Abstract
The practice of transferring patients between acute care hospitals is variable and largely non-standardized. Though often cited reasons for transfer include providing patients access to specialty services only available at the receiving institution, little is known about whether and when patients receive such specialty care during the transfer continuum. We performed a retrospective analysis using 2013 100% Master Beneficiary Summary and Inpatient claims files from CMS. Beneficiaries were included if they were age ≥ 65, continuously enrolled in Medicare A and B, with an acute care hospitalization claim, and transferred to another acute care hospital with a primary diagnosis of acute myocardial infarction, gastrointestinal bleed, renal failure, or hip fracture/dislocation. Associated specialty procedure codes (ICD-9 CM) were identified for each diagnosis. We performed descriptive analyses to compare receipt of specialty procedural services between transferring and receiving hospitals, stratified by diagnosis. Across the 19,613 included beneficiaries, receipt of associated specialty procedures was more common at the receiving than the transferring hospital, with the exception of patients with a diagnosis of gastrointestinal bleed. Depending on primary diagnosis, between 32.4% and 89.1% of patients did not receive any associated specialty procedure at the receiving hospital. Our results demonstrate variable receipt of specialty procedural care across the transfer continuum, implying the likelihood of alternate drivers of inter-hospital transfer other than solely receipt of specialty procedural care.
Keywords: Patient Safety, Care Transitions, Inter-hospital transfer
Introduction
Patients who undergo inter-hospital transfer (IHT), are felt to benefit from receipt of unique specialty care at the receiving hospital.1 Though only 1.5% of all hospitalized Medicare patients undergo hospital transfer,2 the frequency of transfer is much greater within certain patient populations, as may be expected with diagnoses requiring specialty care.3–4 Existent data demonstrate that 5% of Medicare patients admitted to the intensive care unit5 and up to 50% of patients presenting with acute myocardial infarction (AMI) undergo IHT.6
More recent data suggest variability in hospital transfer practices not accounted for by differences in patient or hospital characteristics.2 Although disease-specific guidelines for IHT exist for certain diagnoses,3–4 the process remains largely non-standardized for many patients,7 leading to ambiguity surrounding indications for transfer. As limited data suggest worse outcomes for transferred versus non-transferred patients,8 a better understanding of the specialized care patients actually receive across the transfer continuum may help to elucidate potential indications for transfer, and ultimately help delineate which patients are most (or least) likely to benefit from transfer and why.
In this national study, we examined a select cohort of transferred patients with diagnoses associated with specific specialty procedural services, to determine if they received these procedures, and where along the transfer continuum they were performed.
Methods
We performed a cross-sectional analysis using the Center for Medicare and Medicaid Services (CMS) 2013 100% Master Beneficiary Summary and Inpatient claims files. Our study protocol was approved by the Partners Healthcare Human Subjects Review Committee.
Beneficiaries were eligible for inclusion if they were age ≥ 65 years, continuously enrolled in Medicare A and B, with an acute care hospitalization claim in 2013, excluding Medicare managed care and end stage renal disease (ESRD) beneficiaries, due to incomplete claims data in these groups. We additionally excluded beneficiaries hospitalized at federal or non-acute care hospitals, or critical access hospitals given their mission to stabilize and then transfer patients to referral hospitals.9
Transferred patients were defined as beneficiaries with corresponding “transfer in” and “transfer out” claims, or those with either claim and a corresponding date of admission/discharge from another hospital within 1 date of the claim, as we used in our prior research.2 Beneficiaries transferred to the same hospital, those with greater than one transfer within the same hospitalization, or those cared for at hospitals with “outlier” transfer in rates equal to 100% or transfer out rates greater than 35% were excluded from analysis given the suggestion of non-standard claims practices.
We first identified the top 15 primary diagnoses at time of transfer using ICD-9 codes (Appendix), and then identified those four most likely to require specialty procedural services: AMI, Gastrointestinal bleed (GI bleed), Renal failure, and Hip fracture/dislocation. We then chose associated ICD-9 procedure codes for each diagnosis, via expert opinion (authors SM, JS, hospitalist physicians with greater than 20 years of combined clinical experience), erring on over-inclusion of procedure codes. We then quantified receipt of associated procedures at transferring and receiving hospitals, stratified by diagnosis.
We further explored the cohort of patients with hip fracture/dislocation who underwent a associated procedure at the transferring but not receiving hospital, examining the frequency with which these patients had other (non-related) procedures at the receiving hospital, and identifying which procedures they received.
Results
Of the 101,507 patients transferred to another hospital, 19,613 (19.3%) had a primary diagnosis of AMI, GI bleed, Renal failure, or Hip fracture/dislocation. Table 1 lists the ICD-9 procedure codes associated with each diagnosis.
Table 1.
Associated Specialty Procedures for Diagnoses of Transferred Patients
| Primary Diagnosis, n(%) | † Transferred Patients(n=19,613) | Associated ICD-9 Procedure Code | Description | ‡ Associated Procedures at Transferring Hospital, n (%) | ‡ Associated Procedures at Receiving Hospital, n (%) |
|---|---|---|---|---|---|
| Acute Myocardial Infarction | 12,780 (65.2) | CM 36 | Operations on vessels of heart | 56 (1.4) | 2868 (47.4) |
| CM 37 | Other operations on heart and pericardium | 3480 (88.5) | 2846 (47.1) | ||
| CM 39.6 | Extracorporeal circulation and procedures auxiliary to heart surgery | 2 (0.05) | 27 (0.4) | ||
| CM 88.4 | Arteriography using contrast material | 19 (0.5) | 9 (0.1) | ||
| CM 88.5 | Angiocardiography using contrast material | 189 (4.8) | 227 (3.8) | ||
| CM 89.4 | Cardiac stress tests, pacemaker and defibrillator checks | 35 (0.9) | 20 (0.3) | ||
| CM 89.5 | Other non-operative cardiac and vascular diagnostic procedures | 89 (2.3) | 7 (0.1) | ||
| CM 92 | Nuclear medicine | 8 (0.2) | 2 (0.03) | ||
| CM 99.6 | Conversion of cardiac rhythm | 56 (1.4) | 40 (0.7) | ||
| Gastrointestinal Bleed | 3,014 (15.4) | CM 39.98 | Control of hemorrhage, not otherwise specified | 3 (0.1) | 8 (0.4) |
| CM 39.1 | Intra-abdominal venous shunt (TIPS) | 0 (0) | 11 (0.6) | ||
| CM 42 | Operations on esophagus | 32 (1.4) | 48 (2.5) | ||
| CM 43 | Incision and excision of stomach | 15 (0.6) | 54 (2.8) | ||
| CM 44 | Other operations on stomach (including endoscopy) | 237 (10.1) | 289 (15.2) | ||
| CM 45 | Incision, excision and anastomosis of intestine (including colonoscopy) | 1074 (45.9) | 1183 (62.1) | ||
| CM 46 | Other operations on intestine | 1 (0.04) | 11 (0.6) | ||
| CM 48 | Operations on rectum, rectosigmoid and perirectal tissue | 13 (0.6) | 22 (1.2) | ||
| CM 49 | Operations on anus | 4 (0.2) | 7 (0.4) | ||
| CM 54 | Other operations on abdominal region | 6 (0.3) | 28 (1.5) | ||
| CM 88.4 | Arteriography using contrast material | 17 (0.7) | 38 (2.0) | ||
| CM 89.5 | Other non-operative cardiac and vascular diagnostic procedures | 7 (0.3) | 1 (0.05) | ||
| CM 92 | Nuclear medicine | 4 (0.2) | 3 (0.2) | ||
| CM 96.3 | Non-operative alimentary tract irrigation, cleaning and local instillation | 1 (0.04) | 0 (0) | ||
| CM 99.0 | Transfusion of blood and blood components | 928 (39.6) | 200 (10.5) | ||
| Renal Failure | 2,148 (11.0) | CM 39.95 | Hemodialysis | 39 (27.9) | 80 (34.0) |
| CM 54.95 | Peritoneal dialysis | 0 (0) | 0 (0) | ||
| CM 55 | Operations on kidney (including biopsy) | 29 (20.7) | 96 (40.9) | ||
| CM 56 | Operations on ureter | 3 (2.1) | 9 (3.8) | ||
| CM 57 | Operations on urinary bladder | 57 (40.7) | 39 (16.6) | ||
| CM 58 | Operations on urethra | 4 (2.9) | 3 (1.3) | ||
| CM 87.71-87.79 | X-ray of urinary system | 8 (5.7) | 8 (3.4) | ||
| Hip Fracture/Dislocation | 1,671 (8.5) | CM 78 | Other Operations On Bones, Except Facial Bones | 29 (7.3) | 72 (6.4) |
| CM 79 | Reduction of fracture and dislocation | 218 (55.1) | 555 (49.2) | ||
| CM 80 | Incision and excision of joint structures | 0 (0) | 1 (0.09) | ||
| CM 81 | Repair and plastic operations on joint structures | 149 (37.6) | 501 (44.4) |
Of the 101,507 transferred patients, 19,613 (19.3%) had a primary diagnosis of AMI, GI bleed, Renal failure, or Hip fracture/dislocation
Indicates the number of patients receiving each procedure at transferring and receiving hospitals. Percentages reflect column percentages for each diagnosis.
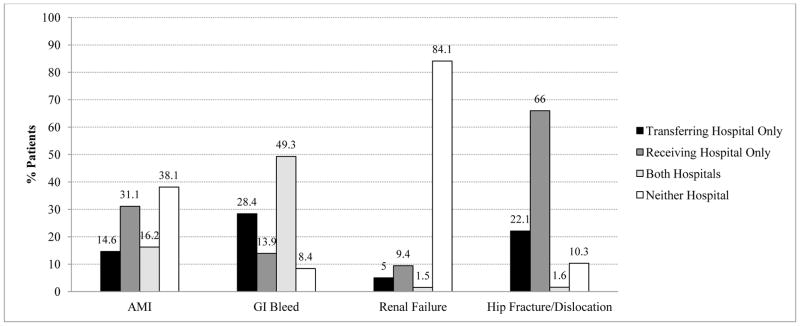
Distribution of receipt of specialty procedures at the transferring and receiving hospitals varied by disease (Figure 1). With the exception of GI Bleed, patients more often received specialty procedural care at the receiving than the transferring hospital. Depending on primary diagnosis, between 32.4% and 89.1% of patients did not receive any associated specialty procedure at the receiving hospital.
Figure 1.
Frequency of Disease-specific Procedures at Transferring and Receiving Hospitals
Of the 370 (22.1%) hip fracture/dislocation patients that received a specialty procedure at the transferring but not receiving hospital, 132 (35.7%) did not receive any procedure at the receiving hospital, while the remaining 238 (64.3%) received an unrelated (not associated with the primary diagnosis) procedure. There was great variety in the types of procedures received, the most common being transfusion of blood products (ICD-9 CM 9904).
Discussion
Among transferred patients with primary diagnoses that have clearly associated specialized procedural services, we found that patients received these procedures at varying frequency and location across the transfer continuum. Across four diagnoses, receipt of associated procedures was more common at the receiving than the transferring hospital with the exception being patients with GI bleed. We additionally found that many transferred patients did not receive any associated specialty procedure at the receiving hospital. These findings suggest the strong likelihood of more diverse underlying reasons for transfer rather than solely receipt of specialized procedural care.
Despite the frequency with which AMI patients are transferred,6 and American Heart Association guidelines directing hospitals to transfer AMI patients to institutions able to provide necessary invasive treatments,4 prior studies suggest these patients inconsistently receive specialty intervention following transfer, including stress testing, cardiac catheterization, or coronary artery bypass graft surgery.10–11 Our findings add to these data, demonstrating that only 47.3% of patients transferred with AMI received any cardiac-related procedure at the receiving hospital. Additionally, we found that 38.1% of AMI patients do not receive any specialty procedures at either the transferring or the receiving hospital. Taken together, these data suggest possible discrepancies in the perceived need for these procedures between transferring and receiving hospitals, reasons for transfer related to these conditions that don’t involve an associated procedure, or reasons for transfer unrelated to specialty care of the primary diagnosis (such as care of comorbidities, hospital location, prior relationships with that hospital, or desire for a second opinion). Although some of these alternate reasons for transfer likely still benefit the patient, some of these reasons may not justify the increased risks of discontinuity of care created by IHT.
Given limited data looking at IHT practices for patients with other diagnoses, the varying patterns of specialty procedural interventions we observed among transferred patients with GI bleed, renal failure, and hip fracture/dislocation are novel contributions to this topic. Notably, we found that among patients transferred with a primary diagnosis of renal failure, the vast majority (84.1%) did not receive any associated procedure at either the transferring or the receiving hospital. It is possible that although these patients carried the diagnosis of renal failure, their clinical phenotype is more heterogeneous, and they could still be managed conservatively without receipt of invasive procedures such as hemodialysis.
Conversely, patients transferred with primary diagnosis of hip fracture/dislocation were far more likely to receive associated specialty procedural intervention at the receiving hospital, presumably reflective of the evidence demonstrating improved outcomes with early surgical intervention.12 However, these data do not explain the reasoning behind the substantial minority of patients who received specialty intervention at the transferring hospital prior to transfer or those that did not receive any specialty intervention at either the transferring or receiving hospital. Our secondary analysis demonstrating great variety in receipt and type of non-associated procedures provided at the receiving hospital did not help to elucidate potential underlying reasons for transfer.
Notably, among patients transferred with primary diagnosis of GI bleed, receipt of specialty procedures was more common at the transferring (77.7%) than receiving (63.2%) hospital, with nearly half (49.3%) undergoing specialty procedures at both hospitals. It is possible that these findings are reflective of the broad array of specialty procedures examined within this diagnosis. For example, it is reasonable to consider that a patient may be stabilized with receipt of a blood transfusion at the transferring hospital, then transferred to undergo a diagnostic/therapeutic procedure (i.e., endoscopy/colonoscopy) at the receiving hospital, as is suggested by our results.
Our study is subject to several limitations. First, given the criteria we used to define transfer, it is possible that we included non-transferred patients within our transferred cohort if they were discharged from one hospital and admitted to a different hospital within 1 day, though quality assurance analyses we conducted in prior studies on these data support the validity of the criteria used.2 Second, we cannot exclude the possibility that patients received non-procedural specialty care (i.e., expert opinion, specialized imaging, medical management, management of secondary diagnoses, etc.) not available at the transferring hospital, although arguably, in select patients such input could be obtained without physical transfer of the patient (i.e., tele-consult). And even in patients transferred with intent to receive procedural care who did not ultimately receive that care, there is likely an appropriate “non-procedure” rate, where patients who might benefit from a procedure receive a timely evaluation to reduce the risk of missing the opportunity to receive it. This would be analogous to transferring a patient to an ICU even if they do not end up requiring intubation or pressor therapy. However, given the likelihood of higher risks of IHT compared with intra-hospital transfers, one could argue that the threshold of perceived benefit might be different in patients being considered for IHT. Additionally, we limited our analyses to only four diagnoses; thus, our findings may not be generalizable to other diagnoses of transferred patients. However, because the diagnoses we examined were ones considered most effectively treated with specialty procedural interventions, it is reasonable to presume that the variability in receipt of specialty procedures observed within these diagnoses is also present, if not greater, across other diagnoses. Third, although we intentionally included a broad array of specialty procedures associated with each diagnosis, it is possible that we overlooked particular specialty interventions. For example, in assuming that patients are most likely to be transferred to receive procedural services associated with their primary diagnosis, we may have missed alternate indications for transfer, including need for procedural care related to secondary or subsequent diagnoses (i.e., a patient may have presented with GIB in the context of profound anemia that requires a bone marrow biopsy for diagnosis, and thus was transferred for the biopsy). Our further examination of unrelated procedures received by hip fracture/dislocation patients at receiving hospitals argues against a select or subset of procedures driving transfers that are not associated with the primary diagnosis, but does not fully rule out this possibility (i.e., if there are a large variety of secondary diagnoses with distinct associated specialty procedures that are required for each). Lastly, though our examination provides novel information regarding variability in receipt of specialty procedures of transferred patients, we were not able to identify exact reasons for transfer. Instead, our results are hypothesis generating and require further investigation to better understand these reasons.
Conclusions
In conclusion, we found that Medicare patients who undergo IHT with primary diagnoses of AMI, GI bleed, renal failure, and hip fracture/dislocation receive associated specialty interventions at varying frequency and location, and many patients do not receive any associated procedures at receiving hospitals. Our findings suggest that specialty procedural care of patients, even those with primary diagnoses that often warrant specialized intervention, may not be the primary driver of inter-hospital transfer as commonly suggested, although underlying reasons for transfer in these and other “non-procedural” transferred patients remains obscure. Given known ambiguity in the transfer process,7 and unclear benefit of IHT,8 additional research is required to further identify and evaluate other potential underlying reasons for transfer, and to examine these in the context of patient outcomes, in order to understand which patients may or may not benefit from transfer and why.
Supplementary Material
Footnotes
Authors’ Conflict of Interest Disclosures:
Dr. Mueller has nothing to disclose.
Ms. Zheng has nothing to disclose.
Dr. Orav has nothing to disclose.
Dr. Schnipper has nothing to disclose.
References
- 1.Iwashyna TJ. The incomplete infrastructure for interhospital patient transfer. Crit Care Med. 2012 Aug;40(8):2470–2478. doi: 10.1097/CCM.0b013e318254516f. [DOI] [PubMed] [Google Scholar]
- 2.Mueller SK, Zheng J, Orav EJ, Schnipper JL. Rates, Predictors and Variability of Interhospital Transfers: A National Evaluation. J Hosp Med. 2017 Jun;12(6):435–442. doi: 10.12788/jhm.2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guidelines for the transfer of critically ill patients. Guidelines Committee of the American College of Critical Care Medicine; Society of Critical Care Medicine and American Association of Critical-Care Nurses Transfer Guidelines Task Force. Crit Care Med. 1993 Jun;21(6):931–937. [PubMed] [Google Scholar]
- 4.Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, Jr, Chavey WE, 2nd, Fesmire FM, Hochman JS, Levin TN, Lincoff AM, Peterson ED, Theroux P, Wenger NK, Wright RS, Smith SC., Jr 2011 ACCF/AHA Focused Update Incorporated Into the ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011 May 10;123(18):e426–579. doi: 10.1161/CIR.0b013e318212bb8b. [DOI] [PubMed] [Google Scholar]
- 5.Iwashyna TJ, Christie JD, Moody J, Kahn JM, Asch DA. The structure of critical care transfer networks. Med Care. 2009 Jul;47(7):787–793. doi: 10.1097/MLR.0b013e318197b1f5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iwashyna TJ, Kahn JM, Hayward RA, Nallamothu BK. Interhospital transfers among Medicare beneficiaries admitted for acute myocardial infarction at nonrevascularization hospitals. Circ Cardiovasc Qual Outcomes. 2010 Sep;3(5):468–475. doi: 10.1161/CIRCOUTCOMES.110.957993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bosk EA, Veinot T, Iwashyna TJ. Which patients and where: a qualitative study of patient transfers from community hospitals. Med Care. 2011 Jun;49(6):592–598. doi: 10.1097/MLR.0b013e31820fb71b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sokol-Hessner L, White AA, Davis KF, Herzig SJ, Hohmann SF. Interhospital transfer patients discharged by academic hospitalists and general internists: Characteristics and outcomes. J Hosp Med. 2015 Nov 20; doi: 10.1002/jhm.2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Department of Health and Human Services, Center for Medicare & Medicaid Services. [Accessed June 29, 2017];Critical Access Hospitals. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/CritAccessHospfctsht.pdf.
- 10.Roe MT, Chen AY, Delong ER, Boden WE, Calvin JE, Jr, Cairns CB, Smith SC, Jr, Pollack CV, Jr, Brindis RG, Califf RM, Gibler WB, Ohman EM, Peterson ED. Patterns of transfer for patients with non-ST-segment elevation acute coronary syndrome from community to tertiary care hospitals. Am Heart J. 2008 Jul;156(1):185–192. doi: 10.1016/j.ahj.2008.01.033. [DOI] [PubMed] [Google Scholar]
- 11.Barreto-Filho JA, Wang Y, Rathore SS, Spatz ES, Ross JS, Curtis JP, Nallamothu BK, Normand SL, Krumholz HM. Transfer rates from nonprocedure hospitals after initial admission and outcomes among elderly patients with acute myocardial infarction. JAMA Intern Med. 2014 Feb 1;174(2):213–222. doi: 10.1001/jamainternmed.2013.11944. [DOI] [PubMed] [Google Scholar]
- 12.Doruk H, Mas MR, Yildiz C, Sonmez A, Kyrdemir V. The effect of the timing of hip fracture surgery on the activity of daily living and mortality in elderly. Arch Gerontol Geriatr. 2004 Sep-Oct;39(2):179–185. doi: 10.1016/j.archger.2004.03.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.