Abstract
Among men who have sex with men (MSM), those with a diagnosis of syphilis or other rectal sexually transmitted infections (STIs) are at a higher risk for human immunodeficiency virus acquisition, which is concerning given the large increase in recently reported syphilis cases in the United States. We have developed the first nonhuman primate model for rectally transmitted syphilis by exposing simian/human immunodeficiency virus–infected and naive rhesus macaques to Treponema pallidum in the rectum. All animals showed mucosal lesions, systemic dissemination, and seroconversion (treponemal antibodies). This model would be valuable for studying the manifestations of and interventions for T. pallidum infection, with and without human immunodeficiency virus coinfection.
Keywords: Rectal syphilis, nonhuman primate model, rhesus, SHIV, HIV, Treponema pallidum, coinfection, MSM
Syphilis can increase the risk of mucosal human immunodeficiency virus (HIV) acquisition and transmission in heterosexuals and men who have sex with men (MSM) through inflammation, ulcerations, and by elevating viral loads in the blood and genital secretions [1–5]. Given the rise in rectal syphilis cases, the current syphilis epidemic has primarily affected MSM. Rectal syphilis has been less studied in animals and humans with respect to natural history because of the asymptomatic nature of rectal lesions. Here, we report the development of the first nonhuman primate (NHP) model for rectally transmitted syphilis. Past researchers, including Marra et al, who inoculated macaques intradermally in the back [6], have demonstrated macaque susceptibility to syphilis. Here, we hypothesized that rectal submucosal exposures with similar Treponema pallidum subspecies pallidum inoculum sizes, albeit with procedural adjustments, would cause syphilis in macaques.
MATERIALS AND METHODS
Animals
All animal procedures were approved by the Centers for Disease Control and Prevention (CDC) Institutional Animal Care and Use Committee. Seven Indian rhesus macaques aged 6–12 years (median, 9 years) were housed at the CDC under the care of veterinarians in accordance with the Guide for the Care and Use of Laboratory Animals.
T. pallidum Infections
T. pallidum Nichols strain was propagated in rabbits as described elsewhere [6] and delivered rectally to 1 anesthetized simian/human immunodeficiency virus (SHIVSF162p3)–naive macaque and 2 SHIV-infected macaques (Table 1). Organisms were injected submucosally, using a 29-gauge needle, approximately 5 cm beyond the anorectal opening. A 0.2-mL volume was administered per site, containing up to 108 organisms/mL/site diluted with normal rabbit serum. A third SHIV-infected animal (animal 3) was exposed to T. pallidum by a needleless syringe immediately following mucosal irritation with a cytobrush (Medscand Medical, Hollywood, FL). Additionally, we administered up to 107T. pallidum/mL (in a 0.2-mL volume per site) intradermally at 4 sites, as described elsewhere [6], into the backs of 1 control SHIV-naive macaques and 2 SHIV-infected macaques to check the infectivity of the bacterial stock (Table 1). All animals but 1 were inoculated with thawed stock recently propagated and frozen at the University of Washington (in the laboratory of S. A. Lukehart) [6]. One SHIV-infected animal (animal 1), received inoculum from a 3-year-old CDC stock. Using a contrast medium, Omnipaque 300 (GE Healthcare, Milwaukee, WI) and radiography, we documented injection sites and dispersal of administered contents in the rectal compartment.
Table 1.
Characteristics of Treponema pallidum–Infected Rhesus Macaques
| Animal | Sex | SHIVa Status | Route of T. pallidum Exposure | Time to First Lesions, d | Time to Ulceration, d | Persistence, d | Lesion Size, mmb | First RPR Reactivity, wk | Highest RPR Titer | Time to First T. pallidum PA Reactivity, wk | Time to First TS Reactivity, wk | SHIVa Viremia Level,c Copies/mL | CD4+ T Cells Count,c Cells/µL |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | Infected | Rectum, submucosal | 16d | 16 | 16 | ND | 22 | 1:4 | 6 | 10 | 13 000 | 40 |
| 2 | Male | Infected | Rectum, submucosal | 3 | 7 | 14 | ND | 24 | 1:1 | 5 | 5 | <50 | 1338 |
| 3 | Female | Infected | Rectum, needlelesse | 6 | 6 | 20 | ND | Neg | Neg | 8 | 9 | <50 | 340 |
| 4 | Male | Naive | Rectum, submucosal | 6 | 6 | 13 | ND | 8 | 1:8 | 6 | 9 | NA | 1054 |
| 5 | Female | Infected | Back, intradermal | 3 | 3 | 119 | 25 | 4 | 1:4 | 1 | 5 | <50 | 1071 |
| 6 | Male | Infected | Back, intradermal | 3 | 3 | 133 | 17 | 12 | 1:8 | 6 | 9 | 759 | 1742 |
| 7 | Male | Naive | Back, intradermal | 3 | 6 | 60 | 12 | 6 | 1:1 | 6 | 8 | NA | 1148 |
Abbreviations: NA, not applicable; ND, not determined; Neg, negative; RPR, rapid plasma reagin assay; PA, particle agglutination assay; TS, Trep-Sure.
aSimian/human immunodeficiency virus (SHIV) is a molecular hybrid of simian immunodeficiency virus (SIV) and human immunodeficiency virus type 1 (HIV-1) that demonstrates SIV’s replicative capacity in macaques, as well as the ability to express HIV-1 envelope proteins
bMaximum size recorded.
cMedian values, based on the readings taken throughout the study.
dIn animal 1, the rectal lesions appeared much later (on day 16) than in other animals, and this could be a result of using a 3-year-old T. pallidum stock (the only stock available at the time) to infect this specific animal.
eImmediately following cytobrush application.T. pallidum was detected by polymerase chain reaction in blood specimens from animals 1 and 5 after lesion development but was undetected in other animals. None of the animals had T. pallidum or lymphocytes detected in cerebrospinal fluid specimens.
Experimental Design and Sampling
Animals were sedated and examined for clinical manifestations of syphilis twice weekly until no additional rectal or intradermal lesions were observed. Rectal lesions were documented using the GIF-XP190N endoscope and Evis Exera III CV-190 processor (Olympus, Center Valley, PA). Animals underwent overnight fasting and received 2 tablets of bisacodyl (Dulcolax; Boehringer Ingelheim Pharmaceuticals, Ridgefield, CT) and psyllium wafers (Metamucil; Proctor & Gamble, Cincinnati, OH) 12–18 hours before the procedure as a cathartic. Immediately prior to endoscopy, 2–3 warm water enemas were performed. Rectal and blood samples were collected before (at baseline) and twice a week for 30 weeks after T. pallidum exposure. From week 18 after exposure, cerebrospinal fluid (CSF) specimens were collected from the cisterna magna with a 20–25-gauge 3.8-cm (1.5-inch) needle every 2 weeks from all animals to evaluate the presence of lymphocytes and T. pallidum. Six months after rectal exposure to T. pallidum, multiple tissue and organ samples as well as vitreous humor, blood, and CSF specimens were collected from 1 euthanized SHIV-infected animal (animal 1) to assess dissemination and disease progression.
Serologic Analysis, Flow Cytometry, and Polymerase Chain Reaction (PCR) Analysis
Serum antibody responses were determined by rapid plasma reagin assay (RPR; Arlington Scientific, Springvale, UT), T. pallidum particle agglutination assay (Fujirebio, Japan), Trep-Sure enzyme immunoassay (Trinity Biotech, Jamestown NY), and Syphilis Health Check (Trinity Biotech, Jamestown NY), as per the manufacturer’s instructions. CD4+ T-lymphocyte levels of all animals, including SHIV-naive animals, were monitored by flow cytometry at baseline and over time after infection. Levels of plasma SHIV RNA and T. pallidum in the CSF and blood were measured by PCR analysis [7–9]. PCR analysis for detection of T. pallidum targeted the gene encoding DNA polymerase I (ie, polA) in T. pallidum, with the gene encoding human ribonuclease P as an internal control [8].
Immunohistochemical (IHC) Staining
Skin and rectal lesion biopsy specimens and necropsy tissue samples were assessed histopathologically and screened by IHC staining for T. pallidum, using a rabbit polyclonal antibody (Abcam, Cambridge, MA) raised against Borrelia burgdorferi, as per the manufacturer’s instructions. We have verified, using known clinical samples, the ability of this antibody to detect T. pallidum. The presence of T. pallidum was further confirmed in our samples with an in-house rabbit polyclonal antibody raised against T. pallidum. Inflammatory cell infiltration was assessed by hematoxylin-eosin staining [10].
RESULTS
Rectal Injections
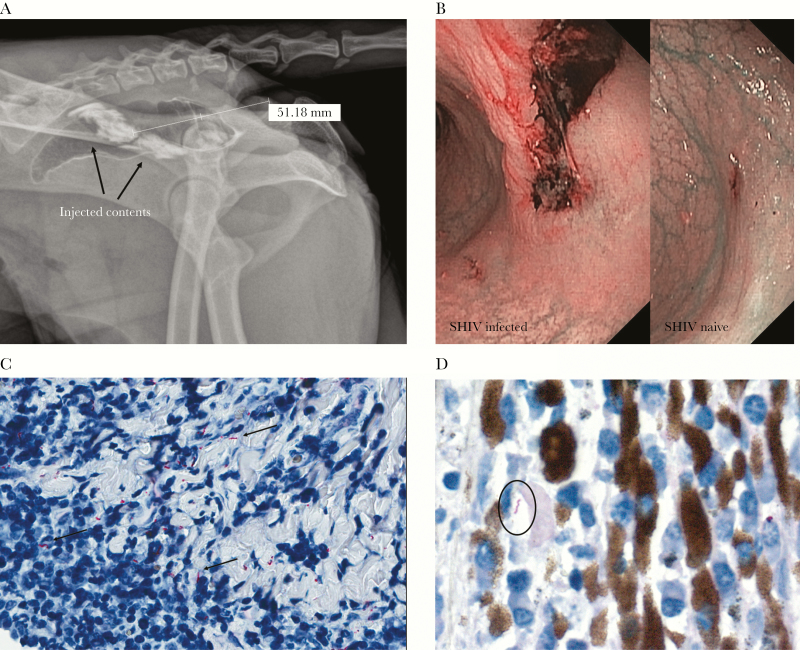
Since this was the first time T. pallidum was submucosally inoculated in the rectum of NHPs, it was important to understand the location and dispersion of the injected contents, which could guide endoscopic examination of lesions. The radiographs showed the location of the inocula at approximately 5 cm beyond the anorectal opening, with the injected contents dispersed in a diameter of approximately 2 cm (Figure 1A).
Figure 1.
A nonhuman primate model for rectally acquired syphilis. A, Radiograph showing the location and dispersion of submucosally injected contents in the rectum of rhesus macaques (2 injections in a 0.2-mL volume; animal 1 in Table 1). Radiography was done separately, not by mixing the contrast medium with Treponema pallidum. The injections were administered approximately 5 cm beyond the anorectal opening. B, Narrow-band imaging showing representative pictures of ulcerated rectal lesions in the rectum of simian/human immunodeficiency virus (SHIV)–infected (day 7; animal 2) and SHIV-naive (day 6; animal 4) macaques. C, Immunohistochemical staining using a commercial rabbit polyclonal antibody raised against Borrelia burgdorferi showing T. pallidum dissemination within lymphoplasmacytic conjunctival infiltrates of animal 1 (400× original magnification). D, Immunohistochemical staining using T. pallidum–specific rabbit polyclonal antibody showing T. pallidum dissemination within lymphoplasmacytic infiltrates in the ciliary body of the eye of animal 1 (630× original magnification). In contrast to biopsy specimens from back lesions, none of the biopsy specimens from rectal lesions showed the presence of T. pallidum by polymerase chain reaction analysis or immunohistochemical staining. We believe this reflects the challenge of sampling specific sites in the macaque rectum without proper visualization.
Syphilitic Lesions
All T. pallidum–exposed animals showed syphilitic lesions (Figure 1B and Table 1). The SHIV-infected animals developed rectal lesions between days 3 and 16 after exposure, while the SHIV-naive animal (animal 4) developed rectal lesions at day 6. Ulceration was observed within 3 days of lesion development in all animals. The lesions persisted for 3 weeks; some ulcers healed within 3 days with persistent erythema (Supplementary Figure 1). The SHIV-infected and naive animals inoculated intradermally in the back developed cutaneous lesions at day 3 after exposure. However, the back lesions persisted longer in the SHIV-infected animals (for up to 120 days) as compared to the SHIV-naive animal (animal 7; 60 days). Also, back lesions were larger in the SHIV-infected animals (up to 25 mm in diameter) as compared to those in SHIV-naive animal (up to 12 mm; Table 1 and Supplementary Figure 2).
CD4+ T-Cell Levels, Viremia Levels, and Antibody Responses
At the time of T. pallidum exposure and over the course of syphilis, CD4+ T-cell levels of animals were >200 cells/µL, except for animal 1, which had low CD4+ T-cell counts and a median plasma viremia level of approximately 13 000 viral copies/mL throughout the study (Table 1). In this animal, plasma viral loads increased transiently, from approximately 25 000 to approximately 63 000 copies/mL, after T. pallidum exposure but fell to preexposure levels within 1 week (data not shown). All other SHIV-infected animals had low or undetectable viral loads (Table 1). All animals showed serologic evidence of syphilis. Serum RPR reactivity was evident in the SHIV-uninfected animal (animal 4) at week 8 following rectal exposure (Table 1), peaked at week 13 at titers of 1:8, and then plateaued. In contrast, the RPR test was nonreactive in 1 SHIV-infected animal (animal 3) and minimally reactive in the remaining 2 SHIV-infected animals, developing reactivity only between weeks 22 and 24 following rectal T. pallidum exposure. All rectally inoculated animals became serum T. pallidum particle agglutination assay reactive by 8 weeks (median, 6 weeks) after T. pallidum infection, and titers plateaued between weeks 14 and 17 (Supplemental Figure 3). The peak T. pallidum particle agglutination assay titers in SHIV-infected animals were lower than that of the naive animal. All animals inoculated in the back became serum T. pallidum particle agglutination assay reactive by week 6, with 1 animal (SHIV infected) showing reactivity by week 1 (median: 6 weeks). It took a median of 7 weeks for rectally exposed animals to show Syphilis Health Check reactivity, while animals inoculated intradermally took a median of 2 weeks. It took a median of 9 weeks for both rectally and intradermally exposed animals to show Trep-Sure reactivity.
Histopathologic Examination and T. pallidum Detection
Histopathological examination of 4-mm punch biopsy samples from the back showed lymphocytic dermal infiltration and the presence of T. pallidum (Supplementary Figure 4), but IHC staining did not detect T. pallidum in the smaller (approximately 1-mm) pinch rectal biopsy specimens (Figure 1). Similarly, T. pallidum was detected by PCR analysis in the larger back biopsy specimens but not in the rectal ones. At 6 months, the immunocompromised SHIV-infected rhesus macaque (animal 1; Table 1) had a reduced appetite, became lethargic, and was euthanized; T. pallidum was detected by PCR analysis in the vitreous humor of both eyes. Ocular histologic analysis showed T. pallidum within lymphoplasmacytic inflammatory infiltrates in the conjunctiva and ciliary body (Figure 1C and 1D). IHC staining of brain sections did not show T. pallidum but revealed minimal, focal, and perivascular meningeal mononuclear infiltrates. T. pallidum was not detected by PCR analysis in specimens from the brain, CSF, rectum, heart, or other tissues of this animal.
DISCUSSION
Here, we describe the first NHP model for rectally acquired syphilis. Currently, the rabbit is the model of choice for propagating T. pallidum and studying syphilis pathogenesis and immunity. To our knowledge, there are no reports of rabbit studies involving experimental T. pallidum infection via the rectal route. Although the rabbit model closely reflects human infection, there are several advantages to the rhesus model, including its relatedness to humans and availability of better immunological reagents, which makes it possible to perform more complex assays. Moreover, an NHP model is invaluable for studies investigating the interplay between T. pallidum and HIV. We showed establishment of T. pallidum infection in SHIV-infected and naive rhesus macaques by submucosal rectal injections and also by T. pallidum exposure immediately following rectal cytobrush application, designed to mirror microabrasions occurring during unprotected anal intercourse. In addition to infecting the macaques rectally, we inoculated control animals intradermally in the back, as previously described [6], to confirm infectivity of bacterial stocks in macaques and compare immune responses.
Rectal lesions in our SHIV-infected animals appeared larger and developed into more-severe ulcerated chancres as compared to those in the SHIV-naive animal. This was also observed in the back lesions, consistent with what Marra et al showed [6], except that back lesions in their rhesus macaques were smaller and did not persist as long as those in our study despite the use of similar doses. They observed lesions in simian immunodeficiency virus (SIV)–infected animals up to 11 mm in diameter, persisting for 38 days. Here, lesions in the SHIV-infected animals were up to 25 mm in diameter, persisting for up to 102 days. However, their animals were SIV-infected and juvenile (2–3 years old), compared with ours, which were older (median age, 9 years) and infected with a less pathogenic virus (ie, SHIV). In rabbits, ulcerative lesions from T. pallidum Nichols strain were observed as early as 7 days after intradermal injections, with a mean maximum lesion diameter (±SD) of 14.7 ± 1.91 mm [11].
The presence of severe and long-lasting rectal lesions potentially enhances the risk of other infections, including HIV infection. The period of greatest vulnerability to rectal HIV acquisition is likely when lesions are present and ulcerating. In our study, rectal lesions persisted for up to 3 weeks, and mucosal surfaces continued to appear inflamed for some time longer, suggesting that the potential window of vulnerability may be >4 weeks following rectal T. pallidum infection. Use of the RPR test, a nontreponemal assay that detects lipoidal antibodies from host tissue damage, in our SHIV-infected animals with rectal T. pallidum exposure yielded either nonreactive or minimally reactive findings as compared to findings for the SHIV-naive animal. But we observed the opposite in animals intradermally exposed to T. pallidum in the back, perhaps a function of the extent of damage to the immune system [12].
This rectal T. pallidum NHP model can thus potentially be used to study manifestations of T. pallidum infections and interventions for syphilis, such as vaccines or novel antibiotic prophylaxis modalities, with or without an HIV coinfection, to mirror the pathogenesis of rectal acquisition among MSM [1–5]. Additionally, it could be used in a repeat low-dose SHIV challenge study to determine whether HIV biomedical interventions can protect macaques from SHIV acquisition despite the presence of STIs like syphilis [1, 13]. Rekart et al recently hypothesized that antiretroviral therapy could alter host immunity so that the risk of syphilis is increased [14]. Their conclusion was speculative, but our NHP model could be used to assess this possibility.
In this study, histopathological assessment of necropsy tissues showed lymphoplasmacytic infiltration and T. pallidum dissemination in parts of the eye in a SHIV-infected animal. These are signs of ocular syphilis that, in humans, can be a manifestation of early syphilis [15] and may be associated with neurosyphilis; T. pallidum infection of the brain and spinal cord is commonly seen in individuals not receiving syphilis treatment, especially in the context of HIV coinfection [12]. This macaque model is being further refined and modified to develop vaginal and penile NHP models for syphilis. Such models will provide a critical means to study the effects of SHIV and T. pallidum coinfection in macaques, which show greater similarities to humans than the rabbit model.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Acknowledgments. We thank David Garber, for programmatic support; Shanon Ellis and Kristen Kelley, for animal procedure assistance; our veterinarians and colleagues, especially Sarah Genzer in the Comparative Medicine Branch, for help with macaque-related work; Sheila Lukehart, Christina Marra, and Barbara Molini (University of Washington), for T. pallidum stocks and helpful input; Tamanna Ahmed, for laboratory support; George Khalil, for help with statistical analyses; and Janet Harouse, Cecilia Cheng-Mayer, Ranajit Pal (National Institutes of Health [NIH] AIDS Reagent Program, National Institute of Allergy and Infectious Diseases [NIAID], NIH) and the Division of AIDS, NIAID, NIH, for SHIV SF162P3.
Disclaimer. The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention. Use of trade names is for identification only and does not imply endorsement by the Department of Health and Human Services, the Public Health Service, or the Centers for Disease Control and Prevention.
Financial support. This work was supported by the Centers for Disease Control and Prevention and by the National Institutes of Health and the CDC (interagency agreement AAI 12041-001-03001).
Potential conflicts of interest. All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Solomon MM, Mayer KH, Glidden DV et al. Syphilis predicts HIV incidence among men and transgender women who have sex with men in a preexposure prophylaxis trial. Clin Infect Dis 2014; 59:1020–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ward H, Rönn M. Contribution of sexually transmitted infections to the sexual transmission of HIV. Curr Opin HIV AIDS 2010; 5:305–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sexton J, Garnett G, Røttingen JA. Metaanalysis and metaregression in interpreting study variability in the impact of sexually transmitted diseases on susceptibility to HIV infection. Sex Transm Dis 2005; 32:351–7. [DOI] [PubMed] [Google Scholar]
- 4. Jarzebowski W, Caumes E, Dupin N et al. Effect of early syphilis infection on plasma viral load and CD4 cell count in human immunodeficiency virus-infected men: results from the FHDH-ANRS CO4 cohort. Arch Intern Med 2012; 172:1237–43. [DOI] [PubMed] [Google Scholar]
- 5. Fox J, Fidler S. Sexual transmission of HIV-1. Antiviral Res 2010; 85:276–85. [DOI] [PubMed] [Google Scholar]
- 6. Marra CM, Handsfield HH, Kuller L, Morton WR, Lukehart SA. Alterations in the course of experimental syphilis associated with concurrent simian immunodeficiency virus infection. J Infect Dis 1992; 165:1020–5. [DOI] [PubMed] [Google Scholar]
- 7. Kennedy EJ, and Creighton ET.. Darkfield microscopy for the detection and identification of Treponema pallidum. In: A manual of tests for syphilis. Washington, DC: American Public Health Association, 1998:119–34. [Google Scholar]
- 8. Chen CY, Chi KH, George RW et al. Diagnosis of gastric syphilis by direct immunofluorescence staining and real-time PCR testing. J Clin Microbiol 2006; 44:3452–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vishwanathan SA, Aubert RD, Morris MR et al. A Macaque model for rectal lymphogranuloma venereum and non-lymphogranuloma venereum Chlamydia trachomatis: impact on rectal simian/human immunodeficiency virus acquisition. Sex Transm Dis 2017; 44:551–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shieh WJ, Blau DM, Denison AM et al. 2009 pandemic influenza A (H1N1): pathology and pathogenesis of 100 fatal cases in the United States. Am J Pathol 2010; 177:166–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lukehart SA, Baker-Zander SA. Roxithromycin (RU 965): effective therapy for experimental syphilis infection in rabbits. Antimicrob Agents Chemother 1987; 31:187–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Karp G, Schlaeffer F, Jotkowitz A, Riesenberg K. Syphilis and HIV co-infection. Eur J Intern Med 2009; 20:9–13. [DOI] [PubMed] [Google Scholar]
- 13. Hoornenborg E, Prins M, Achterbergh RCA et al. Acquisition of wild-type HIV-1 infection in a patient on pre-exposure prophylaxis with high intracellular concentrations of tenofovir diphosphate: a case report. Lancet HIV 2017; 4:e522–8. [DOI] [PubMed] [Google Scholar]
- 14. Rekart ML, Ndifon W, Brunham RC et al. A double-edged sword: does highly active antiretroviral therapy contribute to syphilis incidence by impairing immunity to Treponema pallidum?Sex Transm Infect 2017; 93:374–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ho EL, Lukehart SA. Syphilis: using modern approaches to understand an old disease. J Clin Invest 2011; 121:4584–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.