Abstract
A method based on Melting Temperature analysis of Hypervariable regions (HVR) of S1 gene within a RT-qPCR was developed to detect different genotypes of avian infectious bronchitis virus (IBV) and identify the Mass genotype. The method was able to rapidly identify the Mass genotype among IBV field isolates, vaccine attenuated strains and reference M41 strain in allantoic liquid and also directly in tissues. The RT-qPCR developed detected the virus in both tracheal and pulmonary samples from M41-infected or H120-infected birds, in a larger post-infection period compared to detection by standard method of virus isolation. RT-qPCR method tested provided a sensitivity and rapid approach for screening on IBV detection and Mass genotyping from IBV isolates.
Keywords: avian infectious bronchitis virus, Massachusetts, melting temperature analysis, RT-qPCR, S1 gene
Avian infectious bronchitis (IB) is an acute and highly infect-contagious viral disease, responsible by significant economic loss to the poultry industry worldwide that is caused by avian infectious bronchitis virus (IBV) [6]. IBV genome is well known to be highly prone to undergo mutations, leading to changes on nucleotide and/or amino acids sequences of the major structural IBV genes/proteins, resulting in multiple variants of this virus. Most important target of mutations is the spike 1 (S1) glycoprotein gene, especially those located in HVR I, (region encoding amino acid residues 56–69), and HVR II (region encoding amino acid residues 117–131). These regions of S1 glycoprotein have sites involved on the virus attachment to the receptors in the target host cells and the most important neutralizing epitopes. Mutations in the S gene could result in antigenic changes and emergence of IBV variants. This constant arising of new IB variants in different countries [8, 18] is usually pointed as the main cause of vaccine failures in the field and constitutes a great challenge for the molecular direct diagnosis of IBV.
Variants of IBV are mutants evolving from parental strains of this virus that differ from strains considered classic, such as those from Massachusetts group, regarding genotype, pathotype, antigenicity and/or immunogenicity. Additionally, IBV mutants are constantly subject to host immune selection and only strains with high antigenic variation are able to evade immune responses induced by vaccines and to survive in the population of hosts, leading to the development of clinical disease [25].
Protection studies between commercial vaccines and IBV variants, especially those using Massachusetts (Mass) vaccines, which is the most common attenuated available vaccine, have demonstrated at least partial cross-protection by some authors [9, 10, 12, 14, 34], while another studies have not found cross-protection [7, 35].
Therefore, the rapid detection of IBV infection in poultry flocks and its classification between Mass and variants is considered as major challenge, which requires use of appropriate diagnostic methods. To overcome this issue, several rapid assays have been developed focusing on detection and/or characterization of S1 gene of IBV, including direct gene sequencing, RT-PCR methods with serotype-specific primers, and RT-PCR/RFLP, have become widely used, because their results correlated well with the virus-serotyping [19, 21, 22, 33]. Beside these molecular methods, RT-qPCR methods using primers and probes for S1 gene or UTR region were developed and applied for IBV diagnosis, resulting in high sensitivity and specificity [5]. A SYBR Green RT-qPCR was tested on a wide range of coronaviruses and clinical samples, but it was not able to discriminate the different virus genus or strains [11]. Alternatively, a RT-qPCR based on the 3′-UTR of IBV (RT-PCR/HRM curve analysis model), could detect and rapidly distinguish novel and vaccine-related IBV strains from Australia [15]. Finally, a duplex SYBR Green I based RT-qPCR [1] and a RT-qPCR using specific probes [13, 23] were able to detect and differentiate Mass and non-Mass strains.
Finally, considering that HVR I and HVR II of S1 gene were thought to be closely associated with major neutralization epitopes and consequently a reliable target for genotyping method, we developed a diagnostic method using Melting Temperature analysis based on these regions aiming to rapid detect and differentiate Mass and non-Mass IBV strains in samples previously isolated and directly in clinical samples. Analytical specificity and sensitivity were also evaluated, and the method was compared to the standard method of virus isolation in embryonated eggs.
Seven reference IBV strains (M41, H120, H52, Ma5, JMK, SE17 and Connecticut) and six Brazilian field isolates (IBVSC01, IBVSC02, IBVPR02, IBVPR03, IBVPR05 and IBVPR07) were provided by Empresa Brasileira de Pesquisa Agropecuária-Embrapa (Concórdia, SC, Brazil) and previously molecularly characterized [26] (Table 1). Three other non-related viruses (commercial vaccines) were also used to confirm specificity of our method: Newcastle disease virus (NDV, La Sota vaccine strain), infectious bursal disease (IBDV, Lukert vaccine strain) and avian metapneumovirus (AMPV, PL-21 vaccine strain).
Table 1. Avian Infectious Bronchitis virus strains tested by Melting curve analysis using RT-qPCR with SYBR Green I, respective access number in the Genbank, classification of genotype, Tm, fragment length and percentage of GC for HVR I and HVR II regions.
| S1 region | HVR I | HVR II | ||||||
|---|---|---|---|---|---|---|---|---|
| Virus strain | Accession numbera) | Genotypeb) | Tm (°C) | bp | %GC | Tm (°C) | bp | %GC |
| H120 | M21970 | Massachusetts | 81.77 ± 0.06c) | 228 | 41.23 | 77.77 ± 0.12c) | 191 | 32.46 |
| H52 | AF352315 | Massachusetts | 81.33 ± 0.06c) | 228 | 41.23 | 77.77 ± 0.12c) | 191 | 31.41 |
| Ma5 | AY561713 | Massachusetts | 81.30 ± 0.43c) | 228 | 41.23 | 77.80 ± 0.14c) | 191 | 32.98 |
| M41 | M21883 | Massachusetts | 81.77 ± 0.12c) | 228 | 42.54 | 76.16 ± 0.29d) | 191 | 30.37 |
| IBVSC01 | GQ169246 | Massachusetts | 81.17 ± 0.20c) | 228 | 40.79 | 77.70 ± 0.00c) | 191 | 32.98 |
| IBVPR03 | GQ169241 | Massachusetts | 81.33 ± 0.30c) | 228 | 41.23 | 77.55 ± 0.21c) | 191 | 32.46 |
| IBVPR07 | GQ169244 | Massachusetts | 81.33 ± 0.28c) | 228 | 40.79 | 77.63 ± 0.10c) | 191 | 32.98 |
| Connecticut | L18990 | Connecticut | 80.70 ± 0.10d) | 216 | 39.35 | 77.70 ± 0.05c) | 191 | 31.94 |
| IBVSC02 | GQ169247 | Connecticut | 80.60 ± 0.14d) | 216 | 39.35 | 77.70 ± 0.05c) | 191 | 31.94 |
| JMK | L14070 | JMK | 83.40 ± 0.10e) | 228 | 41.67 | 78.15 ± 0.07e) | 209 | 33.97 |
| SE 17 | AF239984 | SE 17 | 83.70 ± 0.10e) | 228 | 41.23 | 78.25 ± 0.21e) | 212 | 31.60 |
| IBVPR02 | GQ169240 | Brazilian Variant-B | 80.30 ± 0.34d) | 219 | 37.90 | 77.60 ± 0.14c) | 212 | 33.49 |
| IBVPR05 | GQ169242 | Brazilian Variant-C | 83.17 ± 0.12e) | 228 | 38.60 | 76.90 ± 0.14f) | 212 | 33.96 |
Significant differences between Tm’s values were detected by Scott-Knott test and are represented by different letters c–f), with P≤0.05. a) Genbank accession number for S1 gene sequence data where available. b) The genotype of each IBV strain had been examined previously by RFLP or nucleotide sequence of S1 gene [21, 26].
Ninety-six one-day-old chicks (Cobb-Vantress Lineage) from a commercial broiler chick hatchery were separated in three positive pressure isolators. At 28 days of age, first group (n=42) was experimentally infected by intra-ocular and intranasal routes with 105.0 EID50 (50% Embryo Infective Dose) of M41 strain. A negative control group (n=42) was mock infected and maintained under the same conditions. Remaining group (n=12) was inoculated with H120 live attenuated vaccine. Three chickens from the first and second groups were euthanized at 1–10, 12, 15, 17 and 20 days post infection (dpi), while birds from third group were euthanized at 3, 5 e 12 dpi. Trachea and lung samples were collected and kept at −70°C until processing by RNA extraction or virus isolation. Throughout the experimental period, birds received water ad libitum and feed once a day, the room temperature was adapted according with bird’s age. All procedures have been approved by the Veterinary Sciences Animal Care Committee of Universidade Estadual Paulista, according with ethical principles of animal experimentation adopted by Brazilian College of Experimentation.
Virus isolation in Specific Pathogen Free (SPF) embryonated chicken eggs from tissue samples was performed as previously described [28]. Three passages were conducted to confirm negative samples.
Extraction of RNA from virus strains and tissue samples were performed using Trizol Reagent (Invitrogen, Carlsbad, CA, U.S.A.). The cDNA was synthesized according to instructions provided with SuperScript III Reverse Transcriptase (Invitrogen) and Random Primer (Invitrogen). qPCR was carried out in an Applied Biosystems Real-time 7500 Instrument (Applied Biosystems, Foster City, CA, U.S.A.) using 10 µl of Platinum SYBR Green qPCR SuperMix-UDG (Invitrogen), 10 pmol of each primer (Table 2), 2 µl of cDNA, in a final volume of 20 µl. The amplification reaction included a preincubation step at 95°C for 8 min to activate the HotStart Taq DNA polymerase, followed by 40 cycles of amplification including denaturation at 95 for 30 sec, annealing at 49.2°C for 30 sec and extension at 72°C for 30 sec [27]. After amplification by RT-qPCR, a melting analysis curve was performed by raising the incubation temperature from 65 to 95°C in 0.1°C increments with a hold of 1 sec at each increment.
Table 2. Sequences of primers used in RT-qPCR for detection of S1 gene of IBV.
| Region | Primer | Sequence | Positionb) | Reference |
|---|---|---|---|---|
| HVRI | C2 | F-TGG TTG GCA TTT ACA CGG GG | 20487–20506 | [33] |
| C3a) | R-CAA TGT GTA ACA AAC AC | 20698–20714 | ||
| HVRII | HV+ | F-GTT ACA CAT TGT TAT AA | 20704–20720 | [27] |
| HV− | R-ACA AGA TCA CCA TTT AA | 20878–20894 |
F=Forward, R=Reverse. a) Modified, b) Annealing site on S1in M41 reference strain of IBV (sequence accession number: AY851295).
The analytical specificity of RT-qPCR was assessed using three non-related RNA viruses including Newcastle disease virus (NDV, La Sota vaccine strain), infectious bursal disease (IBDV, Lukert vaccine strain) and avian metapneumovirus (AMPV, PL-21 vaccine strain).
The analytical sensitivity of RT-qPCR was assessed using seven serial ten-fold dilutions of plasmidial DNA containing the orf of S1 gene fragment (1.6 kb) of M41 strain of IBV cloned into the PYES 2.1/v5–His TOPO vector (Invitrogen), using two combinations of oligonucleotides to evaluate the analytical sensitivity. Cq (Cycle quantification) results were used to calculate the Log of IBV copies (Log10) using linear equation from a standard curve. The reproducibility was determined by testing in duplicate and in four independent runs, followed by calculation of mean, standard deviation (S.D.) and coefficient of variation (C.V.).
Tm data of the real-time RT-PCR assay was analyzed statistically by the Scott-Knott test [30], and the level of significance was set at P≤0.05.
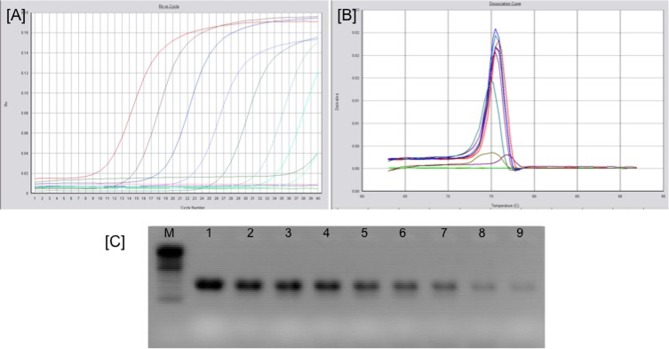
The detection limit of RT-qPCR was 1.32 × 102 copies, R2=0.997, efficiency=93.06% (Fig. 1). The reproducibility ranged from 0.1575 to 0.7585 cycles, while the C.V. inter-assay ranged from 0.56 to 2.64%. All IBV strains were successfully detected and no positive signal was recorded for the three non-related avian RNA-viruses tested.
Fig. 1.
Results obtained from analytical sensitivity test of RT-qPCR for IBV detection using tenfold serial dilutions of plasmidial DNA containing the S1 gene of M41 strain of IBV (10−1 to 10−9): [A] Amplification curves from RT-qPCR, [B] Dissociation curves RT-qPCR, [C] Electrophoresis analysis of amplified products from the dilutions of plasmidial DNA: (M) −100 bp ladder (Invitrogen), (lanes 1 to 9 correspond to dilutions 10−1 to 10−9).
The RT-qPCR developed in this study detected the virus in tracheal samples from birds experimentally infected with M41, or with H120 strains, in the period from 1 to 20 dpi (entire post-infection period evaluated) or from 3 to 12 dpi, respectively, while in pulmonary samples IBV detection varied from 8 to 15 dpi, or only at 3 dpi in M41-infected or H120-infected birds, respectively. Conversely, the standard method of virus isolation in SPF embryonated eggs detected the virus only from 2 to 9 dpi or at 3 dpi for both types of tissue samples from birds infected with M41 or H120, respectively. No positive signal of amplification and no positive results by virus isolation were found in tissues samples from negative control birds (Table 3).
Table 3. Virus detection in pulmonary and tracheal samples from experimentally infected chickens (M41 or H120 strains) by RT-qPCR and virus isolation methods.
| Challenge | RT-qPCR | VI | |
|---|---|---|---|
| Lung | M41 | 11/14 | 8/14 |
| Trachea | M41 | 14/14 | 8/14 |
| Lung | H120 | 1/3 | 1/3 |
| Trachea | H120 | 3/3 | 1/3 |
| Lung | Mock infected | 0/14 | 0/14 |
| Trachea | Mock infected | 0/14 | 0/14 |
Birds of same group/interval (3 biological replicates) were pooled and processed as one sample by both RT-qPCR and VI.
The absence of amplification signal in other non-related RNA viruses and in negative control samples, characterized the specificity of RT-qPCR.
All tested IBV strains were amplified by RT-qPCR using both primer sets (HVR I and HVR II). Amplicons of expected size for S1 gene of IBV using HVR I or HVR II primer sets were also visualized by gel electrophoresis analysis. In the first-derivative melting curve analysis, the S1 gene amplicons displayed melting temperature (Tm) values ranging from 80.30 to 83.70°C, for HVR I amplicons, and from 76.16 to 78.25°C for HVR II amplicons.
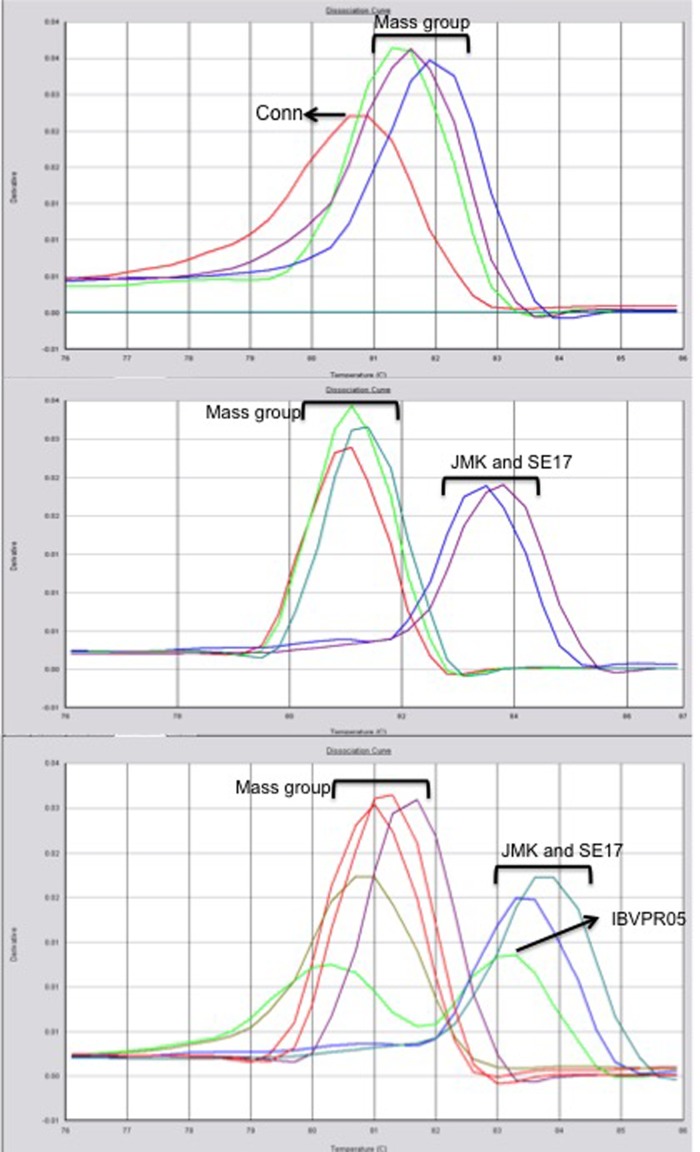
All Mass related IBV strains (reference strains and field isolates) tested in this study presented the same Tm profile (81.38 ± 0.28°C) for melting temperature analysis of HVR I amplicons, as no significant differences were observed, while all the remaining tested strains presented significant differences in their Tm profiles (Fig. 2). Interestingly, the IBVPR05 strain, showed two melting peaks, with the highest peak at 83.17°C, and another one at the same Tm profile as Mass group (Fig. 2). We hypothesized that this sample of Brazilian field isolate was composed by two populations or quasispecies, as described previously [17] for a sample of Beaudette strain of IBV amplified by RT-qPCR using another pair of primers.
Fig. 2.
Dissociation curves obtained from RT-qPCR products using primers flanking HVRI region of S1 of IBV from different IBV strain tested.
However, when the melting temperature analysis was performed using HVR II region, the Mass genotype differentiation was not possible, though the Tm profiles for HVR II amplicons of JMK and SE-17 strains and one Brazilian variant isolate (IBVPR05) were distinct one each other and from the remaining tested IBV strains. A similar distinction was observed in the Tm profile of HVR II amplicon for M41 strain with regard to H120 strain, in spite of these viruses are classified in the Massachusetts genotype.
The detection limit of our method is similar to that recorded for a real-time PCR assay based on 5′-UTR gene of IBV genome [3]. However our assay is less sensitive than another real-time technique targeting an ORF1b of replicase gene of IBV [11]. This difference might be due to the fact that targeting the most conserved and abundant genes of coronavirus, like replicase gene or nucleoprotein gene, can enhance the sensitivity of conventional and RT-qPCR methods [2, 11, 24]. Nonetheless, more conserved target genes do not allow differentiation between different genotypes of IBV [24], as S1 gene RT-PCR does, which remains an important tool for genotyping IBV isolates.
There are several reports demonstrating the use of melting temperature analysis to differentiate genotypes of virus pathogens [4, 20, 29, 31, 32]. Similarly, the method used here provided differentiation of Mass genotype using HVR I region, as all tested strains previously genotyped belonging to Mass genotype presented no significant different Tm values, while the other strains previously genotyped differently from Mass presented significant different Tm values (Table 1). In addition, previous study [16] using primers flanking similar HVRs of S1 gene in RT-qPCR with EVAGREEN succeeded in discriminating IBV strains from Taiwan and H120 from M41 strain of IBV.
Currently, IBV genotype differentiation has been performed using separated molecular assays, which have increased both time and cost. Assays for genotyping based on conventional molecular methods such as PCR, RFLP, hybridization assay and direct sequencing are time-consuming, more complex and expensive. Alternatively, the method described here has allowed simultaneous detection of IBV genome and Mass genotype identification in a single reaction. The specificity of Mass genotyping by our method was confirmed, comparing with the results obtained previously [21, 26].
In conclusion, the method described here provides a practical and effective screening test for simultaneous detection and Mass genotyping of IBV. Moreover, this rapid, simple, specific and sensitive test is applicable for both IBV previously isolated and directly in clinical samples.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
Acknowledgments
The authors thank FAPESP (process number 04/12267-2 and 01/14950-3) and CNPq (process number 01/14950-3) for the financial support; Embrapa (Concórdia, SC, Brazil) for supplying IBV strains; Merial (Campinas, SP, Brazil) for provided the embryonated chickens eggs SPF and Frango Sertanejo (Ipiguá, SP, Brazil) for provided the commercial broilers. We also thank Professor Dr Joao Ademir de Oliveira for statistical advice.
REFERENCES
- 1.Acevedo A. M., Perera C. L., Vega A., Ríos L., Coronado L., Relova D., Frías M. T., Ganges L., Núñez J. I., Pérez L. J.2013. A duplex SYBR Green I-based real-time RT-PCR assay for the simultaneous detection and differentiation of Massachusetts and non-Massachusetts serotypes of infectious bronchitis virus. Mol. Cell. Probes 27: 184–192. doi: 10.1016/j.mcp.2013.06.001 [DOI] [PubMed] [Google Scholar]
- 2.Callison S. A., Hilt D. A., Jackwood M. W.2005. Rapid differentiation of avian infectious bronchitis virus isolates by sample to residual ratio quantitation using real-time reverse transcriptase-polymerase chain reaction. J. Virol. Methods 124: 183–190. doi: 10.1016/j.jviromet.2004.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Callison S. A., Hilt D. A., Boynton T. O., Sample B. F., Robison R., Swayne D. E., Jackwood M. W.2006. Development and evaluation of a real-time Taqman RT-PCR assay for the detection of infectious bronchitis virus from infected chickens. J. Virol. Methods 138: 60–65. doi: 10.1016/j.jviromet.2006.07.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chutinimitkul S., Payungporn S., Theamboonlers A., Poovorawan Y.2005. Dengue typing assay based on real-time PCR using SYBR Green I. J. Virol. Methods 129: 8–15. doi: 10.1016/j.jviromet.2005.05.006 [DOI] [PubMed] [Google Scholar]
- 5.Chousalkar K. K., Cheetham B. F., Roberts J. R.2009. LNA probe-based real-time RT-PCR for the detection of infectious bronchitis virus from the oviduct of unvaccinated and vaccinated laying hens. J. Virol. Methods 155: 67–71. doi: 10.1016/j.jviromet.2008.09.028 [DOI] [PubMed] [Google Scholar]
- 6.Cook J. K. A., Jackwood M., Jones R. C.2012. The long view: 40 years of infectious bronchitis research. Avian Pathol. 41: 239–250. doi: 10.1080/03079457.2012.680432 [DOI] [PubMed] [Google Scholar]
- 7.Darbyshire J. H.1980. Assessment of cross-immunity dm chickens to strains of avian infectious bronchitis virus using tracheal organ cultures. Avian Pathol. 9: 179–184. doi: 10.1080/03079458008418401 [DOI] [PubMed] [Google Scholar]
- 8.De Wit J. J., Cook J. K. A., van der Heijden H. M.2011. Infectious bronchitis virus variants: a review of the history, current situation and control measures. Avian Pathol. 40: 223–235. doi: 10.1080/03079457.2011.566260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Wit J. J., Brandao P., Torres C. A., Koopman R., Villarreal L. Y.2015. Increased level of protection of respiratory tract and kidney by combining different infectious bronchitis virus vaccines against challenge with nephropathogenic Brazilian genotype subcluster 4 strains. Avian Pathol. 44: 352–357. doi: 10.1080/03079457.2015.1058916 [DOI] [PubMed] [Google Scholar]
- 10.Di Fabio J., Rossini L. I., Orbell S. J., Paul G., Huggins M. B., Malo A., Silva B. G., Cook J. K.2000. Characterization of infectious bronchitis viruses isolated from outbreaks of disease in commercial flocks in Brazil. Avian Dis. 44: 582–589. doi: 10.2307/1593097 [DOI] [PubMed] [Google Scholar]
- 11.Escutenaire S., Mohamed N., Isaksson M., Thorén P., Klingeborn B., Belák S., Berg M., Blomberg J.2007. SYBR Green real-time reverse transcription-polymerase chain reaction assay for the generic detection of coronaviruses. Arch. Virol. 152: 41–58. doi: 10.1007/s00705-006-0840-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fernando F. S., Montassier M. F. S., Silva K. R., Okino C. H., Oliveira E. S., Fernandes C. C., Bandarra M. B., Gonçalves M. C. M., Borzi M. M., Santos R. M., Vasconcelos R. O., Alessi A. C., Montassier H. J.2013. Nephritis associated with S1 variant brazilian isolate of infectious bronchitis virus and vaccine protection test in experimentally infected chickens. Int. J. Poult. Sci. 12: 639–646. doi: 10.3923/ijps.2013.639.646 [DOI] [Google Scholar]
- 13.Fraga A. P., Ikuta N., Fonseca A. S., Spilki F. R., Balestrin E., Rodrigues C. D., Canal C. W., Lunge V. R.2016. A Real-Time Reverse-Transcription Polymerase Chain Reaction for Differentiation of Massachusetts Vaccine and Brazilian Field Genotypes of Avian Infectious Bronchitis Virus. Avian Dis. 60: 16–21. doi: 10.1637/11262-081815-RegR.1 [DOI] [PubMed] [Google Scholar]
- 14.Grgić H., Hunter D. B., Hunton P., Nagy E.2009. Vaccine efficacy against Ontario isolates of infectious bronchitis virus. Can. J. Vet. Res. 73: 212–216. [PMC free article] [PubMed] [Google Scholar]
- 15.Hewson K., Noormohammadi A. H., Devlin J. M., Mardani K., Ignjatovic J.2009. Rapid detection and non-subjective characterisation of infectious bronchitis virus isolates using high-resolution melt curve analysis and a mathematical model. Arch. Virol. 154: 649–660. doi: 10.1007/s00705-009-0357-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang S. W., Ho C. F., Chan K. W., Cheng M. C., Shien J. H., Liu H. J., Wang C. Y.2014. The genotyping of infectious bronchitis virus in Taiwan by a multiplex amplification refractory mutation system reverse transcription polymerase chain reaction. J. Vet. Diagn. Invest. 26: 721–733. doi: 10.1177/1040638714547735 [DOI] [PubMed] [Google Scholar]
- 17.Jackwood M. W., Hilt D. A., Callison S. A.2003. Detection of infectious bronchitis virus by real-time reverse transcriptase-polymerase chain reaction and identification of a quasispecies in the Beaudette strain. Avian Dis. 47: 718–724. doi: 10.1637/6075 [DOI] [PubMed] [Google Scholar]
- 18.Jackwood M. W.2012. Review of infectious bronchitis virus around the world. Avian Dis. 56: 634–641. doi: 10.1637/10227-043012-Review.1 [DOI] [PubMed] [Google Scholar]
- 19.Keeler C. L., Jr., Reed K. L., Nix W. A., Gelb J., Jr1998. Serotype identification of avian infectious bronchitis virus by RT-PCR of the peplomer (S-1) gene. Avian Dis. 42: 275–284. doi: 10.2307/1592477 [DOI] [PubMed] [Google Scholar]
- 20.Kong L. L., Omar A. R., Hair Bejo M., Ideris A., Tan S. W.2009. Development of SYBR green I based one-step real-time RT-PCR assay for the detection and differentiation of very virulent and classical strains of infectious bursal disease virus. J. Virol. Methods 161: 271–279. doi: 10.1016/j.jviromet.2009.06.023 [DOI] [PubMed] [Google Scholar]
- 21.Kwon H. M., Jackwood M. W., Gelb J., Jr.1993. Differentiation of infectious bronchitis virus serotypes using polymerase chain reaction and restriction fragment length polymorphism analysis. Avian Dis. 37: 194–202. doi: 10.2307/1591474 [DOI] [PubMed] [Google Scholar]
- 22.Lin Z., Kato A., Kudou Y., Ueda S.1991. A new typing method for the avian infectious bronchitis virus using polymerase chain reaction and restriction enzyme fragment length polymorphism. Arch. Virol. 116: 19–31. doi: 10.1007/BF01319228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marandino A., Tomás G., Hernández M., Panzera Y., Craig M. I., Vagnozzi A., Vera F., Techera C., Grecco S., Banda A., Hernández D., Pérez R.2016. Development of RT-qPCR assays for the specific identification of two major genotypes of avian infectious bronchitis virus. J. Virol. Methods 235: 21–25. doi: 10.1016/j.jviromet.2016.05.007 [DOI] [PubMed] [Google Scholar]
- 24.Meir R., Maharat O., Farnushi Y., Simanov L.2010. Development of a real-time TaqMan RT-PCR assay for the detection of infectious bronchitis virus in chickens, and comparison of RT-PCR and virus isolation. J. Virol. Methods 163: 190–194. doi: 10.1016/j.jviromet.2009.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Montassier H. J.2010. Molecular epidemiology and evolution of avian infectious bronchitis virus. Braz. J. Poultry Sci. 12: 87–96. [Google Scholar]
- 26.Montassier M. F. S., Montassier H. J., Brentano L., Richtzenhain L. J.2008. Genetic grouping of avian infectious bronchitis virus isolated in Brazil, based on RT-PCR/RFLP analysis of the S1 gene. Braz. J. Vet. Res. 28: 190–194. [Google Scholar]
- 27.Okino C. H., dos Santos I. L., Fernando F. S., Alessi A. C., Wang X., Montassier H. J.2014. Inflammatory and cell-mediated immune responses in the respiratory tract of chickens to infection with avian infectious bronchitis virus. Viral Immunol. 27: 383–391. doi: 10.1089/vim.2014.0054 [DOI] [PubMed] [Google Scholar]
- 28.Owen R. L.,, Cowen B. S., Hattel A. L., Naqi S. A., Wilson R. A.1991. Detection of viral antigen following exposure of one-day-old chicken to the Holland-52 strain of IBV. Avian Pathol. 20: 663–673. doi: 10.1080/03079459108418805 [DOI] [PubMed] [Google Scholar]
- 29.Pham H. M., Konnai S., Usui T., Chang K. S., Murata S., Mase M., Ohashi K., Onuma M.2005. Rapid detection and differentiation of Newcastle disease virus by real-time PCR with melting-curve analysis. Arch. Virol. 150: 2429–2438. doi: 10.1007/s00705-005-0603-0 [DOI] [PubMed] [Google Scholar]
- 30.Scott A. J., Knott M. A.1974. Cluster analysis method for grouping means in the analysis of variance. Biometrics 30: 507–512. doi: 10.2307/2529204 [DOI] [Google Scholar]
- 31.Tan S. W., Ideris A., Omar A. R., Yusoff K., Hair-Bejo M.2009. Detection and differentiation of velogenic and lentogenic Newcastle disease viruses using SYBR Green I real-time PCR with nucleocapsid gene-specific primers. J. Virol. Methods 160: 149–156. doi: 10.1016/j.jviromet.2009.05.006 [DOI] [PubMed] [Google Scholar]
- 32.Varga A., James D.2006. Real-time RT-PCR and SYBR Green I melting curve analysis for the identification of Plum pox virus strains C, EA, and W: effect of amplicon size, melt rate, and dye translocation. J. Virol. Methods 132: 146–153. doi: 10.1016/j.jviromet.2005.10.004 [DOI] [PubMed] [Google Scholar]
- 33.Wang C. H., Tsai C. T.1996. Genetic grouping for the isolates of avian infectious bronchitis virus in Taiwan. Arch. Virol. 141: 1677–1688. doi: 10.1007/BF01718291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wood M. K., Ladman B. S., Preskenis L. A., Pope C. R., Bautista D., Gelb J., Jr.2009. Massachusetts live vaccination protects against a novel infectious bronchitis virus S1 genotype DMV/5642/06. Avian Dis. 53: 119–123. doi: 10.1637/8454-082108-ResNote.1 [DOI] [PubMed] [Google Scholar]
- 35.Wu Z. Q., Yang Q. W., Fu C., Zhao X. Y., Ignjatovic J.1998. Antigenic and immunogenic characterization of infectious bronchitis virus strains isolated in China between 1986 and 1995. Avian Pathol. 27: 578–585. doi: 10.1080/03079459808419387 [DOI] [PMC free article] [PubMed] [Google Scholar]