Abstract
Context
Consumption of sugar-sweetened beverages (SSBs) among children has been associated with adverse health outcomes. Numerous behavioral interventions aimed at reducing the intake of SSBs among children have been reported, yet evidence of their effectiveness is lacking.
Objective
This systematic review explored the effectiveness of educational and behavioral interventions to reduce SSB intake and to influence health outcomes among children aged 4 to 16 years.
Data Sources
Seven databases were searched for randomized controlled trials published prior to September 2016. Studies identified were screened for eligibility.
Study Selection
Trials were included in the review if they met the PICOS (Population, Intervention, Comparison, Outcome, and Study design) criteria for inclusion of studies.
Data Extraction
Data were extracted by 2 reviewers following Cochrane guidelines and using Review Manager software.
Results
Of the 16 trials included, 12 were school based and 4 were community or home based. Only 3 trials provided data that could be pooled into a meta-analysis for evaluating change in SSB intake. Subgroup analyses showed a trend toward a significant reduction in SSB intake in participants in school-based interventions compared with control groups. Change in body mass index z scores was not statistically significant between groups.
Conclusions
The quality of evidence from included trials was considered moderate, and the effectiveness of educational and behavioral interventions in reducing SSB intake was modest.
Systematic Review Registration
PROSPERO registration number CRD42014004432.
Keywords: behavior, children, interventions, meta-analysis, sugar-sweetened beverages
INTRODUCTION
Sugar-sweetened beverages (SSBs), namely soft drinks, carbonated beverages, fruit juices, and sweetened milk,1 are sources of high energy that have poor nutritional value and are considered the primary source of added sugar in children’s diets.2–4 The high consumption of SSBs is a widespread phenomenon among children and adolescents worldwide.2 Recent figures show that 80% of youth in the United States consume SSBs on a regular basis, contributing to approximately 11% of daily energy intake.3 Similar intakes are evident globally in both developed and developing countries. For example, SSBs contribute 14% of total energy intake among children in the United Kingdom (aged 4–18 years)5 and 10% of total energy intake among children in Mexico (aged 6–11 years).6 The increase in SSB intake is one of several dietary changes that have been attributed to the nutrition transition, which is characterized by rapid changes in dietary intake favoring the intake of energy-dense foods and beverages coupled with reduced physical activity. In fact, the high intake of SSBs among children and adolescents has been also associated with lower intakes of water, milk, fruits, and vegetables and a higher intake of highly processed foods and beverages. These changes in dietary behaviors are alarming because they are associated with increased risk of adverse health consequences, including lower micronutrient status and increased risk of dental caries, weight gain, diabetes, and hypertension.7–10
Compelling evidence supports the strong association and causal relationship between SSB consumption and increased risk of obesity. Results from well-powered prospective cohort studies and randomized controlled trials (RCTs) support the association between SSB consumption and weight gain in both the short term and the long term among children and adults.4,11,12 Furthermore, a direct dose–response relationship has been established between SSB consumption and long-term weight gain.4 Several plausible biological mechanisms have been proposed to explain these strong associations, such as decreased satiety and failure to reduce energy intake at meals subsequent to the consumption of liquid calories such as SSBs, which can lead to a positive energy balance and weight gain.2 Other proposed mechanisms include increased blood glucose and insulin concentrations resulting from consumption of rapidly absorbed sugars in SSBs, leading to high dietary glycemic loads and a cascade of changes in appetite-regulating hormones and inflammatory biomarkers. These changes in turn can contribute to increased risk of type 2 diabetes and cardiovascular disease in children.2,13,14
Public health interventions targeting SSB consumption and other unhealthy dietary behaviors in children have increased over the past 2 decades in an effort to help curb the rising rates of obesity. The majority of these interventions adopt educational and behavioral approaches that focus on changing the knowledge, the attitude, and, subsequently, the behavior of children toward SSBs. These interventions have been conducted through school-based didactic lessons and interactive classroom activities15–17 or through home- and community-based strategies, including the distribution of simple educational messages to parents highlighting the importance of replacing high-calorie beverages with healthier alternatives.18–20 Other supportive interventions include environmental changes, such as school-level policies to limit the availability of and the access to SSBs and other competitive foods and beverages with minimal nutritional value within the school environment,21,22as well as in-school price policies,23 governmentally mandated SSB taxes, or regulations restricting sales within retail and food service establishments.23–25
Despite the use of diverse interventions to limit SSB consumption among children and adolescents, evidence of what constitutes successful and effective interventions is still minimal. Few reviews26,27 to date explored the effectiveness of interventions aimed at reducing SSB consumption among children and adolescents, with 1 recently published review examining the effects of interventions on both SSB and water intake among children, adolescents, and adults.28 Given the serious implications of high SSB consumption for children’s diet and health and the importance of identifying which educational interventions best predict behavioral change, the aims of the present systematic review are as follows: (1) to explore the impact of educational and behavioral interventions to reduce the intake of SSBs among children and adolescents across different settings (school and nonschool settings); and (2) to assess the effect of these interventions on change in body weight and other health outcomes, taking into consideration which behavioral change techniques were included in these interventions.
METHODS
Inclusion criteria
Table 1 29 describes the PICOS (Participants, Interventions, Comparisons, Outcomes, and Study design) criteria used to define the research question for this review. In addition, the systematic review and meta-analysis were performed in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (see Appendix S1 in the Supporting Information online). Given that RCTs are considered the gold standard for establishing causal conclusions and providing reliable evidence because they minimize the risk of confounding factors influencing the results,30 this systematic review included only RCTs.
Table 1.
PICOS criteria for inclusion and exclusion of studies29
| Parameter | Criteria |
|---|---|
| Participants | Children and adolescents aged 4 to 16 years |
| Intervention | Educational or behavioral interventions targeting the reduction of SSB consumption as one of the main purposes. Acceptable settings in which the educational intervention was delivered were school, home, and community settings |
| Comparison | Control groups with no intervention |
| Outcomes | Primary outcome of interest was the reduction in SSB consumption after delivery of the intervention. Outcome was measured as a decrease in the intake of soft drinks, sweetened juices, or any sweetened drink defined in the included study and was quantified using the difference in consumption of these beverages pre- and postintervention and after follow-up. Secondary outcomes included any of the following clinical or health outcomes affecting a child’s health status: reduction in obesity prevalence (status); changes in body composition measures (eg, body mass index [BMI] z scores based on age- and gender-specific growth charts); reduction in dental caries measured by the difference in decayed, missing, and filled teeth; reduction in cardiovascular disease risk factors; reduction in risk of any chronic disease, including type II diabetes mellitus, hypertension, dyslipidemia, and orthopedic ailments |
| Study design | Any setting, including school-based and out-of-school (home or community) settings, conducted in a developed or developing country |
Search strategy
A comprehensive literature search was conducted for trials assessing the impact of behavioral and educational interventions on health behaviors and outcomes of children and adolescents. The search was limited to articles published in English. Two authors (A.A.R. and L.J.) conducted the initial search and screened the identified articles between June and September 2014. The same 2 authors conducted an updated search and screening in September 2016 by electronically searching the following databases from the start of the databases through September 30, 2016: Applied Social Sciences Index and Abstracts; Cumulative Index of Nursing and Allied Health Literature (accessed via EBSCO); Cochrane Central Register of Controlled Trials; Embase (accessed via Ovid); MEDLINE (accessed via Ovid); PubMed; PsycINFO (accessed via Ovid); Web of Science; and Google Scholar. Appendix S2 in the Supporting Information online provides a complete list of the search strategies used for the electronic databases. Two authors (A.A.R. and L.J.) also hand searched other sources, including relevant journals such as the Journal of Nutrition, Journal of the Academy of Nutrition and Dietetics, Journal of Nutrition Education and Behavior, and Public Health Nutrition. They closely scanned the reference lists of all articles included in this review and of other relevant systematic reviews to identify any additional relevant manuscripts or interventions.
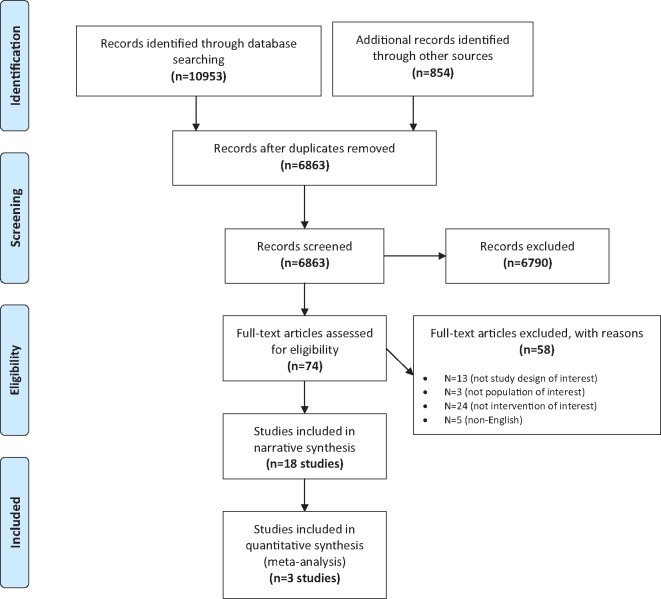
Figure 1 outlines the screening process and shows the number of studies excluded at each stage. A total of 16 trials were included in the systematic review (Table 215,17–20,31–45), whereas 58 studies were excluded from the analysis for reasons summarized in Appendix S3 in the Supporting Information online.
Figure 1.
Flow diagram of the literature search process.
Table 2.
Characteristics of the included studies
| Reference, country | Funding source | Characteristics of participants | Intervention | Setting (type and duration of intervention, follow-up period, if stated) | Change in SSB consumption (pre- and postintervention) | Other health-related outcomes | Overall conclusions |
|---|---|---|---|---|---|---|---|
|
Fogarty International Center, National Institutes of Health, USA |
|
Nutritionists delivered milk at home and provided 1 serving/d for each sibling in the household; educational instructions about consuming the delivered beverages were provided to the family; parents encouraged to remove SSBs from home |
|
SSB intake decreased by a mean of − 711.0 ± 37.7 g/d in intervention group and increased by 71.9 ± 33.6 g/d in control group. Milk intake increased by a mean of 450 g/d in intervention group and did not change in control group | Lean body mass was greater in intervention group (0.92 ± 0.1 kg) than in control group (0.62 ± 0.11 kg) | Change in beverage consumption did not significantly affect fat mass but increased accretion of lean mass (shown by linear growth) for boys but not for girls |
|
Bavarian Ministry of Environment, Health and Consumer Protection, and Stiftung Kindergesundheit, Munich, Germany |
|
|
|
After 6 mo: 60.4% of intervention group and 47.7% of control group reported low consumption of high-calorie drinks (P < 0.0001). After 18 mo, low consumption of high-calorie drinks increased among both intervention and control groups. Odds ratio of low consumption of high-calorie drinks in intervention group vs in control group was 1.66 (1.16–2.38), P < 0.001 | Prevalence of overweight and obesity was not statistically significant between intervention and control groups. Trend of less overweight was observed in intervention group, with 13.9% being overweight in the intervention group vs 18% in the control group (P = 0.053). 15.6% were obese in the intervention group vs 16.7% in control group (P = 0.58) | Intervention affected FV consumption. Effect on intake of energy-rich drinks was seen in lower parental education sample only |
| Norwegian Research Council, Oslo, Norway |
|
|
|
|
|
Intervention was more effective in girls than in boys. Subgroup analyses allowed for observation of significant changes in SSB intake, BMI, and BMI z scores among girls only | |
|
Research Support Foundation for the State of Rio de Janeiro (FAPERJ), Rio de Janiero, Brazil |
|
|
|
Significant decrease in consumption of sodas (P = 0.02) in intervention group (MD = −0.2, 95%CI. −0.30 to − 0.11) vs control group (−0.08; 95%CI, −0.18 to 0.2). No significant decrease in juice intake (P = 0.66). | No statistical difference between intervention and control groups for BMI | Healthy eating was encouraged in addition to reducing intake of SSBs. Replacement of SSBs with sugar-containing juices led to decrease in SSB intake but not in BMI |
|
Not stated |
|
Internet-based intervention consisting of 8 modules (available on the internet) aiming to decrease the intake of SSBs and increase the intake of FV. Teachers were given 15 min to explain the 8 lessons over a 10-wk period |
|
|
Intervention had no significant effect on BMI, WC, or percentage of students being overweight or obese at 2-y follow up | Effect on SSB intake was evident only for short term, whereas the effect on BMI was nonsignificant at 2-y follow-up |
|
Flemish government and the Policy Research Centre for Sport, Physical Activity and Health Leuven, Belgium | 2991 pupils from 15 schools: 5 schools as intervention schools with parental support; 5 schools as intervention schools without parental support; and 5 schools as control group |
|
|
No significant intervention effects on SSB consumption were found among boys or girls at the end of the academic year (after 9 mo) | Intervention affected fat-related outcomes among girls with parental support. No effect for soft drinks and water in boys or in girls. Parental support and environmental support added value to personalized interventions | |
| Scholarship from the Florence Nightingale Foundation, London, UK |
|
Intervention focused on 1 h of additional health education session during each school term. Teachers reiterated the message. Message promoted drinking of water and tasting of FV. In addition, each class was given a tooth immersed in carbonated beverages to shown the harmful effects of these drinks |
|
|
After 1 y, there was no significant difference in BMI (MD = 0.13; SD, −0.1 to 0.3) or z score (MD = 0.04; SD, −0.04 to − 0.12). After 3 y, age- and sex-specific BMI z scores increased in control group by 0.10 (SD, 0.53) from baseline and decreased in intervention group by − 0.01 (SD, 0.58). MD was 0.10 (−0.00 to 0.21), P = 0.06. BMI increased in control group by 2.14 and increased in intervention group by 1.88. MD was 0.26, P = 0.12 | A small reduction in intake of carbonated drinks was associated with a reduction in the number of overweight and obese children at 12 mo, but this modest effect was no longer evident after 36 mo | |
|
National Heart, Lung, and Blood Institute, Bethesda, MD, USA | 303 US girls aged 8–10 y |
|
|
Decrease in SSB consumption was observed among girls in the intervention group, yet this decrease was marginally significant. MD = −0.19 (95%CI, −0.39 to 0.09) | No statistically significant difference between intervention and control groups for BMI or waist circumference | Intervention group showed a decrease in servings/day for SSB intake. Direction of both interventions was encouraging |
|
Baden-Württemberg Foundation, Stuttgart, Germany |
|
|
|
24.6% of boys and 22.6% of girls drank SSBs at least 1 time per week. No significant difference in SSB intake at baseline between intervention and control groups. In addition, there was no significant gender difference between intervention and control groups. SSB intake declined in intervention and control groups, but this decline was not significant | No difference observed between intervention and control groups in the amount of SSBs consumed | |
|
Grant no. 05HS026 from the German Federal Ministry of Food, Agriculture, and Consumer Protection, Bonn, Germany |
|
Intervention included educational and environmental components to promote increased water consumption and aimed to decrease the risk of overweight children. Educational component: Four 45-min classroom lessons about water requirements of the body and the water circuit in nature. Environmental component: water fountains were installed in intervention schools, and students received plastic water bottles |
|
Intervention had no significant effect on juice consumption or soft drink consumption in intervention or control group | Reduction in prevalence of overweight children in intervention schools vs control schools (OR = 0.69; 95%CI, 0.48–0.98; P = 0.04.). Change in BMI SD scores between intervention and control groups, adjusting for baseline BMI SD scores, did not differ significantly (−0.004; 95%CI, 0.045–0.036) | Intervention with educational and environmental components was effective in preventing overweight and obesity among school-aged children |
|
Fundação para a Ciência e Tecnologia (FCT), Lisbon, Portugal |
|
Educational intervention in 2 parts: (1) Training delivered to teachers, and (2) educational intervention delivered to children. Intervention promoted healthy diet by encouraging water intake and discouraging intake of other beverages. Teachers attended 12 sessions over 6 mo. Based on Health Promotion Model and Social Cognitive Theory |
|
Intervention had no effect on SSB consumption before and after the intervention, even after adjustment for confounders. Note: SSB consumption increased in both groups (OR = 1.66, adjusted P = 0.578) | Children who received the intervention showed a reduction in intake of low-nutrient, energy-dense foods and beverages. Intervention had no effect on SSB intake | |
|
Sunflower Foundation: Health Care for Kansas, Topeka, KS, USA |
|
Educational intervention with environmental component and parental involvement. Girls received assignments to be completed at home. Intervention delivered by troop leaders. One of the targeted behaviors was to drink water instead of SSBs at mealtimes. Based on Social Cognitive Theory, including role modeling, skill building, self-efficacy enhancement, and reinforcement |
|
No significant effect on SSB intake | No significant effect on BMI for girls (P = 0.54) or parents (P = 0.26) | Troops in intervention group adhered to healthy eating guidelines more than troops in control groups. Intervention was not efficient, and no evidence was shown for BMI, habitual PA, FV intake eating with TV, and SSB consumption |
|
Brazilian National Research Council, Brasília, Brazil |
|
|
|
|
Mean change in BMI from baseline to end of school year was not significant between intervention and control groups (mean BMI = 0.1; 95%CI, −0.06, P = 0.10). Among girls who were overweight at baseline, a statistically significant reduction in BMI was observed (P = 0.009) | SSB intake decreased, but the need to emphasize reduced total juice intake remained. BMI reduction was significant among overweight girls only |
|
Grants from the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, Bethesda, MD, USA, and the American Diabetes Association, Alexandria, VA, USA |
|
Educational and environmental components emphasizing different themes; 1 specific theme highlighted each. Intervention consisted of 4 integrated components: nutrition, physical education, behavior, and communication. Nutrition intervention goals were to eliminate high-fat milk, fruit juice, and beverages with added sugar. |
|
|
Small effect of intervention on diet | |
| Parental involvement component was included in this intervention | |||||||
|
Netherlands research programme weight gain prevention from the Netherlands Heart Foundation (NHF-NRG) |
|
The nutrition-related educational component of the DOiT intervention was included in 11 lessons. Messages reinforced the elimination of SSBs and high-energy snacks from the diet. DOiT intervention used an intervention mapping protocol and integrated methods of behavioral change, including: self-monitoring and evaluation reward, goal setting, environmental changes, and social encouragement |
|
|
|
Positive effects on SSB intake in all participants, in both short and long term, and on sum of skinfold thickness in girls |
| Grant from ZonMw (major funding body), The Hague, the Netherlands |
|
|
|
van Grieken et al. (2014)45 reported a higher percentage of children drinking ≤ 2 glasses per day (increase from 32% at baseline to 55% at follow-up in intervention group and from 33.3% to 47.9% in control group). Difference between intervention and control groups was not significant | van Grieken et al. (2013)44 reported no change in BMI between intervention and control groups [intervention (BMI=19.53 kg/m2; SD, 1.72) and control (BMI=19.55kg/m2; SD, 1.74)] | Intervention had no effect on the targeted health behavior |
Abbreviations: BMI, body mass index; CD, compact disc; DOiT, Dutch Obesity Intervention in Teenagers; FV, fruit and vegetable; MD, mean difference; PA, physical activity; SSB, sugar-sweetened beverage; STOPP-T2D, Studies to Treat or Prevent Pediatric Type 2 Diabetes; TV, television; WC, waist circumference.
Data collection and analysis
Two authors (A.A.R. and L.J.) independently screened the titles and abstracts of the identified articles. Articles judged as potentially eligible by at least 1 author were retrieved for full-text review. Authors A.A.R. and L.J. independently screened the full text of the retrieved articles for eligibility, using a standardized form with explicit inclusion and exclusion criteria derived from Cochrane guidelines.46 They resolved disagreements through discussion or by consulting a third author (P.A.). Afterward, they independently extracted data from each included study, resolving disagreements through discussion. The Cochrane guidelines and format for data extraction were used when entering data, and Review Manager software (version 5.3.5) was used for data management. The collected data were related to 5 aspects of the review: (1) methods (study design, unit of randomization, and analysis); (2) participants (population characteristics and number of participants randomized and evaluated per arm); (3) intervention (educational and behavioral components, duration of intervention and follow-up, and description of control group); (4) outcomes (primary and secondary outcomes defined for this review); and (5) other notes such as statistical methods used, sources of funding, and registration identifier for interventions and the RCTs, if available. In addition, the authors attempted to contact trial authors if reported data were incomplete.
Agreement between A.A.R. and L.J. regarding study inclusion during the title and abstract screening and the full-text screening was assessed using the Kappa statistic.47 Kappa values were interpreted as following: 0 to 0.20 represented slight agreement; 0.21 to 0.40 fair agreement; 0.41 to 0.60 moderate agreement; 0.61 to 0.80 substantial agreement; and greater than 0.80 almost complete agreement. Agreement between authors on study eligibility was found to be substantial (κ = 0.72).
Risk of bias
The risk of bias was assessed at the study level using the Cochrane risk-of-bias tool. Two authors (A.A.R. and L.J.) independently assessed the methodological quality of each of the included studies. They resolved disagreements by discussion, and persistent discrepancies were resolved by discussion with a third author (P.A.). Risk of bias was assessed according to the following criteria: random sequence generation (selection bias); allocation concealment (selection bias); blinding of participants and personnel (performance bias); blinding of outcome assessment (detection bias); incomplete outcome data (attrition bias); and selective reporting and whether the study was free of selective outcome reporting (reporting bias). Details about risk-of-bias assessment for all included studies are presented in Appendix S4 in the Supporting Information online.
Subgroup analysis and investigation of heterogeneity
Heterogeneity between trials was assessed by visually inspecting the forest plots and by estimating the percentage of heterogeneity between trials that was not due to chance. To measure the latter, the I2 statistic, as described in the Cochrane handbook,46 was used. Sources of heterogeneity were explored if the I2 statistic exceeded 25%. Subgroup analyses were conducted to explore the reason for heterogeneity and the influence of the latter on the effect estimate. For subgroup analyses, studies included in the meta-analysis were stratified into subgroups according to the setting of the intervention (school-based settings and outside-of-school settings such as home- and community-based behavioral interventions).
Assessment of reporting and publication bias
Selective reporting was assessed by trying to identify within-study reporting bias. If the study protocol or trial registered in a certain trial registry was available, the lists of outcomes from those sources were compared with the outcomes reported in the published paper. If not, then outcomes listed in the Methods section of the published paper were compared with the outcome listed in the Results section. Publication bias was further assessed by creating an inverted funnel plot in the Review Manager file for the primary outcome relative to the intake of SSBs.
Data synthesis
For the meta-analysis of continuous outcomes, the mean differences (MDs) in the consumption of SSBs of all trials were pooled using a random-effects model. Following recommendations in the Cochrane handbook,46 the unit of outcome data was converted to a standardized scale before pooling measures. For the change in SSB intake, the unit of measurement used was milliliters per day (mL/d). A nutrient analysis software was used for converting equations and units in this review; for example, 1 g of sugar-sweetened fluid is equivalent to 1 mL, and 1 glass of sugar-sweetened fluid is equivalent to 240 mL (NutritionistPro software, version 7.1.0, First Data Bank, Axxya Systems, San Bruno, CA). Instead of crude body mass index (BMI) measurements, BMI z scores were used to assess change in BMI. Body mass index z scores, which are equivalent to BMI-for-age percentiles, are measures of relative weight adjusted for child’s age and gender that are calculated using appropriate reference growth charts48 such as the Centers for Disease Control and Prevention growth charts,49 the World Health Organization growth charts,50 or other country-specific references. When units could not be converted, the trials reporting those units were not included in the meta-analysis.
RESULTS
Figure 1 shows the detailed steps of the literature search and screening process. A total of 16 trials were included in the systematic review, of which only 3 were included in the meta-analysis of the primary study outcome. Of the 16 trials included, 12 were school based, 8 of which included educational approaches alone (not combined with environmental interventions), whereby the reduction in SSB consumption of children and adolescents was one of the main targeted behaviors.15,17,31,34–36,40,43 The remaining 4 school-based trials included a combination of educational and environmental components.18,19,32,33,39,42 As for the 4 non–school-based trials, 1 included an educational intervention only,44,45 whereas 3 others included both educational and environmental interventions.20,37,41 Details about all included trials, including characteristics of study participants, type of intervention (school or community based), duration of intervention, and length of follow-up, are shown in Table 2.
Effects of interventions were explored on the basis of primary and secondary outcomes of the review.
Reduction in SSB intake (primary outcome)
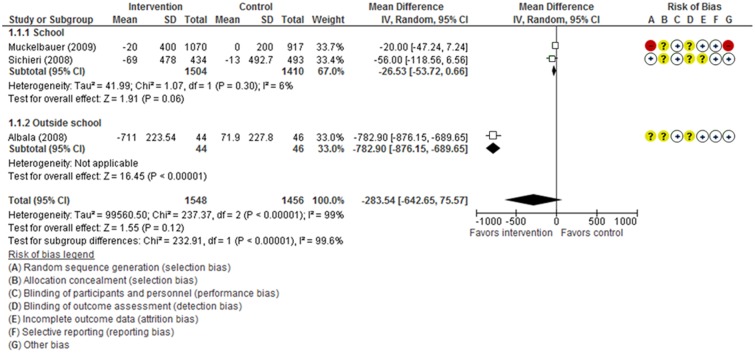
Of the16 included trials evaluating change in SSB intake, only 3 provided statistical data that could be pooled into a meta-analysis. Two of these were conducted in a school-based setting15,39 and 1 in a home-based setting.20 The first school intervention, conducted by Muckelbauer et al.,39 included educational and environmental components, whereby four 45-minute classroom lessons highlighting the water needs of the body and the water circuit in nature, among other nutrition messages, were provided to students by trained teachers. In addition, the intervention component included installing water fountains in intervention schools and providing students with plastic water bottles to be refilled during the school day. The intervention group in the school trial conducted by Sichieri et al.15 received only an educational program, which consisted of ten 1-hour sessions supported by classroom activities, banners, and the distribution of plastic water bottles to all students. In the home-based study conducted by Albala et al.,20 milk was distributed to children at home, and parents were provided with educational instructions supporting the consumption of the delivered beverages and the removal of SSBs from the home environment.
The meta-analysis of these 3 trials (n = 3004 participants) showed that behavioral and educational interventions are associated with a trend toward reduction in SSB intake compared with no intervention; however, this trend did not reach statistical significance [MD, −283.54; 95%CI, −642.65 to 75.57; P = 0.12) (Figure 2). The I2 value indicated that the percentage of the variability in effect estimates, which is due to heterogeneity rather than to sampling error (chance), was very high (I2 = 99%). Thus, the outside-the-school study conducted by Albala et al.20 was removed from the meta-analysis. Sensitivity analysis excluding this study reduced heterogeneity (I2 =6%) while increasing the overall strength of the results to borderline significance (MD, −26.53; 95%CI, −53.72 to 0.66; P = 0.06).
Figure 2.
Forest plot showing the reduction in sugar-sweetened beverage (SSB) intake in the intervention and control group (no intervention) in children in schools (1.1.1), outside schools (1.1.2), and overall. A random-effects model method was employed to calculate standardized mean difference with 95%CIs.
Reduction in prevalence of overweight and obesity and reduction in BMI (secondary outcomes)
Two trials assessed the change in overweight and obesity status and reported change in terms of prevalence.15,17,36 The Christchurch Obesity Prevention Programme in Schools (CHOPPS) trial conducted by James et al.36 was focused primarily on discouraging the consumption of soft drinks among children in southwest England and replacing this behavior with a healthier one. The authors found a significant difference in the prevalence of overweight children between the control and intervention groups at 12 months after the study initiation, but that difference was smaller and nonsignificant after 3 years.36 In the school trial by Sichieri et al.,15 the significant decrease in the intake of carbonated beverages was not coupled with a significant decrease in obesity prevalence. On the contrary, prevalence of obesity increased in both arms within that study, although the difference did not reach statistical significance.
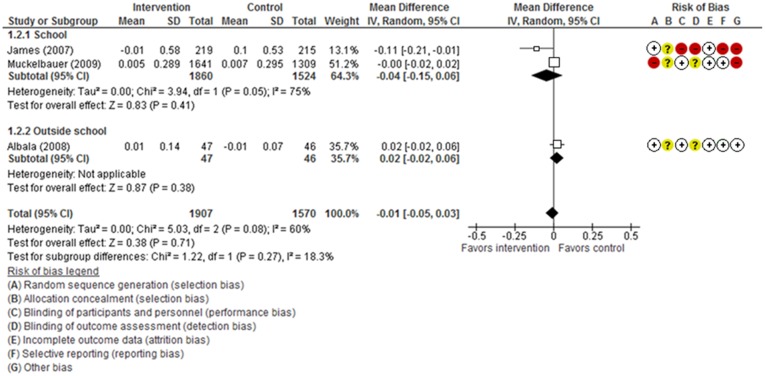
In addition to overall prevalence of overweight and obesity, change in BMI was reported in 11 trials that were included in this review. However, only 3 trials reported this change in terms of age- and gender-adjusted BMI z scores, which could be pooled into 1 analysis.17,20,36,39 The 2 school-based trials included in the meta-analysis, ie, the educational CHOPPS intervention by James et al.17,36 in the United Kingdom and the combined educational and environmental intervention by Muckelbauer et al.39 in Germany, focused on increasing water consumption and reducing the consumption of carbonated beverages and sweetened drinks. Similarly, the out-of-school intervention conducted by Albala et al.20 in Chile focused on reducing SSB consumption by providing milk as a healthy replacement within the home setting, along with supportive educational messages. The meta-analysis of the 3 trials, which included 3474 participants, found that behavioral and educational interventions, compared with no intervention, had no significant effect on the reduction in adjusted BMI z scores (MD, −0.01; 95%CI, −0.05 to 0.03; P = 0.71) (Figure 3). The percentage of the variability in effect estimates that could be attributed to statistical heterogeneity rather than to sampling error (chance) was moderate to high (I2 = 60%). In addition, the test for subgroup effect was not statistically significant for the subgroup analysis (in-school interventions vs out-of-school intervention), with a P value of 0.27. None of the other health-related secondary outcomes, as defined for the present review, were assessed by the trials included in this review.
Figure 3.
Forest plot showing the reduction in body mass index (BMI) z scores in the intervention group relative to the control group (no intervention) among children in schools (1.3.1), outside schools (1.3.2), and overall. A random-effects model method was employed to calculate standardized mean difference with 95%CIs.
Quality of the evidence
Overall, the quality of the evidence from the 16 trials included in this review, as assessed separately by 2 reviewers, was considered moderate, given that the majority of the studies scored “low risk” in the domains related to selection bias (random sequence generation), attrition bias, reporting bias, and other bias. In addition, slightly less than half of the studies scored low in the domain related to performance bias, which includes blinding of participants and personnel. The majority of the studies scored “unclear risk” in the domain of allocation concealment. However, more than a quarter of the included studies scored “high risk” in the domain related to detection bias (blinding of outcome assessment), with the remaining studies scoring between low and unclear risk. Figure 4 shows a summary of the risk-of-bias assessment across all included studies. A more detailed justification supporting the judgments on each of the risks of bias is provided in the risk-of-bias figure shown in Appendix S4 in the Supporting Information online.
Figure 4.
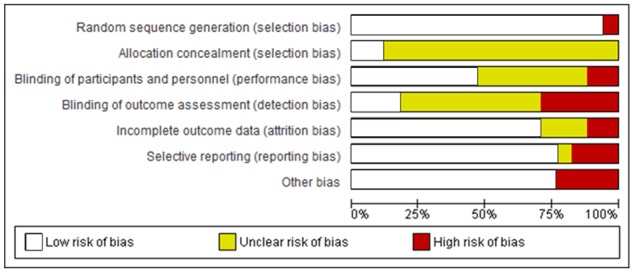
Risk of bias across all included studies.
DISCUSSION
This systematic review aimed to assess the effectiveness of educational and behavioral interventions in reducing SSB intake among children and adolescents aged 4 to 16 years and to determine the impact of such interventions on change in body weight and other related health outcomes. Overall, educational and behavioral interventions included in this review, when compared with no intervention, were found to be successful in reducing SSB intake as the primary outcome among children and adolescents. Meta-analyses of a subset of included studies validated results from individual trials showing that the trend toward reduction in SSB consumption approached statistical significance in those studies conducted within school-based settings (P = 0.06). However, there was insufficient evidence to support a positive effect of these interventions on secondary outcomes such as a reduction in the prevalence of overweight and obesity among children and adolescents as well as other physical measures such as change in BMI z scores adjusted for age and gender.
The present review goes beyond pooling results from various trials into 1 meta-analysis, as it examines the characteristics of interventions and the different approaches used to change the behavior of children and adolescents toward SSB consumption. School-based trials were examined separately from home- or community based trials, and the different intervention strategies and techniques used to implement an educational vs a combination of educational and environmental interventions were elaborated in light of the existing literature.
Effect of school-based educational and environmental interventions on reduction of SSB intake
Twelve school-based trials were included in this review. Results from the meta-analysis of 2 school-based trials15,39 showed a trend toward reduction in SSB intake among young children in the intervention groups compared with the control groups, and this trend approached statistical significance. This finding was in line with results reported in 6 of the remaining 10 school-based trials.17,19,31,34,35,43
There are several reasons for the positive impact of school-based interventions in reducing SSB consumption. First, schools are well positioned to conduct educational and behavioral interventions, since children spend prolonged periods of their day within this setting. At school, children can receive developmentally and culturally appropriate didactic lessons and be involved in interactive activities that promote healthy dietary and lifestyle behaviors.17,51 In addition, schools provide children with practical opportunities to translate learned concepts from the classroom setting to daily behavioral choices reflected in the foods selected from the cafeteria, vending machines, fundraising activities, and other school-based events. In fact, the school environment can dictate what foods and beverages are offered or sold within the school and how these choices can negate or reinforce nutritional messages delivered through the curriculum and other supportive educational strategies. Furthermore, children have the opportunity to learn from their teachers, who can serve as role models,51,52 and from their peers, through observation of peer behaviors and direct personal interaction. In fact, peer influence is considered one of the main factors that can contribute to the change in dietary and lifestyle behaviors of adolescents and has been suggested as an integral component in prevention and intervention efforts aimed at promoting and maintaining healthy behaviors.53
Another possible reason for the success of school-based interventions is the use of behavioral change theories in the design and implementation phases. The Social Cognitive Theory and the Theory of Planned Behavior were the most commonly used behavioral change theories in the included trials.18,34,35,38–40,43 These theory-based educational interventions included a number of constructs that can be summarized as follows: increasing the confidence of children and young people (self-efficacy); developing the knowledge and skills needed to change targeted behaviors (behavioral capacity); and role modeling of healthy behaviors (observational learning). However, only 1 trial, namely the Dutch Obesity Intervention in Teenagers, conducted among 12- to 14-year-old schoolchildren in Amsterdam,43,54 assessed the impact of the planned interventions relative to the mediators of change when addressing targeted behaviors, including SSB consumption.
The benefits of using theoretical frameworks and constructs in the design of educational and behavioral interventions targeting dietary and lifestyle behaviors have been well established in the scientific literature. These benefits include the ability of program planners to specify methods for changing behaviors, identify the timing and duration needed for interventions to be effective, and explore the combination of strategies that can best lead to the anticipated outcomes.55 In addition, theories can assist researchers and program evaluators in identifying what components of interventions succeed in changing mediating variables, which in return can change the intended behaviors.56 Thus, robust instruments need to be developed and used to measure which components or constructs of theories can best explain the reasons behind the success of interventions.55
Other factors that may explain the effectiveness of school-based interventions in reducing SSB intake include parental involvement. A commonly used strategy for involving parents in 7 of the school-based trials15,18,19,31,34,38,42 in this review was the dissemination of educational materials in the form of booklets, tip cards, and fact sheets that promote healthy eating, including the reduction of SSB consumption and replacing SSBs with healthier alternatives such as water and unsweetened milk. These materials are intended as reminders for parents to reinforce at home those messages that children receive at school. In fact, research has shown that involving families and parents in school-based interventions targeting the dietary behaviors of children can be effective, particularly among preschoolers and young children.54–57 Parents can play an important role in guiding the dietary intake and physical activity of their children by providing adequate and healthy foods at home, encouraging children to consume adequate amounts and types of foods, modeling healthy behavior, and encouraging children to be physically active while at home or at school.
Four school-based trials in this review utilized environmental strategies in addition to educational components within the classroom to change the availability and accessibility of soft drinks and to promote water as a healthier alternative.18,39,42 It is worth noting that these environmental strategies are in line with the school policies and programs that have gained momentum over the past decade in an attempt to prevent, if not reverse, the problem of childhood obesity through limiting the consumption of low-nutrient, energy-dense beverages, including SSBs.58–61 Despite these policies, researchers disagree about whether limiting the availability of sodas is sufficient to reduce soda consumption if other nonsoda energy-dense SSBs are still available within schools and if specific nutritional guidelines for all competitive foods and venues are not implemented as part of school policies.62 This is addressed in the trial of Sichieri et al.,15 included in the current review, which shows that the reduction in SSB intake within a school-based intervention was accompanied by an increase in the intake of powdered fruit-flavored juice drinks, which have a higher sugar content than the regular sodas. Thus, evidence suggests that efforts aimed at decreasing energy intake through liquids should focus on all SSBs, and not just sodas. Furthermore, these studies highlight the need for more than policy- and environmental-level changes to achieve the desired behavioral change among children and young people. Environmental interventions alone, without educational interventions at the school level, may not be sufficient to change the attitude and preference of children toward the various types of SSBs and might be inadequate to achieve the buy-in of students, who are the main target group of such programs.
Effect of out-of-school educational and environmental interventions on reduction of SSB intake
In this review, 4 trials were conducted in out-of-school settings: 2 were home/family based,20,44 1 was community based,41 and 1 included a mix of community- and family-based interventions.37 One trial used an educational approach only,37 while the remaining 3 trials included a combination of educational and environmental components.20,41,44 It was not possible to pool the results of the 4 community-/home-based interventions into 1 meta-analysis because the effects of the interventions were reported differently. Nevertheless, 2 of these trials showed independently a significant reduction in SSB intake favoring the intervention,20,37 whereas the other 2 showed no significant effect.41,45 The first trial that showed a positive effect included the delivery of milk to homes, combined with minimal supportive educational material,20 whereas the second, more elaborate trial was based on the Social Cognitive Theory and included 34 educational sessions conducted over 2 years at local community centers.37 As noted earlier, the use of theories of behavioral change, particularly the Social Cognitive Theory, has been shown to be effective in changing the dietary behavior of school-aged children. However, the study by Klesges et al.37and the 2 other trials conducted in out-of-school settings,41,44 all of which used theoretical models, did not explore the impact of these interventions on the mediators of change. Thus, it is still not possible to evaluate what constructs best predict a change in behavior, as is the case with educational school-based interventions.
Effect of SSB reduction on BMI and the prevalence of obesity
This meta-analysis did not support a positive effect of behavioral interventions targeting SSB intake on a reduction in the prevalence of overweight and obesity. These results are not surprising, given that the only 2 trials identified to measure the change in prevalence of overweight and obesity among children in this review, those by Sichieri et al.15 and James et al.,17 focused on a single message that included reducing soda consumption, which may have been insufficient to limit excessive weight gain. Obesity is a complex and multifactorial problem,63 and thus other dietary and lifestyle behaviors besides the consumption of SSBs may have contributed to excessive weight gain in children.64–66 Another explanation is that compensatory behaviors may be adopted by children when sodas are replaced by other sugar-loaded, energy-dense beverages, including sports drinks and flavored juices. The consumption of sugar-rich beverages and low-nutrient, energy-dense foods as a replacement for soda consumption may offset the reduced caloric intake, which in turn can lead to excessive weight gain.15
Furthermore, of the 11 trials in this review that reported changes in BMI, only 3 provided statistical data that could be included in the meta-analysis, which showed no statistical difference between intervention and control groups with regard to reduction in age- and gender-specific BMI scores.20,36,39 In addition, no specific pattern or significant difference in the effect of interventions on changes in BMI was observed when subgroup analysis was conducted to compare school-based interventions with out-of-school interventions. According to the published literature, school-based interventions have considerable impact on the health behaviors of children and adolescents, yet results regarding the effect of these interventions on children’s body weight, BMI, and other anthropometric measurements are inconsistent.57,58 This may be attributable to variations in study design, sample size, and duration of the interventions. Other limiting factors may include high dropout rates, lack of follow-up, and potential selection bias, whereby generally only motivated families permit their children to be enrolled and followed up in these studies.57
STRENGTHS AND LIMITATIONS
This review has a number of strengths. It includes a rigorous methodology whereby explicit eligibility criteria, an exhaustive literature search, and systematic approaches to study selection, data abstraction, and data synthesis were used. In addition, this review included studies with single and multicomponent interventions conducted in various settings (school, home, and community based) and in different countries. Furthermore, the various characteristics of the studies and the behavioral change techniques adopted in these interventions were explored.
On the other hand, findings from this review need to be considered in light of several limitations. The overall completeness of the data from trials was a major challenge: 13 of the 16 eligible trials could not be included in the meta-analysis because of the variability in scales used to report the outcomes of interest. These 13 studies would have contributed 17,555 additional participants within the meta-analysis (as compared with the 3004 participants actually included). In fact, this is a common challenge in the meta-analysis of continuous outcomes, as different scales and units of measure are often used, making it difficult to meta-analyze and interpret outcomes from different interventions.67,68 It is also worth noting that there has been no clear consensus about the minimum number of studies that can be used in a meta-analysis.69 Nevertheless, according to a study by Valentine et al.,70 at least 2 studies are needed to conduct a meta-analysis, given that other synthesis techniques may be less transparent and are less likely to provide valid results. Despite this limitation, most of the trials included in the present review showed effects similar to the findings reported from the meta-analysis conducted of fewer studies within the same review.
As with other reviews, this systematic review may have been subject to potential biases that could not be accounted for, such as clinical heterogeneity. Such heterogeneity may be attributed to variability in the setting, baseline characteristics of participants, or intervention strategies of different trials. Nevertheless, the heterogeneity of trials was taken into consideration, as a random-effects meta-analysis was chosen over fixed-effects meta-analysis. The former is preferable because it allows for differences in treatment effects between studies.71 In addition, as in other meta-analyses, publication bias is a potential concern. However, inspection of the funnel plot in this systematic review produced limited evidence of publication bias. Another limitation of this review is the exclusion of non-English studies.
CONCLUSION
Findings from this systematic review indicate that behavioral interventions conducted in schools are possibly superior to no intervention in reducing SSB intake, although the evidence is still relatively modest. In view of the importance of devising sound public health interventions and policies that aim to reduce SSB consumption and associated adverse health outcomes, the following guidelines are suggested for researchers and reviewers: (1) develop and include well-designed prospective cohort studies in addition to RCTs to increase the pool of studies that might report on continuous outcomes; (2) explore which theories and mediators of change can increase the effectiveness of interventions aimed at reducing SSB consumption and associated adverse health outcomes, including obesity; (3) determine whether single-strategy interventions (educational strategies alone) are more effective than combined-strategy interventions (with educational and environmental components) in reducing SSB consumption; (4) examine whether interventions that target multiple behaviors (eg, reduced SSB intake and increased water, fruit, and vegetable consumption) are more advantageous than single-component interventions in addressing the specific behavior of interest; and (5) utilize standardized evaluation schemes to assist researchers in improving their study protocols and minimizing risks of bias while supporting the task of reviewers and public health professionals in synthesizing the evidence to develop sound, scientifically valid recommendations.
Supplementary Material
Acknowledgments
The authors would like to acknowledge the assistance of the librarians, Ms Rita Kharrat from the University of Balamand and Ms Aida Farha from the American University of Beirut, in conducting the literature search for this review. Gratitude is also extended to Ms. Marwa Diab El Harake for her assistance in editing and reviewing references and the final revisions of the manuscript.
Author contributions. A.A.R., L.J., and P.A. had significant roles in the development of the review questions and the search strategy. A.A.R. and L.J. had the lead roles in designing and conducting the search strategy, screening for articles, extracting and entering data, and interpreting the analyses. A.A.R. and L.J. drafted the manuscript. L.A.K. assisted in the assessment of risk-of-bias of studies, conducted meta-analyses, and contributed to the writing of the manuscript. P.A. and C.P. analyzed the content of the interventions and contributed to the writing and review of the manuscript.
Funding/support. The review was funded by the Faculty of Health Sciences at the University of Balamand, Beirut, Lebanon, and the World Health Organization Collaborating Centre for Research on Oral Health in Deprived Communities, University of Liverpool, Liverpool, United Kingdom.
Declaration of interest. The authors have no relevant interests to declare.
Supporting Information
The following Supporting Information is available through the online version of this article at the publisher’s website:
Appendix S1 Completed PRISMA checklist
Appendix S2 Detailed search strategy
Appendix S3 Data extracted from excluded studies
Appendix S4 Risk of bias of included studies
References
- 1. Pereira MA. The possible role of sugar-sweetened beverages in obesity etiology: a review of the evidence. Int J Obes. 2006;30:S28–S36. [Google Scholar]
- 2. Malik VS, Popkin BM, Bray GA, et al. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. 2010;121:1356–1364.http://dx.doi.org/10.1161/CIRCULATIONAHA.109.876185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wang YC, Bleich SN, Gortmaker SL.. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988–2004. Pediatrics. 2008;121:e1604–e1614. [DOI] [PubMed] [Google Scholar]
- 4. Hu FB. Resolved: there is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes Rev. 2013;14:606–619.http://dx.doi.org/10.1111/obr.12040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ng SW, Mhurchu CN, Jebb SA, et al. Patterns and trends of beverage consumption among children and adults in Great Britain, 1986–2009. Br J Nutr. 2012;108:536–551.http://dx.doi.org/10.1017/S0007114511006465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Barquera S, Campirano F, Bonvecchio A, et al. Caloric beverage consumption patterns in Mexican children. Nutr J. 2010;9:47–57.http://dx.doi.org/10.1186/1475-2891-9-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brownell KD. Fast food and obesity in children. Pediatrics. 2004;113:132. doi:10.1542/peds.113.1.132 [DOI] [PubMed] [Google Scholar]
- 8. Rodríguez-Artalejo F, García EL, Gorgojo L, et al. Consumption of bakery products, sweetened soft drinks and yogurt among children aged 6–7 years: association with nutrient intake and overall diet quality. Br J Nutr. 2003;89:419–428. [DOI] [PubMed] [Google Scholar]
- 9. Libuda L, Kersting M.. Soft drinks and body weight development in childhood: is there a relationship? Curr Opin Clin Nutr Metab Care. 2009;12:596–600. [DOI] [PubMed] [Google Scholar]
- 10. Forshee RA, Storey ML.. Total beverage consumption and beverage choices among children and adolescents. Int J Food Sci Nutr. 2003;54:297–307.http://dx.doi.org/10.1080/09637480120092143 [DOI] [PubMed] [Google Scholar]
- 11. Mattes RD, Shikany JM, Kaiser KA, et al. Nutritively sweetened beverage consumption and body weight: a systematic review and meta-analysis of randomized experiments. Obes Rev. 2011;12:346–365.http://dx.doi.org/10.1111/j.1467-789X.2010.00755.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Malik VS, Pan A, Willett WC, et al. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr. 2013;98:1084–1102.http://dx.doi.org/10.3945/ajcn.113.058362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fung TT, Malik V, Rexrode KM, et al. Sweetened beverage consumption and risk of coronary heart disease in women. Am J Clin Nutr. 2009;89:1037–1042.http://dx.doi.org/10.3945/ajcn.2008.27140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Schulze MB, Liu S, Rimm EB, et al. Glycemic index, glycemic load, and dietary fiber intake and incidence of type 2 diabetes in younger and middle-aged women. Am J Clin Nutr. 2004;80:348–356. [DOI] [PubMed] [Google Scholar]
- 15. Sichieri R, Paula Trotte A, de Souza RA, et al. School randomised trial on prevention of excessive weight gain by discouraging students from drinking sodas. Public Health Nutr. 2009;12:197–202.http://dx.doi.org/10.1017/S1368980008002644 [DOI] [PubMed] [Google Scholar]
- 16. Cunha D, Souza B, Pereira R, et al. Preventing excessive weight gain by encouraging healthy eating habits among adolescents in Brazil: a randomised community trial. FASEB J. 2012;26(suppl 257.7) http://www.fasebj.org/content/26/1_Supplement/257.7. Accessed November 14, 2017. [Google Scholar]
- 17. James J, Thomas P, Cavan D, et al. Preventing childhood obesity by reducing consumption of carbonated drinks: cluster randomised controlled trial [published correction appears in BMJ. 2004;328:1237. doi:10.1136/bmj.38077.458438.EE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Haerens L, Bourdeaudhuij I, Maes L, et al. The effects of a middle-school healthy eating intervention on adolescents' fat and fruit intake and soft drinks consumption. Public Health Nutr. 2007;10:443–449. [DOI] [PubMed] [Google Scholar]
- 19. Bjelland M, Bergh IH, Grydeland MM, et al. Changes in adolescents' intake of sugar-sweetened beverages and sedentary behaviour: results at 8 month mid-way assessment of the HEIA study—a comprehensive, multi-component school-based randomized trial. Int J Behav Nutr Phys Act. 2011;8:63. doi:10.1186/1479-5868-8-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Albala C, Ebbeling CB, Cifuentes M, et al. Effects of replacing the habitual consumption of sugar-sweetened beverages with milk in Chilean children. Am J Clin Nutr. 2008;88:605–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chriqui JF, Pickel M, Story M.. Influence of school competitive food and beverage policies on obesity, consumption, and availability: a systematic review. JAMA Pediatr. 2014;168:279–286.http://dx.doi.org/10.1001/jamapediatrics.2013.4457 [DOI] [PubMed] [Google Scholar]
- 22. Levy TS, Del Carmen Morales-Ruan M, Castellanos CA, et al. School environment and its relationship with obesity in the state of Mexico. FASEB J. 2012;26(suppl 629.9) http://www.fasebj.org/content/26/1_Supplement/629.9.short. Accessed November 14, 2017. [Google Scholar]
- 23. Levy DT, Friend KB, Wang YC.. A review of the literature on policies directed at the youth consumption of sugar sweetened beverages. Adv Nutr. 2011;2:182S–200S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brownell KD, Frieden TR.. Ounces of prevention—the public policy case for taxes on sugared beverages. N Engl J Med. 2009;360:1805–1808. [DOI] [PubMed] [Google Scholar]
- 25. Pomeranz J. Advanced policy options to regulate sugar-sweetened beverages to support public health. J Public Health Policy. 2012;33:75–88.http://dx.doi.org/10.1057/jphp.2011.46 [DOI] [PubMed] [Google Scholar]
- 26. Avery A, Bostock L, McCullough F.. A systematic review investigating interventions that can help reduce consumption of sugar‐sweetened beverages in children leading to changes in body fatness. J Hum Nutr Diet. 2015;28:52–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vézina-Im L-A, Beaulieu D, Bélanger-Gravel A, et al. Efficacy of school-based interventions aimed at decreasing sugar-sweetened beverage consumption among adolescents: a systematic review. Public Health Nutr. 2017;20:2416–2431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Vargas-Garcia EJ, Evans CE, Cade JE.. Impact of interventions to reduce sugar-sweetened beverage intake in children and adults: a protocol for a systematic review and meta-analysis. Syst Rev. 2015;4:17. doi:10.1186%2Fs13643-015-0008-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Petticrew M, Roberts H.. Systematic Reviews in the Social Sciences: A Practical Guide. Malden, MA: Blackwell Publishing; 2006. [Google Scholar]
- 30. Akobeng A. Understanding randomised controlled trials. Arch Dis Child. 2005;90:840–844.http://dx.doi.org/10.1136/adc.2004.058222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bayer O, Kries R, Strauss A, et al. Short- and mid-term effects of a setting based prevention program to reduce obesity risk factors in children: a cluster-randomized trial. Clin Nutr. 2009;28:122–128.http://dx.doi.org/10.1016/j.clnu.2009.01.001 [DOI] [PubMed] [Google Scholar]
- 32. Bjelland M, Hausken SE, Bergh IH, et al. Changes in adolescents’ and parents’ intakes of sugar-sweetened beverages, fruit and vegetables after 20 months: results from the HEIA study—a comprehensive, multi-component school-based randomized trial. Food Nutr Res. 2015;59. doi:10.3402/fnr.v59.25932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Grydeland M, Bergh IH, Bjelland M, et al. Intervention effects on physical activity: the HEIA study— a cluster randomized controlled trial. Int J Behav Nutr Phys Act. 2013;10:17. doi:10.1186/1479-5868-10-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Cunha DB, de Souza BdS, Pereira RA, et al. Effectiveness of a randomized school-based intervention involving families and teachers to prevent excessive weight gain among adolescents in Brazil. PLoS One. 2013;8:e57498. doi:10.1371/journal.pone.0057498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ezendam NP, Brug J, Oenema A.. Evaluation of the Web-based computer-tailored FATaintPHAT intervention to promote energy balance among adolescents: results from a school cluster randomized trial. Arch Pediatr Adolesc Med. 2012;166:248–255.http://dx.doi.org/10.1001/archpediatrics.2011.204 [DOI] [PubMed] [Google Scholar]
- 36. James J, Thomas P, Kerr D.. Preventing childhood obesity: two year follow-up results from the Christchurch obesity prevention programme in schools (CHOPPS). BMJ. 2007;335:762. doi:10.1136/bmj.39342.571806.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Klesges RC, Obarzanek E, Kumanyika S, et al. The Memphis Girls' health Enrichment Multi-site Studies (GEMS): an evaluation of the efficacy of a 2-year obesity prevention program in African American girls. Arch Pediatr Adolesc Med. 2010;164:1007–1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kobel S, Wirt T, Schreiber A, et al. Intervention effects of a school-based health promotion programme on obesity related behavioural outcomes. J Obes. 2014;2014. doi:10.1155/2014/476230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Muckelbauer R, Libuda L, Clausen K, et al. Promotion and provision of drinking water in schools for overweight prevention: randomized, controlled cluster trial. Pediatrics. 2009;123:e661–e667. [DOI] [PubMed] [Google Scholar]
- 40. Rosário R, Araújo A, Oliveira B, et al. Impact of an intervention through teachers to prevent consumption of low nutrition, energy-dense foods and beverages: a randomized trial. Prev Med. 2013;57:20–25. [DOI] [PubMed] [Google Scholar]
- 41. Rosenkranz RR, Behrens TK, Dzewaltowski DA.. A group-randomized controlled trial for health promotion in Girl Scouts: healthier troops in a SNAP (Scouting Nutrition & Activity Program). BMC Public Health. 2010;10:81. doi:10.1186/1471-2458-10-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Siega-Riz AM, El Ghormli L, Mobley C, et al. The effects of the HEALTHY study intervention on middle school student dietary intakes. Int J Behav Nutr Phys Act. 2011;8:7. doi:10.1186/1479-5868-8-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Singh AS, Chin A Paw MJ, Brug J, et al. Dutch Obesity Intervention in Teenagers:, effectiveness of a school-based program on body composition and behavior. Arch Pediatr Adolesc Med. 2009;163:309–317.http://dx.doi.org/10.1001/archpediatrics.2009.2 [DOI] [PubMed] [Google Scholar]
- 44. van Grieken A, Veldhuis L, Renders CM, et al. Population-based childhood overweight prevention: outcomes of the ‘Be active, eat right’ study. PLoS One. 2013;8:e65376. doi:10.1371/journal.pone.0065376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. van Grieken A, Renders CM, Veldhuis L, et al. Promotion of a healthy lifestyle among 5-year-old overweight children: health behavior outcomes of the ‘Be active, eat right’ study. BMC Public Health. 2014;14:59. doi:10.1186/1471-2458-14-59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Higgins JP, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. Vol 4.Chicester, UK: John Wiley & Sons; 2011. [Google Scholar]
- 47. Landis JR, Koch GG.. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174.http://dx.doi.org/10.2307/2529310 [PubMed] [Google Scholar]
- 48. Must A, Anderson S.. Body mass index in children and adolescents: considerations for population-based applications. Int J Obes. 2006;30:590–594.http://dx.doi.org/10.1038/sj.ijo.0803300 [DOI] [PubMed] [Google Scholar]
- 49.Centers for Disease Control and Prevention, National Center for Health Statistics. Clinical growth charts. Centers for Disease Control and Prevention website. https://www.cdc.gov/growthcharts/clinical_charts.htm. Published 2007. Accessed January 30, 2017.
- 50. World Health Organization. Growth reference data for 5-19 years. World Health Organization website. http://www.who.int/growthref/en/. Published 2007. Accessed January 30, 2017.
- 51. Perez-Rodrigo C, Aranceta J.. Nutrition education in schools: experiences and challenges. Eur J Clin Nutr. 2003;57(suppl 1):S82–S85 [DOI] [PubMed] [Google Scholar]
- 52. Story M, Neumark-Sztainer D, French S.. Individual and environmental influences on adolescent eating behaviors. J Am Diet Assoc. 2002;102(3 suppl):S40–S51. [DOI] [PubMed] [Google Scholar]
- 53. Salvy SJ, de la Haye K, Bowker JC, et al. Influence of peers and friends on children's and adolescents' eating and activity behaviors. Physiol Behav. 2012;106:369–378.http://dx.doi.org/10.1016/j.physbeh.2012.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Paw M, Singh AS, Brug J, et al. Why did soft drink consumption decrease but screen time not? Mediating mechanisms in a school-based obesity prevention program. Int J Behav Nutr Phys Act. 2008;5:41. doi:10.1186/1479-5868-5-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Sharma M. Dietary education in school-based childhood obesity prevention programs. Adv Nutr. 2011;2:207S–216S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Bachman CM, Baranowski T, Nicklas TA.. Is there an association between sweetened beverages and adiposity? Nutr Rev. 2006;64:153–174. [DOI] [PubMed] [Google Scholar]
- 57. Kelishadi R, Soleiman FA.. Controlling childhood obesity: a systematic review on strategies and challenges. J Res Med Sci. 2014;19:993–1008. [PMC free article] [PubMed] [Google Scholar]
- 58. Nathan N, Wolfenden L, Williams C, et al. Adoption of obesity prevention policies and practices by Australian primary schools: 2006 to 2013. Health Educ Res. 2015;30:262–271.http://dx.doi.org/10.1093/her/cyu068 [DOI] [PubMed] [Google Scholar]
- 59. Story M, Kaphingst KM, Robinson-O'Brien R, et al. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health. 2008;29:253–272.http://dx.doi.org/10.1146/annurev.publhealth.29.020907.090926 [DOI] [PubMed] [Google Scholar]
- 60. Taber DR, Chriqui JF, Powell LM, et al. Banning all sugar-sweetened beverages in middle schools: reduction of in-school access and purchasing but not overall consumption. Arch Pediatr Adolesc Med. 2012;166:256–262.http://dx.doi.org/10.1001/archpediatrics.2011.200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Van den Berg SW, Mikolajczak J, Bemelmans WJ.. Changes in school environment, awareness and actions regarding overweight prevention among Dutch secondary schools between 2006–2007 and 2010–2011. BMC Public Health. 2013;13:672. doi:10.1186/1471-2458-13-672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Terry-McElrath YM, O'Malley PM, Johnston LD.. Factors affecting sugar-sweetened beverage availability in competitive venues of US secondary schools. J Sch Health. 2012;82:44–55. [DOI] [PubMed] [Google Scholar]
- 63. Malik VS, Willett WC, Hu FB.. Global obesity: trends, risk factors and policy implications. Nat Rev Endocrinol. 2013;9:13–27. [DOI] [PubMed] [Google Scholar]
- 64. Malik VS, Popkin BM, Bray GA, et al. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. 2010;121:1356–1364.http://dx.doi.org/10.1161/CIRCULATIONAHA.109.876185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Hu FB. Resolved: there is sufficient scientific evidence that decreasing sugar‐sweetened beverage consumption will reduce the prevalence of obesity and obesity‐related diseases. Obes Rev. 2013;14:606–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Dehghan M, Akhtar-Danesh N, Merchant AT.. Childhood obesity, prevalence and prevention. Nutr J. 2005;4:24. doi:10.1186/1475-2891-4-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Lin JS, Whitlock EP, Eckstrom E, et al. Challenges in synthesizing and interpreting the evidence from a systematic review of multifactorial interventions to prevent functional decline in older adults. J Am Geriatr Soc. 2012;60:2157–2166. [DOI] [PubMed] [Google Scholar]
- 68. McKenzie JE, Herbison GP, Deeks JJ.. Impact of analysing continuous outcomes using final values, change scores and analysis of covariance on the performance of meta‐analytic methods: a simulation study. Res Synth Methods. 2016;7:371–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Bown M, Sutton A.. Quality control in systematic reviews and meta-analyses. Eur J Vasc Endovasc Surg. 2010;40:669–677.http://dx.doi.org/10.1016/j.ejvs.2010.07.011 [DOI] [PubMed] [Google Scholar]
- 70. Valentine JC, Pigott TD, Rothstein HR.. How many studies do you need? A primer on statistical power for meta-analysis. J Educ Behav Stats. 2010;35:215–247.http://dx.doi.org/10.3102/1076998609346961 [Google Scholar]
- 71. Riley RD, Higgins JP, Deeks JJ.. Interpretation of random effects meta-analyses. BMJ. 2011;342:d549. doi:10.1136/bmj.d549 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.