Abstract
Background
Between 15 and 20% of prevalent cases of chronic obstructive pulmonary disease (COPD) have been attributed to occupational exposures to vapours, gases, dusts and fumes. Dust at construction sites is still a challenge, but no overview exists of COPD among construction workers.
Aims
To assess the occurrence of COPD among construction workers.
Methods
We performed a systematic search in PubMed and Embase between 1 January 1990 and 31 August 2016 in order to identify epidemiological studies with a risk estimate for either COPD morbidity/mortality or a spirometry-based definition of airway obstruction among workers in the construction industry. The authors independently assessed studies to determine their eligibility and performed a quality assessment of the included papers.
Results
Twelve studies were included. Nine studies found a statistically significant association between COPD and work in the construction industry, although only among never-smokers in one study and only for the period after 2000 in another study. One study found that the annual decline in forced expiratory volume in 1 s was significantly higher among construction workers compared with bus drivers.
Conclusions
This review suggests that COPD occurs more often among construction workers than among workers who are not exposed to construction dust. It is not possible to draw any conclusions on specific subgroups as most studies analysed construction workers as one united group. In addition, no potential exposure–effect relationship could be identified.
Keywords: Chronic obstructive pulmonary disease, construction workers, COPD, inorganic dust.
Introduction
Chronic obstructive pulmonary disease (COPD) results in serious morbidity and was the fifth leading cause of death worldwide in 2002 [1]. COPD includes two main conditions, emphysema and chronic bronchitis, associated with fixed airway obstruction. The Global Initiative for Obstructive Lung Disease (GOLD) has defined spirometric criteria for severity dividing COPD into four stages (GOLD I-IV) using the forced expiratory volume in 1 s (FEV1), the forced vital capacity (FVC) and the ratio FEV1/FVC [2]. An FEV1/FVC ratio <0.7 after bronchodilator indicates COPD. Smoking is a well-known risk factor but some non-smokers also develop COPD [3]. In 2010, the American Thoracic Society concluded that there is sufficient evidence to infer a causal relationship between occupational exposures and COPD and a review from 2014 supported this conclusion [4,5]. Various organic and inorganic occupational exposures have been associated with COPD and 15–20% of prevalent cases of COPD have been attributed to occupational exposures [5–7].
Although much effort has been made to reduce dust exposure, the building and construction industry still presents a challenge for occupational safety and health protection [8]. Construction workers have developed restrictive lung diseases due to exposure to asbestos and silica dust [9–11]. However, construction workers are also exposed to non-specific construction dust. The occupational exposure limit (OEL) for respirable dust varies between countries but in all the Scandinavian countries, USA and most European countries, the OEL is set at 5 mg/m3. However, a recent Dutch study showed that this exposure limit for respirable dust was exceeded in 11% of measurements in the construction industry [12]. A German cohort study showed that construction workers were more likely to be granted a disability pension for COPD than the general workforce [13] and a study from the USA found that the lifetime risk of COPD was twice as high among construction workers as among non-construction workers [14]. Construction workers are therefore potentially exposed to respirable dust above the OEL and may have an increased risk of developing COPD. The aim of this review was therefore to assess the occurrence of COPD among construction workers especially in relation to the exposure of non- specific, inorganic dust.
Methods
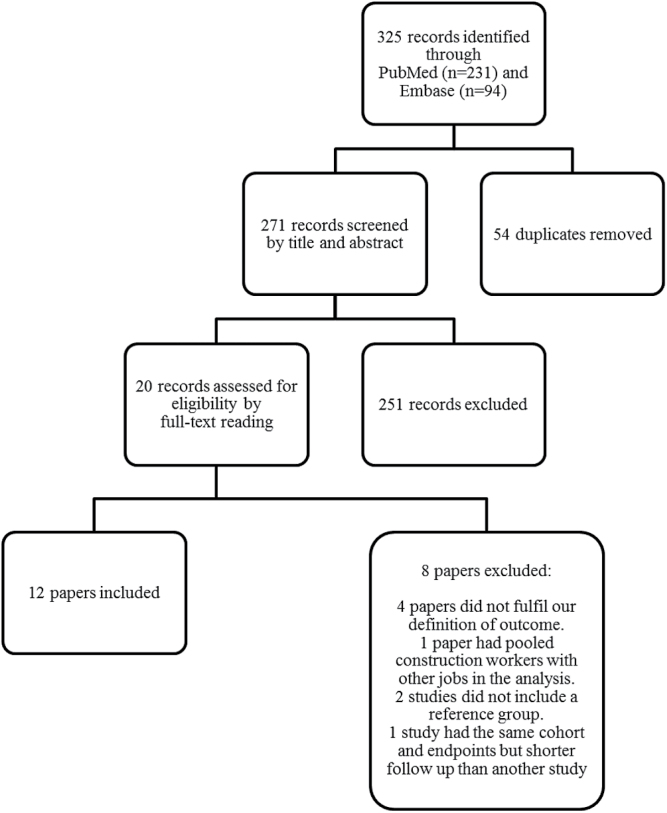
This study included articles using the diagnoses chronic bronchitis and emphysema, the GOLD criteria, spirometric-based indications of chronic obstruction, i.e. FEV1/FVC ratio <0.7 or FEV1/FVC below the lower limit of normal (LLN), or an accelerated annual decline in lung function. We searched the databases PubMed and Embase and included the following search terms: construction industry, construction workers, building industry, demolition workers, insulation workers, carpenters, electricians, painters, plumbers, ironworkers or roofers. These keywords were combined with keywords denoting COPD: chronic obstructive pulmonary disease, chronic obstructive lung disease, chronic lower respiratory diseases, chronic bronchitis, pulmonary emphysema, COPD, respiratory function test or loss of lung function. The reference lists were checked for additional relevant citations. The search was limited to English or Scandinavian literature published between 1 January 1990 and 31 August 2016. The procedure of literature selection is shown in Figure 1. Two researchers (C.B. and H.B.) independently screened for eligibility and agreed on 20 citations for full-text reading, which all four authors read. Two of the papers were based on the same cohort and had the same endpoint but had different observation times. The paper with the shortest follow-up period was excluded. The authors agreed on the inclusion of the final 12 papers.
Figure 1.
Flowchart of the literature search and selection of studies. The search was limited to papers written in English, Danish, Swedish or Norwegian and published between 1 January 1990 and 31 August 2016.
We included cohort, case–control and cross-sectional studies published in peer-reviewed papers if (i) the exposure included construction trades, job titles in the construction industry or dust among construction workers; (ii) the outcome was a spirometry-based definition of airway obstruction, physician-diagnosed COPD, chronic bronchitis or pulmonary emphysema (including cause of death registered on death certificates) or self-reported symptoms of chronic bronchitis (cough and sputum production for at least 3 months per year for at least 2 years) and (iii) there was an analysis of risk by occupation or occupational exposure. Exclusion criteria for the studies were (i) the exposure was defined as brick manufacturing, boilermaking, heavy clay industry, cement factory work, tunnel work, asphalt work, sheet metal work, mining, asbestos, silica, non-specific vapour/gas/dust/fumes or where construction workers were combined with other workers without separate analyses on the construction workers; (ii) the outcome was asthma or pneumoconiosis or (iii) the study did not include a reference group or internal comparator.
For each of the included papers, we used a data extraction sheet used in a recent review on COPD [5] comprising details of the study design, selection of the study sample, characteristics of the study population and comparison group, response rate, sample size, degree and duration of exposure, the outcome studied and confounders considered. We did not reanalyse any of the data in the papers. An evaluation of the quality of the studies was performed independently by two of the authors (C.B. and L.K.). Disagreements were resolved by discussion between the two. Table 1 shows the items in the quality assessment. The items could be scored as positive or negative, where a positive score denoted less risk of bias. We did not sum up the positive ratings to a quality score, because the items were not of equal importance (Table 2).
Table 1.
Checklist for the assessment of quality
| Study design | 1. Positive if the study was a cohort study or a case–control study as opposed to cross-sectional studies |
| 2. Positive if the studied age group was relevant for COPD | |
| Exposure assessment | 3. Positive if exposure assessment happened independently of outcome, for example, through an expert- rated JEM, job title or register data |
| Exposure-response information | 4. Positive if level and/or duration of exposure was assessed |
| Outcome assessment | 5. Positive if COPD was diagnosed by a physician, by spirometry or by death registered on death certificates |
| Confounding | 6. Positive if the analyses were adjusted for the potential confounders: smoking, age and sexa either in stratified or multivariate analysis |
aWhere both sexes were included in analyses.
Table 2.
Quality assessment
| Study [ref.] | Methodological items | |||||
|---|---|---|---|---|---|---|
| Cohort or case−control study | Relevant age group | Independent assessment of exposure/outcome | Exposure- response or duration | COPD diagnosed by a physician, spirometry or cause of death | Relevant potential confounders considered | |
| Albin et al. [15] | + | − | + | + | − | + |
| Clausen et al. [16] | + | + | + | − | − | + |
| Dement et al. [25] | − | + | + | − | + | + |
| Dement et al. [22] | + | + | + | + | + | + |
| Ringen et al. [18] | + | + | + | + | + | + |
| Robinson et al. [19] | + | + | + | − | + | −c |
| Torén and Järvholm [20] | + | + | + | − | + | + |
| De Matteis et al. [24] | − | + | + | − | + | + |
| Hnizdo et al. [7] | − | + | + | −a | + | + |
| Molgaard et al. [17] | + | + | + | − | +b | −c |
| Tüchsen et al. [21] | + | + | + | − | +b | −c |
| Mastrangelo et al. [23] | + | + | + | + | + | + |
Items are scored as positive (+) or negative (−) according to checklist in Table 1. A positive score denotes less risk of bias.
aIn the study by Hnizdo et al. [7], analyses were made for trend with duration of employment, but the results are not shown separately among construction workers.
bThe studies by Molgaard et al. [17] and by Tüchsen et al. [21] included asthma in the diagnosis of COPD.
cThe studies did not adjust for smoking.
Results
Twelve included studies were distributed as follows: seven cohort [15–21], two case–control [22,23] and three cross-sectional [7,24,25]. The main characteristics are presented in Table S1, available as Supplementary data at Occupational Medicine Online. None had measurements of specific exposures to dust, but included occupations in building and construction industry as the exposure. Nine controlled for smoking, age and sex [7,15,16,18,20,22–25]. The occupation-specific studies recruited participants from a voluntary medical screening programme among union members or employees or as part of an occupational safety and health programme in the construction industry. The population-based studies were from the USA, UK and Denmark. Three studies assessed COPD mortality [18–20], four defined COPD according to GOLD stages II–IV (moderate to very severe) or FEV1/FVC < LLN [7,22,24,25], three used clinical diagnosis of COPD [17,21,23] and two assessed annual decline in lung function [15,16]. Table S2, available as Supplementary data at Occupational Medicine Online, shows the associations between some exposures in the construction industry and the above-mentioned outcomes.
Albin et al. [15] used yearly change in the slow vital capacity (VC) and FEV1 and persistent cough as outcomes. Exposure to mineral wool among insulation workers was characterized by a combination of self-reports and job exposure matrix (JEM). They found no effects on VC or FEV1 but showed a significantly increased risk of persistent cough if working with mineral wool for the past 12 months and a dose–response trend indicating that a higher dose of exposure to mineral wool lead to an increased risk of persistent cough. Clausen et al. [16] examined a group of 114 insulation workers twice with a follow-up period of 6 years. They used FVC and FEV1 as outcomes. Job title was used as exposure assessment. The reference group consisted of bus drivers but recruitment was unclear. The seniority was mentioned, but not used in the analyses. They found a significantly lower lung function among the insulation workers at baseline and a significantly excess decline in FVC and FEV1 at follow-up. There was no significant difference between smoking groups. Dement et al. [25] studied current and former workers employed at the Department of Energy (DOE) who participated in a voluntary medical screening programme. A total of 7500 participants underwent a detailed DOE work history interview and a spirometry in a cross-sectional design. Administrative and scientific personnel were used as a reference group. They found significantly increased risk of COPD among carpenters, cement masons/bricklayers/plasterers, electricians, painters and plumbers/steamfitters/pipefitters. Using FEV1/FVC < LLN lead to a similar pattern.
The case–control study by Dement et al. [22] used the same population as above and included construction workers who had a least one spirometry. They found 834 cases and 1243 controls. The working history was not restricted to DOE but based on the lifelong working history. They specifically looked at cement dust and manmade fibres but also ‘Particulates not otherwise regulated’ (PNOR) and found a significant increased odds ratio (OR) for cement dust and PNOR. This study fractionated the upper 95th percentile into four fractions to indicate the exposure level. The general pattern showed an increase in the OR from the lowest to the highest fraction indicating a dose–response pattern. Ringen et al. [18] combined the same population as Dement with the National Death Index and found standardized mortality rates for COPD significantly increased among construction workers, specifically among carpenters and labourers. Robinson et al. [19] studied emphysema as well as other respiratory diseases among members of the United Brotherhood of Carpenters and Joiners of America. The whole US population was used as reference group. They compared the number of deaths in the exposed group with race-, gender-, and cause-specific proportionate mortality. Information on occupation came from union records. They did not adjust for smoking. A significant increased risk of dying from emphysema was found among carpenters in the construction industry, but not among industrial carpenters.
Torén and Järvholm [20] studied the same cohort as Albin et al. [15] but did not have data on spirometry. They looked at inorganic dust exposure characterized by occupation as found in a Swedish central database with a complete coverage of the construction industry and JEM. They had a large cohort, a high participation rate, a long follow-up period and a low drop-out. They used an internal control group of construction workers who were assessed as non-exposed. The mortality due to COPD was assessed and they found a significantly increased risk when exposed to inorganic dust. The risk increased among never-smokers. A similar trend was found for ‘any airborne exposure’. De Matteis et al. [24] used data from the UK Biobank cohort. The study included 228614 participants who all had an acceptable spiro metry. To specify the participants’ job titles, they used Standard Occupational Classification (SOC). Among others, they looked at workers and labourers in building and construction and found a significant increased prevalence ratio among building and construction workers. The study by Hnizdo et al. [7] was based on the third National Health and Nutrition Examination Survey in USA. They used data from spirometry and questionnaire information on occupation and smoking. The industry categories were broad. The reference group consisted of office workers. They studied associations between industry/occupation and COPD. The participation rate was not reported. Analyses were restricted to persons aged 30–75. The sample size was large, but there were only a few cases of COPD. A significantly increased risk of COPD among never-smoking construction workers was found. They looked at trends with duration of employment, but these results were not shown for construction workers separately.
The studies by Molgaard et al. [17] and Tüchsen et al. [21] used data from a Danish occupational hospital register where a person’s occupation and industry were registered annually. The occupation classified was the one which gave the highest income during the year before baseline. They included all male construction workers and used hospital inpatient and outpatient contacts with a diagnosis of obstructive respiratory diseases, including asthma, as outcome. The main job titles from the register were used as exposure. All economically active Danish men were used as reference group. They did not adjust for smoking. Molgaard et al. [17] found that demolition workers had a higher but insignificant risk of being diagnosed in a hospital setting with lower respiratory diseases. Tüchsen et al. [21] found a significant increased risk of lower respiratory diseases among painters and plumbers and construction workers as a whole, but only in the period 2001–09. The number of hospitalized construction workers suffering from obstructive respiratory diseases was reduced over time, but for all Danish males it was reduced even more. Mastrangelo et al. [23] included patients diagnosed with COPD at a department of occupational medicine in Italy in a case–control study of 131 cases and 298 controls without respiratory disease. The exposure was assessed by both self-reported occupational title and JEM. COPD diagnosis was based on symptoms, FEV1 and a test for reversibility. Patients with asthma or pneumoconiosis were excluded. They found a significantly increased risk of COPD among construction workers, carpenters and painters. The risk of COPD increased with length of exposure among painters. For construction workers in general, there was a borderline significant association between COPD and length of exposure indicating an exposure–effect relationship.
Discussion
Overall, this review suggests an increased occurrence of COPD among construction workers. Nine studies found a statistically significant association between COPD and work in the construction industry, although only among never-smokers in one study and only for the period after 2000 in another study [7,18–25]. An accelerated annual decline in lung function was found in one study [16] and another found a significantly increased risk of persistent cough if working with mineral wool with a dose–response pattern [15]. As most studies only had analyses of construction workers as one united profession, it is not possible to give any conclusions on specific subgroups. We focused on well-accepted definitions of COPD but the diagnostic criteria have changed over time and a risk of misclassification exists and thereby a risk of overestimating the results. The literature search was comprehensive and included two databases, but only English and Scandinavian literature with the risk of missing relevant studies in other languages. We might also have missed studies where the focus was not on construction industry, but where construction trades were included as part of the study. We checked the references in the included papers, but found no studies of relevance. We believe that we have included most important literature on the topic.
The quality assessment was made by addressing key components of the design and method. The small number and the limited quality of some of the studies mean that the results should be interpreted with caution. However, the review includes seven cohort studies, mostly of good quality [15–21]. We included three cross-sectional studies [7,24,25] as these may help to reveal potential associations. We did not perform a meta-analysis because of the studies’ heterogeneity. We focused on non-specific, inorganic dust in the construction industry. We included carpenters and insulation workers because they are also exposed to non-specific dust due to their various work tasks as well as by being bystanders. None of the studies had measurements of the exposure level and only few studies focused on the specific type of dust. The exposure was evaluated based on self-report or extract of data from registers. Job titles and trades are a coarse categor ization and do not reflect the different job tasks and exposures that persons within the same trade can have. A few studies [15,20,23] tried to address this problem by adding a JEM in the evaluation of exposure and these studies found significant associations with COPD. One study had occupational information from union records [19], which may be more accurate than the job titles listed on death certificates, but union records may not always be updated when members change jobs.
A few studies had information on duration of employment [7,15,23]. In the study by Hnizdo et al. [7], cases among construction workers were too few to take duration of exposure into account, Albin et al. [15] showed no relation to length of exposure, but in the study by Mastrangelo et al. [23], construction workers had a borderline significantly elevated risk of COPD in relation to length of exposure. In the study by Mastrangelo et al. [23], however, patients with dusty exposures may be overrepresented in the population as most of them were referred from the National Institute for Workers’ compensation, which may lead to an overestimation of the exposure–effect relationship. Of the studies performing spirometry not all explicitly described doing a post-bronchodilator test. This could lead to a risk of outcome misclassification, especially asthma, thus overestimating the risk. The studies relying on diagnoses from registers also risk misclassifications because of inaccuracies in diagnosis. The studies by Molgaard et al. [17] and Tüchsen et al. [21] included asthma in their definition of outcome, which may dilute results and thus tend to bias the results towards unity. It is possible that studies only including GOLD II+ are missing mild cases of COPD [7,25]. Also, the studies using hospitalization or death due to COPD as an end point are likely to underestimate the true presence of COPD [17–21], as hospitalization and death caused by COPD are most likely to represent the most severe cases. All of the population studies involving a health examination were based on voluntary participation, which could lead to selection bias. Admission to hospital because of COPD may have a social gradient, which can affect the data in register studies.
A few studies included in this review did not adjust for smoking [17,19,21]. As smoking is the main risk for development of COPD, the results of these studies must be evaluated with caution. Furthermore, most studies grouped participants in categories as current smokers, never-smokers and former smokers, which is a crude smoking measure and carries the risk of misclassification. In general, the risk of reporting bias also exists, if construction workers who are exposed to dust tend to under-report their smoking habits, which will inflate the risk estimate. Only a few studies adjusted for socio economic status [7,17] in spite of the fact that admin istrative personnel or the whole population were used as reference group. Smoking habits differ much between socioeconomic groups, so this is especially a problem in the studies that did not adjust for smoking. One study [15] had a very young study population in relation to the fact that it takes decades to develop manifest COPD. In their defence, they do not have COPD as an end point but other measures such as spirometry. Effects on other parameters of lung function could represent early signs of COPD. The studies are heterogeneous with respect to exposures and outcomes, which preclude strong conclusions. Nevertheless, the studies of highest quality found significant results and suggest a need for further research on the topic, especially cohort studies and studies that focus on more precise assessment of the character and duration of exposures and of tasks within job titles.
Key points
This systematic review provides an overview of the studies that have assessed the occurrence of chronic obstructive pulmonary disease among construction workers.
The studies suggest that chronic obstructive pulmonary disease occurred more often among construction workers than among workers who were not exposed to construction dust.
Due to the limited number of studies, it was not possible to conclude whether chronic obstructive pulmonary disease occurs more often in specific subgroups among construction workers.
Conflicts of interest
None declared.
Supplementary Material
References
- 1. World Health Organization. Chronic Obstructive Pulmonary Disease (COPD). 2017. http://www.who.int/respiratory/copd/burden/en/ (2017, date last accessed). [Google Scholar]
- 2. From the Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2017. http://goldcopd.org (2017, date last accessed). [Google Scholar]
- 3. Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2013;187:347–365. [DOI] [PubMed] [Google Scholar]
- 4. Eisner MD, Anthonisen N, Coultas D, et al. ; Committee on Nonsmoking COPD, Environmental and Occupational Health Assembly. An official American Thoracic Society public policy statement: novel risk factors and the global burden of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2010;182:693–718. [DOI] [PubMed] [Google Scholar]
- 5. Omland O, Würtz ET, Aasen TB, et al. Occupational chronic obstructive pulmonary disease: a systematic literature review. Scand J Work Environ Health 2014;40:19–35. [DOI] [PubMed] [Google Scholar]
- 6. Blanc PD, Torén K. Occupation in chronic obstructive pulmonary disease and chronic bronchitis: an update. Int J Tuberc Lung Dis 2007;11:251–257. [PubMed] [Google Scholar]
- 7. Hnizdo E, Sullivan PA, Bang KM, Wagner G. Association between chronic obstructive pulmonary disease and employment by industry and occupation in the US population: a study of data from the Third National Health and Nutrition Examination Survey. Am J Epidemiol 2002;156: 738–746. [DOI] [PubMed] [Google Scholar]
- 8. Kirkeskov L, Hanskov DJ, Brauer C. Total and respirable dust exposures among carpenters and demolition workers during indoor work in Denmark. J Occup Med Toxicol 2016;11:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Järvholm B, Englund A. The impact of asbestos exposure in Swedish construction workers. Am J Ind Med 2014;57:49–55. [DOI] [PubMed] [Google Scholar]
- 10. Stocks SJ, McNamee R, Carder M, Agius RM. The incidence of medically reported work-related ill health in the UK construction industry. Occup Environ Med 2010;67:574–576. [DOI] [PubMed] [Google Scholar]
- 11. Suarthana E, Moons KG, Heederik D, Meijer E. A simple diagnostic model for ruling out pneumoconiosis among construction workers. Occup Environ Med 2007;64:595–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. van Deurssen E, Pronk A, Spaan S, et al. Quartz and respirable dust in the Dutch construction industry: a baseline exposure assessment as part of a multidimensional intervention approach. Ann Occup Hyg 2014;58:724–738. [DOI] [PubMed] [Google Scholar]
- 13. Arndt V, Rothenbacher D, Daniel U, Zschenderlein B, Schuberth S, Brenner H. Construction work and risk of occupational disability: a ten year follow up of 14,474 male workers. Occup Environ Med 2005;62:559–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ringen K, Dement J, Welch L, Dong XS, Bingham E, Quinn PS. Risks of a lifetime in construction. Part II: chronic occupational diseases. Am J Ind Med 2014;57:1235–1245. [DOI] [PubMed] [Google Scholar]
- 15. Albin M, Engholm G, Hallin N, Hagmar L. Impact of exposure to insulation wool on lung function and cough in Swedish construction workers. Occup Environ Med 1998;55:661–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Clausen J, Netterstrøm B, Wolff C. Lung function in insulation workers. Br J Ind Med 1993;50:252–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Molgaard EF, Hannerz H, Tüchsen F, Brauer C, Kirkeskov L. Chronic lower respiratory diseases among demolition and cement workers: a population-based register study. BMJ Open 2013;3:e001938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ringen K, Dement J, Welch L, et al. Mortality of older construction and craft workers employed at Department of Energy (DOE) nuclear sites: follow-up through 2011. Am J Ind Med 2015;58:152–167. [DOI] [PubMed] [Google Scholar]
- 19. Robinson CF, Petersen M, Sieber WK, Palu S, Halperin WE. Mortality of Carpenters’ Union members employed in the U.S. construction or wood products industries, 1987–1990. Am J Ind Med 1996;30:674–694. [DOI] [PubMed] [Google Scholar]
- 20. Torén K, Järvholm B. Effect of occupational exposure to vapors, gases, dusts, and fumes on COPD mortality risk among Swedish construction workers: a longitudinal cohort study. Chest 2014;145:992–997. [DOI] [PubMed] [Google Scholar]
- 21. Tüchsen F, Hannerz H, Molgaard EF, Brauer C, Kirkeskov L. Time trend in hospitalised chronic lower respiratory diseases among Danish building and construction workers, 1981–2009: a cohort study. BMJ Open 2012;2:e001761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dement J, Welch L, Ringen K, Quinn P, Chen A, Haas S. A case–control study of airways obstruction among construction workers. Am J Ind Med 2015;58:1083–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mastrangelo G, Tartari M, Fedeli U, Fadda E, Saia B. Ascertaining the risk of chronic obstructive pulmonary disease in relation to occupation using a case–control design. Occup Med (Lond) 2003;53:165–172. [DOI] [PubMed] [Google Scholar]
- 24. De Matteis S, Jarvis D, Hutchings S, et al. Occupations associated with COPD risk in the large population-based UK Biobank cohort study. Occup Environ Med 2016;73:378–384. [DOI] [PubMed] [Google Scholar]
- 25. Dement JM, Welch L, Ringen K, Bingham E, Quinn P. Airways obstruction among older construction and trade workers at Department of Energy nuclear sites. Am J Ind Med 2010;53:224–240. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.