Abstract
Posttraumatic stress disorder (PTSD) is a chronic and debilitating disorder that affects the lives of 7-8% of adults in the U.S. Although several interventions demonstrate clinical effectiveness for treating PTSD, many patients continue to have residual symptoms and ask for a variety of treatment options. Complementary health approaches, such as meditation and yoga, hold promise for treating symptoms of PTSD. This meta-analysis evaluates the effect size (ES) of yoga and meditation on PTSD outcomes in adult patients. We also examined whether the intervention type, PTSD outcome measure, study population, sample size, or control condition moderated the effects of complementary approaches on PTSD outcomes. The studies included were 19 randomized control trials with data on 1,173 participants. A random effects model yielded a statistically significant ES in the small to medium range (ES = −.39, p < .001, 95% CI [−.57, −.22]). There were no appreciable differences between intervention types, study population, outcome measures, or control condition. There was, however, a marginally significant higher ES for sample size ≤ 30 (ES = −.78, k = 5). These findings suggest that meditation and yoga are promising complementary approaches in the treatment of PTSD among adults and warrant further study.
Keywords: complementary health, yoga, meditation, PTSD, traumatic stress
1. Introduction
Several decades of research reveal chronic and debilitating biological, psychological, and social ramifications for individuals suffering from posttraumatic stress disorder (PTSD). The Diagnostic and Statistical Manual of Mental Disorders (5th ed., DSM-5; American Psychiatric Association, 2013) classifies the symptoms of PTSD within four symptom clusters of intrusion, persistent avoidance, negative alterations in cognitions and mood, and marked alterations in arousal. Both pharmacological and psychological interventions are used in the treatment of PTSD. The current evidence base for pharmacological treatment for PTSD is strongest for selective serotonin reuptake inhibitors (SSRIs), and are recommended as second-line treatment for patients that do not engage in or cannot access trauma-focused psychotherapies (Hoskins et al., 2015; Lee et al., 2016). Trauma-focused interventions based on cognitive models address trauma-related beliefs, memories, and emotions and include Prolonged Exposure (PE), Cognitive Processing Therapy (CPT), and eye movement desensitization and reprocessing (EMDR) therapy. Non-trauma focused interventions are also used to treat PTSD, and include any psychological intervention that uses cognitive behavioral therapy (CBT), for example stress inoculation training (SIT). Evidence suggests that trauma-focused CBT (including CPT and PE), EMDR, and non-trauma-focused CBT are effective, though trauma-focused CBT and EMDR are considered more effective than non-trauma-focused CBT (Bisson, Roberts, Andrew, Cooper, and Lewis, 2013). Despite empirical support of effectiveness, these interventions have high rates of incompletion (up to 50%) and many patients, both veterans and civilians, continue to have residual symptoms (Bradley, Greene, Russ, Dutra, & Westen, 2005; Kearney & Simpson, 2015; Schottenbauer, Glass, Arnkoff, Tendick, & Gray, 2008; Steenkamp, Litz, Hoge, & Marmar, 2015). Further, trauma-focused CBT approaches with exposure-based components incur greater dropout rates than non-trauma-focused therapies (Bisson et al., 2013). Some reasons for this difference include that non-trauma-focused CBT may be more appealing to a majority of patients and/or more emotionally tolerable. For this prevalent and devastating disorder, the poor completion rates and relatively poor remission rates of existing, standard PTSD interventions suggest that new, complementary and integrative interventions, whether adjunctive or stand-alone, are likely warranted. Further, both patients and providers have voiced desires for the availability of more PTSD treatment options (Lang et al., 2012).
Complementary health approaches hold promise for treating symptoms of PTSD. Complementary approaches are defined as non-mainstream practices typically used together with conventional medicine (National Center for Complementary and Integrative Health). Interest in complementary approaches among veterans and civilians is growing. Nearly 40% of adults in the U.S. use complementary health approaches and military personnel engage in these health practices at similar rates. A 2011 report by the Veterans Health Administration (VHA) indicated that 80% of VHA facilities offer meditation and stress management to patients (Strauss, 2011). An example of stress management commonly used to treat PTSD is stress inoculation training (SIT), a non-trauma-focused CBT approach to PTSD treatment that teaches skills for managing stress through relaxation and thought-stopping. Though it has been shown to be more effective than non-CBT interventions, like psychodynamic or present-centered therapies, it is not as effective as trauma-focused CBT (Bisson et al., 2013). Both yoga and meditation-based approaches are among the most popular complementary approaches for health promotion used by adults in the U.S. (Clarke, Black, Stussman, Barnes, & Nahin, 2015). Complementary approaches fit well with the interest in interventions that are not trauma-focused.
Increasingly, researchers are investigating the use of complementary approaches for treating PTSD. Complementary therapies used to treat PTSD include acupuncture, mindfulness-based stress reduction, meditation, yoga, deep-breathing exercises, guided imagery, hypnotherapy, progressive relaxation, and tai chi. Reviews of the literature on complementary approaches for the treatment of PTSD by Kim, Schneider, Kravitz, Mermier, and Burge (2013) and the VA’s Health Service Research and Development (Strauss, 2011) found support for beneficial effect of such interventions on symptoms of PTSD; however, their findings were limited by the paucity of well-designed trials.
Here, we focus on a set of complementary health practices that have been used for the treatment of PTSD, namely meditation and yoga, with an explicit focus on randomized controlled trials. The National Center for Complementary and Integrative Health (NCCIH) classifies meditation and yoga as complementary mind and body health approaches. There are many forms of meditation, some of which teach practitioners to observe thoughts, feelings, and sensations in a non-judgmental manner. Mindfulness meditation, for example, teaches participants to orient their attention to the present with curiosity, openness, and acceptance. Experiencing the present moment non-judgmentally and openly may encourage practitioners to approach rather than avoid distressing thoughts and feelings, which may reduce cognitive distortions and avoidance (Gallegos, Cross, & Pigeon, 2015). Present-orientation also avoids excessive orientation toward the past or future, which may reduce worry and rumination. Another meditative practice, known as mantra-based meditation, cultivates focused attention by thinking or repeating a word or phrase. For either meditative practice, attentional control increases control of intrusive memories, allowing a patient to shift attention to coping strategies and problem solving (Lang 2012). In this way, meditation practices have elements of exposure, cognitive change, attentional control, self-management, relaxation, and acceptance (Baer, 2003), all of which are pertinent to the symptoms of PTSD.
Yoga typically combines physical postures, breathing techniques, meditation, and relaxation. Yoga has been shown to reduce physiological arousal in PTSD patients and is believed to affect the pathology of PTSD by improving somatic regulation and body awareness, which are imperative to emotion regulation (van der Kolk et al., 2014). Learning to reflect rather than react to difficult physiological and emotional states has implications for the experience and expression of emotions in PTSD. Overall, these mind and body practices not only allow for a variety of options when choosing an approach to care, but address several domains of PTSD.
No study to date has provided a meta-analytic review of the literature on complementary mind and body approaches to the treatment of PTSD. The aim of this study was to evaluate the effect size (ES) of these complementary health approaches on PTSD outcomes in adult patients. We also examined whether the intervention type (mindfulness meditation, other meditation, and yoga), PTSD outcome measure (clinician administered and self-report), study population (veteran and non-veteran), sample size, or control condition (active and non-active) moderated the effects of complementary approaches on PTSD outcomes. Recommendations are provided for future research based on the review and analysis.
2. Method
2.1. Data Sources and Search Strategy
MEDLINE (from 1946) and PsychINFO (from 1967) were searched through May 31, 2016. Clinicaltrials.gov was also searched to identify unpublished trials that met study eligibility criteria. Selection criteria for interventions were defined a priori and included: mind and body practices rather than natural products (e.g., herbs, vitamins, probiotics, etc.); outside of mainstream, or conventional, medicine; taught by a trained teacher; and encourage participants to take an active role. Boolean search logic and MeSH terms were used to create the following search terms: [(posttraumatic stress disorder or traumatic stress or psychological trauma) and (mind-body or meditation or mindfulness or mindfulness-based stress reduction or mindfulness-based cognitive therapy or transcendental or tai chi or qi gong or yoga or mantram or complementary health or alternative health)]. Data from unpublished trials, when identified, was obtained through direct communication from study investigators.
2.2 Study Selection and Eligibility
All abstracts identified through the literature search were screened with a low threshold. Full text articles were retrieved and evaluated for eligibility by all investigators. Eligible articles contained the following elements: 1) available in English, 2) utilized human subjects 18 years of age or older, 3) original research, 4) randomized controlled trial with any comparator as a control and a minimum sample size of 10, 5) use of a mind and body complementary health approach as categorized by the NCCIH, and 6) use of a PTSD measure with a sample that met criteria for a PTSD diagnosis (see Figure 1 for flow diagram of selection process).
Figure 1.
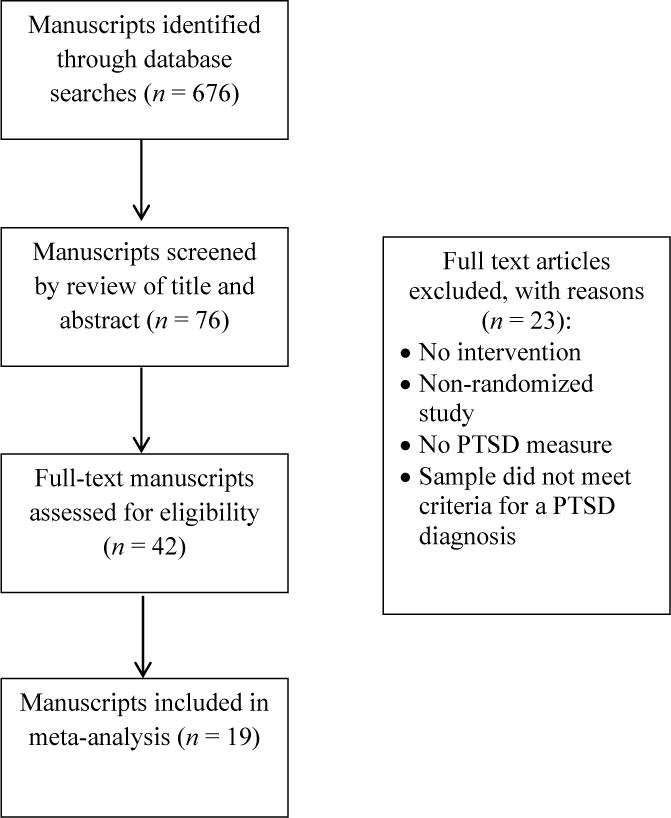
Flow diagram of study selection process
2.3. Data Extraction
A two-stage approach was used to determine study selection. First, three of the investigators (A. G, W. P., & K. H.) independently performed data extraction for the studies based on the above a priori criteria. Second, these investigators met to review the selected studies. Any disagreements were resolved and consensus was reached by these investigators for all studies included in the analysis. We extracted information on population, gender, mean age, intervention type, frequency, and duration, control condition, sample size, and PTSD outcomes. We also used the Cochrane risk of bias tool to assess risk of bias for each study (Higgins, Altman, & Sterne, 2011). Each study was rated as low, high, or unclear risk of bias on random sequence generation, allocation concealment, blinding of outcome assessments, incomplete outcome data, selective reporting, and other forms of bias as well as providing an overall risk of bias rating (Table S1). We did not rate the studies on blinding of participants and researchers since participants were aware of the intervention received, as is typical in most behavioral intervention research trials.
Studies were classified as meditation or yoga based on primary components of the intervention as provided by NCCIH, the main distinction being the emphasis of movement in yoga. We further divided the meditation category between mindfulness meditation and other meditations due to the differences in how the meditative practices engage attention. Specifically, mindfulness meditation uses open-monitoring to attend to sensations, emotions, and thoughts as they enter into awareness. Mantra meditation cultivates a focused attention on an object, word, or phrase. Both propose to cultivate non-judgmental attention to one’s present experience, often producing relaxation and stress reduction. Therefore, studies were grouped into the following three categories of complementary health interventions: (1) mindfulness meditation; (2) other meditation; and (3) yogic movement. PTSD was assessed using self-report measures and clinician administered diagnostic interviews. Here, studies were grouped according to use of the Clinician Administered PTSD Scale (CAPS; Weathers, Ruscio, & Keane, 1999), use of the Posttraumatic Stress Disorder Checklist (PCL; Weathers, Litz, Herman, Huska, & Keane, 1993) as a self-report measure, and other self-report measures.
2.3. Calculation of Effect Sizes and General Analytic Strategies
Hedge’s g (Hedges & Olkin, 1985), which accounts for small sample bias, was the index of effect adjusted for any preintervention differences between intervention and control groups (Durlak, 2009; Wilson, Gottfredson, & Najaka, 2001; Wilson & Lipsey, 2007). Each ES was weighted by the inverse of its variance prior to any analysis. All ESs were calculated such that negative values indicate a favorable result (more symptom reduction) for program participants over controls.
Nineteen studies were included in the current meta-analysis. Of these, however, two studies used a three arm trial design (two intervention groups versus a single control group; Heffner, Crean, & Kemp 2a,b, 2016; Wahbeh, Goodrich, Goy, & Oken, 2016). Two approaches were used to handle these statistically dependent ESs. The first, and more simpler approach, was to average ESs within each of these two studies (Higgins, Meeks, & Altman, 2011; Lipsey & Wilson, 2001) using the formulas put forth by Higgins and Deeks (2011). The second approach utilizes information from all arms of each study and adjusts for the covariance among the dependent ESs (Gleser & Olkin, 2009). Thus, the final sample was comprised of 21 interventions from 19 studies.
For the studies with multiple measures of PTSD, we used the CAPS as the primary measure (8 studies used both CAPS and PCL; 2 only used the CAPS), followed by PCL (8 studies used the PCL). The remaining two studies used differing measures of PTSD (Impact of Events Scale [Weiss & Marmar, 1996] and Post-Vietnam Stress Disorder Scale [Figley & Sprenkle, 1978]). When testing hypotheses, a .05 probability was used to determine statistical significance. A mean ES is considered statistically different from zero when its 95% confidence interval does not include zero.
Heterogeneity of ESs was examined through the Q statistic which is distributed as a chi-square with k − 1 degrees of freedom, where k = the number of studies. A significant Q value suggests studies are not drawn from a common population whereas a nonsignificant value indicates the opposite. Because of the relatively limited number of studies examined (k = 19) and the accompanying low power associated with the Q statistic, we supplemented the Q statistic with the I2 statistic (Higgins, Thompson, Deeks, & Altman, 2003), which reflects the degree (as opposed to the statistical significance) of heterogeneity among a set of studies along a 0%-100% continuum. Whereas the Q statistics assess the statistical significance of the variability of effects within and between study groups, the I2 statistic provides an estimate of the degree of heterogeneity in effects. Higgins and colleagues (2003) suggest that I2 values of at least 15% reflect a mild degree of heterogeneity, between 25% and 50% a moderate degree of heterogeneity, and values greater than or equal to 75% reflect a high degree of heterogeneity.
To assess if subgroups differed significantly, the Q-test assessing heterogeneity across subgroups was used (Borenstein, Hedges, Higgins, & Rothstein, 2009; Lipsey & Wilson, 2001). Finally, all analyses are based on a random effects model, unless otherwise noted, using the restricted maximum likelihood estimation procedure using the metafor statistical package (Viechtbauer, 2010) implemented in the R package for statistical computing. For subgroup analyses, random effects within group with fixed effects between groups were estimated with between study variance pooled across groups, due to limited numbers of studies in many of the subgroups examined. Thus, for subgroup analyses, the restricted maximum likelihood estimate was used to estimate between study variance, with the Q-profile method used to calculate 95% confidence intervals, as suggested by Veroniki and colleagues (2016). The Duval and Tweedie (2000) trim and fill technique as well as the Rosenthal (1970) fail-safe N was applied as a form of sensitivity analysis adjusting for possible publication bias and missing studies.
3. Results
The studies that met inclusion criteria for this meta-analysis were 19 RCTs with data on 1,173 participants. Type of complementary approach (meditation, mindfulness training, yogic movement, and a study that combined mindfulness and mantra meditation), primary outcome measure (self-report or clinician administered), veteran status, sample size, and control condition (active or non-active) were all examined as potential moderators of study ESs. Subgroup analyses are based on pooled variance between studies, due to limited sample sizes in some subgroups and the lack of expected between study variance for veteran status (i.e., we did not treat these subgroups as a random sample of a population of veteran status). Results presented are based on the 19 studies with the three arm studies ESs averaged across the intervention arms, supplemented with the Gleser and Olkin (2009) approach to the treatment of depended ESs. Table 2 summarizes the included studies.
Table 2.
Description of Included Studies
| Study (Reference) |
Intervention | Control condition | Population | Intervention frequency, duration |
|---|---|---|---|---|
| Bormann et al. (2013) | Mantram repetition, group-based | TAU | Combat veterans | 6 sessions, 1.5 hours, 1 time/week |
| Bränström et al. (2012) | MBSR (modified), group-based | WLC | Adults treated for cancer | 8 sessions, 2 hours, 1 time/week |
| Brooks & Scarano (1985) | Transcendental meditation, group-based | Individual psychotherapy (eclectic) | Vietnam veterans | 16 sessions, 1.5 hours, 1 time/day, 4 days followed by 1.5 hours, 1 time/week, 12 weeks |
| Carter et al. (2013) | SKY, group-based | WLC | Vietnam veterans | 22 session hours, 5 days |
| Davis (unpublished) | MBSR, group-based | Present-centered group therapy | Veterans | 8 sessions, 1.5 hours, 1 time/week + 6-hour all-day session |
| Heffner et al. 1 (2016) | Mindfulness-based PTSD treatment (MBPT), individual-based | Prolonged Exposure | Veterans | 8 sessions, 1 time/week |
| Heffner et al. 2a (2016) | Mantra-based meditation, group-based | Present-centered group therapy | Veterans | 8 sessions, 1.5 hours, 1 time/week |
| Heffner et al. 2b (2016) | Transcendental meditation, group-based and individual-based | Present-centered group therapy | Veterans | 10 sessions, 1.5 hours, 1 time/week |
| Heffner et al. 3 (2016) | Combined MBSR with mantra meditation (Inner Resources for Veterans (IRV)), group-based | PTSD education group | Veterans | 8 sessions, 1 hour, 1 time/week |
| Jindani et al. (2015) | Kundalini yoga, group-based | Control | Adults | 8 sessions, 1.5 hours, 1 time/week |
| Kearney et al. (2013) | MBSR, group-based | TAU | Veterans | 8 sessions, 2.5 hours, 1 time/week + 7-hour all-day |
| Kim et al. (2013) | MBX, group-based | Control | Nurses with subclinical PTSD | 16 sessions, 1 hour, 2 times/week |
| Mitchell et al. (2014) | Kripalu-based yoga | Assessment control group (self-monitoring) | Veterans and civilian women | 12 sessions, 75 minutes, 1 or 2 times/week |
| Nakamura et al. (2011) | MBB, group-based | Sleep hygiene (1 hr/week) |
Veterans with self-reported sleep disturbance | 2 sessions, 1.5 hours, 1 time/week |
| Niles et al. (2012) | MBSR, individual-based | Telehealth psychoeducation | Veterans with combat-related PTSD | 8 sessions, 45 minutes in-person (2 times) and 20 minutes telephone (6 times) |
| Polusney et al. (2015) | MBSR, group-based | Present-centered therapy | Veterans | 9 sessions, 2.5 hours, 1 time/week (including 1 PTSD psychoeducation session) + 7-hour all-day |
| Possemato et al. (2016) | MBSR, group-based | PC-TAU | Vetarans | 4 sessions, 1.5 hours, 1 time/week |
| Seppälä et al. (2014) | SKY, group-based | WLC | Veterans | 7 sessions, 3 hours, 1 time/day |
| van der Kolk et al. (2014) | Trauma-Informed yoga, group-based | Supportive women’s health education | Women with chronic, treatment-resistant PTSD | 10 sessions, 1 hour, 1 time/week |
| Wahbeh et al. a (2016) | Mindfulness body scan meditation, individual-based | Sitting quietly | Combat veterans | 6 sessions, 20 minues, 1 time/week |
| Wahbeh et al. b (2016) | Mindfulness awareness of breath, individual-based | Sitting quietly | Combat veterans | 6 sessions, 20 minues, 1 time/week |
Notes. MBB = mind body bridging; MBCT = mindfulness-based cognitive therapy; MBSR = mindfulness-based stress reduction; MBX = mindfulness-based stretching and deep breathing exercise; PC-TAU = Primary care treatment as usual; PTSD = posttraumatic stress disorder; SKY = Sudarshan Kriya Yoga; TAU = treatment as usual; WLC = wait-list control;
Table 3 presents ESs and confidence intervals as well as categorical moderator status for each of the 19 studies and overall risk of bias. Of these 19 studies, six were rated at high risk, eight at low risk, and five at unclear risk of bias. Figure 2 presents forest plot information, by each complementary approach. While visual inspection of the forest plot does suggest that no study appears to be an outlier, statistical evidence suggested that the Jindani, Turner, and Khalsa (2015) study (study 16, Figure 3) may be both an outlier and an influential case (Viechtbauer & Cheung, 2010). For this reason, sensitivity analyses removing the Jindani et al. (2015) study was conducted for all subsequent analyses. The variability between studies warranted the use of a random effects approach. Overall, the random effects model averaging studies with multiple intervention arms yielded a statistically significant ES in the small to medium range (ES = −.39, p < .001, 95% confidence interval (CI) [−.57, −.22]). Though reduced, the overall effect remained significant with the Jindani et al. (2015) study removed (ES = −.33, p < .001, 95% CI [−.45, −.20]). Similar results were noted taking the dependencies of ESs into account for the two studies with three arms. Here, the two ESs (k = 19 for all studies; k = 2 for third arm vs. control) were −.37, p < .001, 95% CI [−.49, −.24] and −.39, p = .036, 95% CI [−.75, −.03], respectively and did not significantly differ (difference = .024, 95% CI [−.34, .39]). Averaging these effects gave an overall ES of −.37. Though again reduced, ESs remained significant after removing the Jindani et al. (2015) study (average ES = −.33). Significant heterogeneity existed when including the Jindani et al. (2015) study. Heterogeneity was not significant after removing this one study.
Table 3.
Study characteristics and effect sizes for participating studies.
| Study | Sample Size | Primary Outcome Measure | ES (95% CI) |
Veteran | Control Condition |
Risk of Bias |
|
|---|---|---|---|---|---|---|---|
| E | C | ||||||
| Mindfulness-Based | |||||||
| Bränström et al., 2012 | 39 | 32 | IES | −.07 (−.54 to .40) |
Non-Veterans | Non-active | Low |
| Davis, unpublished | 96 | 95 | CAPS | −.39 (−.68 to −.10) |
Veterans | Active | Low |
| Heffner et al. 1, 2016 | 7 | 7 | CAPS | −.07 (−1.12 to .98) |
Veterans | Active | High |
| Kearney et al., 2013 | 25 | 22 | PCL | −.22 (−.79 to .36) |
Veterans | Active | Unclear |
| Nakamura et al., 2011 | 35 | 28 | PCL | −.31 (−.81 to .19) |
Veterans | Active | Unclear |
| Niles et al., 2012 | 17 | 16 | CAPS | −1.21 (−1.96 to −.47) |
Veterans | Active | High |
| Polusney et al., 2015 | 58 | 58 | PCL | −.40 (−.76 to −.03) |
Veterans | Active | Low |
| Possemato et al., 2016 | 16 | 26 | CAPS | −.44 (−1.07 to .19) |
Veterans | Active | Unclear |
| Wahbeh et al. a, 2016 | 27 | 25 | PCL | −.17 (−.71 to .38) |
Veterans | Active | Low |
| Wahbeh et al. b, 2016 | 25 | 25 | PCL | −.10 (−.65 to .46) |
Veterans | Active | Low |
| Meditation-Based | |||||||
| Bormann et al., 2013 | 66 | 70 | CAPS | −.27 (−.61 to .07) |
Veterans | Active | Low |
| Brooks & Scarano 1985 | 9 | 9 | PVSDS | −.86 (−1.83 to .11) |
Veterans | Active | High |
| Carter et al., 2013 | 14 | 11 | PCL | −.69 (−1.50 to .12) |
Veterans | Non-Active | Low |
| Heffner et al. 2a, 2016 | 22 | 24 | CAPS | −.04 (−.62 to .54) |
Veterans | Active | Unclear |
| Heffner et al. 2b, 2016 | 19 | 24 | CAPS | −.48 (−1.09 to .13) |
Veterans | Active | Unclear |
| Seppälä et al., 2014 | 10 | 10 | PCL | −.81 (−1.72 to .10) |
Veterans | Active | Low |
| Yoga-Based | |||||||
| Jindani et al., 2015 | 21 | 29 | PCL | −1.41 (−2.03 to −.78) |
Non-Veterans | Non-Active | High |
| Kim et al., 2013 | 11 | 11 | PCL | −1.34 (−2.27 to −.42) |
Non-Veterans | Active | Low |
| Mitchell et al., 2014 | 20 | 18 | PCL | .11 (−.53 to .75) |
Non-Veterans | Active | High |
| van der Kolk et al., 2014 | 32 | 32 | CAPS | −.35 (−.85 to .14) |
Non-Veterans | Active | Unclear |
| Mindfulness/Meditation Combination-Based | |||||||
| Heffner et al. 3, 2016 | 18 | 14 | CAPS | .46 (−.25 to 1.17) |
Veterans | Active | High |
Note. IES = Impact of Events Scale; CAPS = Clinician Administered PTSD Scale; PCL = PTSD Checklist; PVSDS = Post-Vietnam Stress Disorder Scale; ES = effect size Hedge’s g; CI= 95% confidence interval.
Figure 2. Forest plot of participating studies, by program type.
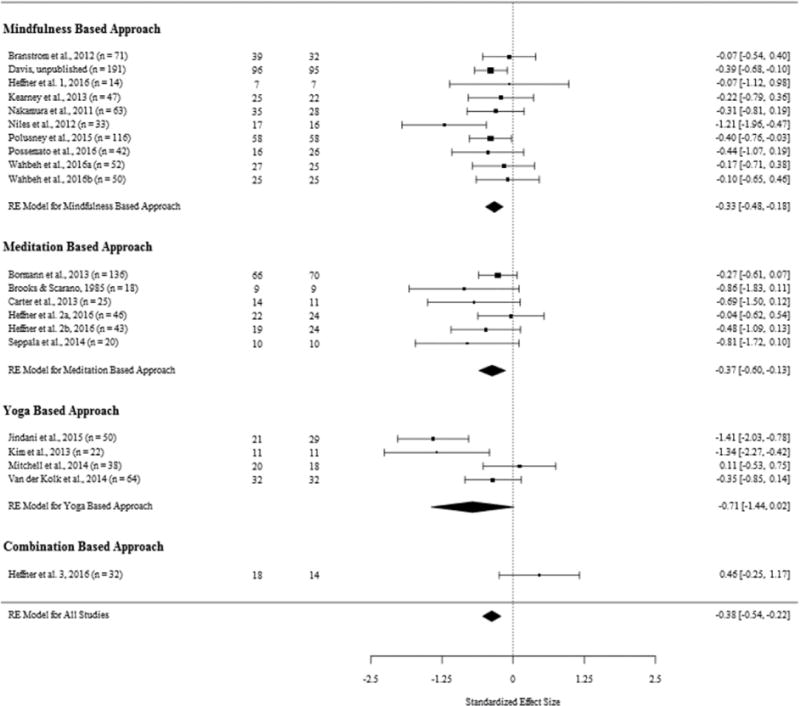
Figure 3.
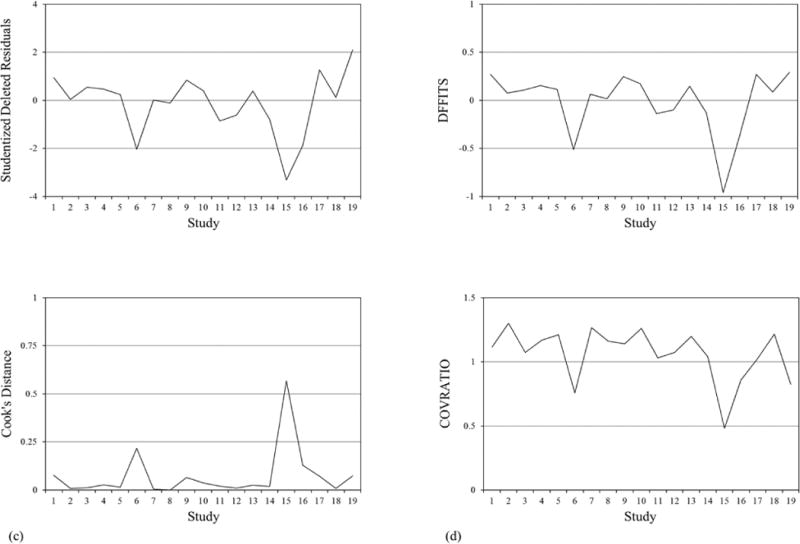
Plot of the (a) studentized deleted residuals; (b) DFFITS values; (c) Cook’s Distance; and (d) COVRATIO values for 19 studies examining the effectiveness of complementary health approaches on PTSD.
Application of Duval and Tweedie’s (2000) trim and fill technique as a form of sensitivity analysis adjusting for possible publication bias and missing studies with the averaged ES for the three arm studies suggested absence of publication bias. Rosenthal’s fail-safe N (1979) suggests that 249 non-significant studies would need to be added to result in a non-significant overall ES, 25 non-significant studies would need to be added to reduce the overall effect to −.20 (Orwin, 1983). With the Jindani et al. (2015) study omitted, however, the procedure suggested the trimming and filling of two studies and resulted in an adjusted mean ES estimate that remained statistically significant (k = 20, ES = −.28, p < .001, 95% CI [−.42, −.14], I2 = 19.14%). Rosenthal’s fail-safe N (1979) suggests that 170 non-significant studies would need to be added to result in a non-significant overall ES, 19 non-significant studies would need to be added to reduce the overall effect to −.20 (Orwin, 1983).
3.1. Moderator Effects
3.1.1. Intervention Formats
Mindfulness Meditation
Mindfulness training teaches moment-to-moment non-judgmental awareness. Studies included in the current analysis evaluated mindfulness-based stress reduction (MBSR; k = 8; Bränström, Kvillemo, & Moskowitz, 2012; Davis (unpublished); Heffner et al. 1, 2016; Kearney, McDermott, Malte, Martinez, & Simpson, 2013; Niles, McDermott, Malte, Martinez, & Simpson, 2012; Polusney et al., 2015; Possemato, Bergen-Cico, Treatman, Allen, Eaker, & Pigeon, 2016; Wahbeh et al., 2016) and mind-body bridging (MBB; k = 1; Nakamura, Lipschitz, Landward, Kuhn, & West, 2011). MBSR is a manualized treatment typically conducted in group format. The program includes awareness of breath meditations, hatha yoga, walking meditations, and meditative body scans. The MBB study was used specifically for sleep and is a mindfulness-based intervention that teaches awareness skills to calm the mind and relax the body. It includes cognitive restructuring, mindfulness training, trigger identification, and grounding (Tollefson, Webb, Shumway, Block, & Nakamura, 2009). Although MBSR includes movement derived from hatha yoga, we distinguished them from other yoga-based studies focusing exclusively on movement.
Other Meditation
Other meditation studies included in the analysis examined the use of transcendental meditation (TM; k = 3; Brooks & Scarano, 1985; Heffner et al. 2a,b, 2016), Sudarshan Kriya Yoga (SKY; k = 2; Carter et al., 2013; Seppälä et al., 2014), and mantra-based meditation (k = 1; Bormann, Thorp, Wetherell, Golshan, & Lang, 2013). Transcendental meditation postulates that practitioners can transcend or detach from their experience through meditation. Sudarshan Kriya Yoga is a type of meditation that instructs practitioners to engage in cyclical controlled breathing. Mantra-based meditation cultivates attention by instructing participants to focus on a word, object, or phrase.
Yoga
Yoga typically combines physical postures, breathing techniques, meditation, and relaxation. The yoga studies in this meta-analysis examined trauma-informed yoga (k = 1; van der Kolk et al., 2014), Kripalu-based yoga (k = 1; Mitchell et al., 2014), Kundalini yoga (k = 1; Jindani et al., 2015), and a mindfulness-based stretching and deep breathing exercise (MBX; k = 1; Kim et al., 2013). Trauma-informed, Kripalu, and Kundalini yoga are all based on hatha yoga, which emphasizes the use of breathing, physical postures, and the connection between the body and mind. MBX instructs participants to mindfully pay attention to each movement and focus on the regulation of the breath.
Nine of the studies used a mindfulness meditation approach (ES = −.34, p < .001, 95% CI = [−.49, −.18]), 5 were other meditation-based (ES = −.38, p = .002, 95% CI = [−.63, −.14]), 4 were yoga-based (ES = −.71, p < .055, 95% CI = [−1.44, .02]) which was only marginally significant, and 1 was a combination of mindfulness and meditative practices (ES = .46, p = .203, 95% CI = [−.25, 1.17]). The marginal significance for the yoga-based treatments was likely a function of both low statistical power and the heterogeneity in treatment effects (Q (3 df) = 14.57, p = .002, I2 = 80.28). There was little heterogeneity in ESs among the mindfulness based (Q (8 df) = 8.29, p = .406, I2 = .01%) or meditation based studies (Q (4 df) = 3.00. p = .558, I2 = 0.00%). There were no overall differences in these 4 ES (Q (3 df) = 6.03, p = .110). These results were largely replicated with the removal of the Jindani (2015) study, though the yoga-based ES was no longer significant (ES = −.46, p = .230, 95% CI [−1.22, .29]); though. heterogeneity among yoga-based studies remained significant (Q (2 df) = 14.57, p = .002). These results were replicated using the Gleser and Olkin approach to dependent ESs.
3.1.2. Outcome Measure
CAPS was used as the primary outcome measure in 8 studies (ES = −.33, p < .001, 95% CI [−.50, −.17]), 9 used PCL (ES = −.51, p = .002, 95% CI [−.84, −.18]), and 2 used a different measure (ES = −.35, p = .357, 95% CI [−1.09, .39]). While each of these overall ESs were in the small-medium range (Lipsey & Hurley, 2009), the ES for other measures (IES and PVSDS) was not statistically significant. However, there were no statistically different ESs based on measure used in the studies (Q (2 df) = .92, p = .630). Significant variability remained among studies using the PCL as the primary measure (Q (8 df) = 19.49, p = .012, I2 = 62.54%). This was not the case for studies using CAPS as the primary outcome measure (Q (7 df) = 10.95, p = .141, I2 = 0.00%). For the studies using other primary outcome measures, while the Q-statistic was not significant (Q (1 df) = 2.08, p = .149), I2 suggest a moderate degree of heterogeneity existed across these two studies (I2 = 51.97%). This non-significant Q-statistic is likely a function of low statistical power (Higgins, Thompson, Deeks, & Altman, 2003). The same pattern of results was found with the Jindani (2015) study removed, though the overall ESs for PCL was somewhat reduced (PCL k = 8, ES = −.34, p = < .001, 95% CI [−.54, −.14]), though heterogeneity of ESs was no longer significant within the remaining 8 studies using the PCL (Q (7 df) = 9.39, p = .226, I2 = 0.00). These results were replicated using the Gleser and Olkin approach to dependent ESs.
3.1.3 Veteran Status
The majority of the studies examined complementary approaches for treating PTSD among veterans (k = 14). The remaining studies (k = 5) examined samples of nurses (1), refugees (1), cancer survivors (1), and women with interpersonal trauma histories (1). One study (Mitchell et al, 2014) was included as a non-veteran study; however, 9 out of 38 participants were veterans. Effect sizes across veteran/non-veteran samples were assessed. Both veteran (k = 14, ES = −.34, p = < .001, 95% CI [−.48, −.21]) and non-veteran studies (k = 5, ES = −.57, p = .066, 95% CI [−1.17, .04]) yielded moderate ESs, though the effects for non-veterans were only marginally significant. These ESs were not significantly different (Q (1 df) = .45, p = .502). Examined as subgroups, significant variability exists in the non-veteran studies (Q (4 df) = 18.20, p = .001; I2 = 80.37%), whereas the veteran studies were much less heterogeneous (Q (13 df) = 15.03 p = .305, I2= 0.00%). With the Jindani et al. (2015) study removed, the ES for non-veterans was not statistically significant (k = 4, ES = −.32, p = .197, 95% CI [−.81, 17]. Despite this, the two ESs did not significantly differ (Q (1 df) = .02, p = .891). Additionally, variability in the non-veteran group was only marginally significant (Q (3 df) = 7.32, p = .062) after removing the Jindani study, though I2 remained moderate (I2 = 62.00%). These results were replicated using the Gleser and Olkin (2009) approach to dependent ESs.
3.1.4 Active versus Non-active Control Condition
Another area of potential concern is the varied nature of the control conditions employed, with particular emphasis on active versus non-active control conditions. In the studies examined, 10 employed an active control condition (of which, 2 were the three arm studies), 8 employed a treatment-as-usual active control condition, and 3 employed a non-active wait-list control condition (one being the potential outlier study). Here, our interest lies in the potential differences among active (k = 16) and non-active (k = 3) control conditions1. Not surprisingly, the effect size for active controls was similar to the overall effect size and remained statistically significant (ES = −.34, p < .001, 95% CI [−.46, −.21]). The non-active controls, however, had a marginally significant effect size (ES = −.70, p = .085, 95% CI [−1.50, −.10]). Further, variability among the 16 active control conditions was non-significant (Q (15 df) = 20.74, p = .145; I2 = 0.00%) while significant variability remained among the 3 non-active control condition studies (Q (2 df) = 11.35, p = .003; I2 = 79.74%). With the Jindani et al. (2015) study removed, the ES for non-active control studies was not statistically significant (k = 2, ES = −.29, p = .331, 95% CI [−.87, 29]). Despite this, the two ESs did not significantly differ, either including (Q (1 df) = .78, p = .377) or excluding (Q (1 df) = .00, p = .960) the Jindani et al. (2015) study. Additionally, variability in the non-active control group studies was not statistically significant (Q (1 df) = 1.69, p = .194) after removing the Jindani study, though I2 remained moderate (I2 = 40.74%). These results were replicated using the Gleser and Olkin (2009) approach to dependent ESs.
3.1.5 Sample Size
There was a significant range of sample sizes used in the studies examined (14 through 191). Previous meta-analytic reviews have noted that small sample size is associated with higher ESs (Ioannidis, Cappelleri, & Lau, 1998; Slavin & Smith, 2009; Sterne, Gavaghan, & Egger, 2000). Here, we examined differences by sample size in those studies comprised of 30 or less (k = 5) versus those with more than 30 participants (k = 14; sample sizes totaled for 2 studies with dependent effect sizes). Both the small studies (ES = −.78, p < .001, 95% CI [−1.19, −.37]) and the larger studies (ES = −.33, p < .001, 95% CI [−.51, −.15]) yielded significant ESs. However, studies with smaller studies had marginally larger ES than those with larger sample sizes (Q (1 df) = 3.80, p = .051). With the Jindani study removed, ES for the larger studies was reduced but remained significant (k = 13, ES = −.28, p < .001, 95% CI [−.41, −.16] and smaller studies had significantly larger ES with the Jindani study omitted (Q (1 df) = 5.10, p = .024). These differences were no longer significant with samples of 40 or more defining the cut-point (successively increasing by 10). Again, these results were replicated with the Gleser and Olkin (2009) approach to dependent ESs.
4. Discussion
In this meta-analytic review, complementary mind and body health approaches for the treatment of PTSD were associated with small to moderate ESs. With a few exceptions, the results also suggest that there were no appreciable differences between the intervention types, studies using clinician administered or self-report as the primary measure of PTSD, or veteran vs. non-veteran samples. The ES for the studies that did not use the PCL or the CAPS (k = 2) was not significant, though this is likely a result of insufficient statistical power. Finally, the small to moderate effects of yoga on PTSD were comparable to mindfulness and meditation approaches, though the finding was only marginally significant.
4.1. Effect Sizes in Context
The current estimates are in line with previously published meta-analyses focused on similar intervention types and/or outcomes. For instance, Bisson, Roberts, Andrew, Cooper, and Lewis (2013) found that psychological therapies were effective in the treatment of adult PTSD. In their meta-analysis of RCTs, interventions were grouped according to individual trauma-focused CBT, EMDR, non-trauma-focused CBT, other therapies (including supportive therapies, non-directive counselling, psychodynamic therapy, present-centered therapy, and other complementary health approaches), group trauma-focused CBT, or group non-trauma-focused CBT and were compared to one another or to a waitlist or usual care group for the treatment of PTSD. Based on clinician rated PTSD symptomatology, individual trauma-focused CBT, EMDR, and non-trauma-focused CBT were each effective (k = 28, ES = −1.62, 95% CI [−2.03, −1.21]; k = 6, ES = −1.17, 95% CI [−2.04, −.30]; k = 4, ES = −1.22, 95% CI [−1.76, −.69], respectively) and found to be more effective than the remaining therapies. Each of the remaining therapies, however, were found to be more effective than treatment as usual (other treatments, k = 3, ES = −.58, 95% CI [−.96, −.20]; group trauma-focused CBT, k = 3, ES = −1.28, 95% CI [−2.25, −.31]). However, many of the studies analyzed were rated as being at “high” or “unclear” risk of bias and the authors assessed the quality of the evidence as very low. Strauss, Cavanagh, Oliver, and Pettman (2014), in a meta-analysis of RCTs of mindfulness-based approaches to the treatment of depression and anxiety in adults found significant between group benefits in symptom severity at post for mindfulness-based approaches compared to control (k = 12, ES = −.59, 95% CI [−1.06, −.12]). Here, however, effects were noted for RCTs with an inactive control group (k = 7, ES = −1.03, 95% CI [−1.66, −.40]) and not for RCTs with an active control group (k = 5, ES = .03, 95% CI [−.48, .54]). Finally, Haagen, Smid, Knipscheer, and Kleber (2015) examined predictors of ESs using metaregression techniques in 57 studies examining treatment for PTSD in soldiers and veterans. The overall ES was −1.12 (95% CI [−1.25, −.98]). These authors found exposure therapy and cognitive processing therapy to be more effective than EMDR and stress management therapy. Individual-only formats performed better than group format or a combination of group and individual format. There was a quadratic relationship between PTSD pretreatment severity levels and treatment outcome, indicating lower treatment gains at low and high baseline PTSD levels, when compared to moderate pretreatment levels.
4.2 Strengths and Limitations
Limitations of the study include the small number of studies available to conduct some of the moderator analyses. For instance, only 4 of the studies in the present study examined the effects of yoga, and heterogeneity in outcomes exists within these 4 studies. Also, we did not access patient-level data, and were therefore unable to evaluate if baseline PTSD severity or other individual level variables, like previous treatment experience, moderated the effects of complementary approaches on PTSD outcomes. For example, in a secondary analysis of MBSR for PTSD, Felleman et al. (2016) found that higher baseline PTSD predicted a greater rate of reduction in PTSD symptoms after MBSR. The analysis also does not assess remission rates, which precludes making a comparison of the complementary approaches to traditional PTSD interventions on this domain. Like previous meta-analyses, a small-sample bias exists in our study with larger ES’s associated with small sample studies – larger trials of the effects of meditation and yoga on PTSD and other symptoms continue to be needed. Finally, though many of the studies in this meta-analysis were rated as low risk of bias, several studies have high or unclear risk of bias, which suggests caution in interpreting results from these studies.
Notwithstanding these limitations, the findings suggest that complementary approaches to the treatment of PTSD that utilize meditation or yoga are warranted among veterans and non-veterans, with interventions yielding small to moderate effects on PTSD symptom reduction. The overall small to medium ES of −.39 should be considered in the context of larger ESs of −1.62 for trauma-focused CBT (e.g., CPT, PE), −1.17 for EMDR, and −1.22 for non-trauma focused CBT (Bisson et al., 2013) in the treatment of PTSD; however, our findings are comparable to medication management of PTSD (ES = .42), which is recommended as second-line treatment for PTSD (Watts et al., 2013; VA/DOD, 2017). Further, our findings are similar to those of mindfulness-based approaches for anxiety and depression (ES = −.59). Considered together, complementary health interventions increase patient choice and may be offered as a second-line treatment option for PTSD. Additionally, complementary health approaches may be more tolerable than trauma-focused interventions, as evidenced by drop-out rates in traditional PTSD treatment. Further research is needed to understand how these modalities complement traditional psychotherapy approaches, or affect various aspects of the disorder not addressed by traditional PTSD interventions.
5. Conclusions
Non-trauma focused, complementary health approaches have several advantages that increase feasibility for implementation. For example, they are usually delivered in a group format and encourage participants to take an active role. These modalities can also be delivered by certified instructors that do not need doctoral-level training. They can be augmented for home practice, as there is no need for highly specialized treatment equipment, making the treatment portable and allowing for wide dissemination. Further, participants are encouraged to incorporate the practices in all aspects of their lives, not just in the event of a maladaptive thought, which increases the frequency of use.
Findings from this meta-analysis provide rationale for ongoing research to pursue several important questions. For instance, a comparison of both completion rates and remission rates among PTSD interventions could inform the design of clinical trials to assess whether complementary approaches are best integrated with evidenced-based psychotherapy, sequenced before or after other interventions as adjunctive treatments, or for whom such complementary approaches suffice as stand-alone interventions for managing PTSD symptoms. Similarly, a comparison of treatment responder characteristics across treatment types could inform programmatic decisions leading to more personalized medicine. The findings here suggest efforts to move toward integrative approaches that leverage mind-body interventions for the management of PTSD warrant further study.
Funding: Dr. Gallegos is supported by the University of Rochester CTSA award number KL2 TR001999 from the National Center for Advancing Translational Sciences of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official view of the National Institutes of Health.
Supplementary Material
Table 1.
Study Eligibility Criteria
| Study Characteristics | Inclusion Criteria |
|---|---|
| Design | Randomized control trial |
| 10 as minimal sample size | |
| Population | Adults ≥18 with PTSD |
| PTSD using clinician or self-report measure | |
| Intervention | mind-body, meditation, tai chi, qi gong, yoga, mindfulness, mindfulness-based stress reduction, mindfulness-based cognitive therapy, mantram |
| Comparator | Any control |
| Database | PubMed; Medline EBSCO; PsychINFO |
| Years | 1946-2016 |
Footnotes
There were no differences between the active control conditions (k = 8, ES = −.32, p < .001, 95% CI [−.49, −.16], I2 = 0.01%) and the treatment-as-usual control conditions (k = 8, ES = −.36, p < .001, 95% CI [−.56, −.16], I2 = 0.00%) across effect sizes (Q (1 df) = .09, p = .759; I2 = 0.00%).
References
References marked with an asterisk indicate studies included in the meta-analysis.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Washington, DC: Author; 2013. [Google Scholar]
- Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice. 2003;10:125–143. doi: 10.1093/clipsy.bpg015. [DOI] [Google Scholar]
- Bisson JI, Roberts NP, Andrew M, Cooper R, Lewis C. Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database of Systematic Reviews. 2013;12:1–242. doi: 10.1002/14651858.CD003388.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis. Chichester, U.K: John Wiley & Sons; 2009. [DOI] [Google Scholar]
- *.Bormann JE, Thorp SR, Wetherell JL, Golshan S, Lang AJ. Meditation-based mantram intervention for veterans with posttraumatic stress disorder: A randomized trial. Psychological Trauma: Theory, Research, Practice, and Policy. 2013;5:259–267. doi: 10.1037/a0027522. [DOI] [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry. 2005;162:214–227. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- *.Bränström R, Kvillemo P, Moskowitz JT. A randomized study of the effects of mindfulness training on psychological well-being and symptoms of stress in patients treated for cancer at 6-month follow-up. International Journal of Behavioral Medicine. 2012;19:535–542. doi: 10.1007/s12529-011-9192-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Brooks JS, Scarano T. Transcendental meditation in the treatment of post-Vietnam adjustment. Journal of Counseling and Development. 1985;64:212–215. doi: 10.1002/j.1556-6676.1985.tb01078.x. [DOI] [Google Scholar]
- *.Carter JJ, Gerbarg PL, Brown RP, Ware RS, D’Ambrosio C, Anand L, Katzman MA. Multi-component yoga breath program for Vietnam veteran post-traumatic stress disorder: Randomized controlled trial. Journal of Traumatic Stress Disorders and Treatment. 2013;2:1–10. doi: 10.4172/2324-8947.1000108. [DOI] [Google Scholar]
- Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: United States, 2002–2012. National Health Statistics Reports. 2015;79:1–16. [PMC free article] [PubMed] [Google Scholar]
- *.Davis L. Unpublished manuscript (unpublished) [Google Scholar]
- Durlak JA. How to select, calculate, and interpret effect sizes. Journal of Pediatric Psychology. 2009;34:917–928. doi: 10.1093/jpepsy/jsp004. [DOI] [PubMed] [Google Scholar]
- Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Figley CR, Sprenkle DH. Delayed stress response syndrome: Family therapy indications. Journal of Marital and Family Therapy. 1978;4:53–60. [Google Scholar]
- Gallegos AM, Cross W, Pigeon WR. Mindfulness-based stress reduction for veterans exposed to military sexual trauma: Rationale and implementation considerations. Military Medicine. 2015;180:684–689. doi: 10.7205/MILMED-D-14-00448. [DOI] [PubMed] [Google Scholar]
- Gleser LJ, Olkin I. Stochastically dependent effect sizes. In: Cooper H, Hedges LV, Valentine JC, editors. The Handbook of Research Synthesis and Meta-Analysis. Second. New York, New York: Russell Sage Foundation; 2009. pp. 357–376. [Google Scholar]
- Hedges LV, Olkin I. Statistical methods for meta-analysis. New York: Academic Press; 1985. [Google Scholar]
- *.Heffner KL, Crean HF, Kemp JE. Meditation programs for veterans with posttraumatic stress disorder: Aggregate findings from a multi-site evaluation. Psychological Trauma: Theory, Research, Practice, and Policy. 2016;8:365. doi: 10.1037/tra0000106. [DOI] [PubMed] [Google Scholar]
- Haagen JFG, Smid GE, Knipscheer JW, Kleber RJ. The efficacy of recommended treatments for veterans with PTSD: A metaregression analysis. Clinical Psychology Review. 2015;40:184–194. doi: 10.1016/j.cpr.2015.06.008. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Altman DG, Sterne JAC. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. The Cochrane Collaboration; 2011. [updated March, 2011] [DOI] [Google Scholar]
- Higgins JPT, Deeks JJ. Chapter 7: Selecting studies and collecting data. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; 2011. (updated March 2011) [DOI] [Google Scholar]
- Higgins JPT, Meeks JJ, Altman (Writers) DG, Higgins JPT, Green (Directors) S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. The Cochrane Collaboration; 2011. Chapter 16: Special topics in statistics. [updated March, 2011] [DOI] [Google Scholar]
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoskins M, Pearce J, Bethell A, Dankova L, Barbui C, Tol WA, Bisson JI. Pharmacotherapy for post-traumatic stress disorder: Systematic review and meta-analysis. The British Journal of Psychiatry: The Journal of Mental Science. 2015;206:93–100. doi: 10.1192/bjp.bp.114.148551. [DOI] [PubMed] [Google Scholar]
- Ioannidis JP, Cappelleri JC, Lau J. Issues in comparisons between meta-analyses and large trials. JAMA. 1998;279:1089–1093. doi: 10.1001/jama.279.14.1089. [DOI] [PubMed] [Google Scholar]
- *.Jindani F, Turner N, Khalsa SBS. A yoga intervention for posttraumatic stress: A preliminary randomized control trial. Evidence-Based Complementary and Alternative Medicine. 2015 doi: 10.1155/2015/351746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Kearney DJ, McDermott K, Malte C, Martinez M, Simpson TL. Effects of participation in a mindfulness program for veterans with posttraumatic stress disorder: A randomized controlled pilot study. Journal of Clinical Psychology. 2013;69:14–27. doi: 10.1002/jclp.21911. [DOI] [PubMed] [Google Scholar]
- Kearney DJ, Simpson TL. Broadening the approach to posttraumatic stress disorder and the consequences of trauma. JAMA. 2015;314:453–455. doi: 10.1001/jama.2015.7522. [DOI] [PubMed] [Google Scholar]
- *.Kim SH, Schneider SM, Bevans M, Kravitz L, Mermier C, Qualls C, Burge MR. PTSD symptom reduction with mindfulness-based stretching and deep breathing exercise: randomized controlled clinical trial of efficacy. The Journal of Clinical Endocrinology & Metabolism. 2013;98:2984–2992. doi: 10.1210/jc.2012-3742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SH, Schneider SM, Kravitz L, Mermier C, Burge MR. Mind-body practices for posttraumatic stress disorder. Journal of Investigative Medicine. 2013;61:827–834. doi: 10.2310/JIM.0b013e3182906862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang AJ, Strauss JL, Bomyea J, Bormann JE, Hickman SD, Good RC, Essex M. The theoretical and empirical basis for meditation as an intervention for PTSD. Behavior Modification. 2012;36:759–786. doi: 10.1177/0145445512441200. [DOI] [PubMed] [Google Scholar]
- Lee DJ, Schnitzlein CW, Wolf JP, Vythilingam M, Rasmusson AM, Hoge CW. Psychotherapy versus pharmacotherapy for posttraumatic stress disorder: Systemic review and meta-analyses to determine first-line treatments. Depression and Anxiety. 2016;33:792–806. doi: 10.1002/da.22511. [DOI] [PubMed] [Google Scholar]
- Lipsey MW, Hurley S. Design sensitivity: Statistical power for applied experimental research. In: Bickman L, Rog DJ, editors. The SAGE handbook of applied social research methods. 2nd. Thousand Oaks, California: SAGE Publications, Inc; 2009. pp. 44–77. [DOI] [Google Scholar]
- Lipsey MW, Wilson DV. Practical Meta-Analysis. Vol. 49. Thousand Oaks, CA: Sage Publications; 2001. [Google Scholar]
- *.Mitchell KS, Dick AM, DiMartino DM, Smith BN, Niles B, Koenen KC, Street A. A pilot study of a randomized controlled trial of yoga as an intervention for PTSD symptoms in women. Journal of Traumatic Stress. 2014;27:1–8. doi: 10.1002/jts.21903. [DOI] [PubMed] [Google Scholar]
- *.Nakamura Y, Lipschitz DL, Landward R, Kuhn R, West G. Two sessions of sleep-focused mind–body bridging improve self-reported symptoms of sleep and PTSD in veterans: A pilot randomized controlled trial. Journal of Psychosomatic Research. 2011;70:335–345. doi: 10.1016/j.jpsychores.2010.09.007. [DOI] [PubMed] [Google Scholar]
- *.Niles BL, Klunk-Gillis J, Ryngala DJ, Silberbogen AK, Paysnick A, Wolf EJ. Comparing mindfulness and psychoeducation treatments for combat-related PTSD using a telehealth approach. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4:538. doi: 10.1037/a0026161. [DOI] [Google Scholar]
- Orwin RG. A fail-safe N for effect size in meta-analysis. Journal of Educational Statistics. 1983;8:157–159. doi: 10.2307/1164923. [DOI] [Google Scholar]
- *.Polusny MA, Erbes CR, Thuras P, Moran A, Lamberty GJ, Collins RC, Lim KO. Mindfulness-based stress reduction for posttraumatic stress disorder among veterans: A randomized clinical trial. JAMA. 2015;314:456–465. doi: 10.1001/jama.2015.8361. [DOI] [PubMed] [Google Scholar]
- *.Possemato K, Bergen-Cico D, Treatman S, Allen C, Wade M, Pigeon W. A randomized clinical trial of primary care brief mindfulness training for veterans with PTSD. Journal of Clinical Psychology. 2016;72:179–193. doi: 10.1002/jclp.22241. [DOI] [PubMed] [Google Scholar]
- Rosenthal R. The “file-drawer problem” and tolerance for null results. Psychological Bulletin. 1979;86:638–641. [Google Scholar]
- Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH. Nonresponse and dropout rates in outcome studies on PTSD: Review and methodological considerations. Psychiatry. 2008;71:134–168. doi: 10.1521/psyc.2008.71.2.134. [DOI] [PubMed] [Google Scholar]
- *.Seppälä EM, Nitschke JB, Tudorascu DL, Hayes A, Goldstein MR, Nguyen DT, Davidson RJ. Breathing-based meditation decreases posttraumatic stress disorder symptoms in US military veterans: A randomized controlled longitudinal study. Journal of Traumatic Stress. 2014;27:397–405. doi: 10.1002/jts.21936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavin RE, Smith D. The relationship between sample sizes and effect sizes in systematic reviews in education. Educational Evaluation and Policy Analysis. 2009;31:500–506. doi: 10.3102/016237370935236. [DOI] [Google Scholar]
- Steenkamp MM, Litz BT, Hoge CW, Marmar CR. Psychotherapy for military-related PTSD: a review of randomized clinical trials. JAMA. 2015;314:489–500. doi: 10.1001/jama.2015.8370. [DOI] [PubMed] [Google Scholar]
- Sterne J, Gavaghan D, Egger M. Publication and related bias in meta-analysis: Power of statistical tests and prevalence in the literature. Journal of Clinical Epidemiology. 2000;53:1119–1129. doi: 10.1016/S0895-4356(00)00242-0. [DOI] [PubMed] [Google Scholar]
- Strauss JL. Efficacy of complementary and alternative medicine therapies for posttraumatic stress disorder. U.S. Department of Veterans Affairs, Health Services Research & Development Service; 2011. Retreived from http://www.hsrd.research.va.gov/publications/esp/cam-ptsd.pdf. [PubMed] [Google Scholar]
- Strauss C, Cavanagh K, Oliver A, Pettman D. Mindfulness-based interventions for people diagnosed with a current episode of an anxiety or depressive disorder: A meta-analysis of randomised controlled trials. PloS One. 2014;9:e96110. doi: 10.1371/journal.pone.0096110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tollefson DR, Webb K, Shumway D, Block SH, Nakamura Y. A mind-body approach to domestic violence perpetrator treatment: Program overview and preliminary outcomes. Journal of Aggression, Maltreatment & Trauma. 2009;18:17–45. doi: 10.1080/10926770802610657. [DOI] [Google Scholar]
- VA/DoD (Department of Veterans Affairs/Department of Defense) VA/DoD Clinical practice guideline for the management of posttraumatic stress and acute stress disorder, version 3.0. Washington, DC: Veterans Health Administration, Department of Defense; 2017. [Google Scholar]
- *.van der Kolk BA, Stone L, West J, Rhodes A, Emerson D, Suvak M, Spinazzola J. Yoga as an adjunctive treatment for posttraumatic stress disorder: A randomized controlled trial. The Journal of Clinical Psychiatry. 2014;75:599–565. doi: 10.4088/JCP.13m08561. [DOI] [PubMed] [Google Scholar]
- Veroniki AA, Jackson D, Viechtbauer W, Bender R, Bowden J, Knapp G, Salanti G. Methods to estimate the between-study variance and its uncertainty in meta-analysis. Research Synthesis Methods. 2016;7:55–79. doi: 10.1002/jrsm.1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viechtbauer W. Conducting meta-analyses in R with the metafor package. Journal of Statistical Software. 2010;36:1–48. doi: 10.18637kss/v036.i03. [DOI] [Google Scholar]
- Viechtbauer W, Cheung MW. Outlier and influence diagnostics for meta-analysis. Research Synthesis Methods. 2010;1:112–125. doi: 10.1002/jrsm.11. [DOI] [PubMed] [Google Scholar]
- *.Wahbeh H, Goodrich E, Goy E, Oken BS. Mechanistic pathways of mindfulness meditation in combat veterans with posttraumatic stress disorder. Journal of Clinical Psychology. 2016;72:365–383. doi: 10.1002/jclp.22255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts BV, Schnurr PP, Mayo L, Young-Xu Y, Weeks WB, Friedman MJ. Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. The Journal of Clinical Psychiatry. 2013;74(6):e541–50. doi: 10.4088/JCP.12r08225. [DOI] [PubMed] [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility; Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies; San Antonio, TX. Oct, 1993. [Google Scholar]
- Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychological Assessment. 1999;11:124–133. doi: 10.1037//1040-3590.11.2.124. [DOI] [Google Scholar]
- Weiss DS, Marmar CR. The Impact of Event Scale – Revised. In: Wilson J, Keane TM, editors. Assessing psychological trauma and PTSD. New York: Guilford; 1996. pp. 399–411. [Google Scholar]
- Wilson DB, Gottfredson DC, Najaka SS. School-based prevention of problem behaviors: A meta-analysis. Journal of Quantitative Criminology. 2001;17:247–272. dx.doi.org/10.1023/A:1011050217296. [Google Scholar]
- Wilson DB, Lipsey MW. School-based intervention for aggressive and disruptive behavior: Update of a meta-analysis. American Journal of Preventive Medicine. 2007;33:S130–S143. doi: 10.1016/j.amepre.2007.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


