Abstract
A small cortical infarction confined to the medial location of the precentral knob on the precentral gyrus may cause isolated shoulder palsy. However, there are no reports indicating intracerebral hemorrhage as a cause of isolated shoulder palsy. We herein report the case of a 48-year-old man who presented with isolated shoulder palsy as an initial symptom of subcortical hemorrhage at the precentral gyrus. Such cases may be easily misdiagnosed as shoulder or cervical spine problems. The distribution of muscle weakness is the key to an accurate diagnosis.
Keywords: isolated shoulder palsy, intracerebral hemorrhage, cervical spondylotic amyotrophy, idiopathic thrombocytopenic purpura
Introduction
Isolated shoulder palsy (ISP) caused by stroke is an extremely rare clinical condition. However, such cases are important for clinicians because they can be misdiagnosed as local lesions of the shoulder or cervical spine (i.e., as peripheral weakness). A few cases of ISP due to cerebral infarction in the precentral gyrus have been reported so far (1-5). However, to the best of our knowledge, there are no previous reports on ISP caused by intracerebral hemorrhage (ICH). We herein describe the case of a patient who presented with ISP due to subcortical hemorrhage at the precentral gyrus.
Case Report
A 48-year-old man experienced difficulty in elevating his right upper limb when he tried to stow baggage on a train shelf while commuting. On that day, he was able to work as usual and did not experience headache or neck pain. The next day, he visited our clinic because the symptom had not improved. He had been previously diagnosed with idiopathic thrombocytopenic purpura (ITP), and had been treated since 28 years of age. Corticosteroid therapy was not effective and the patient refused to undergo splenectomy. Therefore, the patient was treated with thrombopoietin receptor agonists and intravenous immunoglobulin (IVIg).
During the general examination, his consciousness was alert. His blood pressure was 124/78 mmHg and his heart rate was 64/min. A few petechiae were detected on the patient's extremities. There was no cervical or shoulder pain. A neurological examination revealed muscle weakness (Medical Research Council scale: 4/5) in the right lateral deltoid, anterior deltoid, and infraspinatus muscles. Other muscles in the right upper limb, such as the biceps brachii, triceps brachii, wrist extensor, wrist flexor, extensor digitorum, and intrinsic muscles, showed normal strength. The muscle strength of the left upper limb and both lower limbs was also normal. A cranial nerve examination revealed no abnormality. The results of sensory examinations and the patient's tendon reflexes were also normal with no laterality. There was no limb or truncal ataxia, and Babinski's sign was bilaterally negative. Routine blood tests were normal except for thrombocytopenia (0.7×104/μL). A blood coagulation test was also normal.
At first, proximal-type cervical spondylotic amyotrophy (CSA) was suspected based on the neurological findings (6). However, we planned to perform urgent computed tomography (CT) of the head because of the risk of bleeding, and because the distribution of muscle weakness did not completely match the myotome innervation. Specifically, although his weakness was predominantly confined to the muscles innervated by C5, the strength of the biceps brachii, which is innervated by C5 and C6, was normal.
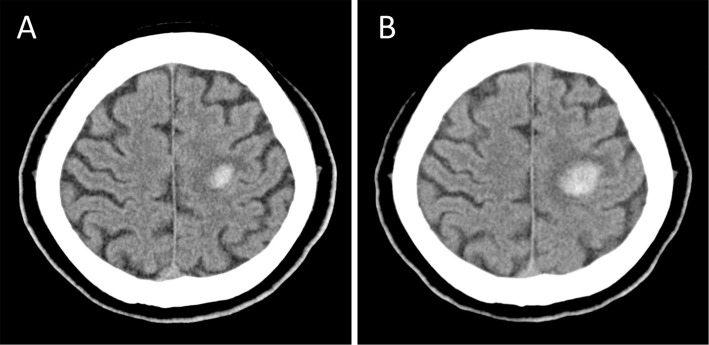
Head CT revealed a subcortical hemorrhage in the left precentral gyrus, which was located medial to the precentral knob (Figure A). The patient was immediately admitted and prescribed bed rest. Additionally, he was treated with antihypertensive agents because his blood pressure increased after admission. The bleeding tendency due to thrombocytopenia was thought to be the cause of the ICH. Therefore, IVIg for ITP was added to the treatment. On the day after admission, weakness of the right upper limb showed further progression to the distal muscles, and follow-up head CT revealed expansion of the hematoma (Figure B). However, the hematoma was gradually absorbed, and the platelet count slowly increased. Finally, he was discharged after 1 month. However, the weakness of the right upper limb, which affected his daily life, remained.
Figure.
Head computed tomography (CT) on admission revealed a left small subcortical hemorrhage in the precentral gyrus (A). Follow-up head CT on the day after admission revealed the expansion of the hematoma (B).
Discussion
In this case, the patient only presented isolated shoulder weakness when he visited our clinic. Initially, on the basis of the neurological findings, an experienced neurologist suspected proximal-type CSA. Thus, such cases are difficult to distinguish from peripheral weakness based on the neurological findings alone. Although head imaging examinations are the key to an accurate diagnosis, these may not be performed if the central weakness is not considered.
Typically, cervical spondylosis shows gradual progression. However, some cases of acute onset cervical spondylosis, especially CSA, have been reported (7). Thus, it may be difficult to distinguish the central weakness from the peripheral weakness based on the clinical course alone.
An important diagnostic clue in this case was that the distribution of muscle weakness did not match the myotome innervation. Commonly, patients with C5 disturbance show weakness of the muscles that are innervated by C5 (i.e., the deltoid, infraspinatus, biceps brachii, and brachioradialis muscles). In this case, the muscle weakness was confined in the shoulder while the biceps brachii strength was completely normal. The presence or absence of muscle weakness, especially in the biceps brachii, is useful for differentiation from proximal-type CSA. This point has not been stressed in previous reports on ISP.
The ICH of the present case was located medially to the precentral knob, which has been reported to be the motor hand area, and the location of the lesion was similar to that in the previous reports of ISP due to cerebral infarction (1-5). These findings indicate that this location is correlated with the shoulder motor area, and are consistent with the findings of motor homunculus described by Penfield and Boldrey (8).
IVIg alone was used as a treatment for thrombocytopenia in the present case. Although the patient's platelet count slowly increased, the hematoma expanded and the weakness progressed despite the treatment. In cases requiring emergency treatment, such as those presenting bleeding with marked thrombocytopenia (as in our case), the combination of concurrent IVIg and platelet transfusion should be considered for the rapid restoration of an adequate platelet count (9).
Previous reports have indicated that the prognosis of ISP due to cerebral infarction is good (10). However, in cases of ISP due to ICH, if an accurate diagnosis and treatment are delayed, the hematoma may increase, thereby leading to a poor outcome (11). Thus, cerebrovascular diseases including ICH should be considered as differential diagnoses in patients who present with acute ISP.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Komatsu K, Fukutake T, Hattori T. Isolated shoulder paresis caused by a small cortical infarction. Neurology 61: 1457, 2003. [DOI] [PubMed] [Google Scholar]
- 2. Nah HU, Park HK, Kang DW. Isolated shoulder weakness due to a small cortical infarction. J Clin Neurol 2: 209-211, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tsuda H, Kubota Y, Tanaka K, Kishida S. Isolated shoulder palsy due to a cortical infarction. Intern Med 50: 947, 2011. [DOI] [PubMed] [Google Scholar]
- 4. Tsuda H, Shinozaki Y, Tanaka K, Miura Y, Kishida S, Karasawa K. Isolated shoulder palsy due to infarction of the cortical branch of the middle cerebral artery. Intern Med 51: 2217-2219, 2012. [DOI] [PubMed] [Google Scholar]
- 5. Kanbayashi T, Hokkoku K, Hatanaka Y, Nishiyama K, Sonoo M. Isolated shoulder palsy diagnosed from needle EMG and an associated movement. Neurol Sci 36: 1527-1529, 2015. [DOI] [PubMed] [Google Scholar]
- 6. Keegan JJ. The cause of dissociated motor loss in the upper extremity with cervical spondylosis. J Neurosurg 23: 528-536, 1965. [DOI] [PubMed] [Google Scholar]
- 7. Sonoo M. Cervical spondylotic amyotrophy. Brain Nerve 68: 509-519, 2016. (in Japanese, Abstract in English). [DOI] [PubMed] [Google Scholar]
- 8. Penfield W, Boldrey E. Somatic motor and sensory representation in the cerebral cortex of man as studied by electrical stimulation. Brain 69: 389-443, 1937. [Google Scholar]
- 9. Spahr JE, Rodgers GM. Treatment of immune-mediated thrombocytopenia purpura with concurrent intravenous immunoglobulin and platelet transfusion: a retrospective review of 40 patients. Am J Hematol 83: 122-125, 2008. [DOI] [PubMed] [Google Scholar]
- 10. Kawasaki A, Suzuki K, Takekawa H, et al. Isolated shoulder palsy due to cortical infarction: a case report and literature review of clinicoradiological correlations. J Stroke Cerebrovasc Dis 22: e687-e690, 2013. [DOI] [PubMed] [Google Scholar]
- 11. LoPresti MA, Bruce SS, Camacho E, et al. Hematoma volume as the major determinant of outcomes after intracerebral hemorrhage. J Neurol Sci 345: 3-7, 2014. [DOI] [PubMed] [Google Scholar]