Abstract
Background
Planning for mass gatherings often includes temporary healthcare systems to address the needs of attendees. However, paper-based record keeping has traditionally precluded the timely application of collected clinical data for epidemic surveillance or optimization of healthcare delivery. We evaluated the feasibility of harnessing ubiquitous mobile technologies for conducting disease surveillance and monitoring resource utilization at the Allahabad Kumbh Mela in India, a 55-day festival attended by over 70 million people.
Methods
We developed an inexpensive, tablet-based customized disease surveillance system with real-time analytic capabilities, and piloted it at five field hospitals.
Results
The system captured 49 131 outpatient encounters over the 3-week study period. The most common presenting complaints were musculoskeletal pain (19%), fever (17%), cough (17%), coryza (16%) and diarrhoea (5%). The majority of patients received at least one prescription. The most common prescriptions were for antimicrobials, acetaminophen and non-steroidal anti-inflammatory drugs. There was great inter-site variability in caseload with the busiest hospital seeing 650% more patients than the least busy hospital, despite identical staffing.
Conclusions
Mobile-based health information solutions developed with a focus on user-centred design can be successfully deployed at mass gatherings in resource-scarce settings to optimize care delivery by providing real-time access to field data.
Keywords: Kumbh Mela, mass gatherings, mHealth, mobile phones, primary care, tablet, user-centered design
Background
Mass gatherings present a complex public health challenge for domestic and international agencies.1 Whether religious, political or cultural, the congregation of a large number of people tests emergency response systems.2 To address the risks of disease outbreaks, clinical emergencies, stampedes and mass casualties, governments have increased investments in temporary healthcare facilities and public health preparedness.3 However, record keeping in these settings is often spotty and paper based, precluding any real-time collation or analysis of data for disease surveillance or resource mobilization.4
Mobile health (mHealth) technologies have the potential to transform healthcare delivery: their ubiquity and low marginal costs make them highly scalable and potentially cost-effective.5,6 The commercial wireless network today covers 80% of the world's population, extending far beyond the distribution of the electrical grid or improved sanitation facilities. The availability of open-source, customizable software, inexpensive mobile technologies and cloud-based analytics provide an unprecedented capacity to rapidly collect and analyse large amounts of data in real time. In addition to data curation, digital platforms can aid the implementation of clinical decision support systems and the dissemination of important public health information via text messaging or social media. The latter will become increasingly important in the coming years, when a rapid public response may be required to spontaneous mass gatherings mobilized by ‘viral’ messaging on online social networks (as was witnessed on several occasions in the Arab Spring). The field is ripe for disruptive innovation.7
The 2013 Kumbh Mela in Allahabad, India, attracted an estimated 70 million pilgrims over a 55-day period, making it the largest human gathering in history.8 Four percent of the $200 million government budget allocated to the Kumbh was spent on providing a temporary, free healthcare system for the attendees (Fig. 1). This system was based on a hub-and-spoke model, with a central referral hospital supported by 13 smaller ‘sector’ hospitals (one for each geographic subdivision of the Kumbh area).9 Each sector hospital housed a 24-hour outpatient clinic, a 20-bed inpatient unit and an on-site pharmacy. Patient encounters were brief, typically lasting <3 min each. A physical examination was seldom performed; no laboratory or radiologic tests were available (Fig. 1). Patients would leave these cursory encounters with prescriptions for one or more medications, and receive a free 3-day supply at the on-site pharmacy. Patients requiring higher levels of care were referred to the central hospital equipped with a 100-bed inpatient unit, a two-bed intensive care unit, facilities for obtaining X-rays and basic blood tests, a basic emergency room and specialty clinics including cardiology, otolaryngology, gynaecology and paediatrics. Patients requiring additional interventions were transferred to tertiary care hospitals in Allahabad city.9
Fig. 1.
Outpatients await their turn to see a physician at a sector hospital at the Kumbh Mela.
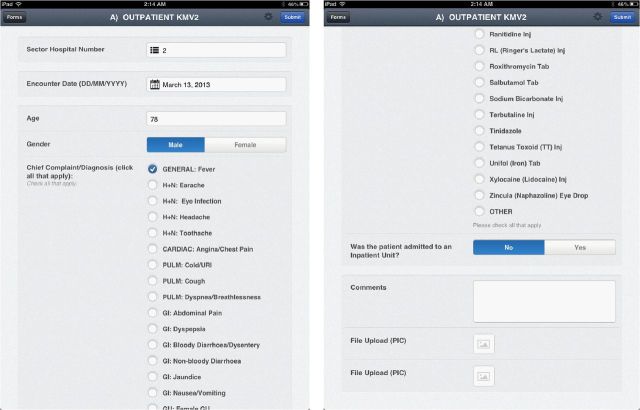
Patient records were paper-based and logged in notebooks held at the clinic (Fig. 2). This system did not allow easy access to data for real-time decision-making. To address this gap, we developed a customized digital surveillance system that relied on ubiquitous, inexpensive mobile technology to rapidly collate and analyse data on outpatient encounters within the temporary health system of the world's largest mass gathering. As this was a pilot study, the existing paper-based system was retained to minimize workflow disruption. Medical students transcribed the written data simultaneously into the digital system. In this paper, we present insights related to the implementation process as well as quantitative analyses of the recorded outpatient encounters. We demonstrate that such low-cost mobile systems can generate reliable, actionable data in mass gatherings, underscoring their potential benefit in other resource-scarce settings including humanitarian emergencies and remote field operations.
Fig. 2.
User-centred design for mobile technology at mass gatherings.
Methods
We developed and deployed our surveillance tool over a period of 2 weeks using principles of user-centred design. User-centred design is a multistage problem-solving process that emphasizes gaining insight into the needs of the end user, invoking participatory design and deploying iterative development to deliver solutions that work in specific socioeconomic and cultural contexts.10,11 During the first week, we interviewed key informants and observed workflow within the Mela's healthcare system to understand the feasibility of using mobile technologies in this setting. In order to minimize any changes in the existing workflow, as requested by the local administrators, local medical and public health students transcribed data from the paper records to the digital tool. We rapidly developed a prototype that comprised a tablet-based application and a remotely accessible cloud-based database to elicit and refine user preferences. Usability testing of early prototypes allowed us to optimize the user interface for efficient data entry by including drop-down menus and radio buttons to improve speed and minimize errors (Fig. 2). The embedded list of drugs reflected the formulary available at each clinical site, but free-text fields allowed the instrument to capture other treatments.
The system had offline synchronization capability by which data were stored locally on the tablets until Internet was available. Data were transferred to the cloud once or twice daily via mobile hotspots. The database could be queried remotely to trend caseloads, graph presenting complaints and monitor resource utilization. No identifiable health information was collected, and role-based passwords and industry-standard encryption ensured data security. See Supplementary data, Appendix, for additional technical details.
The surveillance tool was piloted at five sites: four sector hospitals (from 27 January through 15 February 2013) and the central hospital (26 January through 25 February 2013). This time interval included four highly ‘auspicious days’ when tens of millions attend the festival to bathe at the confluence of the two holy rivers, the Ganga and the Yamuna. The four sector hospitals chosen were on the busiest thoroughfares leading to the main bathing area, consistently drawing the largest numbers of patients. The central hospital was chosen because it was equipped to provide a higher level of care and was the gateway for referral to tertiary hospitals. Daily, teams of three medical students (who had participated in the interface design process) transcribed select data from the physicians’ paper records: patient's age, gender, chief complaint, diagnosis, treatment administered and disposition (discharged from care, hospitalized at the site or referred to the next higher level of care). Patient identifiers were not transcribed.
Raw data analytics were instantly available: these included caseload, gender distribution, epidemiologic trends, frequency of diagnostic tests and prescribed drugs. Further statistical analyses presented in this paper were conducted using Stata 13 (StataCorp, College Station, TX, USA). For the purpose of the quantitative analyses of patient-level data presented in this paper, continuous data were compared using the Student's t-test, while discrete data were compared using the Chi-square test (or Fischer exact test for cell sizes smaller than 20). A P-value of <0.01 was defined as statistically significant.
The study was reviewed and granted exemption by the Institutional Review Board at the Harvard School of Public Health (Public Health Implications of the Kumbh Mela, IRB13-0018), and reviewed and granted permission by the National Disaster Management Authority of India. As only de-identified population data were analyzed, requirement for individual consent was waived.
Results
Iterative optimization of the data entry interface during the development phase was key to usability: after 2 weeks of development, the tool could capture recorded clinical data in <1 min per patient encounter. The system worked reliably over the duration of the study without breakdown or loss of data, although we noted minor upload delays on the busiest days when the large influx of pilgrims overloaded the mobile network. The database could be remotely and reliably queried to generate real-time data analyses. In the following sections, we examine the baseline characteristics and presenting complaints of patients receiving care at the study hospitals, and the system's clinical practice and resource utilization as captured by this digital system.
Baseline characteristics
Our digital surveillance system recorded 49 131 encounters (39 126 from four sector hospitals and 10 005 from the central hospital) during the study period. The median age at the time of presentation was 46 years (interquartile range: 30–60), with patients presenting to the central hospital younger than patients presenting at the sector hospitals (P < 0.001; Table 1). Women comprised only a quarter of the patients presenting at sector hospitals compared with nearly half of the patients presenting for care at the central hospital (P < 0.001 for comparison).
Table 1.
Demographics and clinical presentation
| All hospitals | Central hospital | Sector hospital | P-value for comparison between central and sector hospitals | |
|---|---|---|---|---|
| Total outpatients | 49 131 | 10 005 | 39 126 | – |
| Demographics | ||||
| Age, mean (SD) | 44.7 (19.8) | 34.6 (19.8) | 47.4 (18.9) | <0.001 |
| Age of adult patients, mean (SD) | 48.6 (16.5) | 42.5 (14.7) | 49.9 (16.6) | <0.001 |
| Percentage female, % (SE) | 30.0 (0.2) | 49.5 (0.5)a | 24.9 (0.2) | <0.001 |
| Proportion paediatric patients, age ≤16 years, % (SE) | 9.5 (0.13) | 22.2 (0.42) | 6.2 (0.12) | <0.001 |
| Clinical presentation, by presenting complaintb | ||||
| Musculoskeletal pain, % (SE) | 19.00 (0.18) | 19.17 (0.39) | 18.96 (0.19) | 0.636 |
| Fever, % (SE) | 17.28 (0.17) | 14.53 (0.35) | 17.98 (0.19) | <0.001 |
| Cough, % (SE) | 16.51 (0.17) | 11.20 (0.31) | 17.87 (0.19) | <0.001 |
| Coryza, % (SE) | 16.49 (0.17) | 11.52 (0.32) | 17.77 (0.19) | <0.001 |
| Diarrhoea, % (SE) | 5.35 (0.10) | 3.94 (0.19) | 5.71 (0.12) | <0.001 |
| Abdominal pain, % (SE) | 4.81 (0.10) | 3.87 (0.19) | 5.05 (0.11) | <0.001 |
| Clinical presentation, by systemc | ||||
| Cardiopulmonary, % (SE) | 30.36 (0.21) | 20.59 (0.40) | 32.86 (0.24) | <0.001 |
| Musculoskeletal, % (SE) | 19.21 (0.18) | 19.97 (0.40) | 19.02 (0.20) | 0.033 |
| Gastrointestinal, % (SE) | 4.60 (0.37) | 11.26 (0.32) | 15.87 (0.18) | <0.001 |
| Skin and soft tissues, % (SE) | 4.49 (0.09) | 5.74 (0.23) | 4.18 (0.10) | <0.001 |
| Genitourinary, % (SE) | 0.99 (0.04) | 3.5 (0.18) | 0.33 (0.02) | <0.001 |
SD, standard deviation; SE, standard error.
aWomen constituted 18% of patients at the central hospital after excluding the women's health clinic, which served as a primary care clinic for women.
bProportion of patients presenting with stated complaint.
cProportion of patients presenting with one or more complaints related to stated organ system.
Clinical presentations
The most common recorded complaints were musculoskeletal pain (19%), fever (17%), cough (17%), coryza (16%) and diarrhoea (5%) (Table 1). These were similar at the sector and central hospitals. Trauma was rare, comprising only 0.2% of presenting cases.
Contrary to the concerns about water-borne outbreaks, diarrhoea was a relatively uncommon presenting complaint, and the majority of outpatient presentations were for non-urgent complaints, primarily musculoskeletal and upper respiratory.
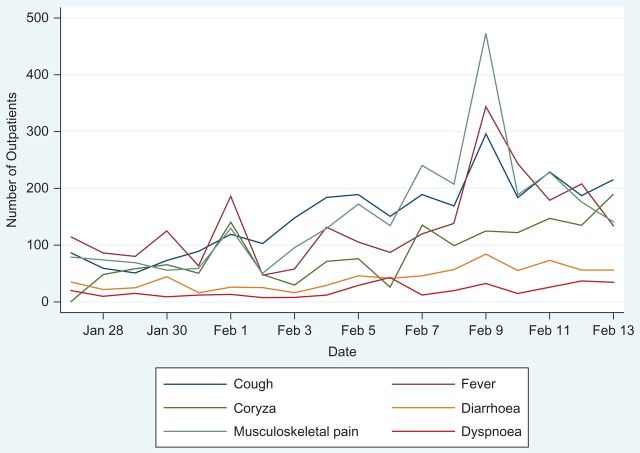
The tool recorded changing trends over time, and we observed that the incidence of disease rose and fell in tandem with the population fluctuations around bathing days as expected. We recorded a significant spike in presentations on 9–10 February, the busiest of all bathing days (Fig. 3).
Fig. 3.
Disease trends (study data).
Resource utilization
The majority of patients were managed in the outpatient setting: only 1.4% of patients presenting to sector hospitals required hospitalization. Among outpatients presenting to the central hospital, 0.1% of the patients received laboratory tests, 1.9% received a radiologic investigation and 0.5% were admitted. Common presenting complaints among patients requiring hospitalization were diarrhoea (23%), abdominal pain (19%), fever (17%) and dyspnoea (14%).
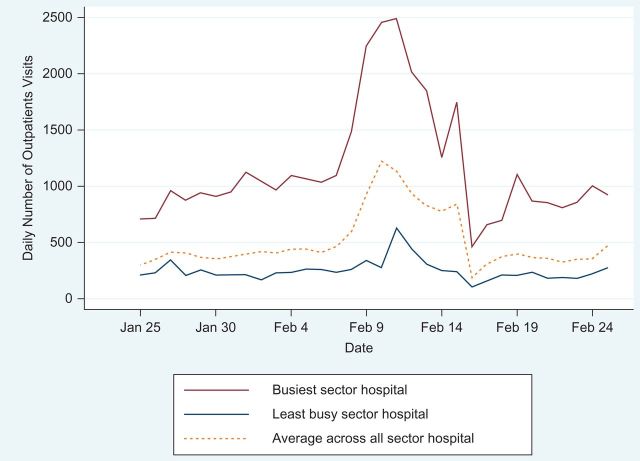
There was great variability in caseload among all hospitals, with the busiest sector hospital seeing 650% more patients than the least busy sector hospital (Fig. 4). Hospitals closest to the bathing sites were busier than those farther removed.
Fig. 4.
Daily number of outpatient visits (official data).
Prescribing practice
The majority of patients received at least one prescription medication (70% of patients presenting to the central hospital compared with 90% of patients presenting to sector hospitals, P < 0.001). The most common prescriptions were for antimicrobials, acetaminophen, non-steroidal anti-inflammatory agents, anti-histamines, vitamins and mineral supplements (Table 2). The digital system made it possible to examine prescription practices for each presenting complaint. The use of symptomatic treatment and placebos was widespread: 25% of patients received a 3-day supply of vitamins or mineral supplements in the absence of a defined indication. Nearly half the patients who presented to the clinics with a complaint of subjective fever received a 3-day prescription for an antimicrobial agent.
Table 2.
Diagnostic studies and prescriptions
| All hospitals | Central hospital | Sector hospitals | P-value for comparison between central and sector hospitals | |
|---|---|---|---|---|
| Total outpatients | 49 131 | 10 005 | 39 126 | – |
| Diagnostic studies | ||||
| X-ray, % (SE) | 0.37 (0.02) | 1.93 (0.13) | 0.00 (0.00) | <0.001 |
| Ultrasound, % (SE) | 0.01 (0.00) | 0.04 (0.02) | 0.00 (0.00) | <0.001 |
| Prescriptionsa | ||||
| One or more prescriptions given, % (SE) | 86.69 (0.15) | 69.72 (0.46) | 91.03 (0.14) | <0.001 |
| Antimicrobial, % (SE) | 31.85 (0.21) | 29.77 (0.46) | 32.39 (0.24) | <0.001 |
| Acetaminophen, % (SE) | 30.79 (0.21) | 28.72 (0.45) | 31.32 (0.23) | <0.001 |
| Non-steroidal anti-inflammatory agents, % (SE) | 28.43 (0.20) | 24.89 (0.43) | 29.34 (0.23) | <0.001 |
| Antihistamines, % (SE) | 26.19 (0.20) | 16.75 (0.37) | 28.61 (0.23) | <0.001 |
| Supplements—vitamins and minterals, % (SE) | 25.23 (0.20) | 23.09 (0.42) | 25.77 (0.22) | <0.001 |
| Vitamins, % (SE) | 19.17 (0.18) | 19.40 (0.40) | 19.11 (0.20) | 0.516 |
| Minerals—calcium and iron, % (SE) | 12.68 (0.15) | 12.62 (0.33) | 12.70 (0.17) | 0.843 |
| Gastroprotectives—PPI, H2 blocker, antacids, % (SE) | 11.52 (0.14) | 9.24 (0.29) | 12.10 (0.16) | <0.001 |
| Anti-parasitic % (SE) | 6.13 (0.11) | |||
| Bronchodilators, % (SE) | 2.69 (0.07) | 1.32 (0.11) | 3.04 (0.09) | <0.001 |
| Steroids, % (SE) | 0.50 (0.03) | 0.87 (0.09) | 0.41 (0.03) | <0.001 |
| Consults/Admission | ||||
| Referral to specialty clinic, % (SE) | 0.06 (0.04) | 2.97 (0.17) | 0.00 (0.51) | <0.001 |
| Inpatient admission, % (SE) | 1.20 (0.05) | 0.54 (0.07) | 1.38 (0.05) | <0.001 |
SE, standard error.
aReported as proportion of patients receiving one or more prescriptions for the stated drug class.
Discussion
Main finding of this study
Our study yielded important insights relevant to the use of mobile technology at mass gatherings and demonstrated that digital data capture, analytics for syndromic surveillance, and monitoring of resource utilization could be conducted in real time across multiple sites, in a locale with no permanent infrastructure.
What is already known about this topic
Record keeping at all previous Kumbh Mela events and at many other mass gatherings has been paper-based, impeding real-time disease surveillance and monitoring of resource utilization. This leads to a significant delay in transmission and analysis of critical health information. Digitization of the health information system may address these needs, but is not considered as a viable solution given the oft-cited barriers to electronic health information systems including physician attitudes, costs, speed and workflow disruption.12,13
What this study adds
Our experience with successfully overlaying the massive temporary healthcare system of the Kumbh Mela with a simple, inexpensive digital surveillance tool holds important public health lessons for mass gathering preparedness anywhere.
The Mela's hub-and-spoke hospital network served 280 000 outpatients over the course of the event, but data from their visits were not easily accessible. Digitally capturing clinical data using an inexpensive, easy-to-use surveillance tool enabled rapid caseload analysis, provided insights into geographic and temporal trends in resource utilization, and identified opportunities for improvement of healthcare quality.
The Importance and Impact of User-Centred Design We demonstrated that user-centred design played a key role in optimizing usability of our mobile health solution. Poorly designed mHealth technology may result in dissatisfied users, poor retention, diminished effectiveness and increased error costs. Iterative development with early and continuous engagement of end users ensures that the final product is efficient and usable, both key to widespread adoption. We observed that engaging with all stakeholders early in the process was particularly useful. The medical students involved in data entry were part of the interface design process, and their presence did not interrupt the existing workflow. The remotely accessed dashboard and rapid analytics were made available to the front-line physicians, the medical students digitally transcribing the data, and to all administrators. At each site, our team presented daily analytics, discussing implications for outbreak monitoring, resource re-allocation and quality control. Site supervisors conducted random checks to ensure the accuracy of data transcription. We observed 100% compliance with data entry at all sites.
Demonstration of Gender Disparity in Healthcare Access Our findings also have key implications for healthcare delivery at future mass gatherings in low- and middle-income countries. Despite constituting 40% of the pilgrims at the Mela, women comprised only a quarter of the patients presenting at sector hospitals, compared with nearly half of the patients presenting for care at the central hospital, despite the fact that sector hospitals were typically more accessible than the central hospital (which was farther from the bathing site). Women may have preferred to seek care at the central hospital because it ran a dedicated women's clinic staffed by female physicians throughout the duration of the Mela. In contrast, the large crowds of patients at sector hospitals meant that there was little room for privacy during the brief interaction with physicians (who were predominantly male). This finding calls for a careful examination of the real and perceived barriers to access for female patients in the setting of future Melas.
-
The Epidemiology and Management of Common Presentations at the Mela: A Cautionary Note The case-mix seen at the clinics may help inform care delivery at future Melas. Although Kumbh Melas have been historically associated with outbreaks of epidemics of diarrhoeal diseases including cholera, diarrhoea was not among the top three most common presenting complaints, possibly due to the widespread availability of piped potable water and improved sanitation facilities at the Kumbh Mela.14 On the contrary, close contact with large crowds and poor air quality may have contributed to respiratory complaints. Fourteen patients were diagnosed with measles, but no contact tracing was conducted.
Nearly half the patients who presented to the clinics with a complaint of subjective fever received a 3-day prescription for an antimicrobial agent. There was no clinical protocol or syndromic definition of infectious diseases to determine who would receive what antibiotic, and no additional laboratory or radiological investigations were systematically employed. This excessive use of a short course of antibiotics is similar to that described in other settings in India.15–17 The concern for development of resistant organisms is particularly significant at the Mela because of the potential for wide dissemination of resistant organisms across India as pilgrims from all over the country return home, ultimately posing a national and global threat.18,19 Our data suggest that preparations for mass gatherings would benefit from establishing clinical guidelines and providing oversight of temporary staff. Protocol adherence may also be enhanced by integrating decision support algorithms into mobile health platforms. The liberal use of analgesics, vitamins and arbitrary mineral supplements suggests the need for future studies to determine whether shifting the focus of the healthcare delivery system from clinical service to screening and awareness may yield greater societal return on investment.
Real-Time Resource Re-allocation The ability to measure temporal and geographic trends in care utilization across a mass gathering could help optimize resource allocation in the future. The sector hospitals were provided with identical infrastructure and staffing without additional surge capacity. This egalitarian distribution of resources resulted in substantial inequities as caseloads varied several fold among sector hospitals depending on the proximity of the hospitals to the main bathing areas and during the ebb and flow of festival activities. The surveillance tool allowed for rapid recognition of these disparities in resource allocation. In the future, this information could allow administrators to redistribute supplies, personnel and critical resources to the busiest facilities, narrowing the gap between supply and demand.
Such remote access to data from field operations would also be invaluable in emergencies and for long-standing aid programs where data, even if digitally transcribed, are often stored locally before they are sequentially transferred up the chain of command to decision-makers stationed at distant head offices. Mobile hotspots allow field practitioners to directly upload time-sensitive information to remotely accessible databases, consequently shortening response times for inventory or personnel re-allocation. The ability to capture real-time disease trends is critical while monitoring outbreaks where rapid fluctuations in disease counts may signal either an impending epidemic or changing population numbers or both, warranting a timely investigation and response.
Limitations of this study
Data were first entered on paper records, and then digitally transcribed on a daily basis by medical students posted at each of the pilot sties. While this study demonstrated the advantages of user-centred design (and 100% uptake), it could not test usability among clinical staff. However, cell-phone penetration in India is now near universal (over 1 billion users)20 and smartphone and tablet-based data collection has been successfully introduced in both the public and private health sector among front-line community workers.21–23 Were this system to be deployed again, we recommend considering replacing paper records with tablet computers to avoid a two-step data entry process, using user-centred design to minimize workflow disruptions. Tablet-based interventions in resource-poor settings must, however, consider the limited availability of electricity, poor internet connectivity and delayed service time in case of hardware failure. Back-up batteries, solar-powered chargers and back-up tablet devices are potential solutions.
Our quantitative analyses are based on data from 4 out of 14 sector hospitals. Although unlikely, we cannot exclude systematic differences in presentations and prescription patterns at other sector hospitals. Our study did not include data from other healthcare delivery systems at the Mela including the homeopathic, Ayurvedic, and Yunani centres (which collectively constituted <2% of healthcare expenditures), and charitable clinics operated by religious organizations.
Limitations of our data preclude important subgroup analyses, such as those based on geographic origins of the patients or the duration of their visit to the Mela. The cross-sectional nature of the study prevents any analysis of long-term outcomes. This is an important limitation: the modal duration of a visit to the Kumbh is 2–3 days while a significant communicable disease such as measles has a 7- to 21-day incubation period, so, the majority of patients who contract the virus during their stay at the Mela would not manifest the disease until after they have returned home to their villages. A cross-sectional digital surveillance system would likely underestimate disease transmission at the Mela.
Temporary digital surveillance systems risk creating their own data silos isolated from domestic or international health information systems. We recommend that new digital solutions be compatible with local or global interoperability standards like HL7 or FHIR.24,25 Industries outside healthcare, such as banking and finance, have successfully achieved software interoperability through Application Programming Interfaces (APIs) that serve as communication gateways between compatible databases or programs. The mHealth solutions that are API-based and compatible with inter-operability standards are likely to demonstrate the greatest staying power in the fast-evolving and rapidly changing ecosystem of mobile technology.
Funding
The study was funded and led by the FXB Center for Health and Human Rights and the South Asia Institute, both at Harvard University, with support from Weill Cornell Medicine and the University of California, San Francisco. The study sponsors had no role in study design; in the collection, analysis and interpretation of data; or in the writing of the report. All authors had full access to the data in the study and assume final responsibility for the decision to submit the article for publication.
Supplementary Material
Acknowledgements
The authors thank the medical and public health students of Motilal Nehru Medical College and Sam Higginbottom Institute of Agriculture, Technology and Sciences, in Allahabad, for their enthusiastic participation in the iterative design process and the daily data transcription.
Supplementary data
Supplementary data are available at Journal of Public Health online.
References
- 1. McConnell J. Mass gatherings health series. Lancet Infect Dis 2012;12(1):8–9. [DOI] [PubMed] [Google Scholar]
- 2. Memish Z, Stephens G, Steffen R et al. Emergence of medicine for mass gatherings: lessons from the Hajj. Lancet Infect Dis 2012;12(1):56–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Steffen R, Bouchama A, Johansson A et al. Non-communicable health risks during mass gatherings. Lancet Infect Dis 2012;12(2):142–9. doi:10.1016/S1473-3099(11)70293-6. [DOI] [PubMed] [Google Scholar]
- 4. Balsari Satchit. Leapfrog Technology and Epidemiology at the World's Largest Gathering. Health & South Asia, Harvard South Asia Institute, 2013.
- 5. Kazi DS, Prabhakaran D, Bolger AF. Rising above the rhetoric: mobile applications and the delivery of cost-effective cardiovascular care in resource-limited settings. Fut Cardiol 2015;11:1–4. [DOI] [PubMed] [Google Scholar]
- 6. Steinhubl SR, Muse ED, Topol EJ. Can mobile health technologies transform health care. JAMA 2013;310:2395–6. [DOI] [PubMed] [Google Scholar]
- 7. Christensen CM, Bohmer R, Kenagy J. Will disruptive innovations cure health care. Harv Bus Rev 2000;78(5):102–12, 99. [PubMed] [Google Scholar]
- 8. The World's Biggest Gatherings The Economist 2013, January 15. http://www.economist.com/blogs/graphicdetail/2013/01/daily-chart-9 (1 February 2015, date last accessed).
- 9. Balsari S, Leaning J.. Health and Safety at the Kumbh Mela In: Kumbh Mela: Mapping the Ephemeral Mega City. Sotuh Asia Institute, Harvard University. Berlin, Germany: Hatje Cantz Publishers, 2015, 150–68. [Google Scholar]
- 10. User Centered Design Basics US Department of Health and Human Services Usablity.gov. Accessed https://www.usability.gov/what-and-why/user-centered-design.html (1 July 2016, date last accessed).
- 11. Dabbs AD, Myers B, McCurry K et al. User-centered design and interactive health technologies for patients. Comput Inform Nurs 2009;27(3):175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Miller RH, Sim I. Physicians’ use of electronic medical records: barriers and solutions. Health Aff 2004;23(2):116–26. [DOI] [PubMed] [Google Scholar]
- 13. Ajami S, Bagher-Tadi T. Barriers for adopting electronic health records (EHRs) by physicians. Acta Inform Med 2013;21(2):129–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Vortmann M, Balsari S, Holman SR et al. Water, sanitation, and hygiene at the world's largest mass gathering. Curr Infect Dis Rep 2015;17(2):461. [DOI] [PubMed] [Google Scholar]
- 15. Kumar R, Indira K, Rizvi A et al. Antibiotic prescribing practices in primary and secondary health care facilities in Uttar Pradesh, India. J Clin Pharm Ther 2008;33(6):625–34. [DOI] [PubMed] [Google Scholar]
- 16. Sahoo KC, Tamhankar AJ, Johansson E et al. Antibiotic use, resistance development and environmental factors: a qualitative study among healthcare professionals in Orissa, India. BMC Public Health 2010;10:629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dua V, Kunin CM, White LV. The use of antimicrobial drugs in Nagpur, India. A window on medical care in a developing country. Soc Sci Med 1994;38(5):717–24. [DOI] [PubMed] [Google Scholar]
- 18. Spellberg B, Guidos R, Gilbert D et al. The epidemic of antibiotic-resistant infections: a call to action for the medical community from the Infectious Diseases Society of America. Clin Infect Dis 2008;46(2):155–64. [DOI] [PubMed] [Google Scholar]
- 19. Fauci AS, Marston ID. The perpetual challenge of antimicrobial resistance. JAMA 2014;311(18):1853–4. [DOI] [PubMed] [Google Scholar]
- 20. Rai Sairta. India Just Crossed 1 Billion Mobile Subscribers Milestone and the Excitement‘s Just Beginning. Forbes Asia. January 6 2016. http://www.forbes.com/sites/saritharai/2016/01/06/india-just-crossed-1-billion-mobile-subscribers-milestone-and-the-excitements-just-beginning/#7d2c6d295ac2 (25 April 2016, date last accessed).
- 21. National Health Portal Government of India http://www.nhp.gov.in/miscellaneous/m-health (25 April 2016, date last accessed).
- 22. Sean Lunde. The mHealth Case in India. Wipro Council for Industry Research 2013. http://www.wipro.com/documents/the-mHealth-case-in-India.pdf (25 April 2016, date last accessed).
- 23. Sorensen Rachel. An Inside Look at Mobile Health for Mothers in India. UN Foundation Blog. Global Connections http://unfoundationblog.org/an-inside-look-at-mobile-health-for-mothers-in-india/#sthash.lM7or2AX.dpuf (25 April 2016, date last accessed).
- 24. Health Level Seven International (HL7) www.HL7.org. (25 April 2016, date last accessed).
- 25. Fast Healthcare Interoperability Resources (FHIR) https://www.hl7.org/fhir/overview.html. (20 April 2016, date last accessed).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.