. doi: 10.1097/00007435-199303000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Kalichman SC. HIV-AIDS prevention videotapes: a review of empirical findings. J Prim Prev. 1996;17:259. doi: 10.1007/BF02248795. [DOI] [PubMed] [Google Scholar]
- 17.Tuong W, Larsen ER, Armstrong AW. Videos to influence: a systematic review of effectiveness of video-based education in modifying health behaviors. J Behav Med. 2014;37:218. doi: 10.1007/s10865-012-9480-7. [DOI] [PubMed] [Google Scholar]
- 18.Zimmers E, Privette G, Lowe RH, et al. Increasing use of the female condom through video instruction. Percept Mot Skills. 1999;88:1071. doi: 10.2466/pms.1999.88.3c.1071. [DOI] [PubMed] [Google Scholar]
- 19.O’Donnell LN, Doval AS, Duran R, et al. Video-based sexually transmitted disease patient education: its impact on condom acquisition. Am J Public Health. 1995;85:817. doi: 10.2105/ajph.85.6.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Solomon MZ, DeJong W. Preventing AIDS and other STDs through condom promotion: a patient education intervention. Am J Public Health. 1989;79:453. doi: 10.2105/ajph.79.4.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kalichman SC, Cherry C, Browne-Sperling F. Effectiveness of a video-based motivational skills-building HIV risk-reduction intervention for inner-city African American men. J Consult Clin Psychol. 1999;67:959. doi: 10.1037//0022-006x.67.6.959. [DOI] [PubMed] [Google Scholar]
- 22.Sanderson CA, Yopyk DJ. Improving condom use intentions and behavior by changing perceived partner norms: an evaluation of condom promotion videos for college students. Health Psychol. 2007;26:481. doi: 10.1037/0278-6133.26.4.481. [DOI] [PubMed] [Google Scholar]
- 23.Wingood GM, Card JJ, Er D, et al. Preliminary efficacy of a computer-based HIV intervention for African American women. Psychol Health. 2011;26:223. doi: 10.1080/08870446.2011.531576. [DOI] [PubMed] [Google Scholar]
- 24.O’Donnell CR, O’Donnell L, San Doval A, et al. Reductions in STD infections subsequent to an STD clinic visit using video-based patient education to supplement provider interactions. Sex Transm Dis. 1998;25:161. doi: 10.1097/00007435-199803000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Neumann MS, O’Donnell L, San Doval A, et al. Effectiveness of the VOICES/VOCES sexually transmitted disease/human immunodeficiency virus prevention intervention when administered by health department staff: does it work in the “real world”? Sex Transm Dis. 2011;38:133. doi: 10.1097/OLQ.0b013e3181f0c051. [DOI] [PubMed] [Google Scholar]
- 26.Card JJ, Kuhn T, Solomon J, et al. Translating an effective group-based HIV program to a program delivered mainly by a computer: methods and outcomes. AIDS Educ Prev. 2011;23:159. doi: 10.1521/aeap.2011.23.2.159. [DOI] [PubMed] [Google Scholar]
- 27.Downs JS, Murray PJ, Bruine de Bruin W, et al. Interactive video behavioral intervention to reduce adolescent females’ STD risk: a randomized controlled trial. Soc Sci Med. 2004;59:1561. doi: 10.1016/j.socscimed.2004.01.032. [DOI] [PubMed] [Google Scholar]
- 28.Higgins J, Altman D, Sterne J. Assessing risk of bias in included studies. In: Higgins J, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions (Version 5.1.0) West Sussex, England: the Cochrane Collaboration; 2011. [Google Scholar]
- 29.Kasen S, Vaughan RD, Walter HJ. Self-efficacy for AIDS preventive behaviors among tenth grade students. Health Educ Behav. 1992;19:187. doi: 10.1177/109019819201900204. [DOI] [PubMed] [Google Scholar]
- 30.Downs JS. Prescriptive scientific narratives for communicating usable science. Proc Natl Acad Sci U S A. 2014;111(suppl 4):13627. doi: 10.1073/pnas.1317502111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Downs JS, Bruine de Bruin W, Fischhoff B, et al. Behavioral decision research intervention reduces risky sexual behavior. Curr HIV Res. 2015;13:439. doi: 10.2174/1570162x13666150511145328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Downs JS, Bruine de Bruin W, Murray P, et al. When “it only takes once fails”: perceived infertility predicts condom use and STI acquisition. J Pediatr Adolesc Gynecol. 2004;17:224. [Google Scholar]
- 33.Downs JS, Bruine de Bruin W, Murray PJ, et al. Specific STI knowledge may be acquired too late. J Adolesc Health. 2006;38:65. doi: 10.1016/j.jadohealth.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 34.Bruine de Bruin W, Downs JS, Fischhoff B, et al. Development and evaluation of an HIV/AIDS knowledge measure for adolescents focusing on gaps and misconceptions. J HIV/AIDS Prev Child Youth. 2007;8:35. [Google Scholar]
- 35.Fischhoff B, Downs JS. Accentuate the relevant. Psychol Sci. 1997;8:154. [Google Scholar]
- 36.Fischhoff B, Downs JS, Bruine de Bruin W. Adolescent vulnerability: a framework for behavioral interventions. Appl Prev Psychol. 1998;7:77. [Google Scholar]
- 37.Murray PJ, Downs JS, White JP, et al. Previous clinical diagnosis of chlamydia helps patients predict outcome of new chlamydia. J Pediatr Adolesc Gynecol. 2000;13:98. doi: 10.1016/s1083-3188(00)00037-1. [DOI] [PubMed] [Google Scholar]
- 38.Murray PJ, Downs JS, Fischhoff B, et al. Contraceptive choice: a behavioral correlate of condom use. J Adolesc Health; Poster presented at San Diego, CA: Society of Adolescent Health and Medicine (SAHM) annual conference; abstract; 2001. p. 136. [Google Scholar]
- 39.Bandura A. Social foundations of thought and action. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 40.Maibach E, Flora JA. Symbolic modeling and cognitive rehearsal using video to promote AIDS prevention self-efficacy. Comm Res. 1993;20:517. [Google Scholar]
- 41.Slovic P, Peters E, Finucane ML, et al. Affect, risk, and decision making. Health Psychol. 2005;24(4 suppl):S35. doi: 10.1037/0278-6133.24.4.S35. [DOI] [PubMed] [Google Scholar]
- 42.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 43.Bandura A. Perceived self-efficacy in the exercise of control over AIDS infection. Eval Program Plann. 1990;13:9. [Google Scholar]
- 44.Sheeran P, Abraham C, Orbell S. Psychosocial correlates of heterosexual condom use: a meta-analysis. Psychol Bull. 1999;125:90. doi: 10.1037/0033-2909.125.1.90. [DOI] [PubMed] [Google Scholar]
- 45.Bandura A. Self-efficacy. In: Ramachauydran VS, editor. Encyclopedia of Human Behavior. Vol. 4. New York: Academic Press; 1994. pp. 71–81. [Google Scholar]