Abstract
Calcinosis cutis is a rare metabolic disorder characterized by cutaneous and subcutaneous deposition of insoluble calcium salts. Ocular adnexal involvement is uncommon but mostly seen in males and in the upper eyelid. Solitary lesions are more common than multiple. The treatment of choice is excision biopsy. Histopathological examination provides a definitive diagnosis. Directed systemic investigations help to rule out underlying pathologies and aids further management. The present case reports the punctal and peripunctal involvement in a case of ocular adnexal calcinosis cutis.
Keywords: Calcinosis cutis, lacrimal, punctum, peripunctal
Calcinosis cutis is a rare metabolic disorder with deposition of insoluble calcium salts in cutaneous and subcutaneous tissues.[1,2] It is subdivided into five types: metastatic calcinosis, dystrophic calcinosis, iatrogenic calcinosis, calciphylaxis, and subepidermal or idiopathic calcinosis.[1,2] Ocular adnexal involvement has been reported in 53 cases so far, and the lesions were found to involve the upper eyelid in 63% of cases, the medial canthus in 28%, and the lower eyelid in 9% of cases.[3] The present case describes the punctal and peripunctal involvement in a case of ocular adnexal calcinosis cutis and its management.
Case Report
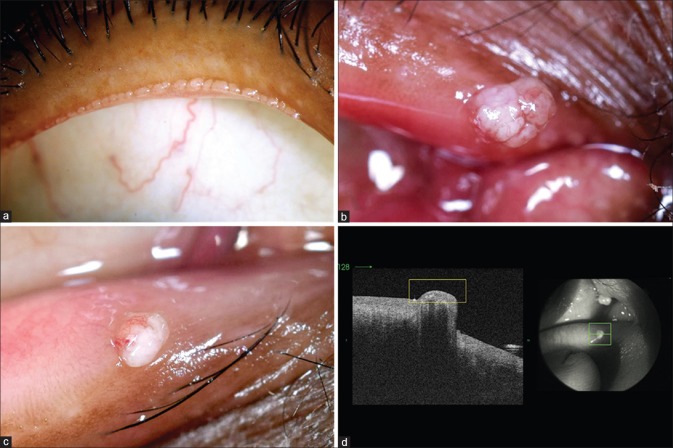
An Indian male, aged 44 years, presented with complaints of right eye upper and lower eyelid lesions, more prominent on the medial side of 1-year duration. The lesions were associated with epiphora without discharge and occasional foreign body sensation. The patient had a past medical history of well-controlled Type II diabetes mellitus of 5-year duration. There were no systemic symptoms or history of any other systemic disorders or eyelid trauma. On examination, the best-corrected visual acuity was 20/20 with normal anterior and posterior segment examinations in both the eyes. Eyelid evaluation showed bilateral numerous pinkish white lesions along the posterior eyelid margins, more in the upper eyelids [Fig. 1a]. The right upper and lower punctal and peripunctal regions showed large (2 mm × 2 mm) keratinized, hard, minimally mobile, pinkish white, papillomatous-like lesion covering the entire punctal and peripunctal regions [Fig. 1b and c]. Fourier domain anterior segment ocular coherence tomography showed elevated lesions completely covering the underlying punctal orifice with a patent proximal vertical canaliculus [Fig. 1d]. The patient underwent excision biopsy of the lesions. Intraoperatively, the eyelid margin lesions could be easily scraped off the surface, and the punctal lesions were gently lifted followed by a shave excision. Following excision, the underlying puncta and the lacrimal drainage system was normal, and the lesion appeared to be arising from the peripunctal rim.
Figure 1.
Slit-lamp photograph of the right upper eyelid in diffuse illumination showing the numerous whitish lesions adjacent to the posterior sharp border (a). External photographs of the medial end of the right upper (b) and lower eyelids (c) demonstrating the papillomatous pinkish white lesion covering the entire punctal orifices. Fourier domain anterior segment ocular coherence tomography of the right lower eyelid, showing the elevated lesion covering the underlying patent punctal orifice (d)
Histopathological evaluation showed the lesion to be lined by stratified squamous epithelium with elongated rete ridges extending downward with no evidence of dysplasia [Fig. 2a]. The subepithelial stroma showed prominent calcification with a sparsely cellular fibrocollagenous stroma [Fig. 2a and b]. There was no evidence of inflammation or malignancy. Histological features were consistent with a diagnosis of calcinosis cutis.
Figure 2.
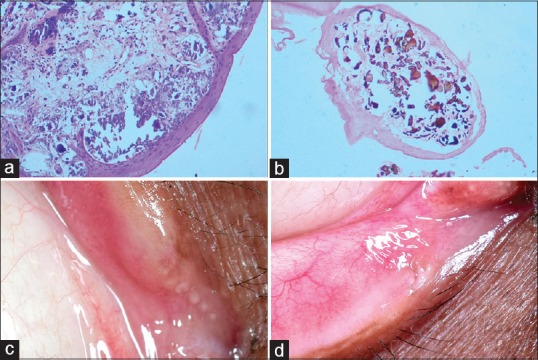
Microphotograph showing the lesion lined by stratified squamous epithelium with rete ridges and purplish calcium deposits in the stroma (H and E, ×100, [a]). Microphotograph with von Kossa stain confirming the presence of calcium deposits in the stroma (von Kossa, ×100 [b]). Postoperative external photographs of the right upper eyelid (c) and lower eyelid (d) demonstrating no recurrence of the lesions in the punctal and peripunctal regions. Compare it with images in Figure 1b and c
The patient was extensively investigated systemically. There was no evidence of any subepidermal calcific nodules elsewhere, and the bone joints were normal. The renal function tests including glomerular filtration rates were normal. The complete hemogram and liver function test were normal. Serum calcium and parathyroid hormone levels were normal; however, serum phosphorus was raised. Serum levels of Vitamin D and serum chloride were low. The patient is currently under endocrinology and nephrology care. Postoperative follow-up at 3 months showed no recurrence of the lesions and the patient was asymptomatic [Fig. 2c and d].
Discussion
Of the five types of calcinosis cutis, dystrophic calcification is the most common and is seen associated with underlying tissue damage or connective tissue disorders. Metastatic calcification is secondary to abnormalities of calcium and phosphate metabolism. Iatrogenic variant occurs following intravenous calcium or para-aminosalicylic acid administration, whereas calciphylaxis refers to cutaneous small vessel affection and subsequent ischemia. Idiopathic calcinosis cutis includes tumoral calcinosis which predominantly involves the joints and ocular involvement is rare,[4] and subepidermal calcinosis involves mostly the head and neck region including the ocular adnexa.[3,5] Serum calcium and phosphorus levels are normal in dystrophic calcinosis and deranged in metastatic variants and calciphylaxis. Idiopathic variants may or may not show such serum abnormalities.[1,2]
Ocular adnexal involvement by idiopathic calcinosis cutis or subepidermal calcinosis presents as whitish firm lesion which can be mistaken for more common eyelid lesions such as papilloma, molluscum contagiosum, seborrheic keratosis, or epidermoid cysts. Definitive diagnosis is usually arrived after a histopathological examination since calcinosis cutis is uncommon without much of distinctive clinical features. Ocular adnexal calcinosis cutis is more commonly documented in young, non-Caucasian males and commonly involves the upper eyelid (63%, n = 53).[3] Unilateral single lesions (82%, n = 53) are more common than multiple lesions or bilateral involvement.[3]
Histopathological examination demonstrates basophilic amorphous calcium deposits in the subepithelial stroma which can be confirmed by von Kossa stain.[1,3,4] The lining stratified squamous epithelium may occasionally show focal hyperplasia. Lymphoplasmacytic inflammatory infiltrates may or may not be present. Surgical excision is usually the procedure of choice, and incomplete resections have been reported to cause recurrences.[3] Biochemical abnormalities, if any, need to be corrected. Other modalities of management which have not gained popularity include corticosteroid therapy, immunoglobulin therapy, and carbon dioxide lasers.[2,3]
Conclusion
In summary, we describe a case of ocular adnexal calcinosis cutis with additional involvement of the punctal and peripunctal regions. Although rare, this should be kept in the differential diagnosis of multiple idiopathic lesions on the eyelid.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Dr. Ali receives royalties from Springer for the textbook “Principles and Practice of Lacrimal Surgery” and the treatise “Atlas of Lacrimal Drainage Disorders”. Other authors have none.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Reiter N, El-Shabrawi L, Leinweber B, Berghold A, Aberer E. Calcinosis cutis: Part I. Diagnostic pathway. J Am Acad Dermatol. 2011;65:1–12. doi: 10.1016/j.jaad.2010.08.038. [DOI] [PubMed] [Google Scholar]
- 2.Reiter N, El-Shabrawi L, Leinweber B, Berghold A, Aberer E. Calcinosis cutis: Part II. Treatment options. J Am Acad Dermatol. 2011;65:15–22. doi: 10.1016/j.jaad.2010.08.039. [DOI] [PubMed] [Google Scholar]
- 3.Khine KT, Shi DS, Bernhisel A, Gertsch KR, Mamalis N, Patel BCK, et al. Subepidermal calcinosis in the ocular adnexa: A Systematic review. Ophthal Plast Reconstr Surg. 2017 doi: 10.1097/IOP.0000000000000936. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Ghanchi F, Ramsay A, Coupland S, Barr D, Lee WR. Ocular tumoral calcinosis. A clinicopathological study. Arch Ophthalmol. 1996;114:341–5. doi: 10.1001/archopht.1996.01100130337022. [DOI] [PubMed] [Google Scholar]
- 5.Bruns DE, Boskey AL, Lieb W, Conway BP, Savory J, Wills MR, et al. Tumoral calcinosis: Seasonal biochemical studies and chemical studies of eyelid lesion. Clin Chem. 1989;35:183–5. [PubMed] [Google Scholar]