Abstract
Introduction
Sublobar resection has become an acceptable alternative to lobectomy in patients with early-stage lung cancer. Most notable among these approaches is indocyanine green fluorescence (ICG) imaging.
Case presentation
Operative finding showed clear green staining of the left upper lobe, S6, superior pulmonary vein, and inferior PV under fluorescence navigation. Soon, the bronchial artery of right lower bronchus showed clear green staining. Next, the whole right lower bronchus is deeply colored green.
Discussion
ICG imaging can lead a planned operation safely in the extreme, especially for situations of special concern for blood supply of the bronchial stump such as pneumonectomy, bronchoplasty and right lower lobectomy.
Conclusion
This report describes a first case concerning the course and blood distribution of the bronchial artery using ICG injection under fluorescence navigation.
Keywords: Indocyanine green fluorescence, Bronchial artery, Surgical resection
Highlights
-
•
ICG fluorescence easily detects not only the segmental plane, but also the course and blood distribution of the bronchial artery at an unexpected moment.
-
•
These marvelous findings lead a planned operation safely in the extreme, especially for situations of special concern for blood supply of the bronchial stump.
1. Introduction
Lung cancer is the leading cause of death worldwide, and its diagnosis has been increasing due to the detection of small nodules by high-resolution computed tomography (CT) [1]. Sublobar resection has become an acceptable alternative to lobectomy in patients with early-stage lung cancer [1]. The use of an inflation-deflation line, bronchoscopy (BF), preoperative three-dimensional imaging, and other techniques have been explored to create an intersegmental plane for segmentectomy. Most notable among these approaches is indocyanine green fluorescence (ICG) imaging [2,3]. We received an enthusiastic response to enroll cases for an ICG prospective study after obtaining approval from the ethics committee of our institution (M416). We haphazardly experienced a case of clear blood distribution of the bronchial artery under fluorescence navigation among serial studies.
2. Case report
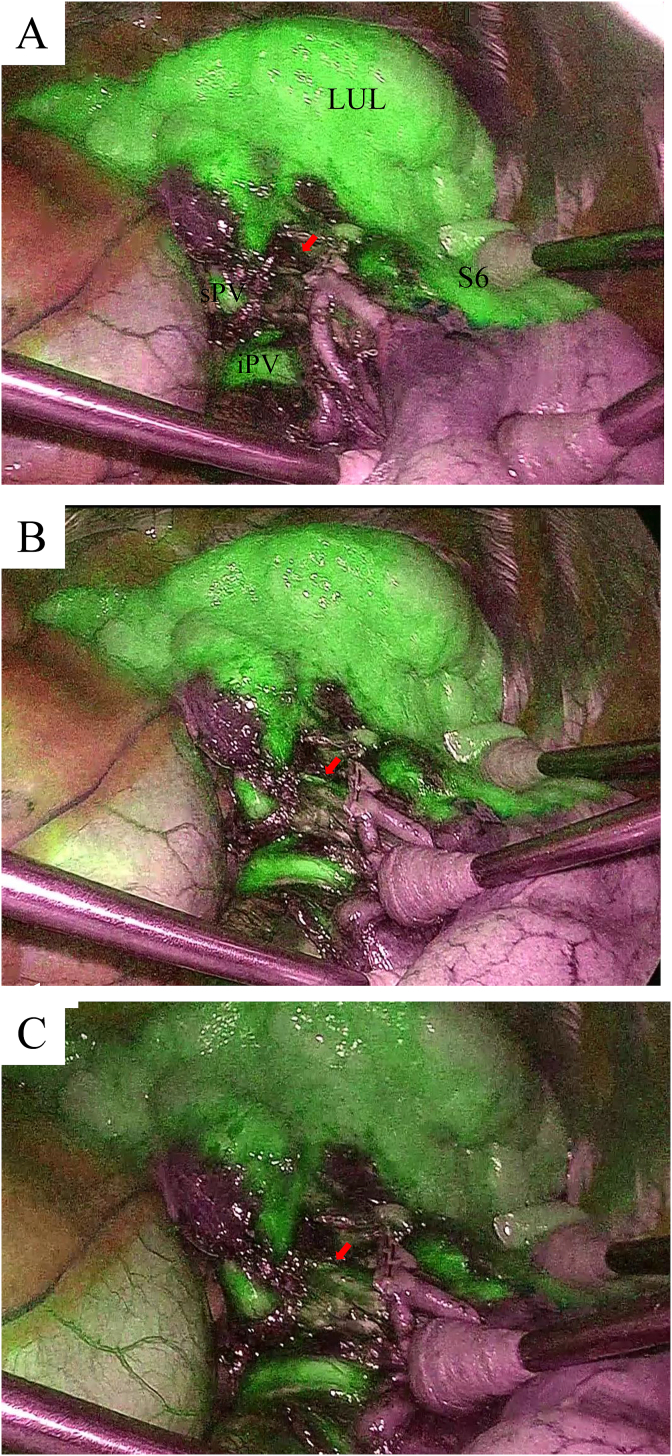
The Institutional Review Board approved this study and informed consent was obtained from the patient.An asymptomatic 71-year-old woman was suspected to have lung cancer. She took a prescribed drug for hypertension and diabetes mellitus and had no relevant family or psychosocial history. Chest CT showed a growing tumor in the central part of the left lung S9, adjacent to the S8, without any evidence of distant metastasis. Therefore, the lesion was clinically diagnosed to be at stage IA1 (cT1aN0M0). Preoperatively, her condition met all of the eligibility criteria, including performance status (ECOG) 0–1 and a good function of the main organs. General anesthesia was performed using a double lumen endotracheal tube for single-lung ventilation. The operation was performed by our team with the patient in the lateral decubitus position. We conformed to The SCARE statement [4]. A 10-mm, 30-degree thoracoscope was placed through the seventh intercostal space (ICS). Subsequently, an additional working port was made in the sixth ICS, just beside the scapula angle without using any trocars for counter-traction of the lung. A utility incision was made in the fourth ICS in the anterior axillary line without rib spreading. Left basal segmentectomy with lymph node dissection was planned. To clarify the surgical plane, ICG 5 mg was injected intravenously after cutting the basal artery under fluorescence navigation (Visera EliteII; Olympus Medical Science, Tokyo, Japan). Operative finding showed clear green staining of the left upper lobe, S6, superior pulmonary vein (sPV), and inferior PV (iPV) (Fig. 1A). Soon, the bronchial artery (BA) of right lower bronchus showed clear green staining (Fig. 1B). Next, the whole right lower bronchus is deeply colored green (Fig. 1C) (Supplementary video). Since S6 had a relatively small volume, left lower resection was performed. Pulmonary vessels, arteries, and bronchus were cut using an endoscopic stapler. The resected lungs were placed in plastic tissue pouches (8 × 10 inch LapSac; Cook Medical, Bloomington, IN). The total operation time was 1 hours and 23 minutes with 20 ml of intraoperative bleeding. The pathological examination revealed minimally invasive adenocarcinoma without hilar lymph node metastases. The tumor size was 10 × 7 mm (invasive size 3 × 2 mm). Therefore, the lesion was pathologically diagnosed to be at stage IA1 (T1miN0M0). No adverse events were seen. She had a good postoperative course without complications, and discharged on day 6 after surgery.
Fig. 1.
A: Operative finding showed clear green staining of the left upper lobe S6, sPV, and iPV following ICG injection. B: The BA shows clear green staining. C: The whole right lower bronchus is deeply colored green, whereas color of left upper lobe and S6 show no such staining.
Supplementary video related to this article can be found at https://doi.org/10.1016/j.amsu.2018.02.004.
The following is the supplementary data related to this article:
To clarify the surgical plane, ICG was injected intravenously after cutting the basal artery under fluorescence navigation. Operative finding showed clear green staining of the left upper lobe, S6, sPV, and iPV. Soon, the BA showed clear green staining. Next, the whole right lower bronchus is deeply colored green. Since S6 had a relatively small volume, left lower resection was performed.
3. Discussion
This report describes a first case concerning the course and blood distribution of the bronchial artery using ICG injection under fluorescence navigation. Until now, ICG technique has been explored to create an intersegmental plane for segmentectomy in our chest surgery. However, high sensitive camera can detect the course and blood distribution clearly. In fact, ICG imaging has been on the verge of a standard intraoperative graft as an assessment tool in coronary artery bypass graft (CABG) in the cardio vascular fields.
The bronchial stump is controlled by tension and the blood flow. It may thus be necessary to release the surrounding tissue to reduce the tension when suturing of the bronchus. However, this maneuver is associated with the risk of reducing the bronchial blood flow. If the blood flow can be clearly visualized, then a planned operation can be safely performed. Our intraoperative findings clearly showed both the course and blood distribution of the BA. Thus, ICG imaging can be used to safely lead a planned operation, especially in extreme situations in which there is special concern for the blood supply of the bronchial stump, such as pneumonectomy, bronchoplasty and right lower lobectomy.
Ethical approval
Not available. Informed and written consent has been given by patient. This study was approved by the ethics committee of the affiliated Kanazawa Medical University.
Funding
The authors reported no proprietary or commercial interest in any product mentioned or concept discussed in the article.
Author contribution
HU contributed to the conception and design. NM, and HU did the data collection. HU did the writing of the article and the critical revisions. NM did the analysis and interpretation.
Conflicts of interest
The authors reported no proprietary or commercial interest in any product mentioned or concept discussed in the article.
Guarantor
Hidetaka Uramoto, Kanazawa Medical University, 1-1 Daigaku, Uchinada, Ishikawa, 920-0293, Japan.
References
- 1.Bedetti B., Bertolaccini L., Rocco R., Schmidt J., Solli P., Scarci M. Segmentectomy versus lobectomy for stage I non-small cell lung cancer: a systematic review and meta-analysis. J. Thorac. Dis. 2017;9:1615–1623. doi: 10.21037/jtd.2017.05.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hsieh C.P., Liu Y.H., Wu Y.C., Hsieh M.J., Chao Y.K. Indocyanine green fluorescence-navigated robotic segmentectomy. Surg. Endosc. 2017;31:3347–3348. doi: 10.1007/s00464-016-5329-4. [DOI] [PubMed] [Google Scholar]
- 3.Iizuka S., Kuroda H., Yoshimura K., Dejima H., Seto K., Naomi A., Mizuno T., Sakakura N., Sakao Y. Predictors of indocyanine green visualization during fluorescence imaging for segmental plane formation in thoracoscopic anatomical segmentectomy. J. Thorac. Dis. 2016;8:985–991. doi: 10.21037/jtd.2016.03.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P. SCARE Steering Group. A protocol for the development of reporting criteria for surgical case reports: the SCARE statement. Int. J. Surg. 2016;27:187–189. doi: 10.1016/j.ijsu.2016.01.094. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
To clarify the surgical plane, ICG was injected intravenously after cutting the basal artery under fluorescence navigation. Operative finding showed clear green staining of the left upper lobe, S6, sPV, and iPV. Soon, the BA showed clear green staining. Next, the whole right lower bronchus is deeply colored green. Since S6 had a relatively small volume, left lower resection was performed.