Abstract
Botulinum toxin A (BTA) injections into lacrimal gland are being used for refractory epiphora due to intractable lacrimal disorders with success rates reported from 18% to 86%. Most common side effects are transient ptosis and diplopia. We report a case of a 59-year-old female injected with 2.5 units of BTA injection in each lacrimal gland for functional epiphora. The patient had a history of herpes simplex viral keratitis that was quiescent for more than 2 years. After 3 weeks, she developed reactivation of viral keratitis bilaterally, which was successfully managed with antivirals and topical steroids. Reactivation of quiescent herpes simplex keratitis is a possibility after lacrimal gland BTA and caution should be exercised in such cases.
Keywords: Botulinum toxin, functional epiphora, herpes simplex keratitis, lacrimal gland, reactivation
Lacrimal gland botulinum toxin A (BTA) injections successfully alleviate epiphora with documented improvement in Munk scores.[1,2,3] The toxin inhibits release of acetylcholine in all parasympathetic and cholinergic postganglionic sympathetic neurons, resulting in reduced tear secretion.[4] Injections are generally well tolerated and the side effects reported after this procedure are transient ptosis (7–25%) and diplopia (7%) in a few cases.[3] Other systemic side effects include an influenza-like illness and, rarely, weakness of distant muscles or generalized weakness, possibly due to the toxin spreading in the blood.[5] Two cases of primary episodes of cutaneous herpes zoster have been reported after BTA injections into forehead and lateral periorbital areas.[6] No case of ocular herpes reactivation postlacrimal gland BTA injection has been reported in the past. We hereby describe an unusual case of bilateral reactivation of herpes simplex keratitis following lacrimal gland BTA injections.
Case Report
A 59-year-old female had complaints of watering and discomfort in both the eyes for 6 months. She had a past history of resolved bilateral herpes simplex viral (HSV) stromal keratitis (maintained on prophylactic dose of oral valacyclovir 500 mg once daily) that occurred 2 years ago. Slit-lamp examination showed residual corneal scars. Grade 1 punctal stenosis in both eyes was successfully managed with punctal dilatation and monocanalicular intubation (Aurostent, Aurolab, India). Stents were removed after 4 weeks; with good anatomical and functional outcome evident by a freely patent lacrimal drainage on irrigation and 90% reduction in epiphora. Five months later, she had recurrence of watering in both the eyes (bilateral Grade 3 Munk score). Grade 1 fluorescein dye disappearance test with freely patent lacrimal drainage system supported the diagnosis of functional epiphora. Two and a half units of BTA were injected transconjunctivally into the palpebral lobe of each lacrimal gland under topical anesthesia. Symptomatic improvement (90% reduction in epiphora) was noted at 1 week but she developed ptosis in the right eye following the injection [Fig. 1a]. She was counseled regarding the eventual spontaneous recovery of ptosis. Schirmer test without anesthesia was 20 mm and 14 mm in both eyes pre- and postinjection, respectively.
Figure 1.
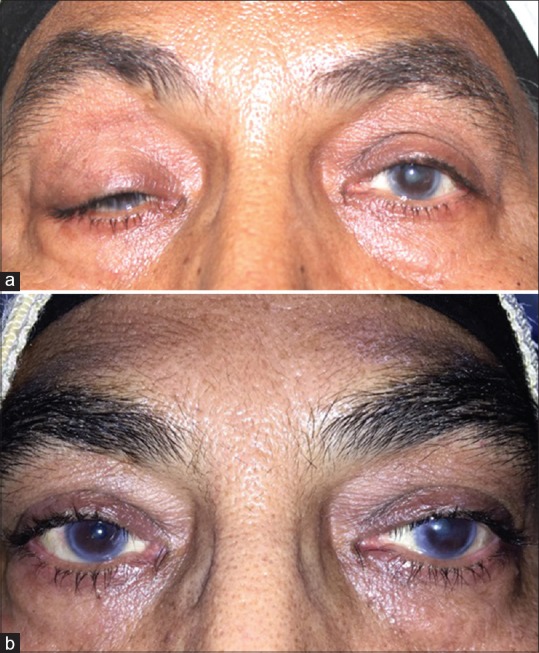
(a) Ptosis of right upper lid 1 week after botulinum toxin A injection into the lacrimal glands for functional epiphora. (b) Complete resolution of ptosis of right upper lid at 4 weeks
Three weeks later, she developed redness, pain, and foreign body sensation in both the eyes. Clinical examination revealed bilateral circumciliary congestion with large epithelial defects and stromal edema [Fig. 2a–d] suggesting a recurrence of HSV stromal keratitis.
Figure 2.
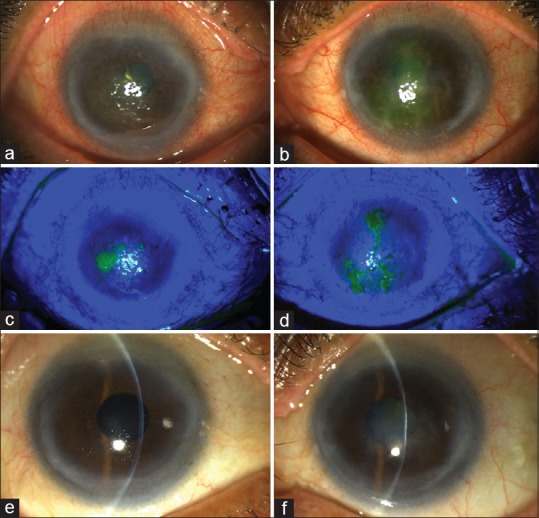
Slit-lamp photograph after reactivation of herpes simplex viral keratitis (large dendritic ulcers), 3 weeks after botulinum toxin A; (a and b) without and (c and d) with fluorescein stain in both eyes, following botulinum toxin A injection. (e and f) Slit-lamp photograph of right and left eyes showing resolution of keratitis within 4 weeks of treatment
Systemic immunosuppression was excluded after physician consultation and appropriate investigations. Patient had stopped oral valacyclovir prophylaxis after stent removal. Topical antiviral (ganciclovir 0.15% gel) and frequent lubricants were started and oral valacyclovir 500 mg was prescribed thrice daily. One week later, after resolution of epithelial defects, topical 1% prednisolone acetate was started at four times daily and tapered over 4 weeks. Complete resolution of viral keratitis and ptosis occurred within a month [Figs. 1b and 2e, f]. Thereafter, she was on a maintenance dose of once daily oral valacyclovir (500 mg) and topical lubricants.
Discussion
This case report describes a reactivation of HSV stromal keratitis after lacrimal gland BTA injection for functional epiphora and highlights the need for oral antiviral prophylaxis before BTA injections.
HSV 1 remains latent in the sensory and autonomic neurons after ocular infection. HSV reactivation is thought to be multi-factorial. According to the Herpetic Eye Disease Study, age, gender, ethnicity, history of epithelial keratitis or of nonocular HSV infection, exogenous catalysts, and psychogenic profile were not significantly associated with recurrences.[7] On the contrary, fever, exposure to wind, sunburn, trauma, and surgical manipulation of the trigeminal ganglion have been implicated in its recurrence by another study.[8] In a report, two patients developed facial herpes zoster along the first branch of trigeminal nerve that erupted soon after cosmetic treatment with BTA without any prior history of the disease.[6] The patients described in that report bring to light the possibility that BTA injections may act as a trigger to reactivate the varicella zoster virus. The exact mechanism is unknown although the role of mechanical trauma and local inflammation was postulated in reactivating varicella infection.
Although the same surgeon has injected the same dose in lacrimal glands on both the sides, painlessly, severe ptosis developed in one eye, maybe due to toxin diffusion into levator muscle. As the patient was very apprehensive regarding the ptosis, this might have induced psychogenic stress, which in turn reactivated the virus on both sides. Another possibility is surgical stress and local inflammation in periocular region which could have altered the local immune response leading to bilateral reactivation of this latent virus. The temporal sequence of recurrence of keratitis postocular intervention can be an association only. Careful probing did not reveal any history of factors reported for HSV recurrence in the current case; thus, this association cannot be purely coincidental. The mentioned contra-indications to the use of BTA are in patients afflicted with a preexisting motor neuron disease, myasthenia gravis, Eaton–Lambert syndrome, neuropathies, psychological instability, history of reaction to toxin or albumin, pregnancy and lactating females, certain drugs, and infection at the injection site.[9] Till date, BTA has not been implicated as a potential risk factor for HSV reactivation. However, based on a single case report, we cannot label patients with quiescent herpes viral keratitis as a contraindication for BTA use. In our case, it seemed that BTA had an association with the recurrence of HSV stromal keratitis although the exact mechanism is not known.
Conclusion
We recommend that caution should definitely be exercised in all cases of resolved herpes viral keratitis undergoing BTA injections, in the form of preinjection patient counseling and appropriate antiviral prophylaxis in such cases.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kaynak P, Karabulut GO, Ozturker C, Fazil K, Arat YO, Perente I, et al. Comparison of botulinum toxin-A injection in lacrimal gland and conjunctivodacryocystorhinostomy for treatment of epiphora due to proximal lacrimal system obstruction. Eye (Lond) 2016;30:1056–62. doi: 10.1038/eye.2016.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ziahosseini K, Al-Abbadi Z, Malhotra R. Botulinum toxin injection for the treatment of epiphora in lacrimal outflow obstruction. Eye (Lond) 2015;29:656–61. doi: 10.1038/eye.2015.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh S, Ali MJ, Paulsen F. A review on use of botulinum toxin for intractable lacrimal drainage disorders. EyInt Ophthalmol. 2017 doi: 10.1007/s10792-017-0661-9. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Münchau A, Bhatia KP. Uses of botulinum toxin injection in medicine today. BMJ. 2000;320:161–5. doi: 10.1136/bmj.320.7228.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhatia KP, Münchau A, Thompson PD, Houser M, Chauhan VS, Hutchinson M, et al. Generalised muscular weakness after botulinum toxin injections for dystonia: A report of three cases. J Neurol Neurosurg Psychiatry. 1999;67:90–3. doi: 10.1136/jnnp.67.1.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Graber EM, Dover JS, Arndt KA. Two cases of herpes zoster appearing after botulinum toxin type a injections. J Clin Aesthet Dermatol. 2011;4:49–51. [PMC free article] [PubMed] [Google Scholar]
- 7.Predictors of recurrent herpes simplex virus keratitis. Herpetic Eye Disease Study Group. Cornea. 2001;20:123–8. doi: 10.1097/00003226-200103000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Toma HS, Murina AT, Areaux RG, Jr, Neumann DM, Bhattacharjee PS, Foster TP. Ocular HSV-1 latency, reactivation and recurrent disease. Semin Ophthalmol. 2008;23:249–73. doi: 10.1080/08820530802111085. [DOI] [PubMed] [Google Scholar]
- 9.Naik MN, Soparkar CN, Murthy R, Honavar SG. Botulinum toxin in ophthalmic plastic surgery. Indian J Ophthalmol. 2005;53:279–88. doi: 10.4103/0301-4738.18915. [DOI] [PubMed] [Google Scholar]


