Abstract
Mobilizing lay health workers (LHWs) to deliver evidence-based treatments (EBTs) is a workforce strategy to address mental health disparities in underserved communities. LHWs can be leveraged to support access to EBTs in a variety of ways, from conducting outreach for EBTs delivered by professional providers to serving as the primary treatment providers. This critical review provides an overview of how LHW-supported or -delivered EBTs have been leveraged in low-, middle-, and high-income countries (HICs). We propose a conceptual model for LHWs to address drivers of service disparities, which relate to the overall supply of the EBTs provided and the demand for these treatments. The review provides illustrative case examples that demonstrate how LHWs have been leveraged globally and domestically to increase access to mental health services. It also discusses challenges and recommendations regarding implementing LHW-supported or -delivered EBTs.
Keywords: lay health workers, mental health disparities, evidence-based treatments
INTRODUCTION
Scaling-up evidence-based treatments (EBTs) has been identified as a priority by institutions such as the World Health Organization (WHO) and the National Institute of Mental Health to address the global mental health burden (Lancet Global Mental Health Group 2007, Collins et al. 2011). EBTs are treatment protocols, such as Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) (Cohen et al. 2006), or techniques, such as exposure therapy for anxiety, that have demonstrated therapeutic change in controlled trials (Kazdin 2008). Although multiple EBTs have been shown to ameliorate symptoms of common mental disorders, such as anxiety, depression, trauma, and disruptive behavior disorders, their public health potential is not being met due to limited accessibility, especially for individuals in low- and middle-income countries (LMICs) and for ethnic and racial minority communities in high-income countries (HICs; Kazdin & Rabbitt 2013, Patel et al. 2011). To increase the reach of EBTs, a public health model of workforce development is required, such as training lay health workers (LHWs) to support access to these treatments (Collins et al. 2011, Kazdin & Rabbitt 2013, van Ginneken et al. 2013).
It has been estimated that annually at least 30% of the population worldwide experiences some sort of mental disorder, with some researchers suggesting that this is an underestimate (Vigo et al. 2016). Of individuals impacted, the vast majority will not receive treatment (Roll et al. 2013). It has been estimated that in LMICs, 72–93% of individuals requiring care are not receiving it (Chisholm et al. 2016, WHO 2008). Racial and ethnic minorities in the United States are less likely to access mental health services compared to non-Hispanic, White individuals (Alegría et al. 2008, Coker et al. 2009, Wells et al. 2001). More than 60% of racial and ethnic minority individuals in the United States requiring mental health services are not receiving treatment (Alegría et al. 2008, Coker et al. 2009, Lee et al. 2014). Immigrant populations are even less likely to access mental health services, with utilization rates that are similar to those found in LMICs (Derr 2015). When underserved communities receive mental health services, they are rarely high quality or based in evidence (Alegría et al. 2008, Dua et al. 2011, Wells et al. 2001). Therefore, a major focus over the past decade has been to implement EBTs domestically and globally in settings that serve the most vulnerable, underserved individuals (Barry & Huskamp 2011, Becker & Kleinman 2013, Lancet Global Mental Health Group 2007).
One of the most pressing challenges to increasing the access of EBTs is a severe workforce shortage of professional mental health providers. Data from the WHO suggest that 239,000 additional full-time providers are needed to address the mental health needs of individuals in 58 LMICs (Bruckner et al. 2011). In the United States, more than 125,000 additional providers are needed just to meet the mental health needs of adults (Konrad et al. 2009), with greater need in low-income and rural settings (Thomas et al. 2009). Furthermore, growing immigrant and refugee populations in the United States create a demographic imperative for a more culturally competent and linguistically diverse mental health workforce (Huang et al. 2004). Linguistically appropriate services are necessary, as individuals who do not speak English proficiently are more likely to prematurely discontinue mental health care even if they access it (Aratani & Cooper 2012, Ohtani et al. 2015). Training LHWs to increase the reach of EBTs in settings with an inadequate workforce may help vulnerable, underserved populations receive quality mental health care (Collins et al. 2011, Kazdin & Rabbitt 2013, Patel et al. 2011, van Ginneken et al. 2013).
Recent policy initiatives, such as the WHO’s Mental Health Gap Action Program, which focuses on scaling-up EBTs for individuals with mental health, neurological, and substance use disorders in LMICs, have led to an increasing body of literature focused on the feasibility and clinical effectiveness of LHW-delivered psychosocial treatment (Dua et al. 2011; WHO 2008, 2015). Recently, two systematic reviews have been conducted to consolidate the findings on LHW-supported or -delivered treatments (Barnett et al. 2017, Singla et al. 2017). The objectives of Singla et al.’s (2017) review were to evaluate the effectiveness of psychological treatments for adults delivered by nonspecialist providers (i.e., LHWs, social workers, and medical providers) in LMICs and to synthesize the implementation processes used in the trials. Singla et al. characterized the types of providers, treatment settings, and the training and supervision received by nonspecialist providers in LMICs. In the 27 studies reviewed, LHWs were the most common provider type, most frequently delivering care in primary care or community settings, such as schools or community meetings. The nature of training and supervision was not consistently reported, and no studies evaluated the competency of the LHWs in delivering the interventions. Findings from this review supported the effectiveness of LHW-delivered EBTs in low-resource settings, with moderate to large intervention effect sizes in client symptom reduction.
Indeed, the majority of research on LHW delivery of EBTs has been conducted in LMICs, which has led to multiple systematic reviews to focus on these settings (Padmanathan & De Silva 2013, Singla et al. 2017, van Ginneken et al. 2013). Increasingly, LHW-supported or -delivered care is being identified as a potential strategy to increase service parity for ethnic and racial minorities in the United States (Acevedo-Polakovich et al. 2013, Kazdin & Rabbitt 2013, Stacciarini et al. 2012). Therefore, we recently conducted a systematic review, which contrasted the nature of LHW involvement in the delivery of mental health interventions in the United States and in LMICs. This review of 43 articles (39 trials) found that LHWs in the United States were less likely to directly administer EBTs or support the delivery of EBTs than LHWs in LMICs (Barnett et al. 2017). As reported by Singla et al., implementation strategies, including LHW training, supervision, and fidelity monitoring, were inconsistently reported in the US and LMIC studies.
Although both of these reviews pointed to the potential clinical effectiveness of LHW-delivered or -supported EBTs, questions still remain about how LHWs can be leveraged in low-resource settings to address mental health disparities between underserved and more adequately served populations. Both reviews found major gaps in research to date related to identifying needed implementation supports (e.g., training, supervision, and fidelity monitoring) to promote the effectiveness of LHW providers. The limited attention to implementation processes makes it challenging to determine the best strategies to replicate and scale-up efforts for LHWs to support or deliver EBTs. Furthermore, although existing research has reported on study outcomes in terms of patient-level clinical effectiveness, few studies have characterized or investigated EBT implementation outcomes for LHW providers, such as fidelity or competence in delivering EBTs and the acceptability of LHW-delivered mental health services for patients and providers (Barnett et al. 2017, Padmanathan & De Silva 2013, Singla et al. 2017).
Goals of Review
In this critical review, we expand on the findings from recent systematic reviews to identify how the field can advance the mobilization of LHWs to improve mental health equity for vulnerable, underserved populations in LMICs and HICs. We propose a conceptual model explaining how LHWs can address the drivers of disparities in access of EBTs for underserved communities. On the basis of health service utilization and health disparities models, these drivers relate to the overall supply of providers trained to deliver EBTs and the recognized demand for these treatments within underserved communities. We present illustrative case examples from both LMICs and low-resource settings in the United States to demonstrate how LHW-delivered or -supported care has been leveraged to address both supply and demand determinants of disparities in care for underserved populations. To address gaps in the literature related to the implementation supports LHWs need to support or deliver EBTs, this review integrates findings from the field of implementation science to identify how to create sustainable systems of care in low-resource settings domestically and globally to make a wide-reaching and long-lasting impact on mental health disparities.
Who Are Lay Health Workers?
LHWs are interventionists without formalized mental health training, who generally are from the same community as the population that they serve (Ayala et al. 2010, Viswanathan et al. 2010). A wide range of terms are used to describe LHWs, including but not limited to promotores, community health workers, lay providers, lay health advisors, indigenous paraprofessionals, peer support specialists, health educators, peer counselors, and natural helpers. For the purpose of this review, LHWs refer to individuals who have not received advanced degrees in a mental health field (e.g., psychiatry, psychology, social work, counseling) or other allied health profession (e.g., nursing, physicians) and who have the role of increasing their community’s access to mental health services.
LHWs’ educational, training, and personal backgrounds differ across studies. LHWs frequently have the equivalent of a high school education (e.g., Barlow et al. 2013, Bolton et al. 2003) or Bachelor’s degrees (e.g., Fayyad et al. 2010), although some studies have included LHWs with lower levels of education (e.g., Nadkarni et al. 2015, Neuner et al. 2008). It has been challenging to identify the qualifications that LHWs need to deliver mental health services, as the selection criteria for identifying LHWs is often under- or unreported in the literature. Some studies have required that LHWs have similar life experiences as the individuals they serve. For example, beyond belonging to the same ethnic or racial group, LHWs may be refugees serving other refugees (Bolton et al. 2014b) or past or present migrant farmers providing care for this population (Hovey et al. 2014). Peer support models require that the LHWs have a history of mental illness similar to the patients they serve (Repper & Carter 2011), and family support models require the LHWs to have children with similar emotional, behavioral, or developmental needs as the parents they serve (Hoagwood et al. 2010, Olin et al. 2014). Finally, LHWs are frequently described as having personal attributes such as being empathetic, motivated to help their communities, and nonjudgmental (e.g., Nadkarni et al. 2015, Neuner et al. 2008).
HOW MIGHT LAY HEALTH WORKERS IMPACT SERVICE DISPARITIES?
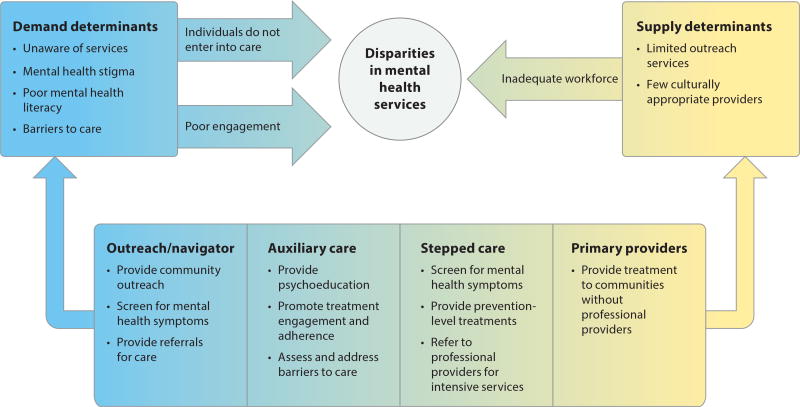
LHWs have the potential to address drivers of disparities, which are associated with both the supply of providers equipped to deliver EBTs and the demand for these interventions within underserved communities. As illustrated in Figure 1, conceptually, both the supply of and demand for mental health EBTs contribute to disparities in care. This conceptual model builds on health service utilization (Andersen 1995, Pescosolido 1991) and health disparities models (Brach & Fraserirector 2000, Kilbourne et al. 2006), which find that a variety of individual, societal, and institutional factors relate to whether an individual accesses care. In Andersen’s (1995) Behavioral Model of Health Services Use, medical utilization is dependent on an individual’s beliefs about care, their need for help, the availability and accessibility of services, and their evaluation of the care they receive. Pescosolido (1991) extended upon this model with the Network-Episode Model, which takes into consideration that patients often are not making individual decisions to enter into mental health care, but instead are informed by the attitudes, beliefs, knowledge and decisions of members of their social networks. Relatedly, models of mental health disparities focus on how an individual’s culture and the provider and organization’s cultural competency impact service utilization (Brach & Fraserirector 2000, Kilbourne et al. 2006).
Figure 1.
Lay health worker models of care can help address supply and demand determinants of disparities in mental health services. Across the continuum, the outreach/navigator model of LHW mobilization predominately seeks to increase the demand for EBTs; whereas with the task-shifting model, LHWs increase the supply of EBTs in the community.
Whether individuals are willing to access available services and if they persist in care once they enroll determine demand for EBTs. Challenges with recruiting and retaining patients in care pose a significant barrier to the viability of implementing and sustaining EBTs in community settings (Hoagwood et al. 2014). The Behavioral Model posits that individual factors, such as health beliefs, values, and social support impact whether an individual is willing to seek care (Andersen 1995). Mental health literacy, negative perceptions of mental health care providers or treatment providers, and culturally based beliefs, preferences, and stigma drive disparities in demand for care (Alegría et al. 2010, Chow et al. 2003, Kilbourne et al. 2006, Nadeem et al. 2007). For example, in the United States, undocumented immigrants may be especially unlikely to seek mental health services due to fear of being reported to authorities and being discriminated against (Philbin et al. 2017). To address these demand determinants of disparities, it has been recommended that providers from similar cultural backgrounds be employed by mental health service organizations and that LHWs may be especially adept at helping patients overcome distrust of health systems, as they share similar life experiences as the clients they serve (Brach & Fraserirector 2000, Katigbak et al. 2015). In relation to Pescosolido’s (1991) Network-Episode Model, as members of the communities they serve, LHWs can be part of a trusted social network that helps individuals link to mental health services and navigate systems of care. In our model, LHWs have the potential to increase demand for services in four specific ways: (a) LHWs can help screen individuals for mental health symptoms using validated tools, such as the Patient Health Questionnaire-9, to identify individuals who would benefit from care and to refer them to services (Patel et al. 2010, Wennerstrom et al. 2011). (b) LHWs can provide information about mental health symptoms and services to address negative beliefs. For example, regarding undocumented immigrants, LHWs may specifically address organizational policies surrounding confidentiality of documentation status so that individuals feel more comfortable seeking care. (c) In the United States, research has demonstrated that racial and ethnic minorities may be more likely to seek mental health services from informal supports, so LHWs may be seen as more acceptable sources of help than professional mental health providers (Derr 2015). (d) In line with the Behavioral Model, structural factors also impact whether individuals seek care, such as having transportation to care and the ability to pay (Andersen 1995, Kilbourne et al. 2006). LHWs can help to address these structural barriers, through case management, through support in addressing barriers, and, potentially, by providing services in more accessible locations in the community.
Regarding provider supply, the Behavioral Model indicates that services need to be available and accessible for individuals to utilize them. As previously mentioned, the global and domestic mental health workforce capable of providing linguistically and culturally appropriate services is inadequate. Given the scarcity of qualified professional providers, mental health services are often reserved for the most clinically severe cases, with little to no services being available for prevention and early intervention services. However, prevention and early intervention services are critical for making a significant impact on the global mental health burden (Collins et al. 2011). Furthermore, when mental health professionals are required to engage in time-consuming tasks that extend beyond providing psychotherapeutic interventions, such as conducting outreach and case management, they may not be able to serve as many individuals.
LHWs can address supply determinants of EBTs in a variety of ways, ranging from supporting the implementation of EBTs delivered by professional providers to providing the EBT services. First, LHWs can be trained to provide auxiliary support to care, such as case management and community engagement strategies, allowing mental health professionals to focus their efforts on being the frontline personnel administering the EBTs (Barnett et al. 2016). Second, accumulating evidence suggests that LHWs can be trained to deliver EBTs effectively in LMICs, increasing the number of providers who can provide these complex, multicomponent psychosocial treatments (Bolton et al. 2003, Murray et al. 2015, Weiss et al. 2015). Given concerns related to LHWs serving clinically complex clients, such as those with a high risk for suicide, it has been recommended that LHWs provide care to individuals with lower levels of psychopathology and that trained professionals such as psychologists or psychiatrists tend to patients with higher need (Patel et al. 2010). This allows LHWs to provide care for individuals who would benefit from prevention and early interventions and trained professionals to dedicate their efforts to patients with higher clinical severity. However, in some settings with very limited specialized mental health professionals, LHWs have been tasked with serving individuals with higher levels of clinical severity (Murray & Jordans 2016).
Lay Health Workers Models of Care
Various models of care related to how LHWs are mobilized in mental health service provision exist. Originally, LHW models of care were developed for the prevention and treatment of physical diseases, such as HIV, hypertension, diabetes, and cancer (Perry et al. 2014). Accumulating evidence suggests that the mobilization of LHWs is a cost-effective strategy to improve a range of health outcomes, including maternal and infant health, management of chronic diseases, and vaccination rates (Lewin et al. 2010, Perry et al. 2014, Rhodes et al. 2007, Viswanathan et al. 2010). Positive outcomes related to health have prompted the inclusion of LHWs in mental health service delivery. However, questions remain about the best roles for LHWs to fulfill in the provision of psychosocial interventions (van Ginneken et al. 2013). On the basis of previous work related to health promotion and mental health services, LHW mobilization can be classified into the following models: (a) Outreach/Navigator, (b) Auxiliary Care, and (d) Task Shifting. Each model addresses the supply and demand determinants of mental health treatment disparities in distinctive ways and may have different benefits and challenges related to implementation.
Outreach/Navigator
One of the most traditional roles for LHWs has been as a “bridge” between the communities they belong to and formal systems of care (Ayala et al. 2010, Eng et al. 1997). LHWs in this model of care are responsible for conducting outreach and care navigation to increase referrals to formal mental health services through a variety of activities, which can include conducting mental health screening, providing referrals to mental health services, or delivering educational presentations about mental health symptoms and services for community members (Honikman et al. 2012, Wennerstrom et al. 2011). The goals of the outreach/navigator model of care include increasing awareness of mental health symptoms and services, decreasing stigma surrounding mental health care, and promoting culturally competent care among formal service providers. Specific to EBTs, the outreach/navigator model can help increase referrals when these treatments are available, but underutilized, in the community. The outreach/navigator Model of LHW mobilization most directly impacts demand determinants of disparities, as the primary intention is to increase the number of individuals who access services.
Auxiliary Care
Another role for LHWs is to support mental health services through case management and promotion of treatment-related behaviors, such as adherence to homework. Specific to EBTs, in this model, patients receive an EBT from a professional mental health provider, and the LHW supports client engagement in the intervention (Barnett et al. 2016). Having LHWs provide separate engagement services has been identified as especially important for children’s mental health services, with the LHWs working directly to increase parent involvement in their child’s care (Rodriguez et al. 2011). Evidence-based engagement strategies include assessment of barriers, accessibility promotion (e.g., coordinating transportation), psychoeducation about services, and appointment reminders (Becker et al. 2015, Lindsey et al. 2014). LHWs can be trained to deliver these engagement strategies (Rodriguez et al. 2011). The auxiliary care model emphasizes both supply and demand determinants of disparities. In this model, LHWs target demand by helping individuals access, engage in, and persist in care. Indirectly, by serving as engagement specialists, LHWs can impact the supply of EBT providers as well, in that professional providers do not have to dedicate time to case management and providing additional engagement strategies (e.g., reminder calls, community-based practice of homework), which could free their time to serve additional patients. Although this team-based approach between LHWs and professional mental health providers has been identified as a potential strategy to improve patient engagement in care and workplace efficiencies, limited research has investigated how to best implement these programs or the clinical effectiveness of the model (Barnett et al. 2017, Hoagwood et al. 2010).
Task-Shifting
Increasingly, LHWs are responsible for providing EBTs using task-shifting models of care. In the task-shifting approach, which was originally used to address physical health concerns (e.g., HIV), health workers who have fewer qualifications complete specific tasks to make more efficient use of human resources (WHO 2007). In the medical field, examples of task shifting include nurses prescribing medications or LHWs providing HIV testing (Zachariah et al. 2009). In mental health, tasking-shifting ranges from less trained individuals delivering components of EBTs in stepped-care models to serving as the sole provider responsible for full treatment delivery.
Stepped-care models
Stepped-cared models of care delivery encourage the provision of the least intensive treatment that is available, with care becoming more intensive as needed (Araya et al. 2006, Bower & Gilbody 2005). Intensity of care is measured by both the individual’s need (e.g., if they would benefit from brief prevention services or need a higher level of care) and the amount of specialist time that is required (Bower & Gilbody 2005). In traditional stepped-care models, LHWs provide lower levels of care to patients with less intensive needs, whereas mental health professionals provide a higher level of care to patients with more severe symptomatology (e.g., Araya et al. 2006, Patel et al. 2010). Stepped-care models have the potential to increase the supply of EBTs and the demand for services. By providing prevention and early intervention services in stepped-care models, LHWs increase the supply of services to capture a wider population than would previously have been seen. Demand also increases, as stepped-care models frequently include the implementation of screening procedures to identify and refer individuals who would benefit from mental health interventions as delivered by either an LHW or professional provider.
Primary providers
In certain under-resourced settings, LHWs may be the only service providers available and can be the primary providers of EBTs. The majority of EBTs were developed in high-resource settings, with the intention that trained mental health professionals would deliver them; however, increasing evidence demonstrates that EBTs delivered by LHWs in LMICs can lead to positive clinical outcomes (Singla et al. 2017). When LHWs are the primary providers of EBTs, they are most directly impacting the supply of care, although there may be an indirect link to demand as individuals may feel more comfortable and less stigmatized seeking care from members of their own communities.
HOW ARE LAY HEALTH WORKERS LEVERAGED IN LOW- AND MIDDLE-INCOME COUNTRY SETTINGS?
Given differences in regulations and available workforces, LHW mobilization is likely to differ in developed countries from that of LMICs. In LMICs, LHWs are typically deployed through task-shifting models given the dearth of a trained mental health workforce in these countries (Singla et al. 2017, van Ginneken et al. 2013). Prompted by two WHO initiatives launched in 2008, significant efforts have focused on scaling-up and evaluating the effectiveness of LHW-delivered EBTs in LMICs (Barbui et al. 2010, Dua et al. 2011, WHO 2008). These initiatives made explicit recommendations regarding the EBTs that should be used to address mental health disorders, such as cognitive-behavioral therapy or interpersonal therapy for depression, and parent management training for childhood behavior disorders. LHWs have been involved in delivering EBTs that target depression, anxiety, trauma, substance use, and disruptive behaviors in LMICs throughout Africa, South Asia, and the Middle East.
Stepped-Care in Low- and Middle-Income Countries
The MANAS (MANashanti Sudhar Shodh, meaning “project to promote mental health” in the Konkani language) trial conducted by Patel et al. (2010) is an impressive case example of how stepped-care interventions can improve the supply of and demand for EBTs in LMICs. This large-scale clustered randomized controlled trial tested the effectiveness of a stepped-care intervention for common mental disorders (e.g., depression, anxiety) compared to usual care in Goa, India. In the MANAS intervention, trained LHWs worked collaboratively with primary care physicians and mental health specialists within public and private primary health care settings. LHWs, who had completed a two-month training course, were responsible for screening patients for common mental disorders (e.g., anxiety and depression) and providing psychoeducation to patients regarding the impact of these disorders on interpersonal relationships and the importance of sharing emotional symptoms with doctors. LHWs also provided basic interventions for symptom reduction, such as breathing exercises to manage anxiety, adherence support for medication management, and referrals to external agencies as needed. LHWs would refer patients with moderate or severe symptomatology to the primary care physician for antidepressant medication. Furthermore, LHWs could provide at least six sessions of interpersonal psychotherapy (an EBT for depression) to patients with moderate to severe common mental disorders, either in conjunction with medication or as an alternative treatment option. Consultation from a visiting psychiatrist was available for individuals who were unresponsive to these treatment options, had high risk of attempting suicide, or had additional clinical complexities, including comorbidities with other mental, substance use, or physical disorders. A psychiatrist also provided monthly supervision to the LHWs and doctors, and LHWs also participated in a monthly peer supervision group. A randomized cluster trial compared the MANAS intervention to usual care in 24 primary care facilities (12 public and 12 private), with 2,796 participants enrolled in the trial. In public facilities, the MANAS intervention demonstrated strong effects, including a 30% decrease in individuals who met diagnostic criteria for common mental disorders and a 36% decrease in suicide attempts. Furthermore, individuals who received the MANAS intervention showed better functioning, including missing fewer days of work.
Interestingly, participants enrolled in private settings did not show any of these intervention effects, with participants served in the usual care facilities showing equal improvement as those in the intervention facilities. The authors attributed these differences in outcomes in private facilities to challenges they had in recruiting physicians from these settings, making it possible that a nonrepresentative group of highly motivated physicians participated in the trial. The authors hypothesized that the physicians who agreed to participate in the MANAS trial already were committed to providing client-centered care to address mental health concerns, negating the impact of the LHW component of care. These hypotheses were supported by qualitative interviews with 115 patients and 119 providers after the trial concluded. In interviews, physicians in private facilities in the usual care arm of the trial reported that they regularly provided psychoeducation, advice on life style change and problem solving, and referrals to specialists, which were similar care components to those delivered by LHWs in the intervention arm (Pereira et al. 2011). These findings were consistent with follow-up qualitative interviews with patients. Patients in public facilities identified the LHWs as playing an instrumental role in their care and symptom improvement and noted more challenges in communicating with their doctors. Patients in private facilities, however, attributed most of their symptom improvement to antidepressants rather than the LHW-delivered interventions and were more likely to express satisfaction with their patient-physician relationships (Shinde et al. 2013). It is promising for disparity reduction that the LHW component of MANAS might have helped public facilities obtain similarly positive outcomes as private facilities.
In the MANAS intervention, LHWs directly targeted the supply and demand for mental health services. The supply of EBTs for anxiety and depression was dramatically increased, because LHWs were able to provide low-intensity interventions to a large percentage of patients with mild to moderate symptomatology. Demand for mental health services was also increased, as the screening procedure and referral process allowed LHWs to identify more individuals with common mental health disorders and they facilitated conversations with patients about how to seek additional services, including how to have conversations about symptoms with their doctors. However, it is noteworthy that LHWs reported significant barriers to delivering interpersonal psychotherapy, because patients were not able to attend the required six sessions and they were skeptical of its potential benefits, preferring medication (Pereira et al. 2011). Therefore, demand for specific types of EBTs continued to be a problem even within this stepped-care model. The MANAS trial indicates the potential for LHWs to improve mental health care for individuals in low-resource primary health care settings; however, future research still needs to investigate how to increase client engagement in multisession EBTs.
Lay Health Workers as Primary Providers in Low- and Middle-Income Countries
Beyond their involvement in stepped-care models, LHWs have also been leveraged as the primary providers of EBTs in LMICs. Randomized controlled trials have demonstrated that LHWs are clinically effective in the delivery of several empirically tested protocols, including TF-CBT for treating traumatic stress in children (Murray et al. 2015), Interpersonal Psychotherapy for depression (Bolton et al. 2003, Petersen et al. 2012), Behavioral Activation for depression (Bolton et al. 2014a), and Cognitive Processing Therapy for traumatic stress (Bolton et al. 2014a, Weiss et al. 2015). Given that these protocols were developed to be delivered by mental health professionals, it is promising that LHW-delivered EBTs have been shown to lead to significant reductions in clinical symptoms. Interventions informed by EBTs, such as parent management training for the treatment of disruptive behavior disorders (Puffer et al. 2015) and cognitive-behavioral therapy (Papas et al. 2011), have also been effective when delivered by LHWs.
The majority of research on LHW-delivered EBTs has been on highly structured protocols, which were developed to target single disorders. The structure of these interventions, such as having prescribed session content, ordering, and treatment length, can be beneficial for LHWs, who have little mental health training. However, given the range of clinical disorders that are present in LMICs, researchers have recognized the value in developing transdiagnostic treatments that can be delivered by LHWs (Murray et al. 2014a, Singla et al. 2017). Transdiagnostic interventions that use common elements from EBTs are increasingly being used in the United States as a way to improve the quality of community mental health care, especially given high rates of comorbidity of diagnoses (Chorpita et al. 2005, 2017; Weisz et al. 2012). In these interventions, decision rules guide how treatment elements are chosen and sequenced, allowing for flexibility to address comorbid presenting problems (Chorpita & Daleiden 2009). Research on common elements treatments conducted in the United States informed the development of the Common Elements Treatment Approach (CETA), which was designed to address comorbid presentations of trauma, anxiety, and depression symptoms in trauma survivors, while at the same time simplifying decision-making tools to facilitate training for LHWs (Murray et al. 2014a). CETA includes a parsimonious list of essential elements from EBTs (e.g., cognitive restructuring, in vivo exposure) and steps sheets that provide guidance on delivering the intervention, including sample wording that the LHWs can use. To simplify the decision-making process, LHWs were trained on how to use validated measures and information from the client to identify the primary problem, and then they were provided with default sequences of the elements they should deliver. The first trial of CETA took place on the Thailand–Myanamar (Burma) border with Burmese refugees, who had high trauma exposure related to decades of military rule and systematic violence. Participants (n = 347) were randomized to CETA or a waitlist control, with improved outcomes for those in the intervention condition for depression, post-traumatic stress, and anxiety symptoms (Bolton et al. 2014b). CETA was also found to be effective in a trial conducted in Southern Iraq with survivors of torture and militant attacks (Weiss et al. 2015). CETA represents a promising approach to address a wider range of mental disorders than typically can be done with a single EBT, which may be especially important in low-resource settings with a limited number of providers (Murray & Jordans 2016, Singla et al. 2017).
One must consider the level of implementation support that was used in the trials on CETA that may have contributed to the effectiveness of the intervention. In these trials, local supervisors were trained simultaneously with the LHWs in CETA, along with supervision strategies. The local supervisors, who were responsible for overseeing the LHWs’ clinical care, received weekly phone consultations with the US-based CETA trainers throughout the studies. These weekly calls included ongoing training for the supervisors and fidelity monitoring for every case. US trainers were able to provide support for implementing the treatment components and decisions regarding the ordering of these components.
Summary of Lay Health Worker Involvement in Low- and Middle-Income Countries
Accumulating evidence regarding the clinical effectiveness of LHW-delivered EBTs in LMICs is encouraging and suggests that task shifting is a potential strategy to reduce the global mental health burden, especially in low-resource settings (Bolton et al. 2003, 2014a; Murray et al. 2015; Patel et al. 2011; Petersen et al. 2012; Singla et al. 2017; Weiss et al. 2015). However, challenges remain in implementing EBTs in these settings before a large-scale impact can be made by these efforts in LMICs. It is still not clear how to successfully scale-up and sustain EBT implementation efforts in LMICs, with the majority of efforts to date including intensive training and ongoing consultation with the research teams from HICs (Murray & Jordans 2016). It is not clear if EBTs continue to be used after studies are completed, especially given concerns with LHW attrition. Turnover is a consistent challenge to sustaining EBTs with professional mental health providers (Stirman et al. 2012); however, this challenge can be even greater with LHWs in LMICs because they do not have formal job positions and may not have the opportunity to use their skills with EBTs after a project is completed (Murray et al. 2014b). Strategies for building and maintaining local capacity to continue these efforts after a study has been completed are critical for addressing global mental health disparities in low-resource settings.
HOW ARE LAY HEALTH WORKERS LEVERAGED IN THE UNITED STATES?
HICs with more resources, such as the United States, have a larger professional mental health workforce to deliver EBTs. However, disparities still plague issues of access to and quality of mental health services in the community settings that are most likely to serve low-income, racial and ethnic minority individuals (Alegría et al. 2008, Wells et al. 2001). Beyond the availability of EBTs, challenges with engagement in care exist. For example, when evidence-based parent training programs are available, less than half of eligible families enroll in them, with lower rates of enrollment for African American and Latino families compared to Caucasian families (Baker et al. 2011). Beyond enrollment, poor attendance and high rates of attrition limit the number of patients who receive an appropriate dosage of an EBT. The consequences of poor participation in EBTs are significant; individuals do not experience improvements in clinical symptoms, public health benefits are diluted, and failed efforts to recruit and retain patients are costly for providers (Hoagwood et al. 2014). In settings with a professional mental health workforce to provide EBTs, LHWs might play an especially important role in increasing demand for such services.
Outreach/Navigation in the United States
One example of how LHWs can increase demand for EBTs through outreach and navigation services occurred in New Orleans in the aftermath of Hurricane Katrina. LHWs were integrated into collaborative care services in New Orleans, as a strategy to address the disaster-related infrastructure limitations to reaching the number of individuals with mental health needs (Wennerstrom et al. 2011). This effort resulted from a community-based participatory research (CBPR) approach, which has been recommended for addressing health disparities (Minkler 2010), to develop the REACH NOLA partnership and Mental Health Infrastructure and Training Project. The project trained providers, including psychiatrists, primary care providers, case managers, and LHWs, in a collaborative care for depression model, which included quality improvement methods, such as care coordination between providers. Collaborative care in primary care settings, which integrates services from primary care providers, patient care managers, and mental health specialists, has been shown to be an effective approach to treat depression, especially for low-income, ethnic and racial minority communities (Angstman et al. 2015). As opposed to training LHWs to provide EBTs as they did in the MANAS collaborative care model in India (Patel et al. 2010), in this setting, mental health providers were trained in EBTs, whereas LHWs were trained in conducting mental health outreach. For example, LHWs were trained to utilize evidence-based screening tools in nonclinical settings in an effort to identify individuals with elevated symptoms of depression and to provide appropriate referrals for treatment. A qualitative evaluation of the training programs indicated that LHWs held positive views of the training and used screening tools in the community (Wennerstrom et al. 2011). However, to date, clinical and service outcomes of these efforts with outreach and navigation have not been evaluated, limiting the conclusions regarding its effectiveness in recruiting patients in care and improving symptoms of depression.
Lay Health Workers as Auxiliary Support and Primary Providers in the United States
One area of LHW-delivered care that has received more attention in the United States is the delivery of home-based parenting interventions. Although a large-scale, randomized control trial of nurse- or paraprofessional-delivered pre- and postnatal home visits demonstrated better outcomes for nurse-delivered care (Olds et al. 2002), efforts have been made to train LHWs to support or provide these services in communities with documented health disparities. To capitalize on the specialized training of nurses to address health and mental health concerns, Roman et al. (2007) developed a prenatal intervention to address mental health and stress for low-income women that was delivered by nurse-LHW teams. LHWs provided auxiliary support, including addressing language and cultural barriers to care, providing peer role modeling for how to address chronic stressors, promoting continued engagement in services, and increasing access to services. In a randomized control trial, mothers (n = 266) who received the nurse-LHW team intervention demonstrated better participation in the intervention compared to the comparison group (n = 266), which received standard community care (Roman et al. 2007). Furthermore, women who received the nurse-LHW team intervention had significantly fewer depressive symptoms compared to women in the comparison condition (Roman et al. 2009). These engagement and clinical outcomes support the potential of LHWs supporting services in conjunction with a trained professional.
LHWs have also been leveraged as the primary providers in the Family Spirit home-visiting intervention program, which was developed to improve parenting and risk behaviors in American Indian teen mothers. Family Spirit was developed using a CBPR approach, in which tribal stakeholders identified family-based approaches to promote effective parenting as a culturally preferred strategy to prevent behavior problems in youth. Community stakeholder feedback was used to determine the intervention content and the importance of the program being delivered by Native LHWs, who spoke English and Native languages (Mullany et al. 2012). The Family Spirit intervention includes 43 lessons, which address parenting skills across infancy and early childhood, maternal drug abuse prevention, and maternal life skills and psychosocial well-being. LHWs were provided with visual table-top flipbooks with lesson plans to use during sessions. A randomized control trial, which compared Family Spirit to optimized standard care, demonstrated the effectiveness of the LHW-delivered intervention, with mothers in the intervention group demonstrating improved outcomes for the parents and infants (Barlow et al. 2013, 2015).
Summary of Lay Health Worker Involvement in the United States
Preliminary evidence is demonstrating that LHW-delivered or -supported mental health care is feasible in the United States (Barlow et al. 2013, 2015; Roman et al. 2009). However, in many ways, the research conducted in the United States on LHW-delivered or -supported EBTs dramatically lags behind efforts in LMICs (Barnett et al. 2017). First, LHWs are more likely to be involved in delivering novel, community-developed interventions in the United States compared to EBTs. Community informed interventions could have significant benefits, as partnership with underrepresented groups in developing interventions has been identified as an important strategy to improving mental health disparities (Minkler 2010). At the same time, accumulating research promotes the effectiveness of EBTs with ethnic and racial minority populations (Miranda et al. 2005), which supports efforts to increase access to these services through LHW models of care. In the investigations of LHW-delivered mental health services in the United States that do exist, many have small samples and/or do not include a comparison group (Han et al. 2012, Hovey et al. 2014, Magaña et al. 2015, Moore et al. 2016). Although these preliminary, small studies are needed to develop an evidence base, methodological limitations make it challenging to draw conclusions about the effectiveness of LHW-delivered care, especially for interventions that target presenting problems other than parenting. It is possible that LHWs have not been deployed in the delivery of EBTs in the United States because there is a perception that there is an adequate professional mental health workforce to deliver these treatments. However, many communities that have the highest level of need, such as immigrants and refugees who are not proficient in English, do not have mental health providers who can meet their needs (Huang et al. 2004). Therefore, it is worthwhile to identify strategies to support LHW-delivered EBTs for these most underserved communities in HICs. Finally, although leveraging LHWs to support EBT delivery through outreach or auxiliary models of care holds promise for addressing mental health disparities, especially related to accessing services, very limited empirical support has evaluated these models.
TRAINING AND SUPERVISING LAY HEALTH WORKERS
For LHWs to effectively support or deliver EBTs, it is critically important to understand their training and supervision needs. Unfortunately, training and supervision protocols for LHW have not been consistently reported in the literature, limiting our ability to draw conclusions about the amount of training or ongoing support that LHWs need to implement EBTs with fidelity. When training protocols have been described, they range in their intensity from three to five days (Fayyad et al. 2010, Magaña et al. 2015, Petersen et al. 2012) to two months of training (Patel et al. 2010). The literature describes a range of training activities including didactic presentations, role-playing, observing professionals deliver the intervention, and proficiency testing. Given the limited descriptions provided and range of training activities, it is not possible to identify the most effective strategies to train LHWs in implementing EBTs or the level of training and continuing support that they need.
Many lessons from the field of dissemination and implementation research are likely to apply to LHWs, even though the majority of this research has focused on the training and supervising of Master’s-level clinicians. Unfortunately, efforts to transport EBTs into community settings with professional mental health workforces have not consistently led to improved client outcomes beyond the delivery of usual care services, suggesting challenges in EBT implementation even with specialized providers (Barrington et al. 2005, Weisz et al. 2013). One potential reason for the diminished effectives of EBTs in community settings could be related to poor fidelity in delivering the EBT protocols (Dusenbury et al. 2003, McHugo et al. 2007). Even professional mental health providers require ongoing support to deliver EBTs with competence (Beidas & Kendall 2010, Herschell et al. 2010). Given these challenges with a specialized workforce, it is critical to identify the level of implementation support that LHWs would need to effectively support or provide EBTs. For professional mental health providers, it has been found that training outcomes improve when there are opportunities to practice and receive feedback on skill use, as opposed to didactic presentations or discussion (Beidas & Kendall 2010; Bearman et al. 2013, 2017). In fact, the importance of keeping didactic training minimal and responsive to the educational level of LHWs has been emphasized, suggesting that these types of activities may be especially important for this segment of the workforce (Acevedo-Polakovich et al. 2013, Calzada et al. 2005, Murray et al. 2011). Unfortunately, very limited research has evaluated the competency of LHWs following training or consultation programs (Barnett et al. 2016, Singla et al. 2017). Ongoing supervision is also critically important to implement EBTs with fidelity (Beidas & Kendall 2010, Herschell et al. 2010). For LHWs, supervision is also needed to address clinical issues that are beyond the scope of EBT delivery, such as risk of harm to oneself and others. As LHWs do not have specialized clinical training in managing these risks, it is likely that the supervisor or another professional provider will need to intervene in these situations.
Additionally, given that many LHWs have experienced the same stressors as the individuals they serve, such as trauma histories and poverty, they may be especially at risk for becoming emotionally exhausted or for experiencing secondary trauma by providing clinical services (Jain 2010). Supervision can help to reduce emotional exhaustion when delivering EBTs (Aarons et al. 2009). When training and supervising LHWs, it is critical to anticipate and address experiences of burnout, stress, and symptoms of secondary trauma that are related to EBT delivery and support (Jain 2010). It may even be valuable to train LHWs in relaxation strategies, such as mindfulness, to decrease stress. In a small study, 26 LHWs who worked in low-income, urban settings in the United States completed six weeks of mindfulness-based skills training and had significant improvements in their sleep quality, stress levels, and emotional exhaustion (Jacobs et al. 2017). These findings suggest that LHWs may improve mental health and workplace functioning if they are specifically equipped with strategies to address stress.
Ethical Considerations of Lay Health Worker–Delivered Evidence-Based Treatments
As LHWs are likely to have overlapping roles with members of their own community, one must consider the potential ethical concerns related to therapeutic boundaries, consent for care, and patient confidentiality that might arise in LHW-supported or -delivered services (Jain 2010, Terpstra et al. 2011). In fact, the same traits that are strengths for LHWs in promoting engagement in EBTs (e.g., having similar lived experiences and being seen as more trustworthy than professional providers) can place them at greater risk for breaking confidentiality or for having multiple roles with the patients. Directly addressing these ethical concerns in training and supervision can help LHWs provide ethical care. In a qualitative study of an LHW training program to conduct outreach for depression treatment, LHWs identified training in confidentiality to be a valuable component of the training (Wennerstrom et al. 2011). Efforts have been made to train Latino LHWs in ethics surrounding research design (e.g., informed consent, confidentiality), which may inform training protocols that can be used to help LHWs understand these ethical concerns in clinical care (Nebeker & López-Arenas 2016). Furthermore, ongoing supervision by trained professionals is important in regards to ethical principles regarding competence. Specifically, supervision is necessary to ensure that LHWs are delivering or supporting EBTs with fidelity.
FUTURE DIRECTIONS FOR RESEARCH AND PRACTICE WITH LAY HEALTH WORKERS
Increasingly, LHWs are being leveraged as part of the mental health workforce to address disparities in the supply of and demand for EBTs in LMICs and HICs. In fact, a systematic review of research on LHW-delivered psychosocial interventions conducted between 1990 and 2015 found that more than 70% of the 43 articles were published since 2010, suggesting that LHW-delivered or -supported mental health interventions is a current and growing strategy to reach vulnerable populations (Barnett et al. 2017). Although accumulating evidence suggests that LHWs can effectively deliver EBTs that target traumatic stress, depression, anxiety, and disruptive behavior disorders, questions remain about the best strategies to mobilize this workforce in HICs and LMICs.
As research on LHW mobilization in EBT delivery has predominately been conducted in LMICs, it is still not clear which roles LHWs should have in HICs to address disparities in care. Even though LHWs have effectively delivered EBTs in LMICs (Bolton et al. 2003, 2014a;Murray et al. 2015; Patel et al. 2011; Petersen et al. 2012; Singla et al. 2017; Weiss et al. 2015), it is likely that they will fulfill other roles in HICs for a variety of reasons. First, HICs, as with the United States, have more professional mental health providers in comparison to LMICs (Bruckner et al. 2011, Saraceno et al. 2007, van Ginneken et al. 2013), which may limit the need for LHWs to be the primary providers of EBTs. However, given the dearth of providers who can provide culturally competent and linguistically appropriate care, it is still possible that LHWs need to be deployed in this capacity. Regulations from insurance providers and organizations that oversee the implementation of different EBT protocols are also likely to limit the type of providers who can provide these services in HICs. For example, LHWs have been leveraged as the primary providers of TF-CBT, an EBT to treat children who have been exposed to trauma, in Zambia (Murray et al. 2013, 2015). However, in the United States, certification requirements include that providers have a Master’s degree in a mental health discipline and professional licensure (see, e.g., https://tfcbt.org/tf-cbt-certification-criteria/TFCBT), which limits the workforce that is trained to deliver this intervention. Therefore, it still needs to be determined if and how LHWs should deliver EBTs in the United States and other HICs. LHW mobilization in high-resource settings might focus more on ways to increase the numbers of individuals who can access EBTs through reaching prevention populations or increasing access to professional delivered services. However, as very limited research has focused on these outreach and auxiliary roles in relation to EBT delivery in LMICs or HICs, further investigation is needed to evaluate whether these models improve service parity and clinical outcomes.
Another important area of future research is to determine the comparative effectiveness of LHW-delivered or -supported EBTs in comparison to services delivered solely by mental health professionals. Although early research found paraprofessionals to be as effective as professionals in helping activities (Durlak 1979, Hattie et al. 1984), this research needs to be extended to address clinical outcomes with EBTs. Furthermore, one must consider the costs associated with training and supporting LHWs in EBT delivery, in comparison to mental health professionals. If LHWs require substantially more time and resources to be able to deliver EBTs to fidelity, the benefits of leveraging them in these roles may not be necessary in settings with an adequate professional workforce. Similarly, if LHW-supported care using an outreach or auxiliary model is not a cost-effective way to improve service engagement, it is unlikely to be adopted in community settings. However, if LHWs are able to increase productivity in community mental health settings by addressing systemic engagement issues such as poor attendance and attrition, then these models could be used to support clinical and implementation outcomes. Therefore, further research on these models is warranted.
Finally, significant questions remain about how to successfully scale-up efforts to mobilize LHWs in the implementation of EBTs, with regard to their training and supervision needs. Many of the successful efforts of LHW-delivered EBTs in LMICs have included high-intensity implementation support (e.g., frequent consultation with treatment developers), which may have aided in the effectiveness of services. However, this is unlikely to lead to long-term sustainability of LHW-delivered interventions (Murray & Jordans 2016). Sustainment of EBTs in community settings is understudied and challenging even in HICs (Stirman et al. 2012). It is exponentially more challenging to sustain EBTs in LMICs, as they have fewer resources, such as local trainers. One innovative strategy has been training local supervisors to oversee the LHWs in LMICs (Murray et al. 2011). In this apprenticeship model, expert trainers select local supervisors, and through modeling, involvement in the training, and coaching, they help the supervisors gain skills in overseeing the LHWs in EBT delivery. Trainers provide ongoing consultation via video conferencing with the supervisors about how to continue to promote treatment fidelity through supervisory activities such as role-plays. Further research is needed to evaluate how this local supervisor model impacts the potential for sustainment over time in these low-resource settings.
CONCLUSIONS
On the basis of this review, the following recommendations can be made for future efforts involving LHW-delivered or -supported EBTs. First, to make sure the model meets the needs of the local context, a community-partnered approach should be employed when developing and testing LHW mobilization in EBT delivery. A community-partnered approach, such as CBPR, has been used to implement EBTs with LHWs (e.g., Murray et al. 2013, Papas et al. 2010). These partnerships are critical to make sure that the intervention meets the local culture and context and increases stakeholder buy-in. Moreover, a community-partnered approach has been shown to improve participation in staff training in evidence-based services (Chung et al. 2015). The community-partnered approach can be used to address the second recommendation, which is to determine if supply or demand determinants are the major drivers of service disparities in the community. By determining if LHWs are needed to address the supply of EBTs, the demand for these services, or a combination of the supply and demand, it can be determined which model of LHW mobilization is most appropriate. Finally, future research on LHW-delivered and -supported EBTs should address areas that have been underreported in the current literature. Studies need to consistently report the selection criteria for LHWs and the training and supervision that LHWs receive. By providing these details, other researchers and systems of care may be able to better replicate these efforts and mobilize LHWs to address service disparities. In summary, developing an LHW workforce may serve as an important strategy to address disparities for underserved communities in LMICs and HICs, but further research is needed to understand the best roles for them with regard to the delivery of EBTs and the implementation supports they need to successfully fulfill these roles.
SUMMARY POINTS.
Accumulating evidences suggests that LHW-delivered EBTs can lead to clinical improvements for individuals in low-resource settings.
Mobilizing LHWs to support or deliver EBTs is a potential workforce solution to reducing the global mental health burden and decreasing mental health disparities for underserved communities.
LHWs can target supply and demand determinants of mental health disparities regarding access to EBTs.
Different models of LHW mobilization can be used to improve access to EBTs, including roles related to outreach and navigation, auxiliary engagement services, and providing the treatments.
LHWs have predominately been tasked with delivering EBTs in LMICs, but increasingly LHWs are being seen as a strategy to promote service equity for racial and ethnic minority individuals in HICs. Lessons from the successful deployment of LHWs in LMICs may be applicable in HICs.
FUTURE ISSUES.
Future research with LHWs must identify the implementation strategies that are necessary for LHWs to competently deliver EBTs and produce clinically effective outcomes.
The most appropriate roles for LHWs to support and deliver EBTs should be identified for LMICs and HICs, in relation to the policies and workforce demands of the different settings.
Further investigations into how different models of LHW mobilization (e.g., Outreach/Navigator, Auxiliary Care, Task Shifting) compare to the effectiveness of EBTs delivered solely by mental health professionals are needed.
Strategies to efficiently scale-up and sustain efforts to mobilize LHWs in EBT implementation must be established.
Acknowledgments
Our review was supported by a National Institute of Mental Health grant K01MH110608 to M.L.B., with A.S.L. and J.M. being primary mentors on the project.
Glossary
- Evidence-based treatments (EBTs)
treatment protocols or techniques that have been shown to lead to therapeutic changes in mental health symptoms and/or functioning in controlled trials
- Low- and middle-income countries (LMICs)
the World Bank’s classification of countries (as per July 2016) as low-income (Gross National Income per capita of $1,005 or less) and middle-income ($1,006 to $12,235)
- High-income countries (HICs)
high-income countries have a Gross National Income per capita above $12,236
- Lay health workers (LHWs)
individuals who do not have a professional degree or training and typically come from the communities that they serve
Footnotes
DISCLOSURE STATEMENT
The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
LITERATURE CITED
- Aarons GA, Fettes DL, Flores LE, Sommerfeld DH. Evidence-based practice implementation and staff emotional exhaustion in children’s services. Behav. Res. Ther. 2009;47:954–60. doi: 10.1016/j.brat.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acevedo-Polakovich ID, Niec LN, Barnett ML, Bell KM. Incorporating natural helpers to address service disparities for young children with conduct problems. Child. Youth Serv. Rev. 2013;35:1463–67. doi: 10.1016/j.childyouth.2013.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Chatterji P, Wells K, Cao Z, Chen CN, et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatr. Serv. 2008;59:1264–72. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Vallas M, Pumariega AJ. Racial and ethnic disparities in pediatric mental health. Child Adol. Psych. Cl. 2010;19:759–74. doi: 10.1016/j.chc.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- Angstman KB, Phelan S, Myszkowski MR, Schak KM, DeJesus RS, et al. Minority primary care patients with depression: Outcome disparities improve with collaborative care management. Med. Care. 2015;53:32–37. doi: 10.1097/MLR.0000000000000280. [DOI] [PubMed] [Google Scholar]
- Aratani Y, Cooper JL. Racial and ethnic disparities in the continuation of community-based children’s mental health services. J. Behav. Health Serv. R. 2012;39:116–29. doi: 10.1007/s11414-011-9261-z. [DOI] [PubMed] [Google Scholar]
- Araya R, Flynn T, Rojas G, Fritsch R, Simon G. Cost-effectiveness of a primary care treatment program for depression in low-income women in Santiago, Chile. Am. J. Psychiatry. 2006;163:1379–87. doi: 10.1176/ajp.2006.163.8.1379. [DOI] [PubMed] [Google Scholar]
- Ayala GX, Vaz L, Earp JA, Elder JP, Cherrington A. Outcome effectiveness of the lay health advisor model among Latinos in the United States: an examination by role. Health Educ. Res. 2010;25:815–40. doi: 10.1093/her/cyq035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker CN, Arnold DH, Meagher S. Enrollment and attendance in a parent training prevention program for conduct problems. Prev. Sci. 2011;12:126–38. doi: 10.1007/s11121-010-0187-0. [DOI] [PubMed] [Google Scholar]
- Barbui C, Dua T, van Ommeren M, Yasamy MT, Fleischmann A, et al. Challenges in developing evidence-based recommendations using the GRADE approach: the case of mental, neurological, and substance use disorders. PLOS Med. 2010;7:e1000322. doi: 10.1371/journal.pmed.1000322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow A, Mullany B, Neault N, Compton S, Carter A, et al. Effect of a paraprofessional home-visiting intervention on American Indian teen mothers’ and infants’ behavioral risks: a randomized controlled trial. Am. J. Psychiatry. 2013;170:83–93. doi: 10.1176/appi.ajp.2012.12010121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow A, Mullany B, Neault N, Goklish N, Billy T, et al. Paraprofessional-delivered home-visiting intervention for American Indian teen mothers and children: 3-year outcomes from a randomized controlled trial. Am. J. Psychiatry. 2015;172:154–62. doi: 10.1176/appi.ajp.2014.14030332. [DOI] [PubMed] [Google Scholar]
- Barnett ML, Gonzalez A, Miranda J, Chavira DA, Lau AS. Mobilizing community health workers to address mental health disparities for underserved populations: a systematic review. Adm. Policy Ment. Hlth. 2017 doi: 10.1007/s10488-017-0815-0. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett ML, Jent JF, Davis EM, White J, Callejas LM, et al. The development and evaluation of a natural helper training program to increase the engagement of urban, Hispanic families in parent-child interaction therapy. Child. Youth Serv. Rev. 2016;65:17–25. [Google Scholar]
- Barrington J, Prior M, Richardson M, Allen K. Effectiveness of CBT versus standard treatment for childhood anxiety disorders in a community clinic setting. Behav. Change. 2005;22:29–43. [Google Scholar]
- Barry CL, Huskamp HA. Moving beyond parity—mental health and addiction care under the ACA. New Eng. J. Med. 2011;36:973–75. doi: 10.1056/NEJMp1108649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bearman SK, Schneiderman RL, Zoloth E. Building an evidence base for effective supervision practices: an analogue experiment of supervision to increase EBT fidelity. Adm. Policy Ment. Hlth. 2017;44:293–307. doi: 10.1007/s10488-016-0723-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bearman SK, Weisz JR, Chorpita BF, Hoagwood K, Ward A, et al. More practice, less preach? The role of supervision processes and therapist characteristics in EBP implementation. Adm. Policy Ment. Hlth. 2013;40:518–29. doi: 10.1007/s10488-013-0485-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker AE, Kleinman A. Mental health and the global agenda. New Eng. J. Med. 2013;369:66–73. doi: 10.1056/NEJMra1110827. [DOI] [PubMed] [Google Scholar]
- Becker KD, Lee BR, Daleiden EL, Lindsey M, Brandt NE, Chorpita BF. The common elements of engagement in children’s mental health services: Which elements for which outcomes? J. Clin. Child Adolesc. Psychol. 2015;44:30–43. doi: 10.1080/15374416.2013.814543. [DOI] [PubMed] [Google Scholar]
- Beidas RS, Kendall PC. Training therapists in evidence-based practice: a critical review of studies from a systems-contextual perspective. Clin. Psychol. 2010;17:1–30. doi: 10.1111/j.1468-2850.2009.01187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton P, Bass J, Neugebauer R, Verdeli H, Clougherty KF, et al. Group interpersonal psychotherapy for depression in rural Uganda: a randomized controlled trial. J. Am. Med. Assoc. 2003;289:3117–24. doi: 10.1001/jama.289.23.3117. [DOI] [PubMed] [Google Scholar]
- Bolton P, Bass JK, Zangana GAS, Kamal T, Murray SM, et al. A randomized controlled trial of mental health interventions for survivors of systematic violence in Kurdistan, Northern Iraq. BMC Psychiatry. 2014a;14:1–15. doi: 10.1186/s12888-014-0360-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton P, Lee C, Haroz EE, Murray L, Dorsey S, et al. A transdiagnostic community-based mental health treatment for comorbid disorders: development and outcomes of a randomized controlled trial among Burmese refugees in Thailand. PLOS Med. 2014b;11:e1001757. doi: 10.1371/journal.pmed.1001757. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower P, Gilbody S. Stepped care in psychological therapies: access, effectiveness and efficiency. Br. J. Psychiatry. 2005;186:11–17. doi: 10.1192/bjp.186.1.11. [DOI] [PubMed] [Google Scholar]
- Brach C, Fraserirector I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med. Care Res. Rev. 2000;57:181–217. doi: 10.1177/1077558700057001S09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruckner TA, Scheffler RM, Shen G, Yoon J, Chisholm D, et al. The mental health workforce gap in low- and middle-income countries: a needs-based approach. Bull. World Health Organ. 2011;89:184–94. doi: 10.2471/BLT.10.082784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calzada EJ, Caldwell MB, Brotman L, Brown EJ, Wallace SA, et al. Training community members to serve as paraprofessionals in an evidence-based, prevention program for parents of preschoolers. J. Child Fam. Stud. 2005;14:387–402. [Google Scholar]
- Chisholm D, Sweeny K, Sheehan P, Rasmussen B, Smit F, et al. Scaling-up treatment of depression and anxiety: a global return on investment analysis. Lancet Psychiatry. 2016;3:415–24. doi: 10.1016/S2215-0366(16)30024-4. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL. Mapping evidence-based treatments for children and adolescents: application of the distillation and matching model to 615 treatments from 322 randomized trials. J. Consult. Clin. Psychol. 2009;77:566–79. doi: 10.1037/a0014565. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL, Park AL, Ward AM, Levy M, et al. Child STEPs in California: a cluster randomized effectiveness trial comparing modular treatment with community implemented treatment for youth with anxiety, depression, conduct problems, or traumatic stress. J. Consult. Clin. Psychol. 2017;85:13–25. doi: 10.1037/ccp0000133. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL, Weisz JR. Identifying and selecting the common elements of evidence based interventions: a distillation and matching model. Ment. Health Serv. Res. 2005;7:5–20. doi: 10.1007/s11020-005-1962-6. [DOI] [PubMed] [Google Scholar]
- Chow JCC, Jaffee K, Snowden L. Racial/ethnic disparities in the use of mental health services in poverty areas. Am. J. Public Health. 2003;93:792–97. doi: 10.2105/ajph.93.5.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung B, Ngo VK, Ong MK, Pulido E, Jones F, et al. Participation in training for depression care quality improvement: a randomized trial of community engagement or technical support. Psych. Serv. 2015;66:831–39. doi: 10.1176/appi.ps.201400099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Deblinger E. Treating Trauma and Traumatic Grief in Children and Adolescents. New York: Guilford Press; 2006. [Google Scholar]
- Coker TR, Elliott MN, Kataoka S, Schwebel DC, Mrug S, et al. Racial/ethnic disparities in the mental health care utilization of fifth grade children. Acad. Pediatr. 2009;9:89–96. doi: 10.1016/j.acap.2008.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins PY, Patel V, Joestl SS, March D, Insel TR, et al. Grand challenges in global mental health. Nature. 2011;475:27–30. doi: 10.1038/475027a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derr AS. Mental health service use among immigrants in the United States: a systematic review. Psych. Serv. 2015;67:265–74. doi: 10.1176/appi.ps.201500004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dua T, Barbui C, Clark N, Fleischmann A, Poznyak V, et al. Evidence-based guidelines for mental, neurological, and substance use disorders in low- and middle-income countries: summary of WHO recommendations. PLOS Med. 2011;8:e1001122. doi: 10.1371/journal.pmed.1001122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durlak JA. Comparative effectiveness of paraprofessional and professional helpers. Psychol. Bull. 1979;86:80–92. [PubMed] [Google Scholar]
- Dusenbury L, Brannigan R, Falco M, Hansen WB. A review of research on fidelity of implementation: implications for drug abuse prevention in school settings. Health Edu. Res. 2003;18:237–56. doi: 10.1093/her/18.2.237. [DOI] [PubMed] [Google Scholar]
- Eng E, Parker E, Harlan C. Lay health advisor intervention strategies: a continuum from natural helping to paraprofessional helping. Health Educ. Behav. 1997;24:413–17. doi: 10.1177/109019819702400402. [DOI] [PubMed] [Google Scholar]
- Fayyad JA, Farah L, Cassir Y, Salamoun MM, Karam EG. Dissemination of an evidence-based intervention to parents of children with behavioral problems in a developing country. Eur. Child Adolesc. Psychiatry. 2010;19:629–36. doi: 10.1007/s00787-010-0099-3. [DOI] [PubMed] [Google Scholar]
- Han M, Valencia M, Lee Y, De Leon J. Development and implementation of the culturally competent program with Cambodians: the pilot Psycho-Social-Cultural Treatment Group program. J. Ethn. Cult. Divers. Soc. Work. 2012;21:212–30. [Google Scholar]
- Hattie JA, Sharpley CF, Rogers HJ. Comparative effectiveness of professional and paraprofessional helpers. Psychol. Bull. 1984;95:80–92. [PubMed] [Google Scholar]
- Herschell AD, Kolko DJ, Baumann BL, Davis AC. The role of therapist training in the implementation of psychosocial treatments: a review and critique with recommendations. Clin. Psychol. Rev. 2010;30:448–66. doi: 10.1016/j.cpr.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoagwood KE, Cavaleri MA, Olin SS, Burns BJ, Slaton E, et al. Family support in children’s mental health: a review and synthesis. Clin. Child Fam. Psychol. Rev. 2010;13:1–45. doi: 10.1007/s10567-009-0060-5. [DOI] [PubMed] [Google Scholar]
- Hoagwood KE, Olin SS, Horwitz S, McKay M, Cleek A, et al. Scaling up evidence-based practices for children and families in New York State: toward evidence-based policies on implementation for state mental health systems. J. Clin. Child Adolesc. Psychol. 2014;43:145–57. doi: 10.1080/15374416.2013.869749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honikman S, van Heyningen T, Field S, Baron E, Tomlinson M. Stepped care for maternal mental health: a case study of the perinatal mental health project in South Africa. PLOS Med. 2012;9:e1001222. doi: 10.1371/journal.pmed.1001222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovey JD, Hurtado G, Seligman LD. Findings for a CBT support group for Latina migrant farmworkers in western Colorado. Curr. Psychol. 2014;33:271–81. [Google Scholar]
- Huang L, Macbeth G, Dodge J, Jacobstein D. Transforming the workforce in children’s mental health. Adm. Policy Ment. Hlth. 2004;32:167–87. doi: 10.1023/b:apih.0000042745.64582.72. [DOI] [PubMed] [Google Scholar]
- Jacobs RH, Guo S, Kaundinya P, Lakind D, Klein J, et al. A pilot study of mindfulness skills to reduce stress among a diverse paraprofessional workforce. J. Child Fam. Stud. 2017;26:2579–88. [Google Scholar]
- Jain S. The role of paraprofessionals in providing treatment for posttraumatic stress disorder in low-resource communities. JAMA. 2010;304:571–72. doi: 10.1001/jama.2010.1096. [DOI] [PubMed] [Google Scholar]
- Katigbak C, Van Devanter N, Islam N, Trinh-Shevrin C. Partners in health: a conceptual framework for the role of community health workers in facilitating patients’ adoption of healthy behaviors. Am. J. Public Health. 2015;105:872–80. doi: 10.2105/AJPH.2014.302411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE. Evidence-based treatment and practice: new opportunities to bridge clinical research and practice, enhance the knowledge base, and improve patient care. Am. Psychol. 2008;63:146–59. doi: 10.1037/0003-066X.63.3.146. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Rabbitt SM. Novel models for delivering mental health services and reducing the burdens of mental illness. Clin. Psychol. 2013;1:170–91. [Google Scholar]
- Kilbourne AM, Switzer G, Hyman K, Crowley-Matoka M, Fine MJ. Advancing health disparities research within the health care system: a conceptual framework. Am. J. Public Health. 2006;96:2113–21. doi: 10.2105/AJPH.2005.077628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konrad TR, Ellis AR, Thomas KC, Holzer CE, Morrissey JP. County-level estimates of need for mental health professionals in the United States. Psych. Serv. 2009;60:1307–14. doi: 10.1176/ps.2009.60.10.1307. [DOI] [PubMed] [Google Scholar]
- Lancet Global Mental Health Group. Scale up services for mental disorders: a call for action. Lancet. 2007;370:1241–52. doi: 10.1016/S0140-6736(07)61242-2. [DOI] [PubMed] [Google Scholar]
- Lee S, Laiewski L, Choi S. Racial-ethnic variation in US mental health service use among Latino and Asian non-US citizens. Psych. Serv. 2014;65:68–74. doi: 10.1176/appi.ps.201200430. [DOI] [PubMed] [Google Scholar]
- Lewin S, Munabi-Babigumira S, Glenton C, Daniels K, Bosch-Capblanch X, et al. Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Syst. Rev. 2010;2010(3) doi: 10.1002/14651858.CD004015.pub3. CD004015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsey MA, Brandt NE, Becker KD, Lee BR, Barth RP, et al. Identifying the common elements of treatment engagement interventions in children’s mental health services. Clin. Child Fam. Psychol. Rev. 2014;17:283–98. doi: 10.1007/s10567-013-0163-x. [DOI] [PubMed] [Google Scholar]
- Magaña S, Li H, Miranda E, de Sayu RP. Improving health behaviours of Latina mothers of youths and adults with intellectual and developmental disabilities. J. Intellectual Disabil. Res. 2015;59:397–410. doi: 10.1111/jir.12139. [DOI] [PubMed] [Google Scholar]
- McHugo GJ, Drake RE, Whitley R, Bond GR, Kikuko C, et al. Fidelity outcomes in the National Implementing Evidence-Based Practices Project. Psych. Serv. 2007;58:1279–84. doi: 10.1176/ps.2007.58.10.1279. [DOI] [PubMed] [Google Scholar]
- Minkler M. Linking science and policy through community-based participatory research to study and address health disparities. Am. J. Public Health. 2010;100:S81–S87. doi: 10.2105/AJPH.2009.165720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda J, Bernal G, Lau A, Kohn L, Hwang WC, LaFrombois T. State of the science on psychosocial interventions for ethnic minorities. Annu. Rev. Clin. Psychol. 2005;1:113–42. doi: 10.1146/annurev.clinpsy.1.102803.143822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore AA, Karno MP, Ray L, Ramirez K, Barenstein V, et al. Development and preliminary testing of a promotora-delivered, Spanish language, counseling intervention for heavy drinking among male, Latino day laborers. J. Subst. Abus. 2016;62:96–101. doi: 10.1016/j.jsat.2015.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullany B, Barlow A, Neault N, Billy T, Jones T, et al. The Family Spirit Trial for American Indian teen mothers and their children: CBPR rationale, design, methods and baseline characteristics. Prev. Sci. 2012;13:504–18. doi: 10.1007/s11121-012-0277-2. [DOI] [PubMed] [Google Scholar]
- Murray LK, Dorsey S, Bolton P, Jordans MJ, Rahman A, et al. Building capacity in mental health interventions in low resource countries: an apprenticeship model for training local providers. Int. J. Ment. Health Syst. 2011;5:30. doi: 10.1186/1752-4458-5-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray LK, Dorsey S, Haroz E, Lee C, Alsiary MM, et al. A Common Elements Treatment Approach for adult mental health problems in low-and middle-income countries. Cogn. Behav. Pract. 2014a;21:111–23. doi: 10.1016/j.cbpra.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray LK, Familiar I, Skavenski S, Jere E, Cohen J, et al. An evaluation of trauma-focused cognitive behavioral therapy for children in Zambia. Child Abuse Negl. 2013;37:175–85. doi: 10.1016/j.chiabu.2013.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray LK, Jordans MJD. Rethinking the service delivery system of psychological interventions in low and middle income countries. BMC Psychiatry. 2016;16:234–40. doi: 10.1186/s12888-016-0938-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray LK, Skavenski S, Kane JC, Mayeya J, Dorsey S, et al. Effectiveness of trauma-focused cognitive behavioral therapy among trauma-affected children in Luska, Zambia: a randomized clinical trial. JAMA Pediatr. 2015;16:761–69. doi: 10.1001/jamapediatrics.2015.0580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray LK, Tol W, Jordans M, Zangana GS, Amin AM, et al. Dissemination and implementation of evidence based, mental health interventions in post conflict, low resource settings. Intervention. 2014b;12:94–112. doi: 10.1097/WTF.0000000000000070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadeem E, Lange JM, Edge D, Fongwa M, Belin T, Miranda J. Does stigma keep poor young immigrant and US-born black and Latina women from seeking mental health care? Psych. Serv. 2007;58:1547–54. doi: 10.1176/ps.2007.58.12.1547. [DOI] [PubMed] [Google Scholar]
- Nadkarni A, Velleman R, Dabholkar H, Shinde S, Bhat B, et al. The systematic development and pilot randomized evaluation of counseling for alcohol problems, a lay counselor-delivered psychological treatment for harmful drinking in primary care in India: the PREMIUM study. Alcoh. Clin. Exp. Res. 2015;39:522–31. doi: 10.1111/acer.12653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nebeker C, López-Arenas A. Building Research Integrity and Capacity (BRIC): An Educational Initiative to Increase Research Literacy among Community Health Workers and Promotores. J. Microbiol. Biol. Educ. 2016;17:41–45. doi: 10.1128/jmbe.v17i1.1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuner F, Onyut PL, Ertl V, Odenwald M, Schauer E, Elbert T. Treatment of posttraumatic stress disorder by trained lay counselors in an African refugee settlement: a randomized controlled trial. J. Consult. Clin. Psychol. 2008;76:686–94. doi: 10.1037/0022-006X.76.4.686. [DOI] [PubMed] [Google Scholar]
- Ohtani A, Suzuki T, Takeuchi H, Uchida H. Language barriers and access to psychiatric care: a systematic review. Psych. Serv. 2015;66:798–805. doi: 10.1176/appi.ps.201400351. [DOI] [PubMed] [Google Scholar]
- Olds DL, Robinson J, O’Brien R, Luckey DW, Pettitt LM, et al. Home visiting by paraprofessionals and by nurses: a randomized, controlled trial. Pediatrics. 2002;110:486–96. doi: 10.1542/peds.110.3.486. [DOI] [PubMed] [Google Scholar]
- Olin SS, Williams N, Pollock M, Armusewicz K, Kutash K, et al. Quality indicators for family support services and their relationship to organizational social context. Adm. Policy Ment. Health. 2014;41:43–54. doi: 10.1007/s10488-013-0499-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padmanathan P, De Silva MJ. The acceptability and feasibility of task-sharing for mental healthcare in low and middle income countries: a systematic review. Soc. Sci. Med. 2013;97:82–86. doi: 10.1016/j.socscimed.2013.08.004. [DOI] [PubMed] [Google Scholar]
- Papas RK, Sidle JE, Gakinya BN, Baliddawa JB, Martino S, et al. Treatment outcomes of a stage 1 cognitive-behavioral trial to reduce alcohol use among human immunodeficiency virus-infected out-patients in western Kenya. Addiction. 2011;106:2156–66. doi: 10.1111/j.1360-0443.2011.03518.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papas RK, Sidle JE, Martino S, Baliddawa JB, Songole R, et al. Systematic cultural adaptation of cognitive-behavioral therapy to reduce alcohol use among HIV-infected outpatients in western Kenya. AIDS Behav. 2010;14:669–78. doi: 10.1007/s10461-009-9647-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Chowdhary N, Rahman A, Verdeli H. Improving access to psychological treatments: lessons from developing countries. Behav. Res. Ther. 2011;49:523–28. doi: 10.1016/j.brat.2011.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Weiss HA, Chowdhary N, Naik S, Pednekar S, et al. Effectiveness of an intervention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa, India (MANAS): a cluster randomized controlled trial. Lancet. 2010;376:2086–95. doi: 10.1016/S0140-6736(10)61508-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira B, Andrew G, Pednekar S, Kirkwood BR, Patel V. The integration of the treatment for common mental disorders in primary care: experiences of health care providers in the MANAS trial in Goa, India. Int. J. Ment. Health Syst. 2011;5:26–35. doi: 10.1186/1752-4458-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry HB, Zulliger R, Rogers MM. Community health workers in low-, middle-, and high-income countries: an overview of their history, recent evolution, and current effectiveness. Annu. Rev. Public Health. 2014;35:399–421. doi: 10.1146/annurev-publhealth-032013-182354. [DOI] [PubMed] [Google Scholar]
- Pescosolido BA. Illness careers and network ties: a conceptual model of utilization and compliance. In: Albrecht G, Levy J, editors. Advances in Medical Sociology. Vol. 2. Greenwich, CT: JAI Press; 1991. pp. 164–81. [Google Scholar]
- Petersen I, Bhana A, Baillie K. The feasibility of adapted group-based interpersonal therapy (IPT) for the treatment of depression by community health workers within the context of task shifting in South Africa. Community Ment. Health J. 2012;48:336–41. doi: 10.1007/s10597-011-9429-2. [DOI] [PubMed] [Google Scholar]
- Philbin MM, Flake M, Hatzenbuehler ML, Hirsch JS. State-level immigration and immigrant-focused policies as drivers of Latino health disparities in the United States. Soc. Sci. Med. 2017 doi: 10.1016/j.socscimed.2017.04.007. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puffer ES, Green EP, Chase RM, Sim AL, Zayzay J, et al. Parents make the difference: a randomized-controlled trial of a parenting intervention in Liberia. Glob. Ment. Health. 2015;2:e15. doi: 10.1017/gmh.2015.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Repper J, Carter T. A review of the literature on peer support in mental health services. JMH. 2011;20:392–411. doi: 10.3109/09638237.2011.583947. [DOI] [PubMed] [Google Scholar]
- Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos: a qualitative systematic review. Am. J. Prev. Med. 2007;33:418–27. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]
- Rodriguez J, Olin SS, Hoagwood KE, Shen S, Burton G, et al. The development and evaluation of a parent empowerment program for family peer advocates. J. Child Fam. Stud. 2011;20:397–405. doi: 10.1007/s10826-010-9405-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roll JM, Kennedy J, Tran M, Howell D. Disparities in unmet need for mental health services in the United States, 1997–2010. Psychiatr. Serv. 2013;64:80–82. doi: 10.1176/appi.ps.201200071. [DOI] [PubMed] [Google Scholar]
- Roman LA, Gardiner JC, Lindsay JK, Moore JS, Luo Z, et al. Alleviating perinatal depressive symptoms and stress: a nurse-community health worker randomized trial. Arch. Women’s Ment. Health. 2009;12:379–91. doi: 10.1007/s00737-009-0083-4. [DOI] [PubMed] [Google Scholar]
- Roman LA, Lindsay JK, Moore JS, Duthie PA, Peck C, et al. Addressing mental health and stress in Medicaid-insured pregnant women using a nurse-community health worker home visiting team. Public Health Nurs. 2007;24:239–48. doi: 10.1111/j.1525-1446.2007.00630.x. [DOI] [PubMed] [Google Scholar]
- Saraceno B, van Ommeren M, Batniji R, Cohen A, Gureje O, et al. Barriers to improvement of mental health services in low-income and middle-income countries. Lancet. 2007;370:1164–74. doi: 10.1016/S0140-6736(07)61263-X. [DOI] [PubMed] [Google Scholar]
- Shinde S, Andrew G, Bangash O, Cohen A, Kirkwood B, Patel V. The impact of a lay counselor led collaborative care intervention for common mental disorders in public and private primary care: a qualitative evaluation nested in the MANAS trial in Goa, India. Soc. Sci. Med. 2013;88:48–55. doi: 10.1016/j.socscimed.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singla DR, Kohrt BA, Murray LK, Anand A, Chorpita BF, Patel V. Psychological treatments for the world: lessons from low-and middle-income countries. Annu. Rev. Clin. Psychol. 2017;13:149–81. doi: 10.1146/annurev-clinpsy-032816-045217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stacciarini JMR, Rosa A, Ortiz M, Munari DB, Uicab G, Balam M. Promotoras in mental health: a review of English, Spanish, and Portuguese literature. Fam. Community Health. 2012;35:92–102. doi: 10.1097/FCH.0b013e3182464f65. [DOI] [PubMed] [Google Scholar]
- Stirman SW, Kimberly J, Cook N, Calloway A, Castro F, Charns M. The sustainability of new programs and innovations: a review of the empirical literature and recommendations for future research. Implement. Sci. 2012;7:17. doi: 10.1186/1748-5908-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terpstra J, Coleman KJ, Simon G, Nebeker C. The role of community health workers (CHWs) in health promotion research: ethical challenges and practical solutions. Health Promot. Pract. 2011;12:86–93. doi: 10.1177/1524839908330809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas KC, Ellis AR, Konrad TR, Holzer CE, Morrissey JP. County-level estimates of mental health professional shortage in the United States. Psych. Serv. 2009;60:1323–28. doi: 10.1176/ps.2009.60.10.1323. [DOI] [PubMed] [Google Scholar]
- van Ginneken N, Tharyan P, Lewin S, Rao GN, Meera S, et al. Non-specialist health worker interventions for the care of mental, neurological and substance-abuse disorders in low- and middle-income countries. Cochrane Database Syst. Rev. 2013;2013(11) doi: 10.1002/14651858.CD009149.pub2. CD009149. [DOI] [PubMed] [Google Scholar]
- Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiat. 2016;3:171–78. doi: 10.1016/S2215-0366(15)00505-2. [DOI] [PubMed] [Google Scholar]
- Viswanathan M, Kraschnewski JL, Nishikawa B, Morgan LC, Honeycutt AA, et al. Outcomes and costs of community health worker interventions: a systematic review. Med. Care. 2010;48:792–808. doi: 10.1097/MLR.0b013e3181e35b51. [DOI] [PubMed] [Google Scholar]
- Weiss WM, Murray LK, Zangana GAS, Mahmooth Z, Kaysen D, et al. Community-based mental health treatments for survivors of torture and militant attacks in Southern Iraq: a randomized control trial. BMC Psychiatry. 2015;15:249–65. doi: 10.1186/s12888-015-0622-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz JR, Chorpita BF, Palinkas LA, Schoenwald SK, Miranda J, et al. Testing standard and modular designs for psychotherapy treating depression, anxiety, and conduct problems in youth: a randomized effectiveness trial. Arch. Gen. Psychiatry. 2012;69:274–82. doi: 10.1001/archgenpsychiatry.2011.147. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Kuppens S, Eckshtain D, Ugueto AM, Hawley KM, Jensen-Doss A. Performance of evidence-based youth psychotherapies compared with usual clinical care: a multilevel meta-analysis. JAMA Psychiatry. 2013;70:750–61. doi: 10.1001/jamapsychiatry.2013.1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells K, Klap R, Koike A, Sherbourne C. Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. Am. J. Psychiatry. 2001;158:2027–32. doi: 10.1176/appi.ajp.158.12.2027. [DOI] [PubMed] [Google Scholar]
- Wennerstrom A, Vannoy SD, Allen CE, Meyers D, O’Toole E, et al. Community-based participatory development of a community health worker mental health outreach role to extend collaborative care in post-Katrina New Orleans. Ethn. Dis. 2011;21:S1. [PMC free article] [PubMed] [Google Scholar]
- World Health Organ. (WHO) Task Shifting: Rational Redistribution of Tasks Among Health Workforce Teams: Global Recommendations and Guidelines. Geneva: WHO; 2007. http://www.who.int/iris/handle/10665/43821. [Google Scholar]
- World Health Organ. (WHO) mhGap: Mental Health Gap Action Programme: Scaling Up Care for Mental, Neurological, and Substance Use Disorders. Geneva: WHO; 2008. http://www.who.int/iris/handle/10665/43809. [PubMed] [Google Scholar]
- World Health Organ. (WHO) mhGAP Humanitarian Intervention Guide (mhGAP-HIG): Clinical Management of Mental, Neurological and Substance Use Conditions in Humanitarian Emergencies. Geneva: WHO; 2015. http://apps.who.int/iris/handle/10665/162960. [Google Scholar]
- Zachariah R, Ford N, Philips M, Lynch S, Massaquoi M, et al. Task shifting in HIV/AIDS: opportunities, challenges and proposed actions for sub-Saharan Africa. Trans. R. Soc. Trop. Med. Hyg. 2009;103:549–58. doi: 10.1016/j.trstmh.2008.09.019. [DOI] [PubMed] [Google Scholar]