Abstract
Study Objectives:
Many studies suggest an association of both short and long sleep duration with all-cause mortality, but the effect of co-occurrence of sleep duration and other lifestyle risk factors or health status remains unclear.
Methods:
A total of 17,184 participants aged 18 years or older from rural areas of China were examined at baseline from 2007 to 2008 and followed up from 2013 to 2014. Cox proportional hazard models were used to estimate the hazard ratio (HR) and 95% confidence interval (CI).
Results:
During 6-year follow-up, we identified 1,101 deaths. The multivariable-adjusted mortality risk was significantly higher with short-duration sleepers (< 6.5 hours) (HR = 1.37, 95% CI 1.01–1.86) and long-duration sleepers (≥ 9.5 hours) (HR = 1.35, 95% CI 1.05–1.74) versus 6.5–7.5 hours. The multiplicative interaction of long sleep duration with some lifestyle risk factors and health statuses increased the mortality risk in men (low level of physical activity: HR = 1.03, 95% CI 1.02–1.04; hypertension: HR = 1.06, 95% CI 1.04–1.09; type 2 diabetes mellitus [T2DM]: HR = 1.07, 95% CI 1.04–1.11). Similar results were found in women (low level of physical activity: HR = 1.03, 95% CI 1.02–1.05; T2DM: HR = 1.07, 95% CI 1.05–1.10).
Conclusions:
Sleep duration could be a predictor of all-cause mortality and its interaction with physical activity, hypertension, and T2DM may increase the risk of mortality.
Citation:
Liu F, Zhang H, Liu Y, Sun X, Yin Z, Li H, Deng K, Zhao Y, Wang B, Ren Y, Zhang L, Zhou J, Han C, Liu X, Zhang D, Chen G, Hong S, Wang C, Hu D, Zhang M. Sleep duration interacts with lifestyle risk factors and health status to alter risk of all-cause mortality: the Rural Chinese Cohort Study. J Clin Sleep Med. 2018;14(5):857–865.
Keywords: cohort studies, interaction, mortality, sleep duration
BRIEF SUMMARY
Current Knowledge/Study Rationale: Many studies suggested that sleep duration was associated with all-cause mortality. However, there is a paucity of studies focused on the interrelation between sleep duration and lifestyle factors and health status. In our study, we tried to examine the relationship between sleep duration and all-cause mortality and detect the interrelationship between sleep duration (both short and long) and those factors.
Study Impact: Results of the study indicated that both short and long sleep duration was associated with all-cause mortality and that long sleep duration interacted with low level of physical activity, hypertension, and type 2 diabetes mellitus. Our study of a rural Chinese population has great public health significance and the conclusions could provide useful and important evidence for future intervention programs.
INTRODUCTION
Sleep is a biobehavioral phenomenon regulated by circadian, homeostatic, and neurohormonal process.1 Accumulating evidence2 shows that as compared with sleep duration of approximately 7 hours, both shorter and longer sleep duration is associated with adverse health outcomes such as cardiovascular disease, diabetes mellitus, and hypertension, and further affects life expectancy and all-cause mortality.
Studies conducted in America suggested that demographic characteristics such as race, sex, age, lifestyle, health status, and socioeconomic status (including marital status, financial strain, and education level) were related to sleep duration.3,4 In China, age, unhealthy lifestyles, poor health conditions, obesity, and dietary fat content were associated with both short and long sleep duration.5,6 Thus, the relationship of sleep to all-cause mortality is complex. Previous studies of sleep-related mortality concluded the relationship as a U shape, but the casual relationship between sleep and all-cause mortality is debated.7 Some researchers suggest poor lifestyle factors8,9 (such as low level of physical activity, smoking, alcohol drinking, and unhealthy diet) or health status7 (hypertension and diabetes) might confound the association or be a primary driving factor of the sleep-mortality relationship. Decreased quantity and quality of sleep may link to hypertension, obesity, diabetes, and dyslipidemia.10 However, only one study explored the interrelation between sleep duration and lifestyle risk factors or health status in terms of all-cause mortality; the risk factors were limited to physical activity, sedentary behavior, and body mass index (BMI).11 Moreover, few cohort studies have focused on sleep-related mortality in China12–16 and none involved the interaction between sleep duration and other risk factors. It is unknown whether the risk of death would be increased or to what degree the extreme sleep duration combined with lifestyle factors or health status could increase the risk of mortality.
Here, we aimed to examine the relationship between sleep duration and all-cause mortality using data from the Rural Chinese Cohort Study, which was initially established to examine chronic noncommunicable diseases such as hypertension and diabetes. In this population, the crude prevalence of high blood pressure was 31.5%, and the age-standardized prevalence of diabetes was 6.98% at baseline.17,18 These participants mainly had primary or secondary education, with smoking and drinking mainly seen in men. Considering the prevalence of health conditions and the special demographic characteristics of the rural population, we could further explore the interaction between sleep duration and smoking, alcohol drinking, physical activity, obesity, hypertension, type 2 diabetes mellitus (T2DM), and dyslipidemia with all-cause mortality risk.
METHODS
Study Population
A total of 20,194 participants aged 18 years or older were selected by a cluster randomization method from July to August of 2007 and July to August of 2008 in rural areas of Henan province of China. All participants were stable residents for at least 10 years. The follow-up survey was conducted from July to August 2013 and July to October 2014 and 17,265 participants (response rate: 85.5%) were successfully followed up. We excluded 3 participants who had no data on sleep duration and 78 participants with outlier of sleep duration (≤ 3 or ≥ 16 hours); finally, 17,184 participants were eligible for the current analysis.
Each study participant gave their signed informed consent and the study protocol was approved by Shenzhen University Medical Ethics Committee.
Data Collection
Baseline data were collected on demographic characteristics, medical history, and lifestyle risk factors by specially trained physicians and public health investigators. Physical examination provided data on height, weight, waist circumference, systolic blood pressure, and diastolic blood pressure. The measurement methods have been described in detail elsewhere.19 Overnight fasting venous blood samples were collected to measure levels of fasting plasma glucose, total cholesterol (TC), triglycerides, and high-density lipoprotein cholesterol (HDL-C) by using an Automatic Biochemistry Analyzer (HITACHI 7060, Tokyo). Low-density lipoprotein cholesterol level was calculated by the Friedewald formula.20
Principal Variables and Definitions
Self-reported sleep duration was collected by asking the following question: During the past month, how many hours do you sleep per day (including both nighttime and daytime sleep)? Sleep duration was divided into 5 groups: < 6.5, 6.5– 7.5, 7.5–8.5, 8.5–9.5, and ≥ 9.5 h/d. Dates of death were acquired by face-to-face interview with participants' family members or the village doctor during the follow-up survey. We also checked the death information with vital registration data from the local Centers for Disease Control and Prevention. The survival time was calculated from the date of the baseline survey to the date of death.
Covariates and Definitions
Marital status was classified as unmarried, married/cohabitating, and widowed/divorced/separated. Education level was classified as primary school, secondary school, and college or above. Monthly per capita income was classified into 3 categories: ≤ 500, 501–1,000, and > 1,000 yuan. Smoking was defined as having smoked ≥ 100 cigarettes during the lifetime and participants were classified as nonsmokers, exsmokers, and current smokers. Nondrinkers included irregular drinkers who drank less than once a month. Daily alcohol consumption (ethanol g/d) was calculated and classified into three categories according to tertiles. Participants who drank tea at least 3 times a week and for more than 6 months were considered tea drinkers. According to the consumption of tea every month, tea drinkers were divided into 100 or fewer and more than 100 g/mo. Given that the physical activity of the rural population in China is mainly farm work, we evaluated work-related physical activity and classified it as low, moderate, and high according the International Physical Activity Questionnaire.21
According to the obesity standard in China, BMI was calculated as weight in kilograms divided by height in meters squared, and classified as underweight (< 18.5 kg/m2), normal weight (18.5–23.9 kg/m2), overweight (24.0–27.9 kg/m2), and obese (≥ 28 kg/m2).22 Hypertension was defined as systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg and/or using antihypertensive medication.23 Fasting plasma glucose ≥ 7.0 mmol/L and/or self-reported current diabetes-related medication were defined as T2DM.24 Dyslipidemia was defined as levels of total cholesterol ≥ 6.22 mmol/L or triglycerides ≥ 2.26 mmol/L or low-density lipo-protein cholesterol ≥ 4.14 mmol/L or high-density lipoprotein cholesterol < 1.04 mmol/L.25
Statistical Analysis
The characteristics of participants were compared by sleep-duration categories. All continuous variables showed a skewed distribution and the Kruskal-Wallis test was used for analyzing both categorical and continuous variables. Linear trend was tested by Cochran-Mantel-Haenszel test. Person-years of follow-up were calculated from baseline to the date of death or the end of follow-up, and all-cause mortality per 1,000 person-years was calculated by using the number of events divided by the total number of person-years.
Cox regression models adjusted for some potential confounders were used to estimate the hazard ratio (HR) and 95% confidence interval (95% CI) for short and long sleep duration. The adjusted HR was calculated in two models. The first model adjusted for sociodemographic variables (sex, age, marital status, education level, and monthly income); the second model further adjusted for lifestyle variables, usual chronic diseases, and indicators (smoking status, alcohol, tea drinking, physical activity level, BMI, systolic blood pressure, fasting plasma glucose and triglycerides, and high-density lipoprotein cholesterol levels).
Because both short and long sleep duration were associated with all-cause mortality, we excluded people with sleep duration 9.5 h/d or more when analyzing interaction between short sleep duration and other risk factors. A similar approach was also applicable to the analysis of long sleep duration and other risk factors. Crossover analysis was conducted to explore an interaction between sleep duration and lifestyle risk factors or health status on all-cause mortality. An HR with 95% CI of the multiplicative interaction was estimated by Cox regression, and variables used in the regression model were all continuous or multicategorical. Testing for multiplicative interaction involved the Wald test. As suggested by the results of previous studies,26 sleep duration 6.5 to 7.5 hours was the reference to compare the risk of death in different situations.
Analyses were performed with SAS 9.13 for Windows (SAS Institute Inc, Cary, North Carolina, United States) and STATA 12.0 (StataCorp, College Station, Texas, United States). A value of P < .05 (two-sided) was considered statistically significant.
RESULTS
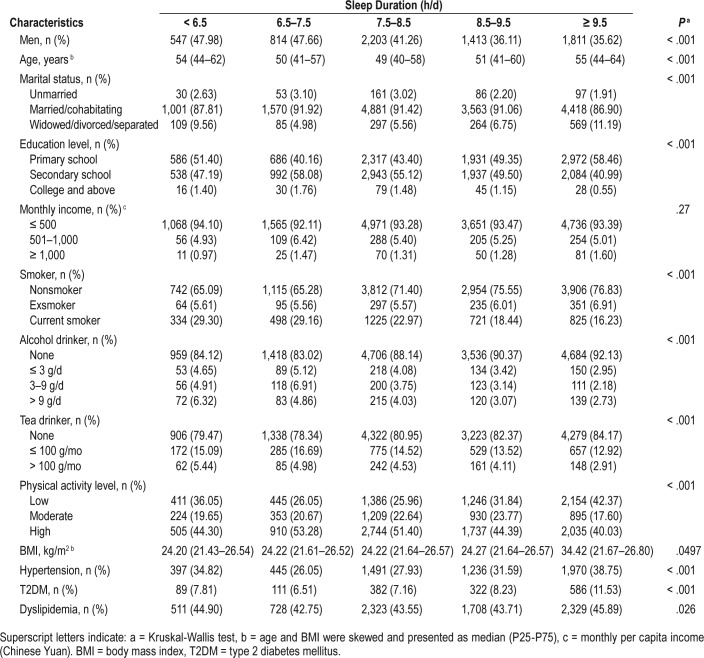
Table 1 shows the baseline characteristics of participants by sleep duration. Participants with 8.5 to 9.5 and 9.5 or more hours of sleep were mainly women and overweight and obese and had T2DM (P for sex and T2DM < .001, P for BMI = .0497). The frequency of smokers decreased with increasing sleep duration (P < .001). Participants with 6.5 to 7.5 hours versus other sleep durations were frequently regular alcohol and tea drinkers (both P < .001). As compared with participants with 6.5 to 7.5 hours of sleep, those with shorter duration (< 6.5 hours) and longer duration (≥ 9.5 hours) were less educated and more frequently widowed/divorced/separated, older, or had a low level of work-related physical activity, hypertension, and dyslipidemia (P < .001 for education, marital status, physical activity and hypertension; P = .026 for dyslipidemia).
Table 1.
General characteristics of the study population at baseline by sleep duration among rural Chinese adults.
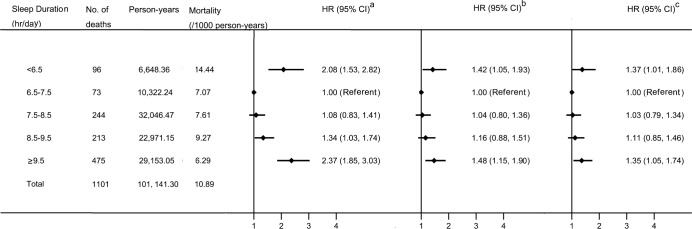
During 101,141.3 person-years of follow-up, we identified 1,101 deaths (cancer: 267, cardiovascular disease: 478, other reason: 356). The all-cause mortality was 10.89/1,000 person-years for all participants, 14.44/1,000 for short-duration sleepers (< 6.5 h/d) and 28.50/1,000 for long-duration sleepers (≥ 9.5 h/d) (Figure 1). Risk of unadjusted mortality was significantly increased with < 6.5 hours (HR = 2.08, 95% CI 1.53–2.82), 8.5–9.5 hours (HR = 1.34, 95% CI 1.03–1.74), and ≥ 9.5 hours (HR = 2.37, 95% CI 1.85–3.03) as compared with 6.5–7.5 hours. The risk decreased only slightly with additional adjustment in the second model (< 6.5 hours: HR = 1.37, 95% CI 1.01–1.86 and ≥ 9.5 hours: HR = 1.35, 95% CI 1.05–1.74).
Figure 1. Association between baseline sleep duration and all-cause mortality for all participants.
Superscript letters indicate: a = unadjusted model; b = model 1: adjusted for sex, age, marital status, education level, and monthly income; c = model 2: adjusted for covariates in Model 1 and smoking status, alcohol, tea drinking, physical activity level, body mass index, systolic blood pressure, fasting plasma glucose, and triglycerides and high-density lipoprotein cholesterol levels. CI = confidence interval, HR = hazard ratio.
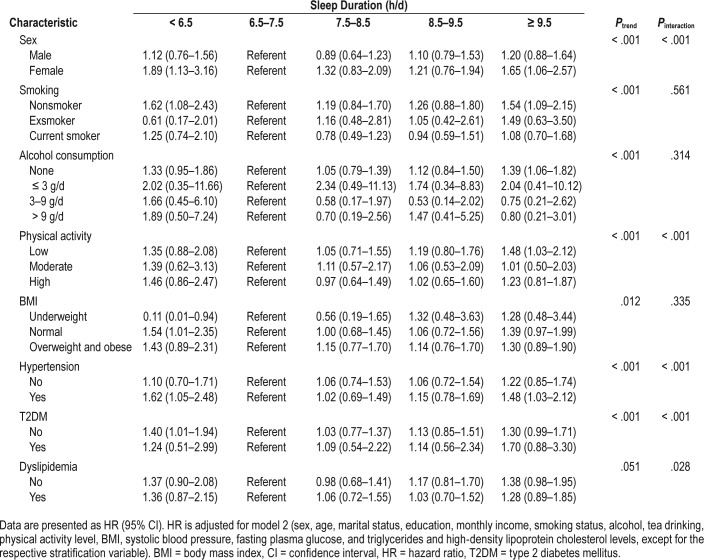
Table 2 presents the relationship between sleep duration and mortality stratified by lifestyle risk factors and health status. For women, the risk of death was increased with fewer than 6.5 hours and 9.5 hours or more of sleep (HR = 1.89, 95% CI 1.13–3.16 and HR = 1.65, 95% CI 1.06–2.57, respectively), as compared with 6.5–7.5 hours. For nonsmokers, the risk of death was increased 62% with fewer than 6.5 hours of sleep and 54% with 9.5 hours or more of sleep. The sleep-mortality association existed similarly in nonalcohol drinkers and people without T2DM. The association between sleep duration and all-cause mortality appeared to be stronger with than without hypertension. With a low level of physical activity, risk of death was increased 48% with 9.5 hours or more of sleep. Sleep duration was not related to mortality in overweight and obese population. However, the underweight population showed reduced risk of death with fewer than 6.5 hours of sleep.
Table 2.
Association between sleep duration and all-cause mortality by sex, behavior risk factors, and selected chronic diseases.
We found a significant interaction between sleep duration and sex in all-cause mortality (P interaction for sex < .001); therefore, we performed interaction analysis with men and women separately. Higher all-cause mortality was observed among people with fewer than 6.5 h/d and with hypertension (women: HR = 2.28, 95% CI 1.09–4.73; men: HR = 2.83, 95% CI 1.60– 5.02) (Table S1 and Table S2 in the supplemental material). For women, the risk of all-cause mortality was increased with fewer than 6.5 hours of sleep duration combined with low level of physical activity (HR = 3.77, 95% CI 1.75–8.12), overweight and obesity (HR = 2.62, 95% CI 1.10–6.23), T2DM (HR = 2.70, 95% CI 1.10–6.64), and dyslipidemia (HR = 2.40, 95% CI 1.14– 5.05). Additionally, we found a statistically significant synergistic interaction between fewer than 6.5 hours of sleep duration and hypertension for men (HR = 1.14, 95% CI 1.07–1.22). Compared with people who reported 6.5–7.5 hours of sleep and without hypertension, the risk of death among hypertensive individuals with fewer than 6.5 hours of sleep was 1.83 times higher (HR = 2.83, 95% CI 1.60–5.02), and 7.4% (0.14/1.89) of the 183% excess risk could be attributed to the interaction of short sleep duration and low level of physical activity in men.
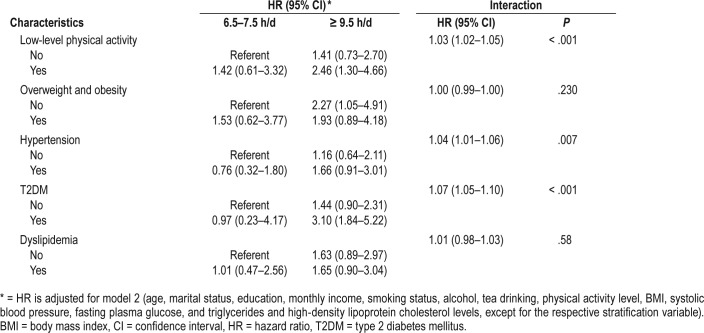
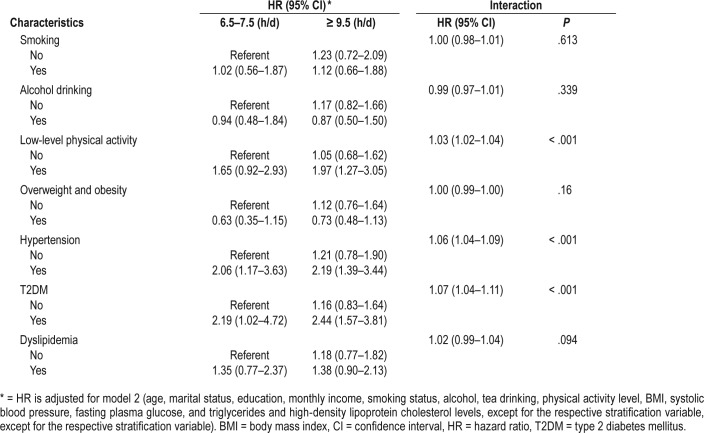
A multiplicative interaction was found between long sleep duration (≥ 9.5 hours) and low level of physical activity and T2DM for both men and women. For women, the risk of death was increased 146% with long sleep duration combined with low level of physical activity (HR = 2.46, 95% CI 1.30–4.66), and 2.1% (0.03/1.46) of the increased risk was caused by the interaction (HR = 1.03, 95% CI 1.02–1.05). With long sleep duration combined with T2DM, the risk of death was increased 2.1-fold (women: HR = 3.10, 95% CI 1.84–5.22), and 3.3% of the excess risk was due to the interaction between long sleep duration and T2DM (HR = 1.07, 95% CI 1.05–1.10) (Table 3). Similarly, the coexistence of long sleep duration and low level of physical activity was associated with 97% increased risk of death for men (HR = 1.97, 95% CI 1.27–3.05), and its multiplicative interaction was also significantly associated with 3.1% increased risk of all-cause mortality (HR = 1.03, 95% CI 1.02–1.04). The combination of long sleep duration and T2DM increased the risk of death 144% for men (HR = 2.44, 95% CI 1.57–3.81), and 4.9% (0.07/1.44) of the increased risk was attributed to the interaction (HR = 1.07, 95% CI 1.04–1.11). Additionally, with long duration of sleep in hypertensive men (≥ 9.5 hours), the risk of death was increased 119% (HR = 2.19, 95% CI 1.39–3.44), and the interaction accounted for 5.0% of the excess risk (HR = 1.06, 95% CI 1.04–1.09) (Table 4).
Table 3.
Cox regression analysis of the multiplicative interaction between long sleep duration and lifestyle factors or health status in women.
Table 4.
Cox regression analysis of the multiplicative interaction between long sleep duration and lifestyle factors or health status in men.
DISCUSSION
In this study, we found increased all-cause mortality with both short (< 6.5 hours) and long (≥ 9.5 hours) sleep duration as compared with 6.5–7.5 h/d, even in participants with healthy lifestyles (not smoking or alcohol drinking), without obesity and T2DM. Moreover, the results of multiplicative interaction analysis suggested a statistically significant synergistic interaction between long sleep duration and low level of exercise and T2DM in relation to all-cause mortality. Specifically, the synergistic interaction was between long sleep duration and hypertension for men and short sleep duration and low level of physical activity for women.
After adjusting for potential confounders, both short and long sleep duration were related to all-cause mortality for all participants and more pronounced for women. Another Chinese study12 including 113,138 participants found an association for men (HR = 1.06, 95% CI 0.90–1.25 and HR = 1.55, 95% CI 1.29–1.86 for 4 to 5 hours and ≥ 10 hours, respectively), with a greater association for women (HR = 1.15, 95% CI 1.01–1.32 and HR = 2.11, 95% CI 1.77–2.52, respectively). The prevalence of sleep problems in women was higher than in men and the rates increased with age.27 Thus, the all-cause mortality can greatly differ in men and women.28
Low level of physical activity contributed to the all-cause mortality in our study, and our results were consistent with a Belgian physical fitness study finding low level of occupational physical activity related to all-cause mortality (HR = 2.07, 95% CI 1.03–4.19).29 The results may be compatible with activity settings and physical fitness. In the stratification of smoker, alcohol drinker, T2DM, and obesity, the U-shaped association between sleep duration and all-cause mortality was not statistically significant. This may be caused by the stronger association between smoking,30 alcohol drinking,31 T2DM and obesity,32 and all-cause mortality. In the underweight population, sleeping fewer than 6.5 hours could reduce the risk of death and this situation may result from nutrition status, potential increasing physical activity, or the smaller sample size with underweight stratification
A meta-regression of 40 prospective cohort studies also confirmed that as compared with 7 hours of sleep, both shortened and prolonged sleep durations were associated with increased risk of all-cause mortality.33 However, there is still a hot debate on whether sleep duration is truly associated with all-cause mortality. Hall et al.7 enrolled 3,075 participants and found that the sleep–mortality association was mainly explained by lifestyle factors and health status. Kurina et al.34 summarized that men, the elderly, and individuals with increased TC/ HDL-C, recent treatment for cancer, or heart attack tended to report longer sleep duration; individuals with obesity, diabetes, hypertension, or poor general health tended to report short sleep duration; black race, unmarried individuals, those with low socioeconomic status, and working long hours were factors more likely to affect both long and short sleep duration. In the current work, however, we found sleep-related mortality in individuals with healthy lifestyles (no smoking and alcohol drinking) or with favorable health status (without T2DM and obesity), which indicated that the sleep–mortality relationship was not entirely driven by poor health and sleep duration could be a predictor of all-cause mortality.
Currently, few studies have focused on the interaction between sleep duration and other factors when researching sleep and all-cause mortality. Xiao et al.11 explored the change in total mortality when short sleep duration coexisted with physical activity, sedentary behavior, and BMI and they found short sleep duration interacted with BMI. In our study, we found that short sleep duration interacted only with hypertension in men. Additionally, the multiplicative interaction of long sleep duration with low level of physical activity and T2DM increased mortality risk both in men and women. Extreme sleep duration was associated with low level of physical activity, hyper-tension, and T2DM. In terms of physical activity, low level of physical activity contributed to reduced quality and duration of sleep and affected sleep onset latency and bedtime.35 An intervention of exercise suggested that a lack of physical activity could increase napping and that regular exercise could be a useful method to improve sleep.36,37 Excessive sleep can lead to an increase in proinflammatory cytokine levels, considered to cause pancreatic beta-cell dysfunction. Lifestyle interventions (fiber intake and physical activity) for long sleepers were effective in lowering diabetes risk.38 In terms of hypertension, short sleep duration could result in overactivity of the reninangiotensin-aldosterone system, proinflammatory responses, endothelial dysfunction, and alter the circadian rhythm, factors considered to contribute to the risk of hypertension. The mechanisms between long duration of sleep and hypertension are not clear. Some studies suggested that long sleep duration was related to high TC or HDL-C level or often accompanied by less physical activity and inactivity, related to increased risk of hypertension.39 In contrast, in individuals with T2DM, hypertension, or low level of physical activity, sleep disorders or excessive or insufficient sleep are more likely to develop.40–42 These factors could contribute to the vicious cycle of too short or long sleep duration and adverse health status.
Various mechanisms of the relation of sleep duration and all-cause mortality have been proposed, but they remain unclear. Sleep duration is influenced by socioeconomic status, lifestyle risk factors, stress, and age.43 Mortality caused by long sleep duration could result from sleep fragmentation and sympathetic nervous system activation,15,44,45 which are considered to influence the physiological reduction of the photoperiod46 and then change the physical condition and physiological cycle. Short sleep duration is linked to the length of leukocyte telomeres in men, which may help to explain the mechanisms between short sleep and poor health outcomes in older men.47 The biologic mechanism proposed for sleep-related mortality could be summarized as extreme sleep duration causing a change in endocrine, immune, and metabolic systems. In detail, excessive sleep is associated with higher levels of evening cortisol, oxygen-free copper-guanosine triphosphate, calcium, uric acid, creatinine, and glucose and reduced levels of alkaline phosphatase, cholinesterase, lactate dehydrogenase, and leptin secretion.48,49 People who lack sleep often have higher levels of lactate dehydrogenase, calcium, and total cholesterol, and lower alkaline phosphatase level.33 Thus, sleep duration could affect homeostasis and further contribute to death. The sleep–mortality association may be explained by a chronic inflammation process. Sleep duration is associated with elevated levels of C-reactive protein and cytokines (such as interleukin-6 and tumor necrosis factor-α),50–52 which are considered related to increased risk of death. Additionally, Kronholm et al.53 hypothesized that extreme sleep duration and risk of death depended on genetic predisposition, and its expression might be modulated by lifestyle factors and health status.
Sleep duration is largely influenced by environmental factors and can be modified by public health measures such as education and counseling.54 Considering our findings, risk of mortality attributable to short or long sleep may increase with the prevalence of extreme sleep duration, especially in individuals with a low level of exercise, hypertension, and T2DM. In terms of public health implications, too-short or too-long sleep duration could be used as a diagnostic tool to detect subclinical or undiagnosed comorbidity or could identify a group at increased risk for all-cause mortality.54 In addition to promoting health education to raise people's awareness of reasonable sleep, public health surveil-lance, especially of a high-risk population, should be strengthened and appropriate interventions should be implemented.
Our study has several strengths. It is a longitudinal study based on a rural population of China, and participants were recruited from a large general population, which allows for reasonable generalization of our results. Total sleep duration rather than nighttime sleep duration was investigated, which is a useful way to evaluate sleep,55 because people often also sleep in the daytime. The stratification analysis can help to understand the role of lifestyle and health status in the sleep-mortality association. Moreover, the multiplicative model showed an interaction between extreme sleep duration and other factors, and the risk was greater than that with the factors alone.
Despite the strengths of the study, there are several limitations. First, because sleep duration was self-reported and assessed by few questions, sleep duration may have been estimated inaccurately. A single measure of exposure could not capture the sustained long-term effects on mortality. Dynamic changes in sleep duration over time may be a better measure of exposure.56 Second, we did not collect data on depression or other affective disease, sleep quality, sleep apnea, or obstructive sleep apnea, which could affect the health of long-duration sleepers. Sleep quality is expected to be interacted with sleep duration to increase the risk of hypertension, diabetes or other health outcomes.57,58 Moreover, sleep quality is considered as an important risk factor for all-cause mortality.59 Thus, further studies with dynamic changes in sleep duration or involving sleep quality are still needed to explore the risk of mortality.
In conclusion, we observed a U-shaped association of sleep duration and all-cause mortality in rural Chinese adults that suggests recommending sleep duration of 7 hours. Furthermore, risk of all-cause mortality may be increased with too-long or too-short sleep duration combined with a low level of exercise, hypertension, and T2DM.
DISCLOSURE STATEMENT
All authors have read and approved the final version of the article. This study was supported by the National Natural Science Foundation of China (No. 81373074, 81402752 and 81673260) and Science and Technology Development Foundation of Shenzhen (No. JCYJ20160307155707264). The authors report no conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the participants and staff members for their important contributions.
ABBREVIATIONS
- BMI
body mass index
- CI
confidence interval
- HR
hazard ratio
- T2DM
type 2 diabetes mellitus
REFERENCES
- 1.Shan Z, Ma H, Xie M, et al. Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. 2015;38(3):529–537. doi: 10.2337/dc14-2073. [DOI] [PubMed] [Google Scholar]
- 2.Da SA, de Mello RG, Schaan CW, Fuchs FD, Redline S, Fuchs SC. Sleep duration and mortality in the elderly: a systematic review with meta-analysis. BMJ Open. 2016;6(2):e8119. doi: 10.1136/bmjopen-2015-008119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kripke DF, Jean-Louis G, Elliott JA, et al. Ethnicity, sleep, mood, and illumination in postmenopausal women. BMC Psychiatry. 2004;4:8. doi: 10.1186/1471-244X-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kalleinen N, Polo-Kantola P, Himanen SL, et al. Sleep and the menopause - do postmenopausal women experience worse sleep than premenopausal women? Menopause Int. 2008;14(3):97–104. doi: 10.1258/mi.2008.008013. [DOI] [PubMed] [Google Scholar]
- 5.Shi Z, McEvoy M, Luu J, Attia J. Dietary fat and sleep duration in Chinese men and women. Int J Obes (Lond) 2008;32(12):1835–1840. doi: 10.1038/ijo.2008.191. [DOI] [PubMed] [Google Scholar]
- 6.Tu X, Cai H, Gao YT, et al. Sleep duration and its correlates in middle-aged and elderly Chinese women: the Shanghai Women's Health Study. Sleep Med. 2012;13(9):1138–1145. doi: 10.1016/j.sleep.2012.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hall MH, Smagula SF, Boudreau RM, et al. Association between sleep duration and mortality is mediated by markers of inflammation and health in older adults: the Health, Aging and Body Composition Study. Sleep. 2015;38(2):189–195. doi: 10.5665/sleep.4394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jankovic N, Geelen A, Streppel MT, et al. Adherence to a healthy diet according to the World Health Organization guidelines and all-cause mortality in elderly adults from Europe and the United States. Am J Epidemiol. 2014;180(10):978–988. doi: 10.1093/aje/kwu229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shi Z, Zhang T, Byles J, Martin S, Avery JC, Taylor AW. Food habits, lifestyle factors and mortality among oldest old Chinese: the Chinese Longitudinal Healthy Longevity Survey (CLHLS) Nutrients. 2015;7(9):7562–7579. doi: 10.3390/nu7095353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kohansieh M, Makaryus AN. Sleep deficiency and deprivation leading to cardiovascular disease. Int J Hypertens. 2015;2015:615681. doi: 10.1155/2015/615681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xiao Q, Keadle SK, Hollenbeck AR, Matthews CE. Sleep duration and total and cause-specific mortality in a large US cohort: interrelationships with physical activity, sedentary behavior, and body mass index. Am J Epidemiol. 2014;180(10):997–1006. doi: 10.1093/aje/kwu222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cai H, Shu XO, Xiang YB, et al. Sleep duration and mortality: a prospective study of 113 138 middle-aged and elderly Chinese men and women. Sleep. 2015;38(4):529–536. doi: 10.5665/sleep.4564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Qiu L, Sautter J, Liu Y, Gu D. Age and gender differences in linkages of sleep with subsequent mortality and health among very old Chinese. Sleep Med. 2011;12(10):1008–1017. doi: 10.1016/j.sleep.2011.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen HC, Su TP, Chou P. A nine-year follow-up study of sleep patterns and mortality in community-dwelling older adults in Taiwan. Sleep. 2013;36(8):1187–1198. doi: 10.5665/sleep.2884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chien KL, Chen PC, Hsu HC, et al. Habitual sleep duration and insomnia and the risk of cardiovascular events and all-cause death: report from a community-based cohort. Sleep. 2010;33(2):177–184. doi: 10.1093/sleep/33.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee WJ, Peng LN, Liang CK, Chiou ST, Chen LK. Long sleep duration, independent of frailty and chronic Inflammation, was associated with higher mortality: a national population-based study. Geriatr Gerontol Int. 2017;17(10):1481–1487. doi: 10.1111/ggi.12899. [DOI] [PubMed] [Google Scholar]
- 17.Zhao Y, Zhang M, Luo X, et al. Association of obesity categories and high blood pressure in a rural adult Chinese population. J Hum Hypertens. 2016;30(10):613–618. doi: 10.1038/jhh.2016.1. [DOI] [PubMed] [Google Scholar]
- 18.Liu X, Li Y, Li L, et al. Prevalence, awareness, treatment, control of type 2 diabetes mellitus and risk factors in Chinese rural population: the RuralDiab study. Sci Rep. 2016;6:31426. doi: 10.1038/srep31426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang M, Han C, Wang C, et al. Association of resting heart rate and cardiovascular disease mortality in hypertensive and normotensive rural Chinese. J Cardiol. 2017;69(5):779–784. doi: 10.1016/j.jjcc.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 20.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502. [PubMed] [Google Scholar]
- 21.Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 22.Chen C, Lu FC. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci. 2004;17(Suppl):1–36. [PubMed] [Google Scholar]
- 23.Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenwich) 2014;16(1):14–26. doi: 10.1111/jch.12237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37(Suppl 1):S81–S90. doi: 10.2337/dc14-S081. [DOI] [PubMed] [Google Scholar]
- 25.Joint Committee for Developing Chinese guidelines on Prevention and Treatment of Dyslipidemia in Adults. [Chinese guidelines on prevention and treatment of dyslipidemia in adults] Zhonghua Xin Xue Guan Bing Za Zhi. 2007;35(5):390–419. [PubMed] [Google Scholar]
- 26.Yeo Y, Ma SH, Park SK, et al. A prospective cohort study on the relationship of sleep duration with all-cause and disease-specific mortality in the Korean Multi-center Cancer Cohort study. J Prev Med Public Health. 2013;46(5):271–281. doi: 10.3961/jpmph.2013.46.5.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6(2):97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 28.Lindahl-Jacobsen R, Hanson HA, Oksuzyan A, Mineau GP, Christensen K, Smith KR. The male-female health-survival paradox and sex differences in cohort life expectancy in Utah, Denmark, and Sweden 1850-1910. Ann Epidemiol. 2013;23(4):161–166. doi: 10.1016/j.annepidem.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clays E, Lidegaard M, De Bacquer D, et al. The combined relationship of occupational and leisure-time physical activity with all-cause mortality among men, accounting for physical fitness. Am J Epidemiol. 2014;179(5):559–566. doi: 10.1093/aje/kwt294. [DOI] [PubMed] [Google Scholar]
- 30.Lam TH, Xu L, Schooling CM, Chan WM, Lee SY, Leung GM. Smoking and mortality in a prospective cohort study of elderly Chinese in Hong Kong. Addiction. 2015;110(3):502–510. doi: 10.1111/add.12776. [DOI] [PubMed] [Google Scholar]
- 31.Mackenbach JP, Kulhanova I, Bopp M, et al. Inequalities in alcohol-related mortality in 17 European countries: a retrospective analysis of mortality registers. PLoS Med. 2015;12(12):e1001909. doi: 10.1371/journal.pmed.1001909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Masters RK, Reither EN, Powers DA, Yang YC, Burger AE, Link BG. The impact of obesity on US mortality levels: the importance of age and cohort factors in population estimates. Am J Public Health. 2013;103(10):1895–1901. doi: 10.2105/AJPH.2013.301379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu TZ, Xu C, Rota M, et al. Sleep duration and risk of all-cause mortality: a flexible, non-linear, meta-regression of 40 prospective cohort studies. Sleep Med Rev. 2017;32:28–36. doi: 10.1016/j.smrv.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 34.Kurina LM, McClintock MK, Chen JH, Waite LJ, Thisted RA, Lauderdale DS. Sleep duration and all-cause mortality: a critical review of measurement and associations. Ann Epidemiol. 2013;23(6):361–370. doi: 10.1016/j.annepidem.2013.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brychta RJ, Arnardottir NY, Johannsson E, et al. Influence of day length and physical activity on sleep patterns in older Icelandic men and women. J Clin Sleep Med. 2016;12(2):203–213. doi: 10.5664/jcsm.5486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Littman AJ, Vitiello MV, Foster-Schubert K, et al. Sleep, ghrelin, leptin and changes in body weight during a 1-year moderate-intensity physical activity intervention. Int J Obes (Lond) 2007;31(3):466–475. doi: 10.1038/sj.ijo.0803438. [DOI] [PubMed] [Google Scholar]
- 37.Sherrill DL, Kotchou K, Quan SF. Association of physical activity and human sleep disorders. Arch Intern Med. 1998;158(17):1894–1898. doi: 10.1001/archinte.158.17.1894. [DOI] [PubMed] [Google Scholar]
- 38.Tuomilehto H, Peltonen M, Partinen M, et al. Sleep duration, lifestyle intervention, and incidence of type 2 diabetes in impaired glucose tolerance: the Finnish Diabetes Prevention Study. Diabetes Care. 2009;32(11):1965–1971. doi: 10.2337/dc08-1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang Y, Mei H, Jiang YR, et al. Relationship between duration of sleep and hypertension in adults: a meta-analysis. J Clin Sleep Med. 2015;11(9):1047–1056. doi: 10.5664/jcsm.5024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kielbasa G, Stolarz-Skrzypek K, Pawlik A, et al. Assessment of sleep disorders among patients with hypertension and coexisting metabolic syndrome. Adv Med Sci. 2016;61(2):261–268. doi: 10.1016/j.advms.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 41.Soltani M, Haytabakhsh MR, Najman JM, et al. Sleepless nights: the effect of socioeconomic status, physical activity, and lifestyle factors on sleep quality in a large cohort of Australian women. Arch Womens Ment Health. 2012;15(4):237–247. doi: 10.1007/s00737-012-0281-3. [DOI] [PubMed] [Google Scholar]
- 42.Lou P, Qin Y, Zhang P, et al. Association of sleep quality and quality of life in type 2 diabetes mellitus: a cross-sectional study in China. Diabetes Res Clin Pract. 2015;107(1):69–76. doi: 10.1016/j.diabres.2014.09.060. [DOI] [PubMed] [Google Scholar]
- 43.Bixler E. Sleep and society: an epidemiological perspective. Sleep Med. 2009;10(Suppl 1):S3–S6. doi: 10.1016/j.sleep.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 44.Grandner MA, Drummond SP. Who are the long sleepers? Towards an understanding of the mortality relationship. Sleep Med Rev. 2007;11(5):341–360. doi: 10.1016/j.smrv.2007.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Youngstedt SD, Kripke DF. Long sleep and mortality: rationale for sleep restriction. Sleep Med Rev. 2004;8(3):159–174. doi: 10.1016/j.smrv.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 46.Aujard F, Dkhissi-Benyahya O, Fournier I, et al. Artificially accelerated aging by shortened photoperiod alters early gene expression (Fos) in the suprachiasmatic nucleus and sulfatoxymelatonin excretion in a small primate, Microcebus murinus. Neuroscience. 2001;105(2):403–412. doi: 10.1016/s0306-4522(01)00202-0. [DOI] [PubMed] [Google Scholar]
- 47.Jackowska M, Hamer M, Carvalho LA, Erusalimsky JD, Butcher L, Steptoe A. Short sleep duration is associated with shorter telomere length in healthy men: findings from the Whitehall II cohort study. PLoS One. 2012;7(10):e47292. doi: 10.1371/journal.pone.0047292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Li Y, Sato Y, Yamaguchi N. Potential biochemical pathways for the relationship between sleep duration and mortality. Sleep Med. 2013;14(1):98–104. doi: 10.1016/j.sleep.2012.08.020. [DOI] [PubMed] [Google Scholar]
- 49.Ayas NT, White DP, Al-Delaimy WK, et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. 2003;26(2):380–384. doi: 10.2337/diacare.26.2.380. [DOI] [PubMed] [Google Scholar]
- 50.Meier-Ewert HK, Ridker PM, Rifai N, et al. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol. 2004;43(4):678–683. doi: 10.1016/j.jacc.2003.07.050. [DOI] [PubMed] [Google Scholar]
- 51.Shearer WT, Reuben JM, Mullington JM, et al. Soluble TNF-alpha receptor 1 and IL-6 plasma levels in humans subjected to the sleep deprivation model of spaceflight. J Allergy Clin Immunol. 2001;107(1):165–170. doi: 10.1067/mai.2001.112270. [DOI] [PubMed] [Google Scholar]
- 52.Richardson MR, Churilla JR. Sleep duration and C-reactive protein in US adults. South Med J. 2017;110(4):314–317. doi: 10.14423/SMJ.0000000000000632. [DOI] [PubMed] [Google Scholar]
- 53.Kronholm E, Laatikainen T, Peltonen M, Sippola R, Partonen T. Self-reported sleep duration, all-cause mortality, cardiovascular mortality and morbidity in Finland. Sleep Med. 2011;12(3):215–221. doi: 10.1016/j.sleep.2010.07.021. [DOI] [PubMed] [Google Scholar]
- 54.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33(5):585–592. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shen X, Wu Y, Zhang D. Nighttime sleep duration, 24-hour sleep duration and risk of all-cause mortality among adults: a meta-analysis of prospective cohort studies. Sci Rep. 2016;6:21480. doi: 10.1038/srep21480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33(5):585–592. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhang P, Lou P, Chang G, et al. [Interaction between quality and duration of sleep on the prevalence of type 2 diabetes] Zhonghua Liu Xing Bing Xue Za Zhi. 2014;35(9):990–993. [PubMed] [Google Scholar]
- 58.Lu K, Chen J, Wu S, Chen J, Hu D. Interaction of sleep duration and sleep quality on hypertension prevalence in adult Chinese males. J Epidemiol. 2015;25(6):415–422. doi: 10.2188/jea.JE20140139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kojima M, Wakai K, Kawamura T, et al. Sleep patterns and total mortality: a 12-year follow-up study in Japan. J Epidemiol. 2000;10(2):87–93. doi: 10.2188/jea.10.87. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.