Abstract
Study Objectives:
According to the diathesis-stress model of insomnia, insomnia may develop in vulnerable individuals in response to stress. Resilience is a psychobiological factor that determines an individual's capacity to adapt successfully to stressful events and low resilience increases vulnerability for development of mental disorders. The aim was to explore resilience in subjects with insomnia and its relationship with the factors that contribute to its development and perpetuation.
Methods:
The study consisted of 58 subjects with Insomnia Disorder according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition and 38 good sleepers. Resilience Scale for Adults (RSA), Ford Insomnia Response to Stress Test (FIRST), Pre-sleep Arousal Scale (PSAS), and Difficulties in Emotion Regulation Scale (DERS) were administered while taking into account psychiatric symptoms. Differences in means between groups were assessed using t test or Mann-Whitney U/Wilcoxon test. Linear/multivariable regression analyses and mediation analyses were performed.
Results:
Subjects with insomnia (24 females, mean age 49 ± 2.1 years) had lower RSA and higher FIRST, DERS, and PSAS scores than good sleepers (22 females, mean age 47.2 ± 1.2 years). After controlling for anxiety/depressive symptoms, low resilience correlated with high stress-related sleep reactivity (P = .004), pre-sleep cognitive hyperarousal (P = .01) and emotion dysregulation (P = .01). Emotion dysregulation mediated the relationship between low resilience and cognitive hyperarousal (Z = 2.06, P = .03).
Conclusions:
Subjects with insomnia showed low resilience, which was related to high stress-related sleep reactivity, emotional dysregulation, and hyperarousal. If resilience helps to minimize the extent of pathogenesis in the developmental process, an early identification of vulnerable candidates should be useful for preventing insomnia development and maintenance.
Commentary:
A commentary on this article appears in this issue on page 709.
Citation:
Palagini L, Moretto U, Novi M, Masci I, Caruso D, Drake CL, Riemann D. Lack of resilience is related to stress-related sleep reactivity, hyperarousal, and emotion dysregulation in insomnia disorder. J Clin Sleep Med. 2018;14(5):759–766.
Keywords: chronic insomnia, emotion dysregulation, pre-sleep arousal, resilience, stress-related sleep activity
BRIEF SUMMARY
Current Knowledge/Study Rationale: According to the diathesis-stress model of insomnia, subjects with insomnia present with a high stress-related sleep reactivity. Resilience is a psychobiological factor that determines an individual's capacity to adapt successfully to stressful events and lower resilience increases vulnerability for the development of mental disorders. The aim was to explore resilience, for the first time in subjects with insomnia, in order to better understand the stress-risk-vulnerability dimension of insomnia.
Study Impact: The study has shown that subjects with insomnia possess low resilience, which was related to high stress-related sleep reactivity, arousal, and emotional dysregulation. This may be helpful in clinical practice for early identification of vulnerable candidates and, by enhancing resilience, for minimizing the extent of insomnia.
INTRODUCTION
Insomnia is one of the most frequent sleep disorders1,2 affecting approximately one-third of the adult population and it is a prevalent health problem. It is an independent risk factor for work disability and reduced work performance and it is associated with high direct and indirect costs for the healthcare system and society.3–5 In the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)2 it has been listed as a distinct condition (insomnia disorder) and there is strong evidence for its relation to a broad range of comorbid conditions including mental and physical illness.6–12 The study of the mechanisms involved in the development and maintenance of insomnia is critical to identify treatment and prevention strategies to improve insomnia and its associated morbidity.
According to one of the most influential models of insomnia, the 3P model,13 the interaction of predisposing, precipitating, and perpetuating factors is proposed to play an important role in its initiation and maintenance. Predisposing factors are present before insomnia is manifested and are hypothesized to interact with precipitating factors, increasing the risk of insomnia in vulnerable individuals. Stressful life events are a common precipitating factor of insomnia13,14: life stressors are associated with the development of new-onset insomnia and individuals with insomnia show elevated cognitive and physiological hyperarousal responses to stressors.15,16 Physiological hyperarousal, which has been identified as a key factor in insomnia, is present over 24 hours15–17 and may interact with cognitive and emotional responses to perpetuate insomnia.18–21
Hyperarousal has been shown to be a characteristic of individuals with elevated stress-related sleep reactivity, which is defined as the degree of sleep disruption in response to stressful events; sleep reactivity has been shown to predispose to the development and maintenance of insomnia disorder.14,22–25
Recently, there has been a paradigm shift in the understanding of the stress-risk-vulnerability dimension in clinical psychology that identified the capacity and dynamic process of adaptively overcoming stress while maintaining normal psychological and physical functioning labeled as resilience.26–29 Resilience is defined as a broad systems construct often referred to as a trait that develops from an individual's experience with stress and a psychobiological factor that determines an individual's capacity to adapt successfully to stressful events.30,31 In contrast, low resilience is related to a dysregulation in stress response and the development of emotional dysregulation and persistent psycho-pathology.31–34 Although the understanding of resilience remains limited, recent investigations have identified mechanisms encompassing genetic, epigenetic, developmental, psychological and neurochemical factors that underlie the development and enhancement of resilience and factors that predict vulnerability to stress and susceptibility to psychiatric disorders in the absence of adequate resilience (for an overview see Wu et al.33).
Notably, the potential to enhance stress resilience in at-risk populations has been hypothesized to prevent the onset of stress-induced psychopathology.31,33
On this basis, we aimed to study resilience in the context of adult insomnia as a trait factor, which may be useful to understand the stress-risk-vulnerability dimension of insomnia. We hypothesized that low resilience in subjects with insomnia may contribute to its development. In addition, we hypothesized that by interacting with predisposing and perpetuating factors of insomnia, such as stress-related sleep reactivity, as well as emotional and arousal dysregulation, low resilience may contribute to insomnia predisposition and perpetuation. If the enhancement of stress resilience in at-risk populations could prevent the onset of stress-induced psychopathology, it should include insomnia.
Hence, the primary objective of this study was to evaluate resilience of subjects with insomnia. The secondary objective was to evaluate the possible association between resilience, sleep reactivity, and arousal/emotional factors that may contribute to insomnia development and perpetuation.
To address these aims, we evaluated resilience, sleep reactivity, pre-sleep state arousal, and emotion regulation, while taking into account insomnia severity, anxiety, and depressive symptoms in a sample of subjects with insomnia disorder compared to a sample of good sleepers.
METHODS
Selection of Subjects and Distribution of Psychometric Questionnaire
Between December 2015 and April 2017, consecutive out-patients visiting the Sleep Center of the Psychiatry Unit II, University of Pisa, Italy, who met the diagnostic criteria for insomnia disorders according to according to the DSM-52 were recruited for the purposes of this study, together with a group of healthy subjects who were matched for sex, age, socioeconomic status, and educational level with the insomnia group.
The subjects of both groups underwent a face-to-face evaluation conducted by a psychiatrist (LP). Their sleep disorders were assessed by means of clinical evaluation and sleep questionnaires. The evaluation also assessed insomnia severity (Insomnia Severity Index [ISI]),35 resilience (Resilience Scale for Adults [RSA]),32 stress-related sleep reactivity (Ford Insomnia Response to Stress Test [FIRST]),22 pre-sleep arousal (Pre-sleep Arousal Scale [PSAS]),36 emotion regulation (Difficulties in Emotion Regulation Scale [DERS]),37 anxiety (Self-rating Anxiety Scale [SAS]),38 and depressive symptoms (Beck Depression Inventory [BDI]).39 The inclusion criteria for subjects with insomnia disorder were (1) difficulty in initiating and/or maintaining sleep and/or early morning awakening (sleep onset latency and/or wake after sleep onset > 30 minutes), (2) for at least 3 months, (3) sleep disturbance that causes clinically significant distress or impairment in important areas of functioning, (4) no sleep-disruptive medical/mental conditions, substance abuse, and/or other sleep disorders. Only individuals who reported sleep difficulties for at least 3 nights per week were enrolled in the study.
The exclusion criteria for subjects with insomnia disorder were: current use of hypnotic or sleep-altering medications, cognitive impairment (Mini Mental State Evaluation; for the Italian version see Measso et al.40), past or current diagnosis of psychiatric disorders, or other sleep disorders (ie, obstructive sleep apnea syndrome, restless legs syndrome, etc.), which were evaluated with the use of medical records and the Sleep-50 Questionnaire41,42 a self-reported questionnaire used to assess sleep disorders.
Good sleepers were recruited from the hospital and from among university personnel. Participants underwent a face-to-face assessment and completed the same set of questionnaires used for the subjects with insomnia. The inclusion criteria of the good sleepers were (1) less than 30 minutes of sleep onset latency and (2) less than 30 minutes of wake time after sleep onset in usual nocturnal sleep.43 The exclusion criteria were the following: (1) past or current diagnosis of cognitive impairment (Mini Mental State Evaluation),40 sleep disorders (ISI)35 (Sleep-50 Questionnaire)41,42 or mental diseases; (2) habitual use of hypnotics or alcohol at bedtime; (3) subjects engaged in shift work; and (4) failure to complete the questionnaires. The study was in conformance with the Declaration of Helsinki and all participants provided written informed consent prior to being enrolled in the study.
Sleep Scales
Insomnia severity was evaluated with the ISI.35 The ISI is a 7-item self-report questionnaire with a 2-week recall period. The sum yields a global score ranging from zero to 28. For the purposes of this study, according to the ISI authors' recommendations, an ISI score of 8 or higher indicated insomnia symptoms. The ISI has been validated in a previous Italian sample.44
Sleep reactivity was evaluated with the FIRST.22 The FIRST is a self-administered questionnaire that provides an indicator of an individual's overall level of “sleep reactivity” or the degree to which he/she is vulnerable to sleep disturbance when exposed to stress. The questionnaire includes items relevant to situational sleep-disturbing stimuli (eg, “When you experience the following situations, how likely is it for you to have difficulty sleeping?”; “After a stressful experience during the day?”; “After an argument?”) with a 4-point Likert scale (1 = not likely; 4 = very likely). The sum yields a global FIRST score ranging from 9 to 36. A higher score indicates a higher level of sleep reactivity to the stimuli and, according to the authors' recommendations, abnormally high sleep reactivity is considered when the FIRST sum score is higher than 19. For the Italian version see the study by Palagini and Manni.42
Arousal Scales
Pre-sleep state arousal was evaluated with the PSAS.36 It is a 16-item self-reported questionnaire comprising both cognitive and somatic manifestations of arousal, with 8 items in each subscale. When responding to the PSAS, subjects were asked to describe how intensely they generally experienced each component as they attempted to fall asleep in their own bedroom, by selecting an appropriate rating between “1 - not at all” and “5 - extremely,” referring to the past week. The sum yields a global PSAS score ranging from 16 to 80. For the Italian version of the PSAS, see the study by Palagini and Manni.42
Resilience
Resilience was evaluated using the RSA.32 RSA is a 33-item self-report scale for adults to measure 6 resilience factors and also provides a total score. Participants were asked to answer on a 7-point semantic differential scale in which each item has a positive and a negative attribute at each end of the scale continuum. Scores may vary between 33 and 231, with higher scores indicating higher levels of resilience. The scale consists of 6 subscales measuring individual's characteristics in: (1) Perception of Self: concerning the confidence in one's abilities, self-confidence, self-efficacy (eg, “No matter what happens I always find a solution”) (2) Planned Future: concerning the ability to plan ahead and formulate clear goals (eg, “My projects for the future are easy to realize”) (3) Social Competence: concerning the individual's own perception of social competence, (eg, “It is important for me to be flexible in social circumstances”) (4) Structured Style: concerning goal oriented, planning ability, organization of one's time, routine oriented (eg, “Rules and regular routines make my daily life easier”) (5) Family Cohesion: concerning shared values, cohesion, loyalty, and mutual appreciation, (eg, “There are strong bonds in my family”), (6) Social Resources: concerning social support (eg, “I always have someone who can help me when needed”). For the Italian version see the study by Capanna et al.45
Emotion Regulation
Emotion regulation was measured with the DERS.37 The DERS is a 36-item scale. When responding to the DERS, subjects were asked to indicate the degree to which the statements of the questionnaire may apply to them by selecting an appropriate rating on a 6-point scale ranging from 1 - almost never to 5 -almost always. The sum yields a global DERS score ranging from 36 to 180, with higher scores reflecting greater difficulties regulating emotion. The questionnaire includes six subscales (1) nonacceptance of emotion (eg, “When I'm upset, I become angry with myself for feeling that way”), (2) difficulties engaging in goal-directed behaviors (eg, “When I'm upset, I have difficulty concentrating“), (3) impulse control difficulties (eg, “I experience my emotions as overwhelming and out of control”), (4) limited access to effective regulatory strategies (eg, “When I'm upset, I believe that there is nothing I can do to make myself feel better”), (4) reduced emotional clarity (eg, “I am confused about how I feel”) and (6) a lack of emotional awareness (eg, “I pay attention to how I feel,” reverse scored). For the Italian version see the study by Sighinolfi et al.46
Psychiatric Scales
Depressive symptoms were assessed using the BDI. The BDI is a self-report 21-question inventory, and it is one of the most widely used instruments for measuring the severity of depression. The total score ranges from 0–63. According to the authors' recommendations, a BDI score > 10 is indicative of depressive symptoms, whereas clinically significant depression is indicated by a score > 20.39
Anxiety symptoms were assessed with the SAS. The SAS is a 20-item self-report assessment, divided into four groups of manifestations: cognitive, autonomic, motor, and central nervous system symptoms. Each question is scored on a Likert-type scale of 1–4. The total score ranges from 0–80. The presence of clinically relevant anxiety symptoms is indicated by scores > 44.38
Statistical Analysis
The statistical analyses were performed using NCSS (2008; NCSS, LLC, Kaysville, Utah, United States). Results were expressed as mean ± standard deviation (SD). The Shapiro-Wilk test was used to determine the normality of the variables. Differences in means between subjects with or without insomnia symptoms were assessed using t tests for normally distributed variables, or the Mann-Whitney U/Wilcoxon test for non-normally distributed variables. Categorical variables were analyzed via the χ2 test. Mean P values were adjusted for the number of tests using the Bonferroni correction with a significance of P < .05. An a priori power estimation analysis provided a sample size of n = 35 with a power of 0.8. A linear regression analysis was performed in order to test the correlations between resilience and stress-related sleep reactivity, pre-sleep arousal, and emotion dysregulation. Multivariable regression models were then built with stress-related sleep reactivity, pre-sleep arousal state, and emotion dysregulation as dependent variables. In the case of a significant correlation between the values and dependent variables on the linear regression analyses, the values were used as independent variables; anxiety and depressive symptoms were used as covariates (expressed by the BDI and the SAS). All the multivariable regression models were checked for multicollinearity. A variable was excluded from the model if it had a variance inflation factor greater than 10 and a condition number greater than 100 in the Eigenvalues of Centered Correlations. A mediation analysis using the Sobel test47 was performed in order to study the possible processes that may underlie the relationships between these variables.
RESULTS
Descriptive Statistics
Of the 182 potential participants evaluated, 58 subjects (39 females, mean age 47.2 ± 13 years, insomnia disorder duration 6.3 ± 0.5 years) met the inclusion/exclusion criteria for insomnia. Twenty-eight subjects evaluated were suspected to suffer from another sleep disorder, 77 subjects suffered from a mental disorder or were using illicit drugs or excluded medications, and 25 subjects did not complete the evaluation. Twenty-eight subjects evaluated were suspected to suffer from another sleep disorder, 77 subjects suffered from a mental disorder or were using illicit drugs or excluded medications, and 25 subjects did not complete the evaluation. Thirty-eight of 50 subjects recruited as healthy controls were included in the study for being matched based on sex and age with the group of insomnia subjects (26 females, mean age 48.4 ± 13 years). In fact, participants with insomnia and healthy controls did not differ in terms of sex distribution (χ2P = .88), mean age (P = .66), socioeconomic status (medium χ2 P = .77), and education level (university degree χ2 P = .78).
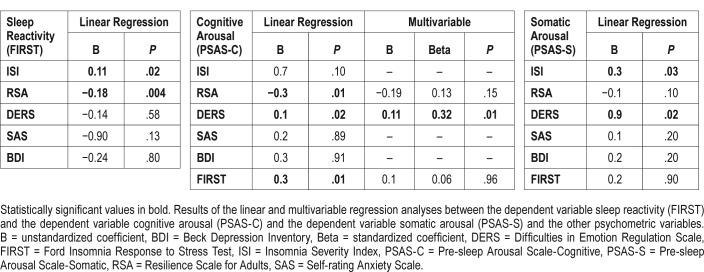
As expected when compared to good sleepers subjects with insomnia showed significantly higher scores on sleep and arousal scales (ie, insomnia severity, sleep reactivity, pre-sleep state arousal < .001) and on all psychiatric scales (depressive symptoms, anxiety symptoms P < .05) (Table 1). In the insomnia group, depressive symptoms were present in 26 individuals, whereas symptoms of anxiety were present in 15 individuals. Subjects with insomnia also presented a lower score in the RAS (P = .002), showing greater problems with resilience. Subjects with insomnia also reported a higher score on the DERS (P < .001), showing elevated difficulties in emotion regulation.
Table 1.
Demographic and psychometric variables.
Determinants of Stress-Related Sleep Reactivity
A linear regression analysis of the good sleepers showed no correlation between sleep-related stress reactivity expressed by FIRST and the variables considered (B = unstandardized coefficient: ISI: B = 0.1, P = .96; RSA: B = 0.03, P = .78; DERS B = −0.15, P = .17; SAS: B = 0.26, P = .10; BDI: B = −0.004, P = .97)
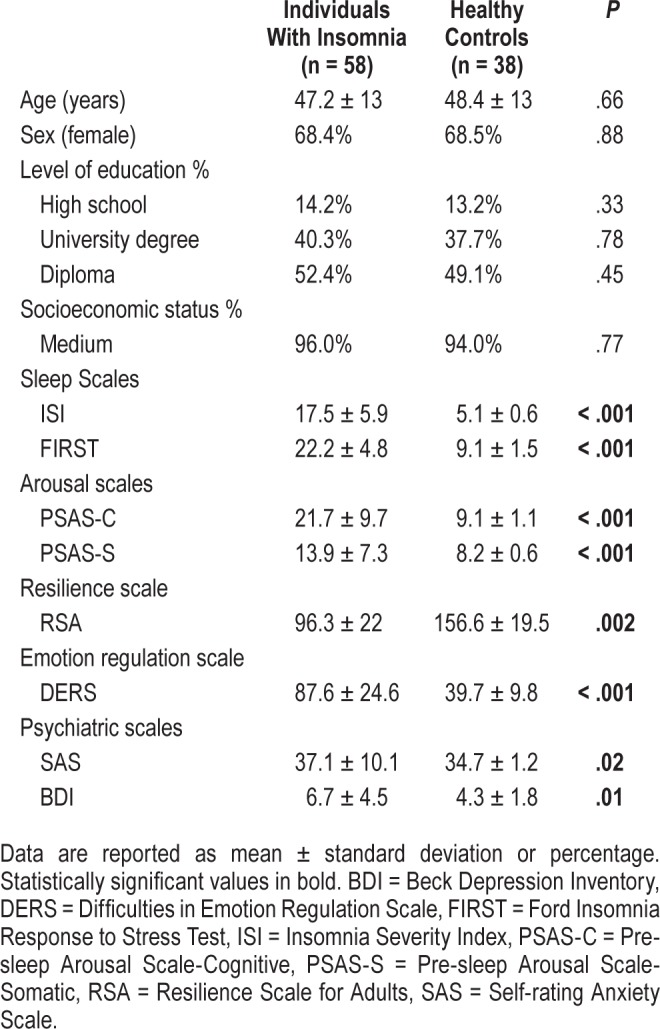
A linear regression analysis of the insomnia participants showed an inverse correlation between high sleep reactivity and resilience (Table 2) (P = .004)
Table 2.
Linear and multivariable regression analyses on stress-related sleep reactivity, cognitive and somatic pre-sleep arousal in subjects with insomnia.
Determinants of Pre-Sleep Arousal
The linear regression analysis in the group of good sleepers showed no correlation between pre-sleep cognitive arousal and the variables considered (B = unstandardized coefficient: ISI: B = 0.02, P = .9; RSA: B = −0.01, P = .23; FIRST: B = 0.02, P = .85; DERS: B = 0.08, P = .4; SAS: B = 0.09, P = .5; BDI: B = 0.07, P = .5).
The linear regression analysis in the insomnia subjects showed an inverse correlation between pre-sleep cognitive hyperarousal, expressed by the PSAS C score, and resilience (P = .01) and a positive correlation with high stress-related sleep reactivity (P = .01) and emotion dysregulation (P = .02) (Table 2).
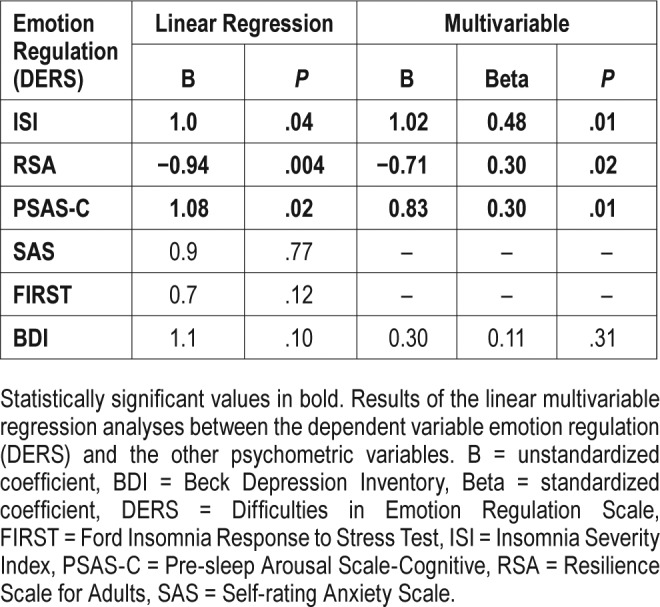
The multivariable-regression model, including the pre-sleep cognitive arousal score as the dependent variable with resilience, and stress-related sleep reactivity and emotion dys-regulation as independent variables, was significant (F = 6.4, P = .005). Emotion dysregulation remained the variable significantly correlated with pre-sleep cognitive hyperarousal (P = .01) (Table 3).
Table 3.
Linear and multivariable regression analyses on emotion dysregulation in subjects with insomnia.
The linear regression analysis in the group of good sleepers showed a correlation between pre-sleep somatic arousal and sleep reactivity (B = unstandardized coefficient: 0.19, P = .02). No other correlations were found with the other variables considered
The linear regression analysis in the insomnia subjects showed a positive correlation between pre-sleep somatic hyperarousal, expressed by the PSAS S score, emotion dysregulation (P = .02) and insomnia symptoms P = .03 (Table 2).
Determinants of Emotion Dysregulation
The linear regression analysis in the group of good sleepers showed no correlation between emotion regulation expressed by DERS and the variables considered (B = unstandardized coefficient: ISI: B = 0.1, P = .4; RSA: B = −0.2, P = .25; FIRST: B = −0.3, P = .1; PSAS C: B = 0.01, P = .4; PSAS S B = 0.9, P = .05; SAS: B = 0.4, P = .07; BDI: B = 0.02, P = .8).
The linear regression analysis in the insomnia participants showed an inverse correlation between emotion dysregulation and resilience score (P = .004), and a positive correlation with insomnia severity (P = .02) and pre-sleep cognitive hyper -arousal (P = .01) (Table 3).
The multivariable-regression model including emotion dys-regulation as the dependent variable, and insomnia symptoms, pre-sleep arousal, and resilience as independent variables, was significant (F = 5.9, P = .004). All three variables remained related to emotion dysregulation (Table 3) and with resilience it resulted in an inverse correlation.
Mediation Analyses
The hypothesis of the study was to investigate the association between resilience emotion dysregulation and pre-sleep hyperarousal. A mediation analysis was conducted with emotion dysregulation as the mediator between resilience and pre-sleep arousal. It revealed a mediation effect of emotion dysregulation in the relationship between low resilience and pre-sleep cognitive hyperarousal in subject with insomnia (Figure 1, Z = 2.06, P = .03).
Figure 1. Mediation analysis.
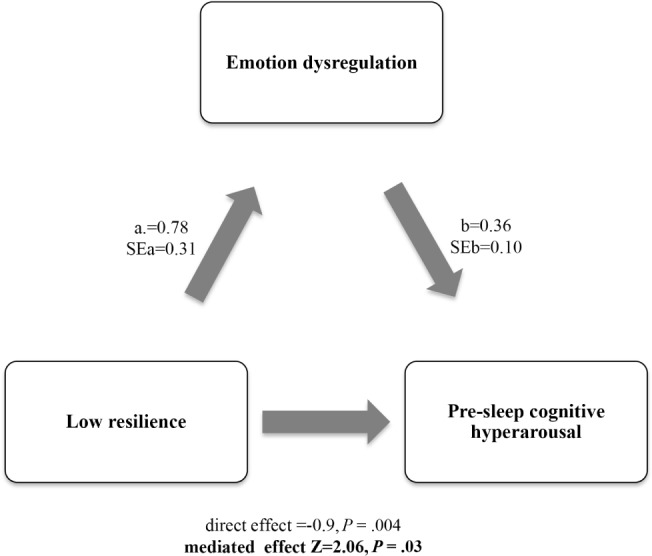
Emotion dysregulation mediates the association between low resilience and pre-sleep hyperarousal. Legend. a: unstandardized regression coefficient for the association between the independent variable and mediator, SEa = standard error of a. b: coefficient for the association between the mediator (in presence of independent variable) and the dependent variable, SEb = standard error of b. Z = Sobel test value. Significance in bold.
DISCUSSION
The stress-risk-vulnerability dimension has been shown to be an important framework for the understanding of insomnia development and maintenance. Within this dimension, there has been a recent paradigm shift in clinical psychology that considers resilience as a critical process for adaptively overcoming stress while maintaining normal psychological and physical functioning. The aim of this research was to evaluate resilience, as a trait characteristic, in subjects with insomnia with the hypothesis that low resilience may contribute to insomnia development and maintenance.
We assessed a sample of subjects with insomnia disorder and a group of good sleepers by evaluating resilience, stress-related sleep reactivity, pre-sleep arousal, and emotion dysregulation while also taking into account psychiatric symptoms and other sleep-related variables.
Among the others we conducted mediation analyses to study the possible processes that may underlie their relationships.
These data provided evidence that subjects with insomnia may present low resilience which in this study was related to high sleep reactivity to stress, cognitive pre-sleep hyperarousal and to emotion dysregulation. Specifically, low resilience was strongly correlated with elevated sleep reactivity, reinforcing the idea that assessing the stress-risk-vulnerability dimension in the context of insomnia should be a priority for prevention and early intervention. Subjects with insomnia may have a low capacity to adaptively overcome stress, and this aspect may negatively influence emotion and arousal regulation thus favoring insomnia development and maintenance.
In the sample of this study, resilience was significantly lower in subjects with insomnia disorder than in good sleepers. Subjects with insomnia showed higher problems with resilience and in particular when compared to good sleepers presented more difficulties concerning goal-oriented planning ability, organization of time and routine, and difficulties in planning ahead and formulating clear goals.
As expected, cognitive and somatic pre-sleep arousal was higher in the insomnia subjects than in good sleepers.15,16 Subjects with insomnia also reported greater difficulties with emotion regulation compared to good sleepers, thus confirming previous reports.48
Although none of the insomnia subjects met DSM-5 criteria for anxiety or depressive disorders, the sample showed some variability in both anxiety and depressive symptoms when compared to good sleepers. This was expected, given that insomnia, depression, and anxiety are highly comorbid.49,50 However, after taking these psychiatric symptoms into account, analyses revealed a close relation between high levels of sleep reactivity and low resilience in insomnia disorder.
The analyses of the relationships of pre-sleep arousal revealed a close relation between cognitive pre-sleep hyper-arousal, low resilience, high sleep reactivity, and emotion dysregulation in insomnia disorder.
Emotion dysregulation in subjects with insomnia was inversely correlated with good resilience in turn being associated with a low capacity to successfully adapt to stressful events. Interestingly, in the mediation analysis, emotion dysregulation was shown to play a role in the relation between trait factors that predispose to psychopathology such as low resilience and state factors that contribute to perpetuate insomnia, such as pre-sleep cognitive hyperarousal. This result is in line with the theory15,16 that predisposing factors are hypothesized to interact with both precipitating factors, increasing the risk of insomnia in response to stress, and with perpetuating factors, including hyperarousal and emotion dysregulation, thus favoring the perpetuation of insomnia. In fact, all of these correlations were not observed in good sleepers. If low resilience has been related to the development of emotional dysregulation and persistent psychopathology,31–34 it should also involve insomnia development and maintenance. Thus we could hypothesize a complex interplay between trait factors that contribute to insomnia in relation to stress, such as low resilience and high stress-related sleep reactivity, and the perpetuating factors of insomnia, such as pre-sleep hyperarousal and emotion dysregulation. Low resilience may predispose to insomnia through a low adaptation to stress, thereby contributing to sleep reactivity and heightened physiologic and emotional responses to stressful situations. Low resilience may also contribute to insomnia perpetuation through emotional and arousal dysregulation, by especially negatively interacting with emotion regulation and consequently with pre-sleep arousal.
These results should be interpreted in light of several limitations including the lack of physiological measures of sleep and arousal. In addition, the cross-sectional design limits any causal interpretation. Consequently, longitudinal studies are needed with larger samples of individuals with chronic insomnia to examine the direction of risk and generalizability of the current findings. In particular, it would be of interest to measure resilience in transitioning from acute to chronic insomnia and after the insomnia was adequately treated.
In conclusion, this study suggests that: (1) subjects with insomnia may possess low resilience, which correlates with higher sleep reactivity to stress and thus predisposing them to insomnia disorder; (2) in particular, low resilience may contribute to insomnia perpetuation by favoring emotion and arousal dysregulation; and (3) emotion dysregulation may play a role in the relationship between trait factors that predispose to insomnia such as a limited capacity to adapt to stressful situations and state factors that perpetuate insomnia such as pre-sleep hyperarousal within a complex interplay. These findings may have clinical implications. It has been found that the assessment of the stress-risk-vulnerability dimension for insomnia should be a priority in order to identify those who may benefit from prevention and early intervention strategies for insomnia and its comorbid conditions. In addition, as low resilience is related to the development of emotional dysregulation,31–34 the evaluation and treatment of emotion dysregulation in insomnia should be useful and approaches targeting emotional regulation could be integrated in insomnia treatments.
DISCLOSURE STATEMENT
Work for this study was performed at the Department of Clinical and Experimental Medicine, Psychiatric Unit, University of Pisa, School of Medicine, Pisa, Italy. All authors have seen and approved the manuscript. The authors report no conflicts of interest.
ABBREVIATIONS
- BDI
Beck Depression Inventory
- DERS
Difficulties in Emotion Regulation Scale
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- FIRST
Ford Insomnia Response to Stress Test
- ICSD
International Classification of Sleep Disorders
- ISI
Insomnia Severity Index
- PSAS-C
Pre-sleep Arousal Scale-Cognitive
- PSAS-S
Pre-sleep Arousal Scale-Somatic
- RSA
Resilience Scale for Adults
- SAS
Self-rating Anxiety Scale
- SD
standard deviation
REFERENCES
- 1.American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association Publishing; 2013. [Google Scholar]
- 3.Léger D, Bayon V. Societal costs of insomnia. Sleep Med Rev. 2010;14(6):379–389. doi: 10.1016/j.smrv.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 4.Leger D, Bayon V, Ohayon MM, et al. Insomnia and accidents: cross-sectional study (EQUINOX) on sleep-related home, work and car accidents in 5293 subjects with insomnia from 10 countries. J Sleep Res. 2013;23(2):143–152. doi: 10.1111/jsr.12104. [DOI] [PubMed] [Google Scholar]
- 5.Kucharczyk E, Morgan K, Hall A. The occupational impact of sleep quality and insomnia symptoms. Sleep Med Rev. 2012;16(6):547–559. doi: 10.1016/j.smrv.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 6.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135(1-3):10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Knutson KL. Does inadequate sleep play a role in vulnerability to obesity? Am J Hum Biol. 2012;24(3):361–371. doi: 10.1002/ajhb.22219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. 2012;73(9):1160–1167. doi: 10.4088/JCP.11r07586. [DOI] [PubMed] [Google Scholar]
- 9.Palagini L, Bruno R, Gemignani A, Baglioni C, Ghiadoni L, Riemann D. Sleep loss and hypertension: a systematic review. Curr Pharm Des. 2013;19(13):2409–2419. doi: 10.2174/1381612811319130009. [DOI] [PubMed] [Google Scholar]
- 10.Fernandez-Mendoza J, Vgontzas A. Insomnia and its impact on physical and mental health. Curr Psychiatry Rep. 2013;15(12):418. doi: 10.1007/s11920-013-0418-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yaffe K, Falvey C, Hoang T. Connections between sleep and cognition in older adults. Lancet Neurol. 2014;13(10):1017–1028. doi: 10.1016/S1474-4422(14)70172-3. [DOI] [PubMed] [Google Scholar]
- 12.Fortier-Brochu E, Morin CM. Cognitive impairment in individuals with insomnia: clinical significance and correlates. Sleep. 2014;37(11):1787–1798. doi: 10.5665/sleep.4172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spielman AJ, Caruso LS, Glovinsky PB. A behavioral perspective on insomnia treatment. Psychiatr Clin North Am. 1987;10(4):541–553. [PubMed] [Google Scholar]
- 14.Drake CL, Roth T. Predisposition in the evolution of insomnia: evidence, potential mechanisms, and future directions. Sleep Med Clin. 2006;1(3):333–349. [Google Scholar]
- 15.Bonnet MH, Arand DL. Hyperarousal and insomnia: state of the science. Sleep Med Rev. 2010;14(1):9–15. doi: 10.1016/j.smrv.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 16.Riemann D, Spiegelhalder K, Feige B, et al. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. 2010;14(1):19–31. doi: 10.1016/j.smrv.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 17.Riemann D, Nissen C, Palagini L, Otte A, Perlis M, Spiegelhalder K. The neurobiology, investigation, and treatment of chronic insomnia. Lancet Neurol. 2015;14(5):547–558. doi: 10.1016/S1474-4422(15)00021-6. [DOI] [PubMed] [Google Scholar]
- 18.Harvey AG. A cognitive model of insomnia. Behav Res Ther. 2002;40(8):869–893. doi: 10.1016/s0005-7967(01)00061-4. [DOI] [PubMed] [Google Scholar]
- 19.Morin CM, Espie CA. Insomnia: A Clinical Guide to Assessment and Treatment. New York, NY: Kluwer Academic/Plenum Publishers; 2003. [Google Scholar]
- 20.Morin CM, Benca R. Chronic insomnia. Lancet. 2012;379(9821):1129–1141. doi: 10.1016/S0140-6736(11)60750-2. [DOI] [PubMed] [Google Scholar]
- 21.Palagini L, Moretto U, Dell'Osso L, Carney C. Sleep-related cognitive processes, arousal, and emotion dysregulation in insomnia disorder: the role of insomnia-specific rumination. Sleep Med. 2017;30:97–104. doi: 10.1016/j.sleep.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 22.Drake C, Richardson G, Roehrs T, Scofield H, Roth T. Vulnerability to stress related sleep disturbance and hyperarousal. Sleep. 2004;27(2):285–291. doi: 10.1093/sleep/27.2.285. [DOI] [PubMed] [Google Scholar]
- 23.Drake CL, Pillai V, Roth T. Stress and sleep reactivity: a prospective investigation of the stress-diathesis model of insomnia. Sleep. 2014;37(8):1295–1304. doi: 10.5665/sleep.3916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fernández-Mendoza J, Vela-Bueno A, Vgontzas AN, et al. Cognitive-emotional hyperarousal as a premorbid characteristic of individuals vulnerable to insomnia. Psychosom Med. 2010;72(4):397–403. doi: 10.1097/PSY.0b013e3181d75319. [DOI] [PubMed] [Google Scholar]
- 25.Jarrin DC, Chen IY, Ivers H, Morin CM. The role of vulnerability in stress-related insomnia, social support and coping styles on incidence and persistence of insomnia. J Sleep Res. 2014;23(6):681–688. doi: 10.1111/jsr.12172. [DOI] [PubMed] [Google Scholar]
- 26.Block JH, Block J. The role of ego-control and ego-resiliency in the origination of behavior. In: Collings WA, editor. The Minnesota Symposia on Child Psychology. Hillsdale, NJ: Erlbaum; 1980. [Google Scholar]
- 27.Masten AS. Resilience in developing systems: progress and promise as the fourth wave rises. Dev Psychopathol. 2007;19(3):921–930. doi: 10.1017/S0954579407000442. [DOI] [PubMed] [Google Scholar]
- 28.Russo SJ, Murrough JW, Han MH, Charney DS, Nestler EJ. Neurobiology of resilience. Nat Neurosci. 2012;15(11):1475–1484. doi: 10.1038/nn.3234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rutter M. Resilience as a dynamic concept. Dev Psychopathol. 2012;24(2):335–344. doi: 10.1017/S0954579412000028. [DOI] [PubMed] [Google Scholar]
- 30.Di Corcia JA, Tronic E. Quotidian resilience: exploring mechanisms that drive resilience from a perspective of everyday stress and coping. Neurosci Biobehav Rev. 2011;3(7):1593–1602. doi: 10.1016/j.neubiorev.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 31.Britt TW, Shen W, Sinclair RR, Grossman MR, Klieger DM. How much do we really know about employee resilience? Ind Organ Psychol. 2016;9(2):378–404. [Google Scholar]
- 32.Hjemdal O, Friborg O, Stiles TC, Rosenvinge JH, Martinussen M. Resilience predicting psychiatric symptoms: a prospective study of protective factors and their role in adjustment to stressful life events. Clin Psychol Psychother. 2006;13:194–201. [Google Scholar]
- 33.Wu G, Feder A, Cohen H, et al. Understanding resilience. Front Behav Neurosci. 2013;15:7–10. doi: 10.3389/fnbeh.2013.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rossetti MC, Tosone A, Stratta P, et al. Different roles of resilience in depressive patients with history of suicide attempt and no history of suicide attempt. Rev Bras Psiquiatr. 2017;39(3):216–219. doi: 10.1590/1516-4446-2016-2045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morin CM. Insomnia: Psychological Assessment and Management. New York, NY: Guilford Press; 1993. [Google Scholar]
- 36.Nicassio PM, Mendlowitz DR, Fussell JJ, Petras L. The phenomenology of the pre-sleep state. The development of the pre-sleep arousal scale. Behav Res Ther. 1985;23(3):263–271. doi: 10.1016/0005-7967(85)90004-x. [DOI] [PubMed] [Google Scholar]
- 37.Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. 2004;30:315. [Google Scholar]
- 38.Zung WWK. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- 39.Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 40.Measso G, Cavarzeran F, Zappalà G, et al. The mini-mental state examination: normative study of an Italian random sample. Dev Neuropsychol. 1993;9:77–85. [Google Scholar]
- 41.Spoormaker VI, Verbeek I, van den Bout J, Klip EC. Initial validation of the SLEEP-50 questionnaire. Behav Sleep Med. 2005;3(4):227–246. doi: 10.1207/s15402010bsm0304_4. [DOI] [PubMed] [Google Scholar]
- 42.Palagini L, Manni R. Misurare il sonno. Torino, Italy: Minerva Medica; 2016. [Google Scholar]
- 43.Lichstein KL, Durrence HH, Taylor DJ, Bush AJ, Riedel BW. Quantitative criteria for insomnia. Behav Res Ther. 2003;41(4):427–445. doi: 10.1016/s0005-7967(02)00023-2. [DOI] [PubMed] [Google Scholar]
- 44.Castronovo V, Galbiati A, Marelli S, et al. Validation study of the Italian version of the Insomnia Severity Index (ISI) Neurol Sci. 2016;37(9):1517–1524. doi: 10.1007/s10072-016-2620-z. [DOI] [PubMed] [Google Scholar]
- 45.Capanna C, Stratta P, Hjemdal O, Rossi A. The Italian validation study of the Resilience Scale for Adults (RSA) Appl Psychol Bull. 2015;272:16–24. [Google Scholar]
- 46.Sighinolfi C, Norcini Pala A, Rocco Chiri L, Marchetti I, Sica C. Difficulties in Emotion Regulation Scale (DERS): Traduzione e adattamento italiano. Psicoterapia Cognitiva e Comportamentale. 2010;1:1–44. [Google Scholar]
- 47.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociol Methodol. 1982;13:290–312. [Google Scholar]
- 48.Baglioni C, Spiegelhalder K, Lombardo C, Riemann D. Sleep and emotions: a focus on insomnia. Sleep Med Rev. 2010;14(4):227–238. doi: 10.1016/j.smrv.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 49.Harvey AG. Insomnia, psychiatric disorders, and the transdiagnostic perspective. Curr Dir Psychol Sci. 2008;17:299–303. [Google Scholar]
- 50.Jansson-Fröjmark M, Lindblom KA. Bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. 2008;64(4):443–449. doi: 10.1016/j.jpsychores.2007.10.016. [DOI] [PubMed] [Google Scholar]