Dear Editor,
Frontal fibrosing alopecia (FFA) and lichen planopilaris (LPP) are the most frequent primary scarring alopecias. The histopathology of both alopecias is almost identical, consisting of inflammatory lymphocytic infiltrates and progressive fibrosis of the hair follicles. Despite the similar histological findings of these diseases, the clinical presentation is completely different. Although rare, some patients present clinical characteristics of FFA associated with LPP (Fig. 1). This association has been described previously in the literature [1, 2, 3, 4], but there are no studies describing the characteristics of this group of patients. The aim of this study was to describe the epidemiological and clinical characteristics of patients diagnosed with FFA and concomitant LPP.
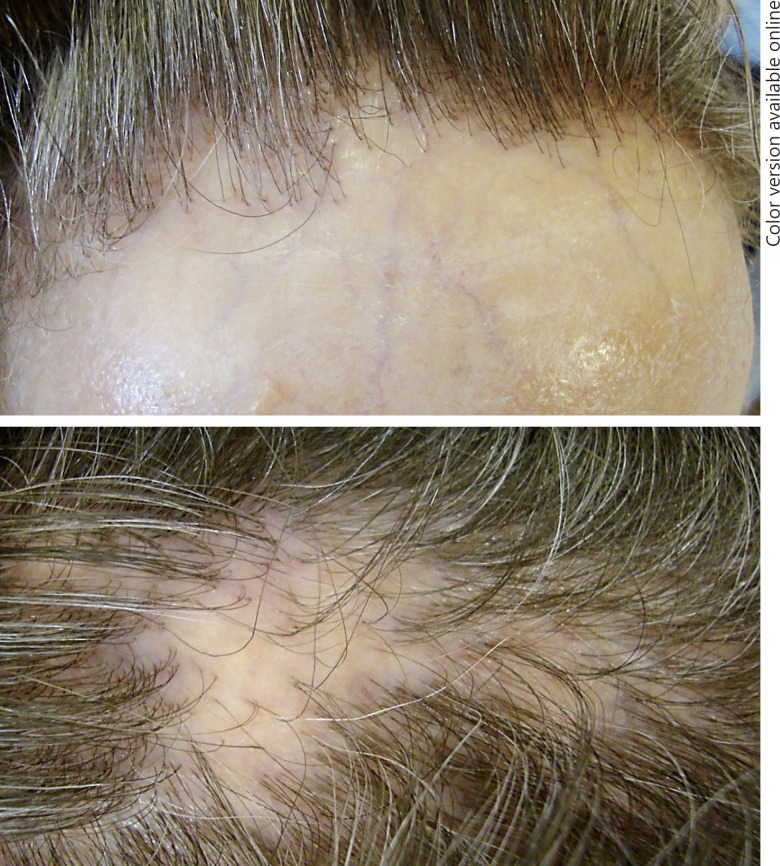
Fig. 1.
Lichen planopilaris associated with frontal fibrosing alopecia. Frontal hair recession and permanent hair loss on the vertex can be observed in the same patient.
A descriptive cross-sectional study was designed including patients diagnosed with both FFA and LPP. Histologic evidence of scarring alopecia (perifollicular lamellar fibrosis) and lichenoid interface inflammation was required to confirm the diagnosis of LPP. Data regarding epidemiology, thyroid disorders, gynecological history, cutaneous comorbidities, clinical presentation, and symptoms were recorded.
We analyzed a group of 103 female patients with FFA. Seventeen patients had LPP concomitant with FFA (16.5%). All patients were women, and their mean age was 67.9 years (range 44–85). The mean age at onset of FFA or LPP was 63.9 years (range 43–82). The onset of FFA preceded LPP in 7 patients (41.2%) by a mean time of 1.6 years (range 1–3). Family history of FFA or LPP was present in just 1 case (mother and 2 aunts). A total of 6 patients had hypothyroidism (35.3%), 3 of them with positive anti-thyroid peroxidase antibodies. The mean ages of menarche and menopause were 12.2 years (range 10–15) and 47.5 years (range 40–52), respectively. Remarkable gynecological history included hysterectomy (3 patients, 17.6%), oophorectomy (3 patients, 17.6%), and breast cancer (2 patients, 11.8%). Cutaneous comorbidities and clinical characteristics of patients are summarized in Table 1.
Table 1.
Clinical characteristics of patients with frontal fibrosing alopecia and concomitant lichen planopilaris
| Present study | Vañó-Galván et al. [4] | Meinhard et al. [9] | Soares et al. [10] | |
|---|---|---|---|---|
| Cases, n | 17 | 355 | 104 | 80 |
| Type of alopecia | FFA and LPP: 17 (100%) | FFA: 355 (100%) | FFA: 32 (30.8%) LPP: 71 (68.2%) GLPLS: 1 (1%) | FFA: 29 (36.3%) LPP: 50 (62.5%) GLPLS: 1 (1.2%) |
| Age of onset of alopecia (range), years | 63.9 (43–82) | 56 (21–81) | Women: 58 years Men: 52 years | ns |
| Median grade of severity of FFAa | III (3–4.99 cm) | II (1–2.99 cm) | ns | ns |
| Clinical presentation of LPP | Random plaques: 15 (88.2%) Vertex involvement: 2 (11.8%) | na | ns | Random plaques: 24 (30%) FAPD: 29 (36.3%) Vertex involvement: 4 (5%) |
| Pruritus | 11 (64.7%) | 124 (35%) | ns | ns |
| Pain | 7 (41.2%) | 71 (20%) | ns | ns |
| Occipital involvement | 4 (23.5%) | 52 (15%) | ns | ns |
| Eyebrow loss | 15 (88.2%) | 283 (80%) | FFA: 19 (59.4%) LPP: 5 (7%) | ns |
| Eyelash loss | 7 (41.2%) | 50 (14%) | ns | 3 (3.8%) |
| Facial papules | 6 (35.3%) | 49 (14%) | ns | ns |
| Body hair involvement | Axillary hair: 8 (47.1%) Pubic hair: 7 (41.2%) Upper and/or lower limbs: 8 (47.1%) | Axillary hair: 75 (21%) Pubic hair: 63 (18%) Upper and/or lower limbs: 86 (24%) | Axillary hair and/or pubic hair: FFA: 5 (15.6%) LPP: 6 (8.5%) | Axillary hair: 16 (20%) Pubic hair: 8 (10%) Upper and/or lower limbs: 9 (11.3%) |
| Mucosal abnormalities | Mucosal LP: 4 (23.5%; 3 reticular form and 1 erosive form) | Mucosal LP: 12 (3.4%) | ns | Mucosal LP: 2 (2.5%; 1 in FFA patient) |
| Nail abnormalities | Pterygium nail: 1 (5.9%) | ns | ns | Pterygium nail: 2 (2.5%; in a FFA patient) Involvement 20 nails: 1 (1.25%) |
| Other cutaneous disorders | Rosacea: 8 (47.1%) Nickel contact dermatitis: 3 (17.6%) Vasculitis: 1 (5.9%) Seborrheic dermatitis: 1 (5.9%) | Cutaneous LP: 23 (6.5%) Vitiligo: 2 (0.6%) Alopecia areata: 2 (0.6%) LSA: 1 (0.3%) LPP: 3 (0.8%) AGA: 150 (42.3%) | FFA Vitiligo: 2 (6.3%) Alopecia areata: 1 (3.1%) LPP Cutaneous LP: 4 (5.6%) Seborrheic dermatitis: 3 (4.2%) Alopecia areata: 1 (1.4%) | Cutaneous LP: 2 (2.5%) |
Values are n (%) unless otherwise specified. AGA, androgenetic alopecia; FAPD, frontal alopecia in a pattern distribution; FFA, frontal fibrosing alopecia; GLPLS, Graham-Little Piccardi-Lassueur syndrome; LPP, lichen planopilaris; LP, lichen planus; LSA, lichen sclerosus et atrophicus. ns, not specified; na, not applicable.
Scale of severity of FFA by Vañó-Galván et al. [4].
It is controversial whether FFA is a clinical variant of LPP. Some authors argue that FFA has a distinct clinical presentation and natural history and should be considered a specific entity. To our knowledge, the association between FFA and LPP has been mentioned in 41 patients in the literature, but large case series did not find significant numbers of cases [1, 2, 3, 4, 5, 6, 7].
The mean age of onset in our study is slightly higher than in other case series; however, most of the patients presented a low-to-moderate grade of severity of FFA (grades I-III in 10 patients, 64.7%). This supports the argument that the coexistence of these 2 entities is not a consequence of long-term evolution of FFA. In fact, a previous report has hypothesized the possibility of a common genetic basis [8].
Interestingly, patients with FFA and LPP had non-scalp hair areas more frequently involved than reported in other case series of FFA or LPP. This was specially marked in eyelashes and body hair, where involvement was present in >40% of the patients. However, some large case series noted similar frequencies [2], and there are no specific studies assessing body hair loss which compare women with FFA to healthy controls, so this hair loss may be due to normal physiological events. Also, facial papules were detected in a significant number of patients (35.3%). Patients with FFA and LPP could have a higher susceptibility to producing intense lichenoid reactions than other patients with isolated FFA or LPP. An intense inflammatory reaction could worsen the symptoms in these patients, and this would also explain the higher percentage of patients with pruritus and pain found in our study.
Among other clinical forms of lichen observed in our study, the involvement of oral mucosae was found in a considerable number of patients (23.5%), and 1 patient had nail lichen planus. It is difficult to know whether this means that associated lichen planus is more common in patients with FFA and LPP, because not all case series on FFA or LPP collected these data systematically.
In conclusion, this is the first published series of patients with FFA associated with concomitant LPP. Although both of these diseases are scarring alopecias, their coexistence could lead to misdiagnosing one of them. Involvement of non-scalp hair areas and presence of symptoms could be more frequent in these patients [9, 10].
Statement of Ethics
Verbal photographic and informed consent was obtained from the patients described in this article. The study protocol has been approved by the institute's committee on human research.
Disclosure Statement
The authors declare that they have no conflicts of interest regarding this study. This article has no funding source.
References
- 1.Kossard S, Lee MS, Wilkinson B. Postmenopausal frontal fibrosing alopecia: a frontal variant of lichen planopilaris. J Am Acad Dermatol. 1997;36:59–66. doi: 10.1016/s0190-9622(97)70326-8. [DOI] [PubMed] [Google Scholar]
- 2.Banka N, Mubki T, Bunagan MJK, McElwee K, Shapiro J. Frontal fibrosing alopecia: a retrospective clinical review of 62 patients with treatment outcome and long-term follow-up. Int J Dermatol. 2014;53:1324–1330. doi: 10.1111/ijd.12479. [DOI] [PubMed] [Google Scholar]
- 3.MacDonald A, Clark C, Holmes S. Frontal fibrosing alopecia: a review of 60 cases. J Am Acad Dermatol. 2012;67:955–961. doi: 10.1016/j.jaad.2011.12.038. [DOI] [PubMed] [Google Scholar]
- 4.Vañó-Galván S, Molina-Ruiz AM, Serrano-Falcón C, Arias-Santiago S, Rodrigues-Barata AR, Garnacho-Saucedo G, Martorell-Calatayud A, Fernández-Crehuet P, Grimalt R, Aranegui B, Grillo E, Diaz-Ley B, Salido R, Pérez-Gala S, Serrano S, Moreno JC, Jaén P, Camacho FM. Frontal fibrosing alopecia: a multicenter review of 355 patients. J Am Acad Dermatol. 2014;70:670–678. doi: 10.1016/j.jaad.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Ladizinski B, Bazakas A, Selim MA, Olsen EA. Frontal fibrosing alopecia: a retrospective review of 19 patients seen at Duke University. J Am Acad Dermatol. 2013;68:749–755. doi: 10.1016/j.jaad.2012.09.043. [DOI] [PubMed] [Google Scholar]
- 6.Dlova N, Goh C-L, Tosti A. Familial frontal fibrosing alopecia. Br J Dermatol. 2013;168:220–222. doi: 10.1111/j.1365-2133.2012.11101.x. [DOI] [PubMed] [Google Scholar]
- 7.Chiang YZ, Bundy C, Griffiths CEM, Paus R, Harries MJ. The role of beliefs: lessons from a pilot study on illness perception, psychological distress and quality of life in patients with primary cicatricial alopecia. Br J Dermatol. 2015;172:130–137. doi: 10.1111/bjd.13259. [DOI] [PubMed] [Google Scholar]
- 8.Rivas MMO, Antolín SC, Sambucety PS, González ES, Ruíz de Morales JMG, Prieto MÁR. Frontal fibrosing alopecia and lichen planopilaris in HLA-identical mother and daughter. Indian J Dermatol Venereol Leprol. 2015;81:162–165. doi: 10.4103/0378-6323.152284. [DOI] [PubMed] [Google Scholar]
- 9.Meinhard J, Stroux A, Lünnemann L, Vogt A, Blume-Peytavi U. Lichen planopilaris: epidemiology and prevalence of subtypes - a retrospective analysis in 104 patients. J Dtsch Dermatol Ges. 2014;12:229–235. doi: 10.1111/ddg.12264. [DOI] [PubMed] [Google Scholar]
- 10.Soares VC, Mulinari-Brenner F, de Souza TE. Lichen planopilaris epidemiology: a retrospective study of 80 cases. An Bras Dermatol. 2015;90:666–670. doi: 10.1590/abd1806-4841.20153923. [DOI] [PMC free article] [PubMed] [Google Scholar]