Abstract
Study Objectives:
Hospital readmissions are an important metric of quality and safety. This study seeks to characterize the relationship between readmissions and obstructive sleep apnea (OSA). A better understanding of this relationship could be utilized to develop preventative measures and reduce readmission rates.
Methods:
A retrospective review of patients discharged over a 24-month period to a Department of Defense hospital was conducted. Medical records review provided demographic data, presence of OSA and comorbid diseases, and whether readmission occurred within 30 days of discharge. Statistical analysis assessed risk factors for readmission, and multivariate analysis was performed. Next, 125 readmitted patients with OSA were randomly selected for detailed chart review and compared to a matched cohort that was not readmitted.
Results:
Of 22,261 unique patients discharged, 1,899 (8.5%) were readmitted. Patients with OSA had a readmission rate of 11.4% versus 7.6% for patients without OSA (P < .00001). Multivariable analysis revealed an odds ratio of 1.46 for readmission in patients with OSA (P < .0001). For the detailed chart review of 250 patients, length of hospital stay differed for the readmitted and non-readmitted groups (5.1 versus 3.6 days; P = .007). Apnea-hypopnea index (24.1 versus 27.2 events/h; P = .48) was similar between the groups. Also, inpatient (27.2% versus 26.4%) and outpatient (38.4% versus 37.6%) positive airway pressure (PAP) treatment rates were not different.
Conclusions:
This study found OSA to be an independent risk factor for readmission within 30 days of discharge. PAP therapy appears to be underutilized in patients with known OSA. Additional studies are needed to define the relationship between OSA, PAP adherence, and hospital readmission.
Citation:
Scalzitti NJ, O'Connor PD, Nielsen SW, Aden JK, Brock MS, Taylor DM, Mysliwiec V, Dion GR. Obstructive sleep apnea is an independent risk factor for hospital readmission. J Clin Sleep Med. 2018;14(5):753–758.
Keywords: hospital readmission, obstructive sleep apnea, positive airway pressure
BRIEF SUMMARY
Current Knowledge/Study Rationale: Obstructive sleep apnea is commonly associated with comorbidities that are known to affect hospital readmission rates. Our study sought to explore whether obstructive sleep apnea itself is a modifiable risk factor for hospital readmission.
Study Impact: This study identifies obstructive sleep apnea as an independent risk factor for hospital readmission. There appears to be inadequate use of positive airway pressure both during hospitalization and after discharge in patients with obstructive sleep apnea.
INTRODUCTION
Improving the quality and effectiveness of medical care is an ongoing challenge for health care organizations. Therefore, hospital readmissions within 30 days of discharge are an important quality metric reported to the Centers for Medicare and Medicaid Services. Because 1 in 5 Medicare patients is read-mitted within 30 days of discharge, determining risk factors that lead to hospital readmission is an important step to improving patient outcomes and reducing readmission.1 Chronic medical conditions such as heart failure, chronic obstructive pulmonary disease, and diabetes are associated with increased hospital readmission risk.2 As a result, efforts to reduce hospital readmission have focused on improving outcomes for these illnesses.
Obstructive sleep apnea (OSA) is a condition of recurring collapse of the upper airway during sleep. Its incidence appears to be increasing in adults in the United States, possibly due to growing awareness and rising obesity rates.3–6 Up to 20% to 25% of middle-aged adults have OSA, with male sex, increasing age, and obesity being the most common risk factors.3–6 Additionally, OSA is associated with, and an independent risk factor for, several important health conditions including pulmonary and systemic hypertension, coronary artery disease, stroke, atrial fibrillation, and diabetes, as well as mortality.5,6 OSA also may result in hypoxia and increased sympathetic activity, which can promote arrhythmias and contribute to heart failure. These untoward associations and downstream effects make it possible that OSA itself could be associated with read-mission to the hospital.
Positive airway pressure (PAP) therapy effectively treats excessive somnolence related to OSA, which can improve quality of life for these patients.7 In addition, physiologic factors such as hypoxia, hypercarbia, and catecholamine surges are ameliorated, which can have disease-specific implications.8–11 However, these benefits of therapy have only been consistently shown to occur when patients meet a minimum standard of adherence (usually defined as ≥ 70% of nights using therapy ≥ 4 h/night). Despite known health benefits associated with PAP adherence, studies report that long-term adherence to that degree remains approximately 50% to 60%.5,6 Treatment of OSA may be particularly important for people who are hospitalized for other conditions. For instance, postsurgical patients with OSA are at increased risk of complications after surgery, and the perioperative use of PAP is recommended by the American Society of Anesthesiologists in these patients to minimize that risk.12 Because OSA can adversely affect heart failure, hyper-tension, and arrhythmias, untreated OSA can hinder effective treatment of cardiovascular patients in the hospital. Furthermore, treatment of OSA is associated with reduced rate of hospital readmission in cardiac patients with adequate adherence to PAP compared to nonusers or partial users.13
This study aimed to assess the relationship between OSA and hospital readmission. We hypothesized that OSA is an independent risk factor for hospital readmission within 30 days of discharge. We also aimed to characterize the relationship between OSA severity and its treatment with PAP to hospital readmission, including the rate of PAP use in patients with OSA during hospitalization. A better understanding of the relationship between the presence of OSA and use of inpatient PAP therapy could lead to the development of preventive measures to reduce hospital readmission.
METHODS
The study was approved by the Institutional Review Board at our hospital prior to evaluation of individual patient charts. A retrospective chart review was conducted through the electronic medical record (EMR) system including all hospital discharges over a 24-month period (August 2011–July 2013) at the largest Department of Defense hospital. As some patients had multiple discharges during this time frame, each patient was considered independently by including only their first discharge, and additional discharges on the same patient were excluded. Other recorded data included basic demographics (age and sex), length of stay, body mass index (BMI) and any diagnosis code listed during the hospital stay for OSA, chest pain, angina, gastroesophageal reflux disease (GERD), postoperative infection, chronic obstructive pulmonary disease (COPD), asthma, pneumonia, influenza, atrial fibrillation, congestive heart failure (CHF), acute myocardial infarction, acute coronary syndrome (ACS), and syncope. International Classification of Diseases (ICD-9) codes used to capture OSA diagnoses were “Obstructive Sleep Apnea” (327.23) and “Sleep Apnea, Unspecified” (780.57). Any patient readmitted to the hospital within 30 days was noted in the dataset. In patients with multiple discharges, only the first discharge was included in the analysis for readmission. Patients admitted for pregnancy, chemotherapy regimens, or other routine monitoring protocols requiring readmission within 30 days were excluded from the analysis. The resulting database of discharged individuals was linked to the outpatient EMR system for collection of additional data. Chi-square analysis was performed to determine which factors were significantly related to hospital readmission, and logistic regression analysis was performed to calculate odds ratios for readmission. Previously mentioned comorbid conditions were each assessed for their effect on re-admission. Factors identified as not significant were removed from the analysis, and this model was applied to assess factors significant for hospital readmission in a multivariable analysis.
To explore the relationship between OSA severity and its treatment with hospital readmission, a case-control study was performed. A random number generator was utilized to select 125 of the possible 603 patients discharged with OSA who went on to readmission. Then, age- and sex-matched patients were identified from the group of patients with OSA who were not readmitted. From these, 125 matched patients were selected by a random number generator. A comprehensive chart review was undertaken for each of the 250 patients to identify if there was a polysomnography (PSG) documented in the EMR. PSG data recorded included apnea-hypopnea index (AHI), respiratory disturbance index (RDI), OSA severity (mild: AHI 5–15 events/h, moderate: AHI 15–30 events/h, severe: AHI > 30 events/h), and lowest oxygen saturation. BMI data were collected for covariate analysis of obesity with OSA. If a patient was ordered a PAP device, then adherence data were collected from the EMR, to include either downloaded adherence report from the PAP machine or physician documentation of patient-reported regular use. Inpatient medical records including nursing and/or respiratory therapy notes were reviewed to determine rates of inpatient PAP therapy for OSA as well as to assess length of hospital stay. A chi-square test was used to compare categorical variables, and a t test was used for continuous variables. All statistics for this project were completed using SPSS Version 19 (IBM, Armonk, New York).
RESULTS
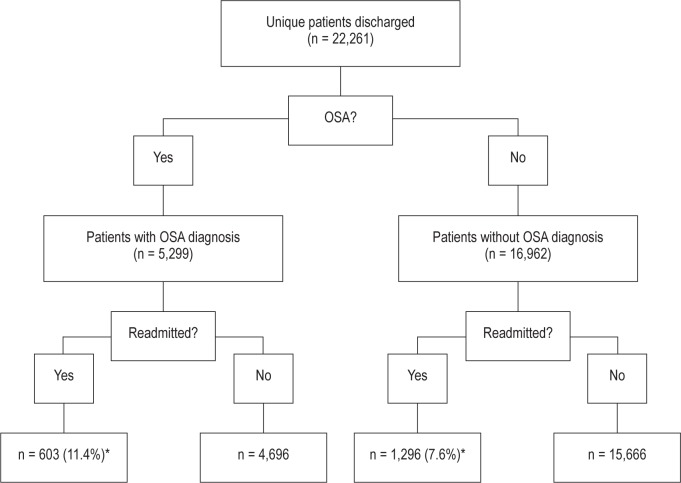
During the study period there were 22,261 unique adult patients discharged from our tertiary care hospital between August 1, 2011 and July 31, 2013. Of these, 5,299 patients (23.8%) had a diagnosis of OSA according to a search for ICD-9 codes of the outpatient record at the time of admission. Readmission within 30 days of discharge occurred for 1,899 patients (8.5%). Readmitted patients had a higher rate of having OSA compared to those not readmitted (31.8% versus 23.1%; P < .00001). In conjunction, the readmission rate for patients with OSA was 11.4% (603 of 5,299), and the rate for patients without OSA was 7.6% (1,296 of 16,962), which was significantly different (P < .00001). Figure 1 depicts the entire cohort of patients with respect to OSA status and readmission.
Figure 1. Patient flowchart.
Flowchart depicting all unique patients discharged over the 2-year time period in regard to OSA status and readmission status. * = P < .00001. OSA = obstructive sleep apnea.
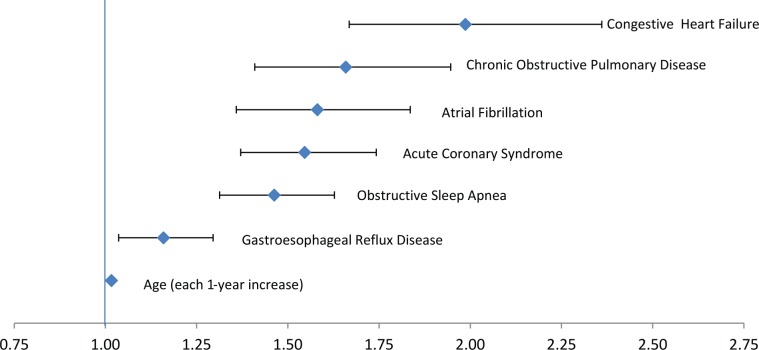
Logistic regression multivariable modeling revealed OSA was independently correlated with hospital readmission. When controlling for significant comorbid conditions (age, COPD, CHF, ACS, GERD, and atrial fibrillation), there was a significant increase in the odds of readmission (odds ratio 1.46; 95% confidence interval 1.31–1.63; P < .0001) for patients with OSA. For this logistic regression model, the area under the curve was 0.7308. Table 1 displays the odds ratio for read-mission for each variable that was found to be independently significant, whereas Figure 2 is a forest plot representation of these factors that were predictive of readmission.
Table 1.
Odds ratios for readmission on multivariate logistic regression analysis.
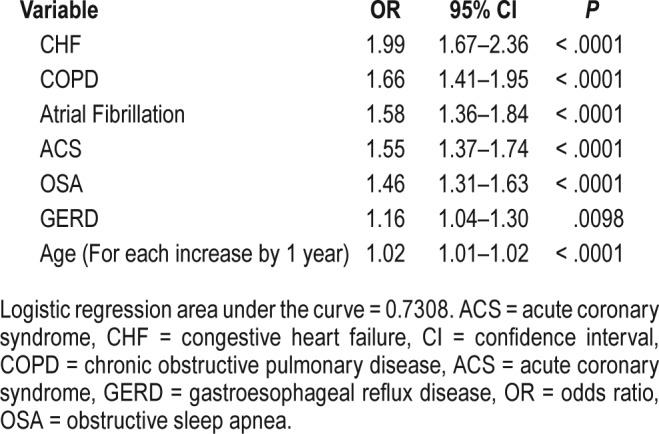
Figure 2. Forest plot of predictors of readmission.
This figure depicts the factors significant for readmission on multivariable analysis. The x axis represents odds ratios.
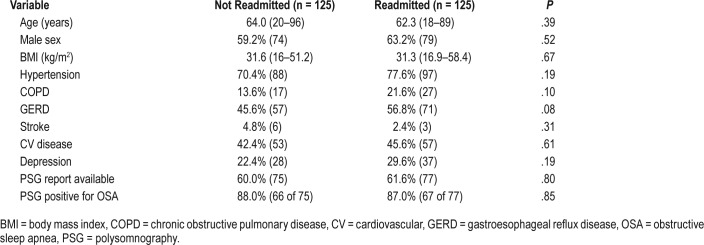
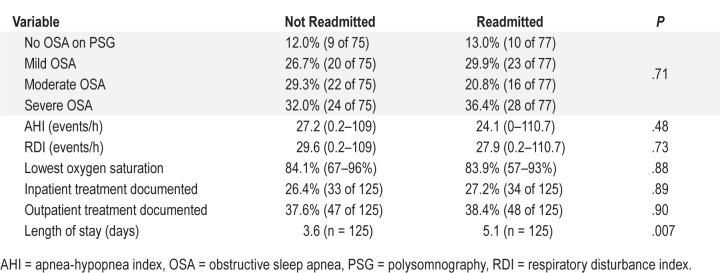
In the case-control part of the study, a group of patients with an ICD-9 diagnosis code for OSA were randomly selected for a detailed review to determine if OSA severity or adherence with PAP therapy were associated with readmission. For the 250 patients, ages ranged from 18 to 96 years (mean 63.2 years). PSG data were available for 152 patients (77 readmitted and 75 non-readmitted). Based on these PSG reports, only 67 readmitted and 66 non-readmitted patients met criteria for a diagnosis of OSA. In the patients with a PSG report that did not support a diagnosis of OSA (AHI < 5 events/h), the diagnosis of OSA may have been assigned incorrectly or assigned prior to obtaining the PSG. Table 2 demonstrates demographic and comorbidity data, as well as which patients had PSG data available. For those with PSG data, the rates of not meeting criteria for OSA (13% versus 12%), having mild (29.9% versus 26.7%), moderate (20.8% versus 29.3%), and severe OSA (36.4% versus 32%) were similar between the readmitted and nonreadmitted groups. Also, measures of OSA severity on PSG were not clinically or statistically different between the groups (Table 3). The AHI ranged from zero to 110.7 events/h (mean 24.1) and 0.2 to 109 events/h (mean 27.2) for the readmitted and non-readmitted groups, respectively (P = .48). Similarly, RDI averaging 29.6 events/h and 27.9 events/h (P = .73), lowest oxygen saturations averaging 83.9% and 84.1% (P = .88), and BMI averaging 31.3 and 31.6 (P = .67) were not different. These results held true even when excluding those patients with a PSG that was not diagnostic of OSA.
Table 2.
Patient demographics, comorbidities, and availability of polysomnography data for randomly selected group of patients with OSA diagnosis by ICD-9 code.
Table 3.
Polysomnography, treatment, and length of stay data.
Regarding OSA treatment with PAP, there were also no significant differences between the groups (Table 3). Inpatient treatment during the initial admission was documented (in nursing and/or respiratory therapy notes or treatments) in 34 of the patients (27.2%) who were readmitted and 33 (26.4%) of those who were not (P = .89). A similar rate of documented outpatient use of PAP therapy was found between the readmitted (n = 48, 38.4%) and non-readmitted (n = 47, 37.6%) groups (P = .90). Very few patients had PAP downloads present in the medical record; only 3 patients in the readmitted group and 2 in the non-readmitted group were identified as meeting the minimum standard of PAP adherence (≥ 70% of nights using therapy ≥ 4 h/night). This low number precluded statistical analysis. All other outpatient adherence was determined based on physician documentation of regular use as reported by the patient. Of the identified characteristics, only length of stay during initial hospitalization (5.1 versus 3.6 days), in the read-mitted and non-readmitted OSA groups respectively, differed (P = .007).
DISCUSSION
As the prevalence of OSA continues to rise, its effect on a patient's general health and associated disease outcomes is gaining increased recognition. Beyond the detriment in sleep quality that results, evidence has mounted regarding the role of OSA in exacerbating and perpetuating hypertension, atrial fibrillation, coronary artery disease, chronic obstructive pulmonary disease, insulin resistance, and cerebrovascular disease.5,6 Many of these comorbid diseases have been implicated in elevated readmission rates following hospital discharge. The findings of this study support the hypothesis that OSA is an independent risk factor for hospital readmission in the 30 days following discharge. On review of more than 22,000 unique patients discharged, patients with OSA had a significantly higher rate of readmission than patients without OSA. Similarly, readmitted patients were more likely to have a diagnosis of OSA than those not readmitted, even when controlling for confounding variables using logistic regression modeling. Our findings provide initial evidence that OSA should be specifically addressed as an illness that contributes to hospital readmission.
Despite increasing awareness of OSA and the potential benefits of PAP therapy among health care providers, the long-term adherence to home PAP therapy remains approximately 50% to 60%.5,6,14 Surprisingly, use of PAP therapy for hospitalized patients is worse, ranging from 5% in a National Hospital Discharge Survey to 26% at a single tertiary medical center.15,16 In our study, inpatient PAP therapy was similarly low, with documentation of use in only 26.4% of the non-re-admitted group and 27.2% of the readmitted group. Unfortunately, inpatient treatment of OSA is frequently overlooked. At first glance, it would seem that a hospital admission would be an ideal time to enforce OSA treatment because providers have more control over patients' treatments for this period of time; however, the acute nature of their admission may overshadow the presence of OSA. Given the low in-hospital utilization, it is not unexpected that usage did not differ between the readmitted and non-readmitted groups. Correspondingly in our cohort, documentation of home PAP therapy was low, with only approximately 38% of the patients in each group (48 in readmitted and 47 in non-readmitted) having recorded usage of outpatient PAP therapy. Far fewer patients met criteria for the minimum standard of PAP adherence defined as ≥ 70% of nights using therapy for ≥ 4 h/night. A previous study demonstrated that adequate PAP adherence is associated with decreased readmission in cardiac patients.13 It is possible that similar findings would be present in all patients with adequately treated OSA following hospital discharge.
Although the presence of OSA was associated with a higher rate of hospital readmission, our data in the case-control portion of the study did not identify a link between OSA severity and readmission. In a detailed review of 250 patients with OSA, no differences were found between the readmitted and non-readmitted patient groups with respect to OSA severity as measured by the AHI, RDI, or lowest oxygen saturation. This was an unexpected result, although it is possible that the readmitted and non-readmitted groups were not found to have differences in OSA severity because the groups were matched for age and sex. Also, we did not find evidence to support the idea that treatment of OSA would mitigate the increased risk of hospital readmission, noting that the documented rate of PAP adherence was low in both the inpatient and outpatient setting in our study. One key difference between this study and a recent study of cardiac patients that demonstrated a reduced readmission rate with OSA treatment was that in that study, only the cohort of patients that achieved adequate adherence (≥ 70% of nights using therapy ≥ 4 h/night) with PAP had a significant reduction in readmission, whereas readmission in partial users and nonusers of PAP remained similar.13 Unfortunately, our retrospective study design did not provide a large-enough cohort of patients who were adequately adherent with treatment for meaningful statistical analysis. Further investigation into this topic is warranted to ascertain whether OSA is a modifiable risk factor for readmission. There appears to be a significant need to improve recognition and documentation of adherence with PAP therapy in patients with a known diagnosis of OSA in both the inpatient and outpatient settings.
Although analysis of the randomly selected 250 patients with OSA did not reveal OSA-related factors that were associated with higher risk of readmission, length of hospital stay was significantly different between the readmitted and non-re-admitted groups. Although an interesting and significant finding, it does not relate specifically to OSA diagnosis, which was the main objective of this study, and it could be a confounding variable. Alternatively, the low rate of inpatient OSA treatment in our study may have contributed to longer admission.
The retrospective nature of this study does present limitations. First, patients were identified as having OSA based on a query of their records for ICD-9 codes. An inherent risk of performing a large review of previously coded diagnoses is that patients may be classified into incorrect groups if a diagnosis is omitted or coded inaccurately. Based on our study design, we were reliant on these assigned codes to classify patients as having or not having OSA. Also, we were only able to locate the PSG data for 62% and 60% of the readmitted and non-readmitted patients, respectively, in the case-control portion of the study. This is likely related to the fact that in our military health care system, many PSGs are outsourced to the civilian sector, and these reports may not always get uploaded into the military EMR. Of the 250 patients studied, 10 (8%) in the readmitted and 9 (7.2%) in the non-readmitted groups actually did not have OSA (based on AHI or RDI < 5 events/h). The inability to locate PSG data on review of the EMR suggests that documentation of OSA is not necessarily accurate or that providers may suspect that OSA can be a clinical diagnosis and not require objective testing. Furthermore, only 250 of the more than 22,000 total unique discharged patients were randomly selected for the detailed review of the record. This small segment of the overall cohort may not represent the group as a whole. Also, the overall poor adherence rate that we found could have significantly limited the results. It is possible that a cohort with an adequate level of adherence could have decreased readmission rates. However, the nature of this study did not facilitate that comparison.
Early readmission to the hospital represents one measure of health care quality and patient safety that health care organizations are striving to improve. This study identified OSA as an independent risk factor for readmission within 30 days in a large sample of patients. A detailed review of a subset of patients with OSA did not identify predictive factors for which patients with OSA are more likely to be readmitted. Further investigation is needed to better define the relationship between OSA, its treatment, and hospital readmission.
DISCLOSURE STATEMENT
All authors verify that they have seen and approve the final version of the manuscript. The authors report no conflicts of interest. Disclaimer: The views expressed herein are those of the author(s) and do not reflect the official policy or position of the San Antonio Military Medical Center, the United States Army Medical Department, the United States Army Office of the Surgeon General, the Department of the Army, Department of the Air Force, Department of Defense, or the United States Government.
ABBREVIATIONS
- ACS
acute coronary syndrome
- AHI
apnea-hypopnea index
- BMI
body mass index
- CHF
congestive heart failure
- COPD
chronic obstructive pulmonary disease
- EMR
electronic medical record
- GERD
gastroesophageal reflux disease
- ICD
International Classification of Diseases
- OSA
obstructive sleep apnea
- PAP
positive airway pressure
- PSG
polysomnography
- RDI
respiratory disturbance index
REFERENCES
- 1.Steiner C. New AHRQ Database Tracks Hospital Readmission Rates. Agency for Healthcare Research and Quality website. [Accessed June 26, 2017]. https://www.ahrq.gov/news/blog/ahrqviews/112015.html. Published November 20, 2015.
- 2.Jencks S, Williams M, Coleman E. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 3.Young T, Palta M, Dempsey J, et al. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 4.Peppard P, Young T, Barnet J, et al. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–1014. doi: 10.1093/aje/kws342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bue A, Salvaggio A, Isodoro S, et al. Usefulness of reinforcing interventions on continuous positive airway pressure compliance. BMC Pulm Med. 2014;14:78. doi: 10.1186/1471-2466-14-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kamel G, Munzer K, Espiritu J. Use of CPAP in patients with obstructive sleep apnea admitted to the general ward: effect on length of stay and readmission rate. Sleep Breath. 2016;20(3):1103–1110. doi: 10.1007/s11325-016-1328-x. [DOI] [PubMed] [Google Scholar]
- 7.Patel S, White D, Malhotra A, Stanchina M, Ayas N. Continuous positive airway pressure therapy for treating sleepiness in a diverse population with obstructive sleep apnea: results of a meta-analysis. Arch Intern Med. 2003;163(5):565–571. doi: 10.1001/archinte.163.5.565. [DOI] [PubMed] [Google Scholar]
- 8.Montesi S, Edwards B, Malhotra A, Bakker J. The effect of continuous positive airway pressure treatment on blood pressure: a systematic review and meta-analysis of randomized controlled trials. J Clin Sleep Med. 2012;8(5):587–596. doi: 10.5664/jcsm.2170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fava C, Dorigoni S, Dalle Vedove F, et al. Effect of CPAP on blood pressure in patients with OSA/hypopnea a systematic review and meta-analysis. Chest. 2014;145(4):762–771. doi: 10.1378/chest.13-1115. [DOI] [PubMed] [Google Scholar]
- 10.Haentjens P, Van Meerhaeghe A, Moscariello A, et al. The impact of continuous positive airway pressure on blood pressure in patients with obstructive sleep apnea syndrome: evidence from a meta-analysis of placebo-controlled randomized trials. Arch Intern Med. 2007;167(8):757–764. doi: 10.1001/archinte.167.8.757. [DOI] [PubMed] [Google Scholar]
- 11.Marin J, Carrizo S, Vicente E, Agusti A. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365(9464):1046–1053. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 12.American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Obstructive Sleep Apnea. Practice guidelines for the perioperative management of patients with obstructive sleep apnea: an updated reported by the American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Obstructive Sleep Apnea. Anesthesiology. 2014;120(2):268–286. doi: 10.1097/ALN.0000000000000053. [DOI] [PubMed] [Google Scholar]
- 13.Kauta S, Keenan B, Goldberg L, Schwab R. Diagnosis and treatment of sleep disordered breathing in hospitalized cardiac patients: a reduction in 30-day hospital readmission rates. J Clin Sleep Med. 2014;10(10):1051–1059. doi: 10.5664/jcsm.4096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hussain S, Irfan M, Waheed Z, et al. Compliance with continuous positive airway pressure (CPAP) therapy for obstructive sleep apnea among privately paying patients- a cross sectional study. BMC Pulm Med. 2014;14:88. doi: 10.1186/1471-2466-14-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spurr K, Graven M, Gilbert R. Prevalence of unspecified sleep apnea and the use of continuous positive airway pressure in hospitalized patients, 2004 National Hospital Discharge Survey. Sleep Breath. 2008;12(3):229–234. doi: 10.1007/s11325-007-0166-2. [DOI] [PubMed] [Google Scholar]
- 16.Sorscher A, Caruso E. Frequency of provision of CPAP in the inpatient setting: an observational study: “CPAP provision in the inpatient setting”. Sleep Breath. 2012;16(4):1147–1150. doi: 10.1007/s11325-011-0621-y. [DOI] [PubMed] [Google Scholar]