Abstract
Outdated federal and state occupational lead standards leave workers and their families vulnerable to the adverse effects of lead. Standards should be updated to reflect the best available scientific and medical evidence, which documents harm to multiple organ systems even at low levels of exposure. This commentary will review the inadequacies of existing policies, highlight susceptible populations, and summarize state revision efforts to date. Federal policies must be strengthened to protect our workers and their families from this well-documented hazard.
Keywords: lead, occupational health, workplace safety, neurotoxicology, family, children, policy
Graphical abstract

Figure adapted from Centers for Disease Control and Prevention (CDC)/National Institute for Occupational Safety & Health (NIOSH)(1).
Abbreviations and references: OSHA: Occupational Safety and Health Administration (2). Healthy People 2020 Objectives (3). CSTE: Council of State and Territorial Epidemiologists (4). ABLES: Adult Blood Lead Epidemiology & Surveillance(5). CDC Nationally Notifiable Condition (6). AOEC: Association of Occupational and Environmental Clinics (7). California Department of Public Health Medical Guidelines (8). CDC ACCLPP: Advisory Committee on Childhood Lead Poisoning Prevention (9). CDC National Report on Human Exposure to Environmental Chemicals (10).
INTRODUCTION
Lead poisoning returned to the national consciousness through the tragic events in Flint, Michigan, but drinking water is only one of many exposure routes. Outdated federal workplace safety standards allow for potential acute and chronic occupational lead exposure. While all workplace standards are traditionally less stringent than for exposures in the general public, the existing workplace standards for lead are dangerously inappropriate.
Lead is a well-studied metal toxicant with no known safe level of exposure (11). Occupational exposure has long been linked to increased cancer and mortality (12–20). Yet even low lead levels in adults can cause numerous other adverse health outcomes, including hypertension, renal injury, cognitive impairments, and reproductive effects (21, 22). Workplace lead may also affect children, who can be exposed prenatally or through lead dust carried into the home (23–27). The consequences of these exposures across the population are substantial. A recent analysis suggests that the combined direct and indirect costs of occupational lead in the United States are greater than $392 million (28).
We need to protect workers and their families from significant adverse health effects and related financial costs by updating federal workplace lead standards based on the latest scientific research. Revising these standards, in addition to other outdated lead policies in this country (29, 30), is essential to reducing harmful exposures across the population and meeting federal agency health goals.
DISCUSSION
Existing Standards Provide Inadequate Protections
The U.S. Occupational Safety and Health Administration (OSHA) estimates that 804,000 general industry workers and 838,000 construction industry workers are potentially exposed to lead through their jobs (31). While data from the state-based Adult Blood Lead Epidemiology and Surveillance (ABLES) Program indicate that there has been a substantial reduction in the prevalence of elevated adult blood lead levels (BLLs), workplace lead exposures are still a serious concern. Overall, approximately 94% of adults with elevated BLLs are exposed to lead in the workplace (32). There is likely substantial underreporting, however, given that not all employers provide BLL testing to their workers (even though this is a requirement of OSHA guidelines) and not all states participate in the ABLES program (28, 32, 33). There is also no system in place to test and report BLLs of workers’ family members, and thus comprehensive data on take-home lead exposure is not available.
OSHA regulates workplace lead exposure at the national level through two standards: the general industry standard and the construction standard (34, 35). While OSHA’s mandate is to “assure so far as possible every working man and women in the Nation safe and healthful working conditions” (36) these goals have not been met for workplace lead exposure. Existing federal standards are severely outdated, based on information available in the 1970’s instead of the latest scientific and medical evidence. Selected inadequacies of the standards are outlined below.
Medical Removal
Under the existing regulations, workers can be exposed to levels of lead that result in 60 micrograms (μg) of lead per deciliter (dL) of blood (or an average of 50 μg/dL on three or more tests) before medical removal is required, and they can return to work after their blood lead levels are as high as 40 μg/dL. As comparison, the Centers for Disease Control and Prevention (CDC) has set a “Healthy People 2020” national public health goal that aims to reduce the proportion of workers with blood lead levels above 10 μg/dL (3) (see graphical abstract).
Exposure to levels of lead much lower than what is allowable under OSHA’s current standards have been linked to high blood pressure, decreased kidney function, reproductive effects and neurological impairments (21, 22). In particular, the National Toxicology Program Monograph on the Health Effects of Low-Level Lead concluded that there is “sufficient evidence” that BLLs < 5 ug/dL are associated with decreased renal function and reduced fetal growth. There was also “sufficient evidence” that BLLs <10 ug/dL are associated with hypertension and essential tremor (22). There is also a substantial body of literature linking occupation-related elevated blood lead levels to increased cancer and mortality (12–18, 20), and a recent multi-country cohort study adds to this evidence base by documenting an association between lead-exposed workers (with median blood lead 26 ug/dL) and increased risk of lung cancer, chronic obstructive pulmonary disease (COPD), stroke, and heart disease (19).
Air Lead Levels: Standards & Entry Requirements
Equally problematic are the existing guidelines regarding allowable levels of lead in the air. Current regulations set a permissible exposure limit (PEL) of 50 μg/m3 averaged over 8 hours for both general industry and construction. These levels were determined based on the goal of keeping worker BLLs below 60 μg/dL (37). To keep worker BLLs below 10 μg/dL over a working lifetime – in line with current CDC Healthy People 2020 goals – models indicate that the PEL needs to be significantly lowered (38).
The action level (AL), which triggers exposure monitoring and medical surveillance, is currently set as 30 μg/m3 averaged over an 8 hour period. This level was set based on the goal of maintaining BLLs below 30 μg/100 g for individuals planning pregnancies (37). However, current scientific evidence indicates that adverse reproductive effects occur at much lower BLLs (21). Therefore, this insufficient AL must also be updated.
The current air lead standards are unacceptably high for both the general industry standard and the construction standard, but additionally problematic is the overreliance on air lead levels to prompt action within general industry scenarios. Studies indicate that, at least in some circumstances, there is little correlation between air lead levels and BLLs (39–42). Lead exposure through ingestion is likely responsible for the discrepancy in these measurements (42–45). Therefore, the general industry standard must be updated to account for other routes of exposure by including alternative criteria for “entry” into the lead standard. For example, the standard could include specific “trigger tasks” or activities known to contain lead hazards that would automatically initiate monitoring and related protective measures for workers, analogous to what currently exists in the construction standard.
Training, Hygiene, & Risk Communication
Improved lead education and safety training for the workplace is urgently needed. Employers should be responsible for providing designated lead-free areas for eating and drinking as well as changing areas for removal of lead-contaminated clothing to prevent take-home lead pathways. For example, lead-exposed shoes and boots should not be worn into the car or home. Frequent training in an appropriate and understandable format must be provided to employees, and clear warnings signs should be located in areas or with specific activities containing lead hazards. Protective equipment should be provided whenever lead is present, instead of the current protocol that only requires protective clothing and shoes when lead is present above the PEL (34). The overarching concept that there is no safe level of lead exposure, especially for children, needs to be emphasized.
Vulnerable Populations
ABLES data indicate that industries with high potential for occupational lead exposure include manufacturing, construction, services, and mining. Table 1 lists specific trades within each of these industries that accounted for the highest percentage of reported occupational lead exposure cases in 2013 (32).
Table 1.
Industries reporting the highest percentage of BLLs ≥ 25 among workers, 2013 (32)
| Manufacturing | Construction | Services | Mining |
|---|---|---|---|
| Storage battery manufacturing | Painting and wall covering contractors | Remediation services | Copper, nickel, lead, zinc mining |
| Alumina and aluminum production and processing | Highway, street, and bridge construction | Amusement and recreation services | |
| Nonferrous metal (except copper and aluminum) rolling, drawing, extruding, and alloying | Residential building construction | Automotive, mechanical, and electrical repair and maintenance |
Another problematic industry is indoor firing ranges, which represent important sources of lead exposure for workers as well as individuals participating in target practice (46). There are estimated to be between 16,000–18,000 indoor firing ranges in the United States (47). Lead-based projectiles can result in immediate and significant airborne lead concentrations, and settled lead dust that is improperly cleaned can present a delayed hazard even after active shooting practice has ceased (47, 48).
In these and other industries, not only are workers at risk, but their families may also be exposed inadvertently through take-home lead dust (23–25, 49–53). In a meta-analysis by Roscoe et al. (1999), the authors concluded that there were at least 48,000 families with young children and household individuals subject to occupational lead exposure. Their limited data suggested that approximately 50% of the young children in these families had BLLs greater than 10 ug/dl (53). This analysis, albeit dated, indicates that occupational lead exposure presents risks for lead exposure in children. Further work is urgently needed to quantify the frequency and magnitude of take-home exposures.
Children are particularly vulnerable to lead, since they absorb a greater percentage of the metal from the gastrointestinal tract compared to adults (54). Because lead substitutes for calcium, children, pregnant or lactating women, and individuals with nutritional deficiencies exhibit increased absorption (54, 55). Children’s developing nervous systems are highly susceptible to the effects of environmental toxicants (56), and even low level lead exposure can result in long-term intellectual impairment (57–60). The economic and societal implications of lead exposures across the population are significant and have been discussed previously (61).
Women working in industries with potential lead exposure are themselves at risk for adverse effects from lead (21), and they may also be putting the next generation at risk. Lead released from bones during pregnancy easily crosses the placenta (27), and children born to lead-exposed workers experience neurodevelopmental and other adverse health effects (26, 62).
It should also be noted that the Fair Labor Standards Act has set 14 years of age as the general minimum age of employment (63). Certain types of hazardous work are prohibited for individuals under the age of 18 years of age, but situations with high risk of lead exposure are not explicitly listed in this regulation (64). The potential for adolescent exposure to such high levels of lead is very concerning, given that even low lead exposures (below 10 μg/dL) have been associated with cognitive deficits (65). Furthermore, the brain continues to undergo crucial development through young adulthood (66, 67) – and thereby remains vulnerable to disruption from lead exposure.
Additionally, preliminary reports suggest that occupational exposure may occur disproportionately among minority communities. In King County (Seattle, WA), Asian, Hispanic, and other workers of color are more likely to be exposed to high levels of lead through the workplace (68, 69). For example, the 2010 U.S. Census indicates that only 6.6% of Seattle residents are Hispanic/Latino (70), but a recent analysis indicates almost one third of workers exposed to lead through bridge painting were Hispanic (71). These disproportionate exposures further emphasize the need for changes to the existing standards.
New State Standards on the Horizon
OSHA sets minimum national standards for worker lead exposure, but these standards can be superseded if a state has an occupational safety and health program. Currently, 22 states have OSHA-approved state plans, including California and Washington. However, currently, these state standards are identical to the insufficient federal standards. Recognizing the need for improved protections, both California and Washington are in the process of updating their state occupational lead standards. The California Department of Public Health Occupational Lead Poisoning Prevention Program conducted extensive research on the latest scientific and medical literature and made specific recommendations for improvements in 2010 and 2011. Their guidance includes: lowering the BLL for medical removal to two BLLs above 20 μg/dL or one BLL above 30 μg/dL; increasing the frequency of BLL testing; triggering BLL testing based on activities that create lead hazards instead of the results of air monitoring; and lowering the PEL to 0.5–2.1 μg/m3 averaged over an 8-hour workday (38). The latter recommendation regarding the lower PEL was based on a report produced by the Office of Environmental Health Hazard Assessment (OEHHA), California Environmental Protection Agency (Cal/EPA) that used an updated physiologically-based pharmacokinetic (PBPK) model to characterize the relationship between air lead levels and blood lead levels (72). After over six years and a series of advisory meetings to receive feedback on discussion draft updates, it appears that California has still not completed the process to promulgate revised standards.
Washington State has begun a similar process. In 2012, Public-Health Seattle & King County (PHSKC) petitioned Governor Jay Inslee and the Washington State Department of Labor & Industries (L&I) to update the state’s outdated occupational lead standards. Drawing on the much of the same research conducted to support California’s update process, PHSKC has developed recommendations to ensure that worker BLLs remain below 10 μg/dL over a working lifetime. These recommendations include: reductions in air lead levels that trigger regulatory actions, to an AL of 2 μg/m3 and a PEL of 10 μg/m3; lowering the BLL that triggers medical removal to two BLLs above 20 μg/dL or one BLL above 30 μg/dL; improved medical monitoring for lead-related health effects; stricter standards for protective clothing, hygiene, training, and education (71). L&I released a first draft of their updated regulations in summer 2017 and is currently considering stakeholder feedback in a revision process. Key aspects of their initial draft include an AL μg/m3 of 10, a PEL of 20 μg/m3, a chronic removal BLL of 20 μg/dL, and an acute removal BLL 30 μg/dL.
CONCLUSION
Scientific Considerations
Scientifically, it is well established that even low levels of lead exposure can cause lifelong damage to the neurologic system and can lead to complications for numerous other organ systems (21, 22). Previous literature – including a Congressional report–has demonstrated that workers exposed to lead on the job can bring lead into the home on their clothing, thereby exposing their families (23–25, 49–53). Given that children exhibit higher absorption of lead than adults (54), that their developing organ systems are highly susceptible to the adverse health effects of all chemicals (73), and that early life lead exposure can have long term consequences (58, 74, 75), it is critical that occupational lead regulations consider not only the health of workers but also of their young family members.
Historical Considerations
Decades of data document the adverse effects of lead across the population, and this information has resulted in a dramatic drop in the acceptable childhood blood lead level (see Figure 1). One driving factor for these changes has been the recognition that the most serious consequences of childhood lead exposure are its neurological effects. Unfortunately, however, despite the scientific and medical information on the harmful effects of lead in adults, the occupational standards have not been changed in over forty years.
Figure 1.
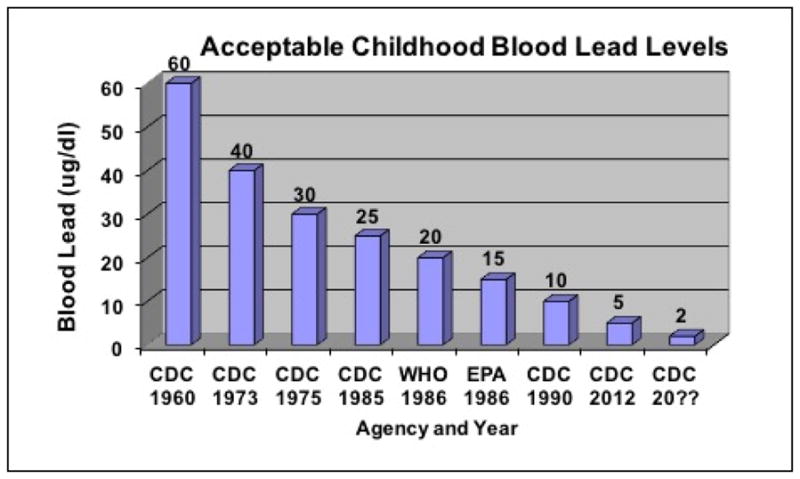
Decrease in Acceptable Childhood Blood Lead Levels. Adapted from Gilbert and Weiss (2006) (61)
Ethical Considerations
Everyone has a right to a lead-free environment that allows him/her to reach and maintain his/her full potential. As described above, occupational lead exposure can have direct adverse health effects on the exposed workers. Yet, occupational lead exposures may also cause adverse health effects on family members and future generations. For example, when parents or young adult workers bring workplace contamination into the home, they can expose their families and children to lead. In addition, though the consequences have yet to be fully elucidated, lead exposure has been linked to epigenetic changes (76). Further work is needed to better understand the intergenerational implications of lead exposure, but this potential suggests the need for epiprecaution (77).
Overall, CDC has determined there is no safe level of blood lead for children (11), and recent research documents the hazards to adults from even low levels of lead (<10 ug/dL) (22). With this scientific knowledge comes ethical and political responsibility. Scientists and health professionals are fully aware of the hazards of lead for children and adults, and we must now press for standards that are fully protective for the entire population.
National Action Needed
The existing occupational lead standards are so outdated that some private companies have actually implemented more protective standards for their own employees (78). The state-specific actions in Washington and California, as described above, are important, but why should workers in only two states be privileged to improved health protections? OSHA standards should also be strengthened to adequately protect workers and families across the country, as all workers have a right to a healthy and safe work environment. The American College of Occupational and Environmental Medicine (ACOEM) recently released a position statement endorsing updated occupational lead standards for all American workers (79).
We have the scientific and medical evidence that documents the harms of elevated blood lead levels, and we have the technology to reduce occupational lead exposure. Now is the time to take action by:
Adopting a occupational lead standard that is aligned with CDC’s existing public health guidance;
Ensuring that OSHA receives sufficient financial support for necessary enforcement actions in the coming years;
Implementing routine BLL testing for family members of workers at risk for occupational lead exposure.
Updated federal occupational standards are a critical component of broader, nationwide efforts to reduce lead exposure across the general population, such as through improvements to existing regulations related to residential property and drinking water. Stronger standards for all lead-related policies will ensure a stronger, healthier country for generations to come.
Highlights.
Occupational lead standards do not reflect current scientific information
Occupational lead exposure poses risks to workers and their family members
Updates to occupational lead standards are critical to protect public health
There is no safe level of lead exposure and everyone has a right to a lead-free life
Acknowledgments
Funding: RMS was supported by the National Institute of Environmental Health Sciences grant T32ES015459. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agency.
Footnotes
Competing Financial Interests: The authors declare no conflict of interest or competing financial interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health. Reference Blood Lead Levels for Adults in the US. 2013 https://www.cdc.gov/niosh/topics/ables/pdfs/referencebloodlevelsforadults_2013-10-22.pdf.
- 2.Occupational Safety and Health Administration. Lead. Safety and Health Topics. https://www.osha.gov/SLTC/lead/; Undated.
- 3.US Office of Disease Prevention and Health Promotion. Occupational Safety and Health Objectives. Healthy People. 2020 https://www.healthypeople.gov/2020/topics-objectives/topic/occupational-safety-and-health/objectives.
- 4.Council of State and Territorial Epidemiologists (CSTE) Position Statement 09-OH-02: Public Health Reporting and National Notification for Elevated Blood Lead Levels. 2009 http://c.ymcdn.com/sites/www.cste.org/resource/resmgr/PS/09-OH-02.pdf.
- 5.National Institute for Occupational Safety and Health (NIOSH) Adult Blood Lead Epidemiology and Surveillance (ABLES) 2017 https://www.cdc.gov/niosh/topics/ABLES/description.html.
- 6.National Notifiable Diseases Surveillance System (NNDSS) Lead, Elevated Blood Levels. 2016 https://wwwn.cdc.gov/nndss/conditions/lead-elevated-blood-levels/
- 7.Association of Occupational and Environmental Clinics (AOEC) Medical Management Guidelines for Lead-Exposed Adults. 2007 http://www.aoec.org/documents/positions/MMG_FINAL.pdf.
- 8.California Department of Public Health (DPH) Medical Guidelines for the Lead-Exposed Worker. 2009 https://www.cdph.ca.gov/Programs/CCDPHP/DEODC/OHB/OLPPP/CDPHDocumentLibrary/medgdln.pdf.
- 9.(ACCLPP) CACoCLPP. CDC Response to Advisory Committee on Childhood Lead Poisoning Prevention, Recommendations in “Low Level Lead Exposure Harms Children: A Renewed Call of Primary Prevention”. 2010 https://www.cdc.gov/nceh/lead/acclpp/cdc_response_lead_exposure_recs.pdf.
- 10.CDC. Fourth National Report on Human Exposure to Environmental Chemicals; Updated Tables. Atlanta, GA: Jan, 2017. [Google Scholar]
- 11.Centers for Disease Control and Prevention. Lead. 2017 https://www.cdc.gov/nceh/lead/
- 12.Anttila A, Heikkila P, Pukkala E, Nykyri E, Kauppinen T, Hernberg S, et al. Excess lung cancer among workers exposed to lead. Scand J Work Environ Health. 1995;21(6):460–9. doi: 10.5271/sjweh.62. [DOI] [PubMed] [Google Scholar]
- 13.Winegar DA, Levy BS, Andrews JS, Jr, Landrigan PJ, Scruton WH, Krause MJ. Chronic occupational exposure to lead: an evaluation of the health of smelter workers. J Occup Med. 1977;19(9):603–6. [PubMed] [Google Scholar]
- 14.Gwini S, MacFarlane E, Del Monaco A, McLean D, Pisaniello D, Benke GP, et al. Cancer incidence, mortality, and blood lead levels among workers exposed to inorganic lead. Ann Epidemiol. 2012;22(4):270–6. doi: 10.1016/j.annepidem.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 15.Ilychova SA, Zaridze DG. Cancer mortality among female and male workers occupationally exposed to inorganic lead in the printing industry. Occup Environ Med. 2012;69(2):87–92. doi: 10.1136/oem.2011.065201. [DOI] [PubMed] [Google Scholar]
- 16.Steenland K, Selevan S, Landrigan P. The mortality of lead smelter workers: an update. Am J Public Health. 1992;82(12):1641–4. doi: 10.2105/ajph.82.12.1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stollery BT, Broadbent DE, Banks HA, Lee WR. Short term prospective study of cognitive functioning in lead workers. British Journal of Industrial Medicine. 1991;48(11):739–749. doi: 10.1136/oem.48.11.739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schwartz BS, Lee B-K, Bandeen-Roche K, Stewart W, Bolla K, Links J, et al. Occupational Lead Exposure and Longitudinal Decline in Neurobehavioral Test Scores. Epidemiology. 2005;16(1) doi: 10.1097/01.ede.0000147109.62324.51. [DOI] [PubMed] [Google Scholar]
- 19.Steenland K, Barry V, Anttila A, Sallmen M, McElvenny D, Todd AC, et al. A cohort mortality study of lead-exposed workers in the USA, Finland and the UK. Occup Environ Med. 2017 doi: 10.1136/oemed-2017-104311. [DOI] [PubMed] [Google Scholar]
- 20.Chowdhury R, Ebelt Sarnat S, Darrow L, McClellan W, Steenland K. Mortality among participants in a lead surveillance program. Environmental Research. 2014;132(Supplement C):100–104. doi: 10.1016/j.envres.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 21.Kosnett MJ, Wedeen RP, Rothenberg SJ, Hipkins KL, Materna BL, Schwartz BS, et al. Recommendations for Medical Management of Adult Lead Exposure. Environmental Health Perspectives. 2007;115(3):463–471. doi: 10.1289/ehp.9784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Toxicology Program. NTP Monograph: Health Effects of Low-Level Lead. NTP monograph. 2012;(1):i. [PubMed] [Google Scholar]
- 23.Newman N, Jones C, Page E, Ceballos D, Oza A. Investigation of childhood lead poisoning from parental take-home exposure from an electronic scrap recycling facility—Ohio, 2012. MMWR Morb Mortal Wkly Rep. 2015;64:743–745. [PMC free article] [PubMed] [Google Scholar]
- 24.Hipkins KL, Materna BL, Payne SF, Kirsch LC. Family lead poisoning associated with occupational exposure. Clin Pediatr (Phila) 2004;43(9):845–9. doi: 10.1177/000992280404300909. [DOI] [PubMed] [Google Scholar]
- 25.Whelan EA, Piacitelli GM, Gerwel B, Schnorr TM, Mueller CA, Gittleman J, et al. Elevated blood lead levels in children of construction workers. Am J Public Health. 1997;87(8):1352–5. doi: 10.2105/ajph.87.8.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goyer RA. Results of lead research: prenatal exposure and neurological consequences. Environmental Health Perspectives. 1996;104(10):1050–1054. doi: 10.1289/ehp.961041050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Silbergeld EK. Lead in bone: implications for toxicology during pregnancy and lactation. Environmental Health Perspectives. 1991;91:63–70. doi: 10.1289/ehp.919163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Levin R. The attributable annual health costs of U.S. occupational lead poisoning. International Journal of Occupational and Environmental Health. 2016;22(2):107–120. doi: 10.1080/10773525.2016.1173945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Center for Healthy Housing. Find it, Fix it, Fund it: A Lead Elimination Action Drive. 2016. [Google Scholar]
- 30.Bellinger DC, Chen A, Lanphear BP. Establishing and achieving national goals for preventing lead toxicity and exposure in children. JAMA Pediatrics. 2017 doi: 10.1001/jamapediatrics.2017.0775. [DOI] [PubMed] [Google Scholar]
- 31.Occupational Safety and Health Administration. Safety and Health Topics. Lead. Undated. [Google Scholar]
- 32.Alarcon WA. MMWR. Morbidity and Mortality Weekly Report. 2016. Elevated Blood Lead Levels Among Employed Adults—United States, 1994–2013; p. 63. [DOI] [PubMed] [Google Scholar]
- 33.Leigh JP. Costs of occupational injuries and illnesses. University of Michigan Press; 2000. [Google Scholar]
- 34.29 CFR 1910.1025. In.
- 35.29 CFR 1926.62. In.
- 36.Williams-Steiger Act Occupational Safety and Health Act of 1970 Public Law, 1970, 91, 596
- 37.43 CFR 1910.1025 1978. In.
- 38.California Department of Public Health; California Department of Public Health OHB, editor. Revising the Workplace Lead Standards: At a Glance. 2014 http://www.cdph.ca.gov/programs/olppp/Documents/LeadStdRev-At-A-Glance.pdf.
- 39.Richter ED, Yaffe Y, Gruener N. Air and blood lead levels in a battery factory. Environmental research. 1979;20(1):87–98. doi: 10.1016/0013-9351(79)90088-4. [DOI] [PubMed] [Google Scholar]
- 40.Lai J-S, Wu TN, Liou S-H, Shen C-Y, Guu C-F, Ko K-N, et al. A study of the relationship between ambient lead and blood lead among lead battery workers. International archives of occupational and environmental health. 1997;69(4):295–300. doi: 10.1007/s004200050150. [DOI] [PubMed] [Google Scholar]
- 41.Lormphongs S, Miyashita K, Morioka I, Chaikittiporn C, Miyai N, Yamamoto H. Lead exposure and blood lead level of workers in a battery manufacturing plant in Thailand. Industrial health. 2003;41(4):348–353. doi: 10.2486/indhealth.41.348. [DOI] [PubMed] [Google Scholar]
- 42.Ho SF, Sam CT, Embi GB. Lead exposure in the lead-acid storage battery manufacturing and PVC compounding industries. Occup Med (Lond) 1998;48(6):369–73. doi: 10.1093/occmed/48.6.369. [DOI] [PubMed] [Google Scholar]
- 43.Askin DP, Volkmann M. Effect of personal hygiene on blood lead levels of workers at a lead processing facility. Am Ind Hyg Assoc J. 1997;58(10):752–3. doi: 10.1080/15428119791012414. [DOI] [PubMed] [Google Scholar]
- 44.Ulenbelt P, Lumens ME, Geron HM, Herber RF, Broersen S, Zielhuis RL. Work hygienic behaviour as modifier of the lead air-lead blood relation. Int Arch Occup Environ Health. 1990;62(3):203–7. doi: 10.1007/BF00379433. [DOI] [PubMed] [Google Scholar]
- 45.Cherrie JW, Semple S, Christopher Y, Saleem A, Hughson GW, Philips A. How important is inadvertent ingestion of hazardous substances at work? Ann Occup Hyg. 2006;50(7):693–704. doi: 10.1093/annhyg/mel035. [DOI] [PubMed] [Google Scholar]
- 46.Laidlaw MAS, Filippelli G, Mielke H, Gulson B, Ball AS. Lead exposure at firing ranges—a review. Environmental Health. 2017;16(1):34. doi: 10.1186/s12940-017-0246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Beaucham C, Page E, Alarcon WA, Calvert GM, Methner M, Schoonover TM. Indoor firing ranges and elevated blood lead levels-United States, 2002–2013. MMWR Morb Mortal Wkly Rep. 2014;63:347–351. [PMC free article] [PubMed] [Google Scholar]
- 48.National Shooting Sports Foundation. Lead Management and OSHA Compliance for Indoor Shooting Ranges. 2011. [Google Scholar]
- 49.US Department of Health and Human Services. Report to Congress on Workers’ Home Contamination Study Conducted Under The Workers’ Family Protection Act (29 U.S.C. 671a) 1995. [Google Scholar]
- 50.Baker EL, Folland DS, Taylor TA, Frank M, Peterson W, Lovejoy G, et al. Lead poisoning in children of lead workers: home contamination with industrial dust. N Engl J Med. 1977;296(5):260–1. doi: 10.1056/NEJM197702032960507. [DOI] [PubMed] [Google Scholar]
- 51.Take-home lead exposure among children with relatives employed at a battery recycling facility - Puerto Rico, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(47):967–70. [PubMed] [Google Scholar]
- 52.Aguilar-Garduño C, Lacasaña M, Tellez-Rojo MM, Aguilar-Madrid G, Sanin-Aguirre LH, Romieu I, et al. Indirect lead exposure among children of radiator repair workers. American Journal of Industrial Medicine. 2003;43(6):662–667. doi: 10.1002/ajim.10204. [DOI] [PubMed] [Google Scholar]
- 53.Roscoe RJ, Gittleman JL, Deddens JA, Petersen MR, Halperin WE. Blood lead levels among children of lead-exposed workers: A meta-analysis. American journal of industrial medicine. 1999;36(4):475–481. doi: 10.1002/(sici)1097-0274(199910)36:4<475::aid-ajim9>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 54.Lidsky TI, Schneider JS. Lead neurotoxicity in children: basic mechanisms and clinical correlates. Brain. 2003;126(1):5. doi: 10.1093/brain/awg014. [DOI] [PubMed] [Google Scholar]
- 55.Ettinger AS, Lamadrid-Figueroa H, Tellez-Rojo MM, Mercado-Garcia A, Peterson KE, Schwartz J, et al. Effect of calcium supplementation on blood lead levels in pregnancy: a randomized placebo-controlled trial. Environ Health Perspect. 2009;117(1):26–31. doi: 10.1289/ehp.11868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Grandjean P, Landrigan PJ. Developmental neurotoxicity of industrial chemicals. The Lancet. 2006;368(9553):2167–2178. doi: 10.1016/S0140-6736(06)69665-7. [DOI] [PubMed] [Google Scholar]
- 57.Lanphear BP, Hornung R, Khoury J, Yolton K, Baghurst P, Bellinger DC, et al. Low-Level Environmental Lead Exposure and Children’s Intellectual Function: An International Pooled Analysis. Environmental Health Perspectives. 2005;113(7):894–899. doi: 10.1289/ehp.7688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Needleman HL, Schell A, Bellinger D, Leviton A, Allred EN. The long-term effects of exposure to low doses of lead in childhood: an 11-year follow-up report. New England journal of medicine. 1990;322(2):83–88. doi: 10.1056/NEJM199001113220203. [DOI] [PubMed] [Google Scholar]
- 59.Bellinger DC, Stiles KM, Needleman HL. Low-level lead exposure, intelligence and academic achievement: a long-term follow-up study. Pediatrics. 1992;90(6):855–861. [PubMed] [Google Scholar]
- 60.Centers for Disease Control and P. Report of Advisory Committee on Childhood Lead Poisoning Prevention. Atlanta, GA: CDC; 2012. Low level lead exposure harms children: a renewed call for primary prevention. [Google Scholar]
- 61.Gilbert SG, Weiss B. A rationale for lowering the blood lead action level from 10 to 2 microg/dL. Neurotoxicology. 2006;27(5):693–701. doi: 10.1016/j.neuro.2006.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schnaas L, Rothenberg SJ, Flores MF, Martinez S, Hernandez C, Osorio E, et al. Reduced intellectual development in children with prenatal lead exposure. Environ Health Perspect. 2006;114(5):791–7. doi: 10.1289/ehp.8552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.29 CFR 570.2. In.
- 64.29 CFR 570.50–68. In.
- 65.Lanphear BP, Dietrich K, Auinger P, Cox C. Cognitive deficits associated with blood lead concentrations <10 microg/dL in US children and adolescents. Public Health Reports. 2000;115(6):521–529. doi: 10.1093/phr/115.6.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Casey BJ, Giedd JN, Thomas KM. Structural and functional brain development and its relation to cognitive development. Biological Psychology. 2000;54(1):241–257. doi: 10.1016/s0301-0511(00)00058-2. [DOI] [PubMed] [Google Scholar]
- 67.Sowell ER, Thompson PM, Holmes CJ, Jernigan TL, Toga AW. In vivo evidence for post-adolescent brain maturation in frontal and striatal regions. Nature neuroscience. 1999;2(10):859–861. doi: 10.1038/13154. [DOI] [PubMed] [Google Scholar]
- 68.Karasz HN. Q and A: Public Health Takes on Lead Poisoning at Work. Public Health Insider. 2016 Sect. https://publichealthinsider.com/2016/10/19/qa-public-health-takes-on-lead-poisoning-at-work/
- 69.Public Health King County. Updating the Occupational Lead Standards in Washington State. Seattle, WA: 2016. http://www.lni.wa.gov/Safety/Rules/WhatsNew/LeadSafety/pdfs/OccupationalLeadStandardsObjective.pdf. [Google Scholar]
- 70.City of Seattle Office of Planning and Community Development. About Seattle: Race and Ethnicity. 2010. [Google Scholar]
- 71.Hayes P. Soiza A, editor. Public Health - Seattle and King County: Requested updates to Washington state’s occupational lead standards. 2016 http://www.lni.wa.gov/Safety/Rules/WhatsNew/LeadSafety/pdfs/SeattleKingCountyLeadRuleRecommendations.pdf.
- 72.Vork K, Carlisle J, Brown JP. Estimating Workplace Air and Worker Blood Lead Concentration using an Updated Physiologically-based Pharmacokinetic (PBPK) Model. Office of Environmental Health Hazard Assessment (OEHHA), California Environmental Protection Agency; 2013. [Google Scholar]
- 73.Landrigan PJ, Goldman LR. Children’s vulnerability to toxic chemicals: a challenge and opportunity to strengthen health and environmental policy. Health Affairs. 2011;30(5):842–850. doi: 10.1377/hlthaff.2011.0151. [DOI] [PubMed] [Google Scholar]
- 74.Reuben A, Caspi A, Belsky DW, et al. Association of childhood blood lead levels with cognitive function and socioeconomic status at age 38 years and with iq change and socioeconomic mobility between childhood and adulthood. JAMA. 2017;317(12):1244–1251. doi: 10.1001/jama.2017.1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bellinger DC. Childhood lead exposure and adult outcomes. JAMA. 2017;317(12):1219–1220. doi: 10.1001/jama.2017.1560. [DOI] [PubMed] [Google Scholar]
- 76.Ruiz-Hernandez A, Kuo C-C, Rentero-Garrido P, Tang W-Y, Redon J, Ordovas JM, et al. Environmental chemicals and DNA methylation in adults: a systematic review of the epidemiologic evidence. Clinical epigenetics. 2015;7(1):55. doi: 10.1186/s13148-015-0055-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gilbert SG. Epigenetics, the Environment, and Children’s Health Across Lifespans. Springer; 2016. Ethical Implications of Epigenetics; pp. 327–334. [Google Scholar]
- 78.Dupont. Safety Data Sheet 7484. In; 2016.
- 79.Holland MG, Cawthon D. Workplace lead exposure. Journal of occupational and environmental medicine. 2016;58(12):e371–e374. doi: 10.1097/JOM.0000000000000928. [DOI] [PubMed] [Google Scholar]


