Abstract
Objectives:
To investigate the effect of Ramadan fasting on the symptoms of chronic heart failure with a reduced ejection fraction (HFrEF). Globally, more than one billion Muslims fast during Ramadan. Data regarding the effect of fasting in heart failure patients with a reduced ejection fraction are limited.
Methods:
We prospectively studied 249 outpatients with HFrEF who undertook Ramadan fasting at tertiary care cardiac center in Saudi Arabia in 2017. We obtained information regarding the clinical assessment, diagnosis, emergency department visits, and hospitalization during and in the month preceding Ramadan.
Results:
We enrolled 249 patients, 227 (91%) undertook the fast for the entire month. During Ramadan, 209 (92%) patients remained hemodynamically stable, whereas 18 (8%) developed instability. The mean New York Heart Association (NYHA) functional class was significantly lower in the stable than in the unstable group (1.46±0.7 vs. 3.22±0.55, p<0.0001), although no intergroup differences were observed before Ramadan. Patients from the unstable vs. the stable group showed significantly less adherence to medications (67% vs. 94%, p<0.0001) and to diet (39% vs. 79%, p<0.0001), and a lower likelihood of demonstrating ischemic cardiomyopathy as an underlying etiology of HFrEF (33% vs. 57%, p=0.046). Dependent t-test analysis including all patients showed that the NYHA classification before Ramadan was significantly higher than during Ramadan (2.19±0.9 vs. 1.6±0.8, t-value 8.5, p<0.0001).
Conclusion:
In most patients with chronic HFrEF, Ramadan fasting is considered safe. Non-adherence to medication and diet are significantly associated with decompensated heart failure during Ramadan.
The holy month of Ramadan is the 9th month of the Islamic calendar. Ramadan fasting is considered one of the 5 fundamental pillars of the Islamic religion. Most Muslims worldwide voluntarily abstain from any food, drink or oral medications between dawn and sunset during this holy month. Although patients diagnosed with chronic illnesses are exempt from fasting based on religious dictates/principles, most patients voluntarily choose to fast.1 During this period, it is observed that the dietary habits and daily lifestyle of an individual undergo significant alterations in terms of the daily caloric intake obtained from 2 meals eaten during the night, and this is associated with changes in sleeping patterns.1,2 Several reports have shown that patients with cardiovascular diseases such as coronary artery disease , hypertension, and atrial fibrillation can safely fast without a consequent risk of the development of acute cardiac events.3-5 Additionally, a few studies have reported that patients diagnosed with acute heart failure remain stable with no deterioration following fasting for religious purposes.6,7 However, no prospective study has investigated the effect of Ramadan fasting on the symptoms of chronic heart failure with a reduced ejection fraction (HFrEF). We hypothesized that in patients diagnosed with chronic HFrEF, Ramadan fasting is safe and is not associated with significant changes in the symptoms of HF or an increased risk of cardiac events.
Methods
Study design and population
We conducted a prospective observational study carried out in the central province of Saudi Arabia between February and July 2017. We enrolled 272 patients diagnosed with chronic HFrEF who had been regularly followed-up at HF clinics. Exclusion criteria were: patients newly diagnosed with HFrEF (diagnosed <3 months prior to the enrollment to the study), those with advanced HF (at least 2 emergency department visits/hospitalization in the last 3 months prior to enrollment or 3 emergency department visits 6 months prior to enrollment), and those diagnosed with left ventricular ejection fraction (LVEF) ≥40%.8 All patients provided voluntary consent to participate in the study after receiving adequate information on the aims and methods of the research that were to be used. The study protocol was duly approved by the institutional Board and the regional Ethical committee.
Demographic data collection
Basic demographic variables/data were obtained from patients during the interview/ history-taking at the HF outpatient clinics. The following information was documented: medical history of hypertension, dyslipidemia, diabetes, smoking status, family history of premature coronary artery disease, history of previous coronary revascularization procedure(s), current medication intake, HF symptoms based on the New York Heart Association (NYHA) Functional Classification, and the occurrence of palpitations and/or chest pain.9
Furthermore, we obtained information from patients’ medical records regarding the etiology of HF (ischemic or non-ischemic), any previous history of the placement of cardiac resynchronization therapy (CRT) and/or an implantable cardioverter-defibrillator (ICD).
Ischemic cardiomyopathy was defined as the presence of ≥70% stenosis of the epicardial coronary arteries with a history of myocardial infarction or the occurrence of coronary revascularization procedures.10
Results of electrocardiography, echocardiography, and laboratory investigations
We performed electrocardiographic examination to assess the heart rhythm and to determine the presence of a left bundle branch block. We performed echocardiographic examination to assess the left ventricular size and EF, the grade of diastolic dysfunction, to detect the presence of any valvular heart disease, and to measure the pulmonary artery systolic pressure. We also performed laboratory investigations to assess the levels of the N-terminal pro-brain natriuretic peptide, hemoglobin, and the lipid profile.
Follow-up of heart failure symptoms
Follow-up of the clinical data was performed by telephonic interviews during Ramadan and the month preceding and following this period. These interviews were conducted by a trained physician who obtained the following information: NYHA functional classification of dyspnea, any changes in HF symptoms, medication and diet adherence, and episodes of acute HF requiring emergency department visits or hospital admission. Patients considered to be drug non-adherent if the taken pills were less than 80% of the total prescribed HF pills for more than 7 days.11 Furthermore, the non-adherence to diet was defined as non-compliance with salt and fluid restriction as recommended by the health care provider for more than 7 days.
Statistical analysis
Categorical variables were expressed as frequencies, and quantitative variables were expressed as an±standard deviation. A 2-sample t-test was used to analyze normally distributed continuous variables, while the chi-squared test was used for categorical variables to compare the NYHA classifications (prior to and during fasting), the echocardiographic and electrocardiographic data, and the compliance to medications between the fasting and the non-fasting groups. The same variables were compared between the stable and the unstable groups using the same model. Dependent t-test analysis was used to compare the NYHA classifications of the same patient prior to and during fasting. A p-value of <0.05 was considered statistically significant. All statistical analyses were performed using the Statistical Package for the Social Science (SPSS) software version 19.0 (IBM Corp., Armonk, NY, USA).
Results
Clinical characteristics
We enrolled 272 patients in the study. However, 23 were excluded, because it was not possible to follow up with these individuals. Out of the 249 patients who completed the follow-up, 227 (91%) patients undertook a fast for the entire month, whereas 22 (9%) either could not fast or discontinued fasting. Baseline clinical characteristics of patients (fasting vs. the non-fasting group) are shown in Table 1.
Table 1.
Baseline characteristics of patients enrolled in the study and an intergroup comparison between the Ramadan fasting and the non-fasting groups.
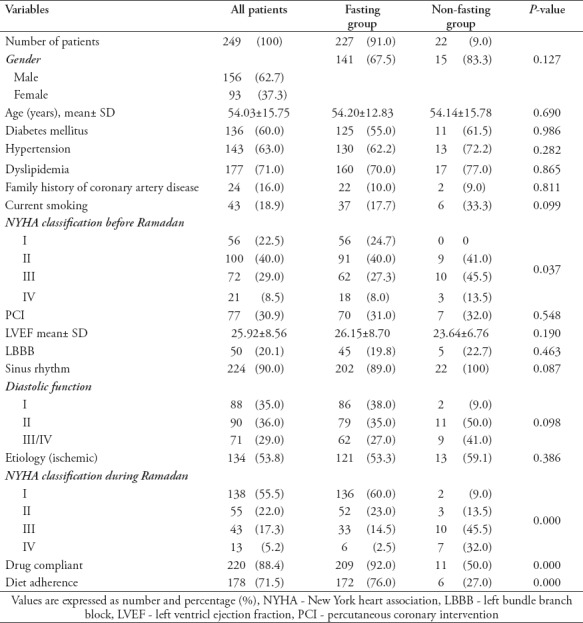
The non-fasting group, comprising 22 (9%) patients, showed a higher statistically significant NYHA functional classification (2.7±0.7 vs. 2.2±0.9, p<0.0001), a lower adherence to drugs administered for HF (50% vs. 92%, p<0.0001) and to a strict diet (27% vs. 76%, p<0.0001), when compared to the fasting group. Other baseline characteristics did not show statistically significant intergroup differences (Table 1).
Changes in symptoms observed during Ramadan
During Ramadan, 209 (92%) patients remained stable (either showed no changes or showed an improvement in their NYHA functional classification), whereas 18 (8%) showed the onset of hemodynamic instability (worsening of HF symptoms) with a mean NYHA functional classification of 1.46±0.7 vs. 3.22±0.55 (p<0.0001). No statistically significant intergroup differences were noted in the NYHA functional classification prior to Ramadan (Table 2).
Table 2.
Difference between patients who had worsened symptoms vs patients with no change or improving dyspnea.
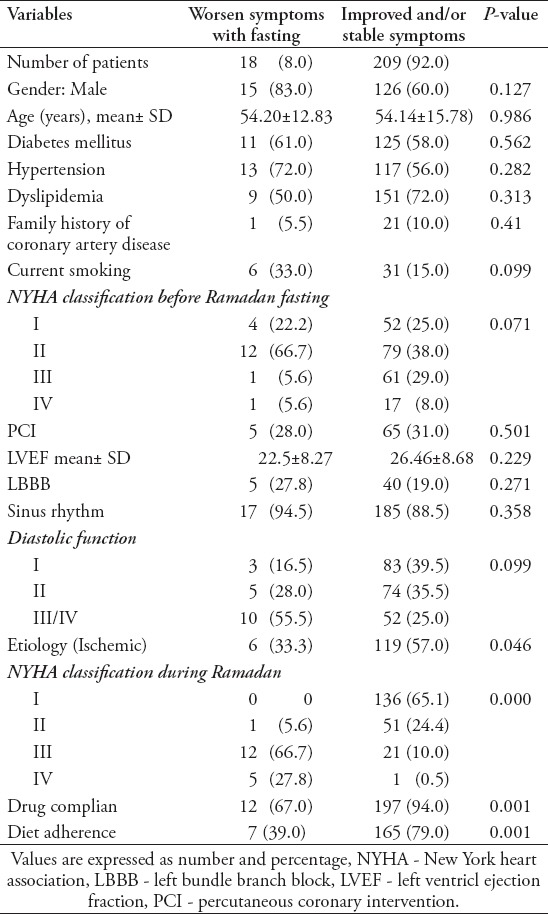
Patients with symptoms that were getting worse showed significantly less adherence to drugs administered to treat HF (67% vs. 94%, p<0.0001) and a strict diet (39% vs. 79%, p<0.0001) during Ramadan, and a lower likelihood for ischemic cardiomyopathy to be the underlying etiology of HF (33% vs. 57%, p=0.046). The other baseline characteristics did not show statistically significant intergroup differences (Table 2).
Dependent t-test analysis, which includes all patients, showed that the NYHA functional classification grades observed prior to Ramadan were significantly higher than those observed during Ramadan (2.19±0.9 vs. 1.6±0.8, t-value= 8.5, p<0.0001) (Figure 1).
Figure 1.
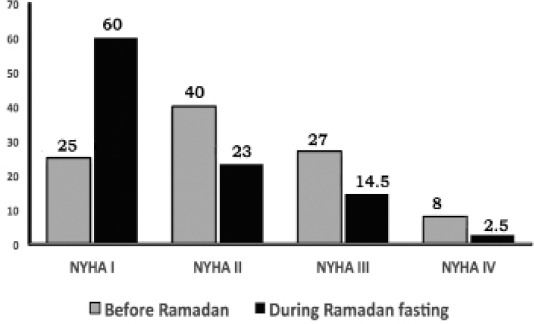
The New York heart association (NYHA) before Ramadan and during the fasting month
Discussion
The effect of Ramadan fasting on HF symptoms in patients with HFrEF was investigated. The NYHA functional classification improved or remained unchanged in 92% of patients who undertook a fast during Ramadan. Furthermore, we observed that patients who were experiencing deteriorating HF symptoms showed statistically significant non-adherence to medications, and/or a lower likelihood of adhering to a strictly controlled diet prescribed for HF patients.
Ramadan fasting significantly affects the lifestyle of individuals, secondary to the reduced frequency of meals and the consequent consumption of larger amounts of calories overnight. Notably, the difficulty in maintaining 8 to 12 hour dosing intervals for several medications administered during this month may cause variable therapeutic effects in patients due to unpredictable pharmacodynamics of medications with shorter intervals.11,12
It is noteworthy that hospitalized patients with decompensated HF showed a 12-month all-cause mortality rate of approximately 17% and re-hospitalization rate of approximately 44%.13 Multiple factors are known to trigger acute HF symptoms such as the non-adherence to drugs/diet, acute coronary syndrome, infection, and/or tachyarrythmias.14 We observed that the non-adherence to drugs/diet was the most important factor precipitating decompensated chronic HF, which necessitated re-hospitalization in patients who undertook a fast during Ramadan.
Although intermittent fasting over a period of several days and alternate-day fasting result in the improvement of cardiovascular health, a few reports have suggested that skipping meals or that the consumption of a large single meal per day worsens the morning glucose tolerance and lipid profile, when compared to an isocaloric diet distributed across 3 meals.15-18
Several studies investigated the relationship between Islamic fasting and cardiovascular diseases. Kul et al19 performed a meta-analysis of 30 studies and reported that Ramadan fasting demonstrated a positive effect on cardiovascular risk factors. Furthermore, Al Suwaidi J et al4 reported no significant detrimental effects in patients with stable cardiovascular diseases during Ramadan fasting. However, in contrast to our study, this study defined HF based on the clinical diagnosis; thus, most enrolled patients showed heart failure with a preserved ejection fraction (HFpEF) (mean EF=51%). Al Suwaidi J et al7 also performed a retrospective analysis, which showed that the number of hospitalization required in patients with congestive HF during Ramadan fasting was not significantly different when compared to those required in patients during the non-fasting months. Similarly, a recent report by Salam AM et al6 showed that patients presenting with acute HF during Ramadan demonstrated significantly less symptoms, although immediate or long-term outcomes did not show statistically significant differences. Interestingly, this study reported an observation that differed from that of our study. They observed that ischemic HF showed a significant worsening of symptoms during Ramadan than that observed with non-ischemic cardiomyopathy. These discrepancies might be explained by the difference in the patient inclusion criteria employed by the studies (clinical diagnosis of HF vs. the use of HFrEF as a diagnostic criterion employed in our study).
This study highlights the importance of patient education regarding diet/drug control to reduce the occurrence of decompensated HF during Ramadan fasting. Additionally, physicians should consider alterations in drug regimens such as institut ing once-daily dosing to replace multiple-daily dosing of medications.
Study limitations
1) Climatic conditions, and therefore, fasting hours differ between regions (15-16 hours in our study). Therefore, our results are not generalizable to regions with a cold climate or a different season; 2) A longer follow-up period is necessary to study the outcome of fasting on hospitalization occurrences or death; 3) Patients with an EF ≥40% were excluded from our study, thus, the results of our study may not be applicable to patients with HFpEF; 4) The number of patients included in the study was small. Therefore, further multi-regional studies involving a larger sample size, and long-term follow-up are warranted to analyze and conclusively establish the effect of fasting in different geographical locations (variable climatic conditions) in patients with HF.
In conclusion, Ramadan fasting is considered safe in most patients with HFrEF. Appropriate patient education explaining the importance of medication compliance for drugs administered for the management of HF and the need for a low-sodium and fluid-restricted diet needs to be emphasized prior to undertaking Ramadan fasting during the Holy month.
Footnotes
www.smj.org.sa.
Saudi Medical Journal Online features
-
*
Instructions to Authors
-
*
Uniform Requirements
-
*
STARD
-
*
Free access to the Journal’s Current issue
-
*
Future Contents
-
*
Advertising and Subscription Information
All Subscribers have access to full text articles in HTML and PDF format. Abstracts and Editorials are available to all Online Guests free of charge.
References
- 1.Chamsi-Pasha M, Chamsi-Pasha H. The cardiac patient in Ramadan. Avicenna J Med. 2016;6:33–38. doi: 10.4103/2231-0770.179547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chamsi-Pasha H. Islam and the cardiovascular patient- Pragmatism in practice. Br J Cardiol. 2013;20:1–2. [Google Scholar]
- 3.Salim I, Al Suwaidi J, Ghadban W, Alkilani H, Salam AM. Impact of religious Ramadan fasting on cardiovascular disease: A systematic review of the literature. Curr Med Res Opin. 2013;29:343–354. doi: 10.1185/03007995.2013.774270. [DOI] [PubMed] [Google Scholar]
- 4.Al Suwaidi J, Zubaid M, Al-Mahmeed WA, Al-Rashdan I, Amin H, Bener A, et al. Impact of fasting in Ramadan in patients with cardiac disease. Saudi Med J. 2005;26:1579–1583. [PubMed] [Google Scholar]
- 5.Habbal R, Azzouzi L, Adnan K, Tahiri A, Chraibi N. Variations of blood pressure during the month of Ramadan. Arch Mal Coeur Vaiss. 1998;91:995–998. [PubMed] [Google Scholar]
- 6.Salam AM, Sulaiman K, Alsheikh-Ali AA, Singh R, Asaad N, Al-Qahtani A, et al. Acute heart failure presentations and outcomes during the fasting month of Ramadan: an observational report from seven middle eastern countries. Curr Med Res Opin. 2017;34:237–245. doi: 10.1080/03007995.2017.1376629. [DOI] [PubMed] [Google Scholar]
- 7.Al Suwaidi J, Bener A, Hajar HA, Numan MT. Does hospitalization for congestive heart failure occur more frequently in Ramadan: A population-based study (1991-2001) Int J Cardiol. 2004;96:217–221. doi: 10.1016/j.ijcard.2003.06.018. [DOI] [PubMed] [Google Scholar]
- 8.Stevenson LW, Pagani FD, Young JB, Jessup M, Miller L, Kormos RL, et al. INTERMACS profiles of advanced heart failure: the current picture. J Heart Lung Transplant. 2009;28:535–541. doi: 10.1016/j.healun.2009.02.015. [DOI] [PubMed] [Google Scholar]
- 9.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Colvin MM, et al. 2017 ACC/AHA/HFSA Focused update of the 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology/American Heart association task force on clinical practice guidelines and the heart Failure Society of America. Circulation. 2017;136:137–161. doi: 10.1161/CIR.0000000000000509. [DOI] [PubMed] [Google Scholar]
- 10.Felker GM, Shaw LK, O'Connor CM. A standardized definition of ischemic cardiomyopathy for use in clinical research. J Am Coll Cardiol. 2002;39:210–218. doi: 10.1016/s0735-1097(01)01738-7. [DOI] [PubMed] [Google Scholar]
- 11.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 12.Smith DA, Beaumont K, Maurer TS, Di L. Relevance of Half-Life in Drug Design. J Med Chem. 2017 Nov 17; doi: 10.1021/acs.jmedchem.7b00969. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 13.Maggioni AP, Dahlstrom U, Filippatos G, Chioncel O, Crespo Leiro M, Drozdz J, et al. EURObservational Research Programme: regional differences and 1-year follow-up results of the Heart Failure Pilot Survey (ESC-HF Pilot) Eur J Heart Fail. 2013;15:808–817. doi: 10.1093/eurjhf/hft050. [DOI] [PubMed] [Google Scholar]
- 14.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Eur J Heart Fail. 2016;18:891–975. doi: 10.1002/ejhf.592. [DOI] [PubMed] [Google Scholar]
- 15.Schless GL, Duncan GG. The beneficial effect of intermittent total fasts on the glucose tolerance in obese diabetic patients. Metabolism. 1966;15:98–102. doi: 10.1016/0026-0495(66)90029-1. [DOI] [PubMed] [Google Scholar]
- 16.Pedersen CR, Hagemann I, Bock T, Buschard K. Intermittent feeding and fasting reduces diabetes incidence in BB rats. Autoimmunity. 1999;30:243–250. doi: 10.3109/08916939908993805. [DOI] [PubMed] [Google Scholar]
- 17.Carlson O, Martin B, Stote KS, Golden E, Maudsley S, Najjar SS, et al. Impact of reduced meal frequency without caloric restriction on glucose regulation in healthy, normal weight middle-aged men and women. Metabolism. 2007;56:1729–1734. doi: 10.1016/j.metabol.2007.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Farshchi HR, Taylor MA, Macdonald IA. Deleterious effects of omitting breakfast on insulin sensitivity and fasting lipid profiles in healthy lean women. Am J Clin Nutr. 2005;81:388–396. doi: 10.1093/ajcn.81.2.388. [DOI] [PubMed] [Google Scholar]
- 19.Kul S, Savas E, Öztürk ZA, Karadag G. Does Ramadan fasting alter body weight and blood lipids and fasting blood glucose in a healthy population?A meta-analysis. J Relig Health. 2014;53:929–942. doi: 10.1007/s10943-013-9687-0. [DOI] [PubMed] [Google Scholar]


