Abstract
Introduction
The extent of peripheral artery disease (PAD) measured by the ankle-brachial index (ABI) and intima-media thickness (IMT) is correlated with the complexity of coronary artery disease (CAD) in stable angina patients. However, data regarding patients with acute coronary syndromes are still lacking.
Aim
To compare coronary complexity measured by the SYNTAX score in patients with and without PAD presenting with myocardial infarction (MI).
Material and methods
Both ABI and IMT were measured in 101 consecutive patients who underwent primary diagnostic due to MI. Patients were divided into three tertile groups depending on the SYNTAX score (0–4; 5–11; 12 and more points).
Results
Mean ABI in the general population was 0.9 ±0.26, mean IMT was 0.8 ±0.3 mm and mean SYNTAX score was 7.8 ±5.4 points. We found significant correlations between ABI and SYNTAX score (p = 0.01), IMT and SYNTAX score (p < 0.001), and IMT and ABI (p < 0.001). The highest mean values of IMT (p < 0.001) and lowest mean values of ABI (p = 0.015) were found in patients in the highest SYNTAX score group. When analyzing receiver operating characteristics (ROC) curves, IMT had greater specificity and sensitivity than ABI.
Conclusions
Both IMT and ABI are correlated with SYNTAX score (positively for IMT and negatively for ABI values). In our study, IMT was a better predictor of SYNTAX score than ABI. Our study suggests that the higher rate of cardiovascular events in patients with PAD presenting with MI may be partially explained by greater coronary lesion complexity.
Keywords: coronary artery disease, acute coronary syndrome, carotid intima-media thickness, peripheral artery disease, ankle-brachial index, SYNTAX score
Introduction
Peripheral artery disease (PAD) measured by the ankle-brachial index (ABI) is an important marker of cardiovascular mortality and morbidity and is positively associated with the extent of coronary artery disease (CAD) [1, 2]. Most of the events in PAD patients are attributed to coronary atherosclerosis – which means that the cardiovascular risk profile is more pronounced in concomitant CAD and PAD [3–7]. The complexity of CAD may be measured by the Synergy Between PCI With TAXUS and Cardiac Surgery (SYNTAX) score, which is used as a prognostic tool in the short- and long-term risk stratification in patients who underwent coronary intervention [8]. Interestingly, this scoring system has been positively associated with PAD [9, 10]. There is substantial evidence that carotid intima-media thickness (IMT) is, similarly to ABI, associated with SYNTAX score and may be considered as a marker of increased cardiovascular risk [11, 12]. Moreover, IMT is a recommended measure of vascular age, which is usually different from the metric one, and thus may allow one to identify individuals with advanced subclinical atherosclerosis and as such to alternate cardiovascular risk estimates [13]. Measuring IMT and ABI may be an easy method to predict the extent of CAD and possible future cardiac events in patients with stable angina [14]. However, data regarding patients with acute coronary syndromes are still lacking.
Aim
Therefore, we sought to assess whether measuring both IMT and ABI may predict the extent of CAD in patients undergoing primary percutaneous coronary intervention (PCI) due to myocardial infarction (MI).
Material and methods
All data were gathered in a single cardiology center. Both ABI and IMT were measured in 101 consecutive patients who underwent primary PCI due to MI – with ST-segment elevation (STEMI) or without ST-segment elevation (NSTEMI). Patients who died during hospitalization, were hemodynamically unstable, or could not have ABI or IMT measured were excluded. All patients provided written informed consent to participate. The study followed the ethical principles for clinical research based on the Declaration of Helsinki. No funding was used to support this research.
During the hospital stay (more than 3 days after the procedure), after 10 min rest in a horizontal position ABI was measured on the posterior and anterior tibial artery of both legs and the brachial artery of both arms using a volume plethysmograph. ABI was measured twice by two different physicians. The second measurement was taken 5 min after the first one. For the study, the lowest ABI obtained for either side was reported.
To avoid bias in measurements, IMT was assessed by two sonographers who had no knowledge of the results of either the ABI measurements or the IMT measurements of the other physician. Only one certified scanner (VIVID 7 DIMENSION, GE Healthcare, USA) was used. It was equipped with a 7.5-MHz linear array transducer. Patients were examined in the supine position with their heads tilted backward and rotated slightly to expose an area from the clavicle to the angle of the jaw. Firstly, the sonographer localized the carotid artery (CA) and its bifurcation using a transverse scan. After that, the probe was rotated 90° to obtain longitudinal images of the walls of the CA. The IMT was measured 1 cm under the bifurcation. The higher IMT (from the right or left common CA) was taken for the study.
The SYNTAX score was measured by two physicians who were blinded to the results of both IMT and ABI measurements. The score was calculated using the algorithm available on the SYNTAX website [15]. The angiographic films just before stent implantation were used to score the culprit lesion [13].
Patients were stratified into two groups based on ABI (> or ≤ 0.9). In addition, patients were divided into three tertile groups depending on the SYNTAX score – low (0–4 points), medium (5–11 points) and high score (≥ 12 points).
To combine both IMT and ABI we used 4 groups as proposed by Ikeda et al. [16] – group A with IMT < 0.9 mm and ABI ≥ 0.9, group B with IMT < 0.9 mm and ABI < 0.9, group C with IMT ≥ 0.9 mm and ABI ≥ 0.9, group D with IMT ≥ 0.9 mm and ABI < 0.9.
Statistical analysis
All continuous variables are presented as mean with standard deviation (SD). Categorical variables are presented as percentages or number of patients. All variables were tested for normal distribution. For categorical variable comparison we used Fisher or χ2 tests. The Kruskal-Wallis (nonparametric test) test was used to compare multiple groups. To compare continuous variables we used the 2-sample unpaired Student’s t-test (normal distribution) or Mann-Whitney U-test. Correlations were tested using the Spearman rank order test. Two-sided p < 0.05 was considered significant. Receiver operating characteristics (ROC) curve analysis was used to assess the ability of ABI and IMT to predict SYNTAX score ≥ 12 points. Area under the curve (AUC) and confidence intervals (CI) were calculated. The StatSoft Statistica package (version 10, StatSoft Inc., Tulsa, OK, USA) and IBM SPSS version 23 (IBM Corp. in Armonk, NY) were used.
Results
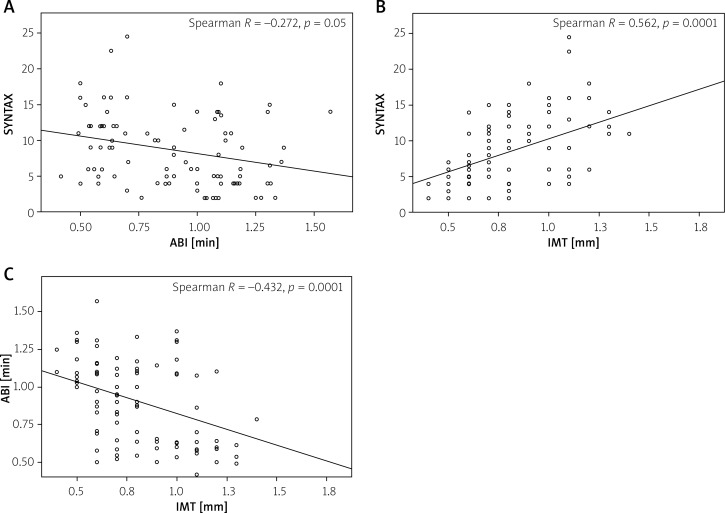
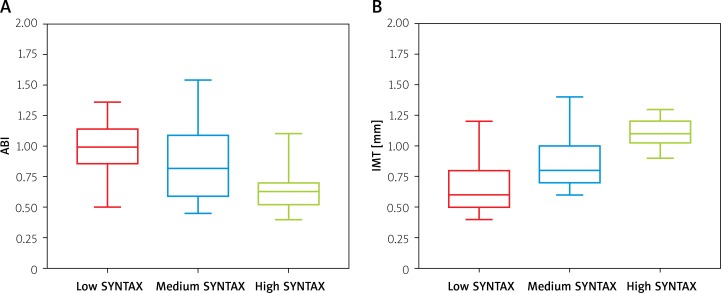
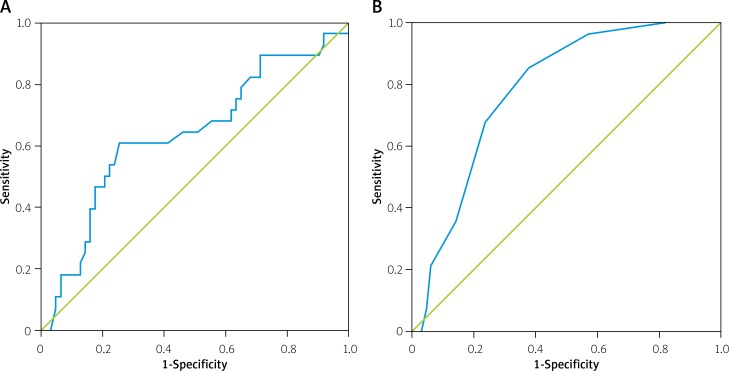
We recruited 101 patients, of whom 56 (55.4%) were males. Mean age was 64.7 ±11.6 years, 53 (52.5%) out of 101 patients had hyperlipidemia, 28 (27.7%) had diabetes, and 24 (23.8%) were smokers. Out of the general population, in 34 (33.7%) patients the left anterior descending artery (LAD) was responsible for MI. The right coronary artery (RCA) was responsible for MI in 36 (35.6%) patients. There were 20 (19.8%) patients with the left circumflex artery (Cx) as the infarct-related artery (IRA). In 1 (1.0%) patient the left main (LM) coronary artery was identified as the infarct-related artery (IRA). Stents were deployed in 87 (86.1%) patients. Mean ABI in the general population was 0.9 ±0.26, mean IMT was 0.8 ±0.3 mm and mean SYNTAX score was 7.8 ±5.4 points. After dividing patients into two ABI and two IMT groups, patients’ characteristics were comparable (Tables I and II). Interestingly, those patients with lower ABI or higher IMT had significantly higher troponin levels on admission. We observed a significant correlation between IMT and SYNTAX score, ABI and SYNTAX score, and ABI and IMT (Figure 1, Tables I and II). When combining both IMT and ABI, the highest mean SYNTAX score was in group D (11.9 ±5.4 points). The mean score was 6.4 ±4.0 for group A; 7.6 ±3.8 for group B; and 11.7 ±4.5 for group C (p < 0.002). Patients with ABI ≥ 0.9 had a lower SYNTAX score and IMT than patients with ABI < 0.9 (7.5 ±4.6 vs. 10.0 ±5.2 points; p < 0.001 and 0.7 ±2.5 mm vs. 0.9 ±2.4 mm; p < 0.001, respectively). Results showing low, intermediate and high SYNTAX scores combined with IMT and ABI are shown in Figure 2. Differences between groups were statistically significant with p < 0.001 for IMT and p = 0.006 for ABI. ROC curves for ABI, IMT and high SYNTAX score (12 points and more) were calculated (Figure 3). For prediction of a high SYNTAX score we achieved 60% sensitivity and 75% specificity with ABI < 0.7 (AUC = 0.637, 95% CI: 0.507–0.768; p = 0.040) and 86% sensitivity and 62% specificity with IMT > 0.75 mm (AUC = 0.796, 95% CI: 0.710–0.883; p < 0.001).
Table I.
Baseline patients’ characteristics according to ankle-brachial index
| Parameter | ABI ≤ 0.9 (n = 45) | ABI > 0.9 (n = 56) | P-value |
|---|---|---|---|
| Age [years] | 63.8 ±10.9 | 65.5 ±12.2 | 0.426 |
| BMI [kg/m2] | 29.3 ±2.8 | 29.0 ±4.3 | 0.607 |
| Gender (male), n (%) | 29 (64.4) | 70 (48.2) | 0.056 |
| Smokers, n (%) | 13 (28.9) | 11 (19.6) | 0.242 |
| Hyperlipidaemia, n (%) | 23 (51.1) | 30 (53.6) | 0.983 |
| Diabetes, n (%) | 14 (31.1) | 14 (25.0) | 0.302 |
| Arterial hypertension, n (%) | 31 (68.9) | 43 (76.8) | 0.879 |
| Previous PCI, n (%) | 13 (28.9) | 13 (23.2) | 0.507 |
| Previous MI, n (%) | 16 (35.6) | 19 (33.9) | 0.626 |
| Troponin cTnT on admission [μg/l] | 2.7 ±5.1 | 0.99 ±1.9 | 0.003 |
| IMT [mm] | 0.93 ±0.25 | 0.69 ±0.24 | < 0.001 |
Values are mean ± standard deviation (SD) or n (%). ABI – ankle-brachial index, BMI – body mass index, IMT – intima-media thickness, MI – myocardial infarction, PCI – percutaneous coronary intervention.
Table II.
Baseline patients’ characteristics according to intima-media thickness
| Parametr | IMT ≤ 0.9 mm (n = 30) | IMT > 0.9 mm (n = 71) | P-value |
|---|---|---|---|
| Age [years] | 68.4 ±10.8 | 63.3 ±11.6 | 0.056 |
| BMI [kg/m2] | 29.2 ±3.4 | 29.1 ±4.0 | 0.862 |
| Gender (male), n (%) | 16 (53.3) | 40 (56.3) | 0.942 |
| Smoker, n (%) | 9 (30.0) | 15 (21.1) | 0.265 |
| Hyperlipidaemia, n (%) | 18 (60.0) | 35 (49.3) | 0.337 |
| Diabetes, n (%) | 11 (36.7) | 17 (23.9) | 0.084 |
| Arterial hypertension, n (%) | 25 (83.3) | 49 (69.0) | 0.103 |
| Previous PCI, n (%) | 9 (30.0) | 17 (23.9) | 0.577 |
| Previous MI, n (%) | 12 (40.0) | 23 (32.4) | 0.592 |
| Troponin cTnT on admission [μg/l] | 2.1 ±2.4 | 1.7 ±4.3 | 0.024 |
| ABI | 0.79 ±0.28 | 0.95 ±0.24 | 0.005 |
Values are mean ± standard deviation (SD) or n (%). ABI – ankle-brachial index, BMI – body mass index, IMT – intima-media thickness, MI – myocardial infarction, PCI – percutaneous coronary intervention.
Figure 1.
Correlations between intima-media thickness (IMT), ankle-brachial index (ABI) and SYNTAX score
Figure 2.
Ankle-brachial index (ABI) (A) and intima-media thickness (IMT) (B) for low (0–4 points), medium (5–11 points) and high SYNTAX score (12 points and more). Means for low SYNTAX score were 1 ±0.2 for ABI and 0.7 ±0.3 mm for IMT; for medium SYNTAX score were 0.9 ±0.3 for ABI and 0.9 ±0.2 mm for IMT; for high SYNTAX score were 0.7 ±0.2 for ABI and 1.1 ±0.1 mm for IMT. Markings on the graphs outside box plots represent outliers. Box shows range from first to third quartile. Whiskers show maximal and minimal non-outlier values. The vertical line in the box plot shows the median. All results were significant with p < 0.001 for IMT and p = 0.006 for ABI
Figure 3.
Receiver operating characteristics (ROC) curves for ankle-brachial index (ABI) (A), intima-media thickness (IMT) (B) and SYNTAX score. A high-risk score was defined as a SYNTAX score of 12 points or more
Discussion
Patients with PAD are known to have a greater plaque burden and inflammatory burden, and worse endothelial function, which may explain the higher frequency cardiovascular events in those patients [17, 18]. SYNTAX score has consistently been shown to be an independent predictor of adverse events such as MI and target-lesion revascularization (TLR), both in short-term and long-term follow-up [19–21]. This score is assessed based on the anatomy of coronary arteries and lesion types; thus predicting the SYNTAX score might be helpful before preparing for elective procedures. Several studies have reported a correlation between IMT or ABI and SYNTAX score [16, 22–25]. However, the majority of them correlated ABI or IMT with SYNTAX score in patients undergoing elective procedures due to stable angina. Thus, the relationship between SYNTAX score and PAD in patients presenting with MI remains widely unexplored. Our study provides some additional insights into CAD complexity as measured by the SYNTAX score in patients presenting with MI and advanced PAD.
One of the main advantages of ABI is its simplicity and high availability. In our study patients with lower ABI had higher a SYNTAX score. This result is consistent with other studies. Sebastianski et al. [10] observed that patients with ABI < 0.9 (PAD group) had about a 70% higher mean SYNTAX score (17.6 points) than patients in the normal ABI group (ABI 1.0 to 1.4). Similarly, Korkmaz et al. [22] assessed 150 patients with non-ST-segment elevation acute coronary syndrome undergoing coronary angiography and correlated ABI with SYNTAX score. They observed the highest SYNTAX score in the PAD group. Likewise, in our study, after dividing patients into SYNTAX tertiles, the lowest ABI was observed in the highest SYNTAX group.
When comparing three groups with low, medium and high SYNTAX scores, we observed a significant difference in IMT. Accordingly, Korkmaz et al. [12] divided patients into two groups with a SYNTAX score < and > 16. Patients with a SYNTAX score > 16 had significantly greater IMT. These results are comparable to other studies where carotid artery remodeling and complex atherosclerotic plaques in carotid arteries were positively associated with atherosclerosis in coronary arteries [26, 27]. Of note, a cardiovascular magnetic resonance study reported that patients with more advanced CAD had a higher prevalence of lipid-rich necrotic core in carotid arteries [28]. Moreover, the study presented by Aslan et al. showed that patients with three-vessel CAD, as compared to one-vessel disease, had the highest carotid stiffness, fibrinogen and hs-CRP levels [6]. Notably, IMT is associated not only with CAD but also with pan-vascular atherosclerosis. Wrotniak et al. in their recent study observed that IMT > 1.3 mm was an independent predictor of multi-territorial atherosclerosis [29].
We evaluated both IMT and ABI to assess whether the combination of these two measurements may predict SYNTAX score as precisely as each modality alone. We used the grouping method proposed by Ikeda et al. [16], who used the definition from the PARTNERs program for ABI [30]. Ikeda et al. reported that the highest mean SYNTAX score was observed in patients with the lowest ABI and highest IMT. Similarly, we found significant differences between groups, and the highest ones were observed between groups A (normal ABI and IMT) and D (low ABI and high IMT), where we noted almost a two-fold difference between the groups.
Our study showed that patients with PAD measured by ABI or IMT had substantially higher troponin levels on admission. Our work adds to the body of findings that patients with PAD have greater myocardium at risk, as patients with higher troponin levels were found to have higher mortality rates [31]. Our findings show that patients with PAD may have more extensive MI, which may be explained by more complex CAD.
Finally, using ROC curves, we confirmed that both IMT and ABI might predict high SYNTAX score, but IMT has greater specificity and sensitivity. These findings are in line with the study from Ikeda et al. [32]. However, that study used automatic carotid IMT measurement and was not limited to patients with MI.
Our study has some limitations. First of all, our design was observational. Moreover, our study population is relatively small, and there was no clinical follow-up. Further, although we found significant differences between SYNTAX score, ABI and IMT, we observed overlap in IMT and ABI between the 3 groups of SYNTAX score. It is highly probable that with a greater study population the overlap could be reduced. Lastly, the SYNTAX score was measured during acute MI although it was created to be used in stable CAD and has some limitations when used in patients with AMI. There are several ways to calculate the SYNTAX score in acute MI [33–35], such as residual SYNTAX score, baseline SYNTAX score (pre-wiring) or measuring the SYNTAX score after wiring IRA. We decided to use the latter method, as it should have given us the nearest possible SYNTAX score not only during the acute phase but also just before acute MI.
Conclusions
Our study showed that both IMT and ABI are correlated with SYNTAX score (positively for IMT and negatively for ABI). We found that combining both IMT and ABI in patients with MI is also feasible to predict the SYNTAX score. In our study, IMT was responsible for better prediction of the SYNTAX score than ABI. Finally, we showed that the correlation between PAD and extent of CAD is not limited to stable angina patients, but also applies to patients presenting with AMI. Our study confirms that the higher rate of cardiovascular events in patients with PAD presenting with MI may be partially explained by greater coronary lesion complexity. Patients with PAD may present with more complex lesions and more extensive MI. Thus, this group of patients may be more likely to benefit from more highly potent antiplatelet and lipid-lowering therapy.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation. 2004;110:738–43. doi: 10.1161/01.CIR.0000137913.26087.F0. [DOI] [PubMed] [Google Scholar]
- 2.Zheng ZJ, Sharrett AR, Chambless LE, et al. Associations of ankle-brachial index with clinical coronary heart disease, stroke and preclinical carotid and popliteal atherosclerosis: the Atherosclerosis Risk in Communities (ARIC) Study. Atherosclerosis. 1997;131:115–25. doi: 10.1016/s0021-9150(97)06089-9. [DOI] [PubMed] [Google Scholar]
- 3.Fowkes FGR, Low LP, Tuta S, et al. AGATHA Investigators Ankle-brachial index and extent of atherothrombosis in 8891 patients with or at risk of vascular disease: results of the international AGATHA study. Eur Heart J. 2006;27:1861–7. doi: 10.1093/eurheartj/ehl114. [DOI] [PubMed] [Google Scholar]
- 4.Steg PG, Bhatt DL, Wilson PWF, et al. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA. 2007;297:1197–206. doi: 10.1001/jama.297.11.1197. [DOI] [PubMed] [Google Scholar]
- 5.Brevetti G, Giugliano G, Brevetti L, Hiatt WR. Inflammation in peripheral artery deisease. Circulation. 2010;122:1862–75. doi: 10.1161/CIRCULATIONAHA.109.918417. [DOI] [PubMed] [Google Scholar]
- 6.Aslan AN, Özcan AN, Ayhan H, et al. Evaluation of local carotid stiffness and inflammatory biomarkers in stable angina pectoris. Adv Interv Cardiol. 2017;13:122–9. doi: 10.5114/pwki.2017.68046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arslan S, Yuksel IO, Koklu E, et al. Clinical and morphological features of patients who underwent endovascular interventions for lower extremity arterial occlusive diseases. Adv Interv Cardiol. 2015;11:114–8. doi: 10.5114/pwki.2015.52284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Capodanno D, Salvo MED, Cincotta G, et al. Usefulness of the SYNTAX Score for predicting clinical outcome after percutaneous coronary intervention of unprotected left main coronary artery disease. Circ Cardiovasc Intervent. 2009;2:302–8. doi: 10.1161/CIRCINTERVENTIONS.108.847137. [DOI] [PubMed] [Google Scholar]
- 9.Falcão FJ de A, Rodrigues Alves CM, Caixeta A, et al. Relation between the ankle-brachial index and the complexity of coronary artery disease in older patients. Clin Interv Aging. 2013;8:1611–6. doi: 10.2147/CIA.S52778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sebastianski M, Narasimhan S, Graham MM, et al. Usefulness of the ankle-brachial index to predict high coronary SYNTAX scores, myocardium at risk, and incomplete coronary revascularization. Am J Cardiol. 2014;114:1745–9. doi: 10.1016/j.amjcard.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 11.Ikeda N, Kogame N, Iijima R, et al. Carotid artery intima-media thickness and plaque score can predict the SYNTAX score. Eur Heart J. 2012;33:113–9. doi: 10.1093/eurheartj/ehr399. [DOI] [PubMed] [Google Scholar]
- 12.Korkmaz L, Bektas H, Korkmaz AA, et al. Increased carotid intima-media thickness is associated with higher SYNTAX score. Angiology. 2012;63:386–9. doi: 10.1177/0003319711419837. [DOI] [PubMed] [Google Scholar]
- 13.Stein JH, Korcarz CE, Hurst RT, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a Consensus Statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force Endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr. 2008;21:93–111. doi: 10.1016/j.echo.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 14.Ueki Y, Miura T, Miyashita Y, et al. Predictive value of combining the ankle-brachial index and SYNTAX Score for the prediction of outcome after percutaneous coronary intervention (from the SHINANO Registry) Am J Cardiol. 2016;117:179–85. doi: 10.1016/j.amjcard.2015.10.042. [DOI] [PubMed] [Google Scholar]
- 15.Anon SYNTAX score calculator. Available at: http://www.syntaxscore.com.
- 16.Ikeda N, Kogame N, Iijima R, et al. Impact of carotid artery ultrasound and ankle-brachial index on prediction of severity of SYNTAX score. Circ J. 2013;77:712–6. doi: 10.1253/circj.cj-12-1087. [DOI] [PubMed] [Google Scholar]
- 17.Grenon SM, Vittinghoff E, Owens CD, et al. Peripheral artery disease and risk of cardiovascular events in patients with coronary artery disease: insights from the Heart and Soul Study. Vasc Med. 2013;18:176–84. doi: 10.1177/1358863X13493825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bryniarski KL, Yamamoto E, Takumi H, et al. Differences in coronary plaque characteristics between patients with and those without peripheral arterial disease. Coron Artery Dis. 2017;28:658–63. doi: 10.1097/MCA.0000000000000531. [DOI] [PubMed] [Google Scholar]
- 19.Wykrzykowska JJ, Garg S, Girasis C, et al. Value of the SYNTAX score for risk assessment in the all-comers population of the randomized multicenter LEADERS (Limus Eluted from A Durable versus ERodable Stent coating) trial. J Am Coll Cardiol. 2010;56:272–7. doi: 10.1016/j.jacc.2010.03.044. [DOI] [PubMed] [Google Scholar]
- 20.Garg S, Serruys PW, Silber S, et al. The prognostic utility of the SYNTAX score on 1-year outcomes after revascularization with zotarolimus- and everolimus-eluting stents: a substudy of the RESOLUTE All Comers Trial. JACC Cardiovasc Interv. 2011;4:432–41. doi: 10.1016/j.jcin.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 21.Caixeta A, Généreux P, Palmerini T, et al. Prognostic utility of the SYNTAX score in patients with single versus multivessel disease undergoing percutaneous coronary intervention (from the Acute Catheterization and Urgent Intervention Triage StrategY [ACUITY] trial) Am J Cardiol. 2014;113:203–10. doi: 10.1016/j.amjcard.2013.08.035. [DOI] [PubMed] [Google Scholar]
- 22.Korkmaz L, Adar A, Erkan H, et al. Ankle-brachial index and coronary artery lesion complexity in patients with acute coronary syndromes. Angiology. 2012;63:495–9. doi: 10.1177/0003319711429561. [DOI] [PubMed] [Google Scholar]
- 23.Aykan AÇ, Gül I, Gökdeniz T, et al. Ankle brachial index intensifies the diagnostic accuracy of epicardial fat thickness for the prediction of coronary artery disease complexity. Heart Lung Circ. 2014;23:764–71. doi: 10.1016/j.hlc.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 24.Ikeda N, Gupta A, Dey N, et al. Improved correlation between carotid and coronary atherosclerosis SYNTAX score using automated ultrasound carotid bulb plaque IMT measurement. Ultrasound Med Biol. 2015;41:1247–62. doi: 10.1016/j.ultrasmedbio.2014.12.024. [DOI] [PubMed] [Google Scholar]
- 25.Amer MS, Tawfik HM, Elmoteleb AMA, Maamoun MMA. Correlation between ankle brachial index and coronary artery disease severity in elderly Egyptians. Angiology. 2014;65:891–5. doi: 10.1177/0003319713510594. [DOI] [PubMed] [Google Scholar]
- 26.Kato M, Dote K, Habara S, et al. Clinical implications of carotid artery remodeling in acute coronary syndrome: ultrasonographic assessment of positive remodeling. J Am Coll Cardiol. 2003;42:1026–32. doi: 10.1016/s0735-1097(03)00905-7. [DOI] [PubMed] [Google Scholar]
- 27.Lombardo A, Biasucci LM, Lanza GA, et al. Inflammation as a possible link between coronary and carotid plaque instability. Circulation. 2004;109:3158–63. doi: 10.1161/01.CIR.0000130786.28008.56. [DOI] [PubMed] [Google Scholar]
- 28.Underhill HR, Yuan C, Terry JG, et al. Differences in carotid arterial morphology and composition between individuals with and without obstructive coronary artery disease: a cardiovascular magnetic resonance study. J Cardiovasc Magn Reson. 2008;10:31.. doi: 10.1186/1532-429X-10-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wrotniak L, Kablak-Ziembicka A, Karch I, et al. Multiterritory atherosclerosis and carotid intima-media thickness as cardiovascular risk predictors after percutaneous angioplasty of symptomatic subclavian artery stenosis. J Ultrasound Med. 2016;35:1977–84. doi: 10.7863/ultra.15.10042. [DOI] [PubMed] [Google Scholar]
- 30.Hirsch AT, Criqui MH, Treat-Jacobson D, et al. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001;286:1317–24. doi: 10.1001/jama.286.11.1317. [DOI] [PubMed] [Google Scholar]
- 31.Antman EM, Tanasijevic MJ, Thompson B, et al. Cardiac-specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. N Engl J Med. 1996;335:1342–9. doi: 10.1056/NEJM199610313351802. [DOI] [PubMed] [Google Scholar]
- 32.Ikeda N, Araki T, Sugi K, et al. Ankle-brachial index and its link to automated carotid ultrasound measurement of intima-media thickness variability in 500 Japanese coronary artery disease patients. Curr Atheroscler Rep. 2014;16:393. doi: 10.1007/s11883-013-0393-x. [DOI] [PubMed] [Google Scholar]
- 33.Kul S, Akgul O, Uyarel H, et al. High SYNTAX score predicts worse in-hospital clinical outcomes in patients undergoing primary angioplasty for acute myocardial infarction. Coron Artery Dis. 2012;23:542–8. doi: 10.1097/MCA.0b013e3283599486. [DOI] [PubMed] [Google Scholar]
- 34.Farooq V, Serruys PW, Bourantas CV, et al. Quantification of incomplete revascularization and its association with five-year mortality in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial validation of the residual SYNTAX score. Circulation. 2013;128:141–51. doi: 10.1161/CIRCULATIONAHA.113.001803. [DOI] [PubMed] [Google Scholar]
- 35.Garg S, Sarno G, Serruys PW, et al. Prediction of 1-year clinical outcomes using the SYNTAX score in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: a substudy of the STRATEGY (Single High-Dose Bolus Tirofiban and Sirolimus-Eluting Stent Versus Abciximab and Bare-Metal Stent in Acute Myocardial Infarction) and MULTISTRATEGY (Multicenter Evaluation of Single High-Dose Bolus Tirofiban Versus Abciximab With Sirolimus-Eluting Stent or Bare-Metal Stent in Acute Myocardial Infarction Study) trials. JACC Cardiovasc Interv. 2011;4:66–75. doi: 10.1016/j.jcin.2010.09.017. [DOI] [PubMed] [Google Scholar]