Abstract
Background: There is uncertainty regarding which factors are associated with in-hospital mortality among patients with pulmonary TB (PTB). The aim of this systematic review and meta-analysis is to identify predictors of in-hospital mortality among patients with PTB. Methods: We searched MEDLINE, EMBASE, and Global Health, for cohort and case-control studies that reported risk factors for in-hospital mortality in PTB. We pooled all factors that were assessed for an association, and presented relative associations as pooled odds ratios (ORs). Results: We identified 2,969 records, of which we retrieved 51 in full text; 11 cohort studies that evaluated 5,468 patients proved eligible. Moderate quality evidence suggested an association with co-morbid malignancy and in-hospital mortality (OR 1.85; 95% CI 1.01–3.40). Low quality evidence showed no association with positive sputum smear (OR 0.99; 95% CI 0.40–2.48), or male sex (OR 1.09, 95% CI 0.84–1.41), and very low quality evidence showed no association with diabetes mellitus (OR 1.31, 95% IC 0.38–4.46), and previous TB infection (OR 2.66, 95% CI 0.48–14.87). Conclusion: Co-morbid malignancy was associated with increased risk of in-hospital death among pulmonary TB patients. There is insufficient evidence to confirm positive sputum smear, male sex, diabetes mellitus, and previous TB infection as predictors of in-hospital mortality in TB patients.
Introduction
Tuberculosis (TB) continues to be a major public health issue worldwide, particularly in low and middle-income countries despite rigorous efforts to contain its spread and implementation of effective treatment strategies. In 2014 an estimated 12 million people worldwide were living with active pulmonary TB, with 9.6 million new cases and 1.5 million deaths due to TB occurring annually1–7.
TB does not usually require hospital admission for treatment, but if symptoms such as shortness of breath, and deterioration in a systemic condition are present, hospitalization may be necessary. A large proportion of patients with TB are hospitalized8,9, and estimates of in-hospital mortality range from 2% to 12%10–14; most of the current costs of TB treatment result from hospitalization15.
A variety of predictors have been associated with a greater risk of death among TB patients, including poverty, homelessness, alcohol or drug addiction, irregular or inadequate treatment, late diagnosis of the disease, multidrug-resistant TB (MDR-TB), and advanced age4,6. Human immunodeficiency virus (HIV) infection is an important factor related to the increased morbidity and mortality of TB in different world regions4,10. In addition, diabetes has been reported to be associated with increased risk of mortality16–18. Also, men have higher rates of mortality and worse outcomes compared with women19,20. Previous TB with multiple treatments has also been associated with in-hospital mortality21–23. Furthermore, patients with malignant tumors are immunocompromised and can have unusual clinical presentations, both related to delayed diagnosis and high mortality24–26.
In TB program monitoring, TB deaths are crucial indicators of the impact of TB control measures10–14, especially in areas with high HIV and TB prevalence. Data on TB deaths should provide us with a better understanding of the factors associated with these deaths and help guide interventions to reduce mortality; however, there is uncertainty regarding which factors are associated with in-hospital mortality among patients with pulmonary TB10.
We therefore conducted a systematic review and meta-analysis to establish predictors of in-hospital mortality among patients with pulmonary TB.
Methods
Search strategy
We used a multimodal search strategy focused on 3 bibliographical databases (MEDLINE, EMBASE and Global Health). An experienced librarian (RC) used medical subject headings, adding terms and keywords from a preliminary search to develop the database search strategies. In each database, the librarian used an iterative process to refine the search strategy through testing several search terms and incorporating new search terms as new relevant citations were identified. There were no language restrictions. The search included the following databases from inception to November 2015: MEDLINE, EMBASE and Global Health. The search consisted of three concepts combined using the AND operator1: tuberculosis2, hospitalization and3 mortality (Appendix 1). The protocol of this study was published elsewhere27.
Study selection
Eligibility criteria
Eligible trials met the following criteria1: cohort or case-control design2; explored risk factors for in-hospital mortality among patients with pulmonary TB in an adjusted analysis.
Assessment of study eligibility
Two reviewers (CPBA and DRS) trained in health research methodology screened, independently and in duplicate, the titles and abstracts of all citations identified in our search. The same reviewers screened all full text articles for eligibility; disagreements were resolved by consensus, with consultation of a third investigator (JWB) when resolution could not be achieved. We measured agreement between reviewers with the kappa statistic to assess the reliability of full-text review using the guidelines proposed by Landis and Koch28: <0.20 as slight agreement, 0.21–0.40 as fair agreement, 0.41–0.60 as moderate agreement, 0.61–0.80 as substantial agreement and >0.80 as almost perfect agreement.
Assessment of study quality
Two reviewers (CPBA and DRS) assessed risk of bias for each eligible study, independently and in duplicate, using the Newcastle-Ottawa quality assessment scale (NOS) for Cohort Studies29. The scale consists of nine items that cover three dimensions1: patient selection (4 items)2; comparability of cohorts on the basis of the design or analysis (2 items); and3 assessment of outcome (3 items). A point is awarded for each item that is satisfied by the study. The total score therefore ranges from zero to nine, with higher scores indicating higher quality. A total score ≥7 represents high quality.
Data Extraction and Analysis
Two reviewers (CPBA and DRS) extracted data from each eligible study, including demographic information (e.g. sex, age, race), methodology, and all reported predictors.
We performed meta-analysis for all predictors that were reported by more than one study. We used odds ratios (ORs) with associated 95% CI to measure the association of binary predictors and in-hospital mortality. We used random effects models for all meta-analyses. If a study reported more than 1 regression model, we used data from the most fully adjusted model presented. We also presented the results from the predictors explored by the studies but that were not eligible for meta-analysis.
We evaluated heterogeneity for all pooled estimates through visual inspection of forest plots, because statistical tests of heterogeneity can be misleading when sample sizes are large and CIs are therefore narrow30. We used the software R.
Publication bias
For meta-analyses with at least 10 studies, we assessed publication bias by visual assessment of asymmetry of the funnel plot and performed the Begg rank correlation test31.
Quality of evidence
We used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to summarize the quality of evidence for all meta-analyses32. We categorized the confidence in estimates (quality of evidence) as high, moderate, low or very low, on the basis of risk of bias33, imprecision34, indirectness, inconsistency35 and publication bias36. We used GRADE evidence profiles to provide a succinct, easily digestible presentation of the quality of evidence and magnitude of associations32. In case of doubt or missing details about the studies, authors were contacted for clarification.
Ethics and Dissemination
This study is based on published data, and therefore ethical approval was not a requirement. This systematic review and meta-analysis is expected to serve as a basis for evidence to reduce in-hospital mortality in TB patients, and as a guide for future research based on identified knowledge gaps. It is anticipated that findings from this review will be useful for informing policy, practice and research priorities, improving the management of in-hospital TB patients. We also plan to update the review in the future to monitor changes and guide health services and policy solutions.
Results
Search Results and Study Characteristics
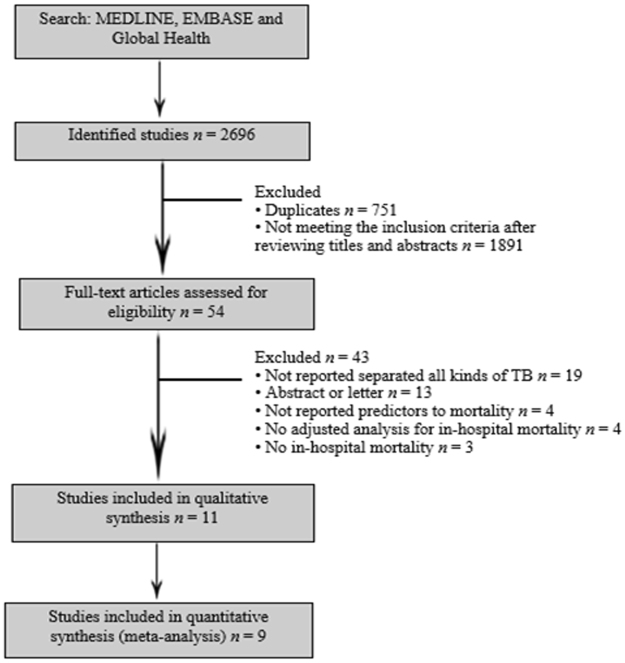
We identified 2,969 unique records, of which we retrieved 51 English and 3 non-English language articles in full text; 11 cohort studies, published between 2003 and 2013, that evaluated 5,468 patients proved eligible. Figure 1 shows the study selection flow diagram. There was substantial agreement (κ = 0.64) at the titles and abstract screening stage and perfect agreement (κ = 1.00) between reviewers at the full-text review stage.
Figure 1.
Flow diagram of study selection.
All 11 eligible studies1,4,15,37–44 were single-center and there was one non-English (Chinese) study included in our analysis. Two studies38,42 were conducted in Japan, two40,41 in Taiwan, three15,39,43 in Korea, one37 in Germany, one4 in Israel, one1 in Iran and one44 in China. One study39 used TB-related mortality as defined by the World Health Organization (the number of TB patients who died during treatment, irrespective of cause)45, two38,42 used all-cause mortality, and eight1,4,15,37,40,41,43,44 used TB-related mortality as judged by the investigators. The majority (9 of 11)1,4,15,37,39–41,43,44 acquired data from medical records, with eight retrospective cohorts1,4,37–42 and one prospective cohort study15 (Table 1).
Table 1.
Studies describing in-hospital mortality among pulmonary tuberculosis patients.
| First author, reference | Year of publication | Definition of TB death* | Country | Sample size | No. Deaths (%) | Predictors |
|---|---|---|---|---|---|---|
| Alavi-Naini1 | 2013 | Investigators judgment of TB death | Iran | 715 | 75 (13.9%) | Smoking, hepatites, DM, Hx of previous TB, anemia, drug abuse, positive sputum smear |
| Erbes37 | 2006 | Investigators judgment of TB death | Germany | 58 | 15 (25.9%) | Acute renal failure, mechanical ventilation, pneumonia, chronic pancreatitis, sepsis, ARDS |
| Horita38 | 2012 | All-cause mortality | Japan | 244 | 48 (19.7%) | Age, oxygen requirement, albumin, ADL |
| Kim15 | 2010 | Investigators judgment of TB death | Korea | 156 | 21 (13.5%) | Male sex, old age, underprivileged, predisposing factors, AFB smear, CRP, lung involvement, high NRS |
| Kim39 | 2012 | WHO definition | Korea | 269 | 82 (30.5%) | Admission Route, AFB Smear Positivity, albumin, BUN, creatinine, CRP, Drug-resistance TB, general weakness, Hb, hx of stopping anti-TB medication, hospital length of stay, initial ICU care, lymphocyte, poor oral intake, severity on chest X-ray, sodium, total cholesterol, under treatment for TB, WBC |
| Lee40 | 2003 | Investigators judgment of TB death | Taiwan | 41 | 27 (64.8%) | Multiple organ failure, consolidation on chest X-ray |
| Lin41 | 2009 | Investigators judgment of TB death | Taiwan | 59 | 40 (67.8%) | Acute renal failure, gastrointestinal bleeding, multi-organ dysfunction syndrome, nosocomial pneumonia, treatment delay > 30 days |
| Lubart4 | 2007 | Investigators judgment of TB death | Israel | 461 | 65 (14%) | Older age, IHD, cachexia, corticosteroid use, low albumin level |
| Okamura42 | 2013 | All-cause mortality | Japan | 246 | 27 (11%) | Serum Albumin, total lymphocite – cat 1, total limphocite – cat2, total limphocite – cat3 |
| Ryu43 | 2006 | Investigators judgment of TB death | Korea | 32 | 16 (50%) | APACHE II, sepsis, tuberculous-destroyed lungs |
| Sun44 | 2011 | Investigators judgment of TB death | China | 62 | 36 (58%) | APACHE II, liver damage, respiratory failure, fungal infection |
ADL = activities of daily living; APACHE II = Acute Physiology and Chronic Health Evaluation; ARDS = acute respiratory distress syndrome; DM = Diabetes Mellitus; Hx = history; IHD = ischemic heart disease; TB = tuberculosis; PTB = pulmonary TB; NR = Not reported; WHO = World Health Organization.
Risk of bias
Overall, the quality, evaluated by the NOS checklist for the outcome “mortality”, was high (Table 2). We did not have a sufficient number of studies in our meta-analyses to assess publication bias.
Table 2.
Newcastle-Ottawa scoring system for cohort studies.
Predictors of in-hospital mortality
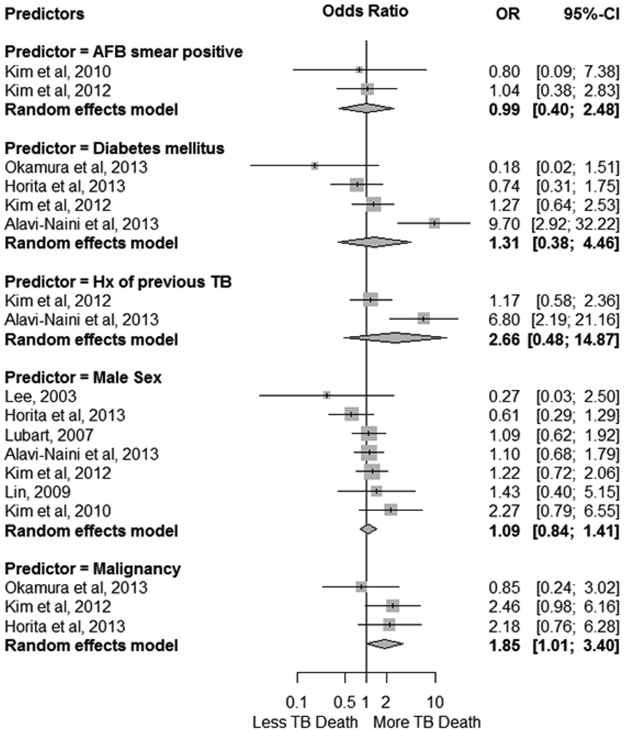
A total of 11 studies, involving a total of 2343 patients, reported the association of 60 factors with in-hospital mortality1,4,15,37–42. On the basis of our criteria, we conducted meta-analyses for 5 predictors of in-hospital mortality1: acid-fast bacilli (AFB) smear positive2, diabetes mellitus3, malignancy4, history of previous TB, and5 male sex.
Moderate quality evidence showed a significant association between malignancy and in-hospital mortality among TB patients (OR 1.85; 95% CI 1.01–3.40). Low quality evidence showed no association between in-hospital mortality and AFB smear positive test (OR 0.99; 95% CI 0.40–2.48), or male sex (OR 1.09; 95% CI 0.84–1.41). Very low quality evidence showed no association between mortality and diabetes mellitus (OR 1.31; 95% CI 0.38–4.46), or previous TB (OR 2.66; 95% CI: 0.48–14.87) (Fig. 2; Table 3).
Figure 2.
Association between AFB smear positive, Diabetes Mellitus, Hx of previous TB, Malignancy, male sex and in-hospital mortality among pulmonary TB patients.
Table 3.
GRADE Evidence Profile: Predictors of in-hospital mortality among TB patients.
| Predictor/Time/N° of patients | N° of studies | Risk of bias | Inconsistancy | Indirectness | Imprecision | Quality | Relative effect (95% CI) |
|---|---|---|---|---|---|---|---|
| AFB smear positive/At baseline/1116 patients | 2 | No serious risk of bias | No serious inconsistancy | No serious indirectness | Serious imprecision | Low | OR 0.99 (0.40–2.48) |
| DM/At baseline/2165 patients | 4 | No serious risk of bias | Serious inconsistancy | No serious indirectness | Serious imprecision | Very low | OR 1.31 (0.38–4.46) |
| Hx of previous TB/At baseline/1675 patients | 2 | No serious risk of bias | Serious inconsistancy | No serious indirectness | Serious imprecision | Very low | OR 2.66 (0.48–14.87) |
| Male sex/At baseline/1880 patients | 7 | No serious risk of bias | No serious inconsistancy | No serious indirectness | Serious imprecision | Low | OR 1.09 (0.84–1.41) |
| Malignancy/At baseline/694 patients | 3 | No serious risk of bias | No serious inconsistancy | No serious indirectness | No serious imprecision | Moderate | OR 1.85 (1.01–3.40) |
*DM = Diabetes Mellitus; Hx = history.
Table 4 presents the associations with in-hospital mortality for the factors that were not amenable to meta-analysis.
Table 4.
Unpooled predictors for in-hospital mortality among TB patients.
| Predictors | OR/HR* | p-value |
|---|---|---|
| Sociodemographic factors | ||
| Age (for 1 year increase) | — | 0.007 |
| Old age (>65 years) | 5.7 (0.8–38.9) | 0.076 |
| Older age | — | <0.001 |
| Underprivileged | 4.1 (0.8–21.4) | 0.098 |
| Substance use | ||
| Drug abusers | 7.8 (2.4–25.5) | 0.008 |
| Smoking | 12.9 (3.9–27.3) | 0.001 |
| Previous TB | ||
| Tuberculous-destroyed lungs | 6.61 (1.21–36.04)* | 0.029 |
| History of stopping anti-TB medication | 4.58 (0.90–23.38) | 0.068 |
| Symptoms | ||
| General weakness | 1.23 (0.35–4.32) | 0.744 |
| Cachexia | — | <0.001 |
| Chest X-ray | ||
| Consolidation | 7.73 (1.03–57.68)* | 0.046 |
| Extensive radiographic lung involvement | 5.0 (0.6–42.8) | 0.140 |
| Severity on chest X-ray - Mild | 1.00 | 0.796 |
| Severity on chest X-ray -Moderate | 1.63 (0.34–7.83) | 0.543 |
| Severity on chest X-ray - Severe | 1.37 (0.26–7.16) | 0.706 |
| Laboratorial exams | ||
| Sputum AFB smear >3 | 2.00 (0.59–6.75)* | 0.264 |
| Multidrug-resistant tuberculosis | 2.65 (0.28–25.33)* | 0.397 |
| Drug-resistance TB | 2.06 (0.69–6.11) | 0.195 |
| Hb | 1.20 (0.40–1.60) | 0.742 |
| Lymphocyte | 1.99 (0.79–4.97) | 0.143 |
| WBC | 2.06 (0.89–4.78) | 0.091 |
| Total Lymphocite – cat 1 | 1.00 | — |
| Total Limphocite – cat 2 | 0.13 (0.03–0.59) | 0.010 |
| Total Limphocite – cat 3 | 0.46 (0.13–1.65) | 0.235 |
| Albumin | 1.76 (0.68–4.53) | 0.245 |
| Serum Albumin | 0.15 (0.06–0.37) | <0.0001 |
| Albumin (for 1 g/dl increase) | 0.22 (–) | 0.003 |
| Low albumin level | — | <0.001 |
| CRP, g/L | 1.00 (0.87–1.15) | 0.883 |
| CRP, mg/dL | 1.62 (0.38–6.95) | 0.517 |
| BUN | 3.23 (1.23–8.49) | 0.018 |
| Creatinine | 2.00 (0.60–6.64) | 0.256 |
| Sodium | 2.48 (0.99–6.21) | 0.052 |
| Total cholesterol | 0.87 (0.18–4.11) | 0.857 |
| Findings during hospitalization | ||
| Admission Route | 0.83 (0.33–2.08) | 0.695 |
| Initial admission ward - ICU | 6.17 (2.08–18.32) | 0.001 |
| Under treatment for PTB at admission | 3.35 (1.12–9.99) | 0.030 |
| APACHE II score | 4.91 (1.99–12,11)* | <0.01 |
| APACHE II score >20 | 4.90 (1.43–16.80)* | 0.012 |
| Treatment delay >30 days | 2.37 (0.49–69.4) | — |
| Nosocomial pneumonia | 5.77 (1.33–44.36) | — |
| Nosocomial pneumonia | — | 0.002 |
| Respiratory failure | 4.03 (1.56–10.38)* | <0.01 |
| Drug hepatitis | 12.3 (6.7–24.7) | 0.001 |
| Liver damage | 3.96 (1.23–12.1)* | <0.05 |
| Gastrointestinal bleeding | 0.5 (0.203–26.18) | — |
| Acute renal failure | 0.6 (0.215–7.15) | — |
| Acute renal failure | — | 0.001 |
| Fungal infection | 3.44 (1.23–9.62)* | <0.05 |
| Multiple organ failure | 0.60 (0.14–2.60)* | 0.495 |
| Multi-organ dysfunction syndrome | 8.59 (1.85–101.27) | — |
| Multiple organ failure | 2.65 (1.16–6.04)* | 0.020 |
| Sepsis | 5.84 (1.63–20.95)* | 0.007 |
| Sepsis | — | 0.001 |
| Hospital length of stay | 1.51 (0.58–3.91) | 0.395 |
| Anemia | 19.8 (5.6–35.5) | <0.0001 |
| Oxygen requirement | 2.29 (−) | 0.132 |
| Mechanical ventilation | — | 0.002 |
| Chronic pancreatitis | — | 0.001 |
| ARDS | — | 0.008 |
| IHD | — | <0.001 |
| Other | ||
| Poor oral intake | 0.94 (0.24–3.71) | 0.930 |
| Activity of Daily living (for 1 point increase) | 0.58 (−) | 0.141 |
| High NRS | 23.5 (2.9–194.2) | 0.003 |
| Predisposing factors | 9.1 (1.5–56.8) | 0.019 |
| Corticosteroid use | — | <0.001 |
Discussion
We found moderate quality evidence that co-morbid malignancy was associated with increased in-hospital mortality among TB patients. Low quality evidence showed that sex and AFB smear positive were not associated with in-hospital mortality, and very low quality evidence showed no association with previous TB infection and diabetes mellitus.
Our review has a number of strengths. Our search, which had no language restrictions, was designed and implemented by a research librarian, and literature screening and data extraction were performed independently and in duplicate by two reviewers using pretested, standardized extraction forms. The main limitation of our review was the small numbers of events that contributed to our meta-analyses, resulting in wide estimates of precision for our pooled measures of association.
Other studies24–26 also found that malignancy increases the risk of death in TB patients. Patients with malignant tumors are immunocompromised due to the local or systemic effects of the disease itself, as well as to the treatment regimens, which can impair the immune system and make these patients particularly susceptible to developing TB46. In addition, TB can have an unusual clinical presentation, making diagnosis more difficult in these patients, contributing to delay in diagnosis and high mortality rates47,48.
While not significantly associated with mortality in our review, previous TB has been reported to be associated with in-hospital mortality in many studies1,21–23. Patients who undergo multiple treatment regimens for TB can develop resistance to drugs with the subsequent emergence of MDR-TB and XDR-TB, conditions highly associated with greater risk of death21. Further, in settings other than hospitals, studies49,50 have demonstrated that smear positive patients have a better prognosis regarding mortality than smear negative patients. Indeed, indicators of atypical manifestations, such as smear-negative sputum, were associated with delayed diagnosis and mortality12,51. Recently, a retrospective cohort study from Brazil6 reported a high mortality rate during hospitalization (16.1%), and negative sputum smear microscopy was an in-hospital mortality predictor in the population studied. However, patients with pulmonary and extrapulmonary TB were included in this study.
We did not find a significant association between male sex and in-hospital mortality among pulmonary TB patients. Worldwide TB notification data show that far more men than women have TB7. Some studies showed that mortality rates are higher in females during their reproductive years, but after that they are higher in men19,20.
Diabetes was also not associated with mortality in pulmonary TB patients in this study. Only one study1 included in this meta-analysis showed that diabetes was a predictor of mortality in TB patients, possibly because they included a larger number of diabetes patients (18% of the enrolled individuals). Some studies1,16–18 have found that diabetes increases risk of early mortality during TB treatment. This effect may be explained by impaired TB treatment response16.
In conclusion, the presence of malignancy was significantly associated with in-hospital death in pulmonary TB patients. Other predictors were not associated with in-hospital mortality in TB patients, probably due to the small number of events. Further research should explore promising predictors of in-hospital mortality in large prospective studies.
Electronic supplementary material
Acknowledgements
For screening the full text of a Korean article, the authors thank Eunji Park, Institute for Evidence based Medicine, The Korean Branch of the Australasian Cochrane Center, Seoul, Korea. No financial compensation was provided to Eunji Park. This study was supported by Fundo de Incentivo à Pesquisa (FIPE)/Hospital de Clínicas de Porto Alegre (HCPA). Carlos Podalirio Borges de Almeida is supported by a Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (Capes). For helping with the forms and the protocol, the authors thank Samantha Craigie, The Michael G. DeGroote Institute for Pain Research and Care, McMaster University, Hamilton, Ontario, Canada.
Author Contributions
All authors made substantial contributions to conception and design. C.P.B.A. designed the study, collected data, and wrote the manuscript. R.C. designed the search strategy. L.W. designed the study and collected data. P.Z. analyzed data and wrote the paper. J.B. designed the study and wrote the paper. D.R.S. designed the study, collected data, and wrote the paper. All authors provided final approval of the version to be published.
Competing Interests
The authors declare no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-25409-5.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Alavi-Naini R, Moghtaderi A, Metanat M, Mohammadi M, Zabetian M. Factors associated with mortality in tuberculosis patients. J Res Med Sci. 2013;18(1):52–55. [PMC free article] [PubMed] [Google Scholar]
- 2.Haque G, et al. Prognostic factors in tuberculosis related mortalities in hospitalized patients. Tuberc Res Treat. 2014;2014:624671. doi: 10.1155/2014/624671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lawn SD, Zumla AI. Tuberculosis. Lancet. 2011;378(9785):57–72. doi: 10.1016/S0140-6736(10)62173-3. [DOI] [PubMed] [Google Scholar]
- 4.Lubart E, Lidgi M, Leibovitz A, Rabinovitz C, Segal R. Mortality of patients hospitalized for active tuberculosis in Israel. Isr Med Assoc J. 2007;9(12):870–873. [PubMed] [Google Scholar]
- 5.Lui G, et al. High mortality in adults hospitalized for active tuberculosis in a low HIV prevalence setting. PLoS One. 2014;9(3):e92077. doi: 10.1371/journal.pone.0092077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Silva DR, Menegotto DM, Schulz LF, Gazzana MB, Dalcin PT. Factors associated with mortality in hospitalized patients with newly diagnosed tuberculosis. Lung. 2010;188(1):33–41. doi: 10.1007/s00408-009-9224-9. [DOI] [PubMed] [Google Scholar]
- 7.WHO. Global Tuberculosis Report 2015. Geneva: World Health Organization. Available at: www.who.int (2015).
- 8.Silva DR, Silva LP, Dalcin PT. Tuberculosis in hospitalized patients: clinical characteristics of patients receiving treatment within the first 24 h after admission. J Bras Pneumol. 2014;40(3):279–285. doi: 10.1590/S1806-37132014000300011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sreeramareddy CT, Panduru KV, Menten J, Van, den Ende J. Time delays in diagnosis of pulmonary tuberculosis: a systematic review of literature. BMC Infect Dis. 2009;9:91. doi: 10.1186/1471-2334-9-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hansel NN, Merriman B, Haponik EF, Diette GB. Hospitalizations for tuberculosis in the United States in 2000: predictors of in-hospital mortality. Chest. 2004;126(4):1079–1086. doi: 10.1378/chest.126.4.1079. [DOI] [PubMed] [Google Scholar]
- 11.Hansel NN, Wu AW, Chang B, Diette GB. Quality of life in tuberculosis: patient and provider perspectives. Qual Life Res. 2004;13(3):639–652. doi: 10.1023/B:QURE.0000021317.12945.f0. [DOI] [PubMed] [Google Scholar]
- 12.Rao VK, Iademarco EP, Fraser VJ, Kollef MH. The impact of comorbidity on mortality following in-hospital diagnosis of tuberculosis. Chest. 1998;114(5):1244–1252. doi: 10.1378/chest.114.5.1244. [DOI] [PubMed] [Google Scholar]
- 13.Singleton L, et al. Long-term hospitalization for tuberculosis control. Experience with a medical-psychosocial inpatient unit. JAMA. 1997;278(10):838–842. [PubMed] [Google Scholar]
- 14.Greenaway C, et al. Delay in diagnosis among hospitalized patients with active tuberculosis–predictors and outcomes. Am J Respir Crit Care Med. 2002;165(7):927–933. doi: 10.1164/ajrccm.165.7.2107040. [DOI] [PubMed] [Google Scholar]
- 15.Kim HJ, et al. The impact of nutritional deficit on mortality of in-patients with pulmonary tuberculosis. Int J Tuberc Lung Dis. 2010;14(1):79–85. [PubMed] [Google Scholar]
- 16.Faurholt-Jepsen D, et al. Diabetes is a strong predictor of mortality during tuberculosis treatment: a prospective cohort study among tuberculosis patients from Mwanza, Tanzania. Trop Med Int Health. 2013;18(7):822–829. doi: 10.1111/tmi.12120. [DOI] [PubMed] [Google Scholar]
- 17.Reed GW, et al. Impact of diabetes and smoking on mortality in tuberculosis. PLoS One. 2013;8(2):e58044. doi: 10.1371/journal.pone.0058044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Workneh MH, Bjune GA, Yimer SA. Diabetes mellitus is associated with increased mortality during tuberculosis treatment: a prospective cohort study among tuberculosis patients in South-Eastern Amahra Region, Ethiopia. Infect Dis Poverty. 2016;5(1):22. doi: 10.1186/s40249-016-0115-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holmes CB, Hausler H, Nunn P. A review of sex differences in the epidemiology of tuberculosis. Int J Tuberc Lung Dis. 1998;2(2):96–104. [PubMed] [Google Scholar]
- 20.Weiss MG, Sommerfeld J, Uplekar MW. Social and cultural dimensions of gender and tuberculosis. Int J Tuberc Lung Dis. 2008;12(7):829–830. [PubMed] [Google Scholar]
- 21.Chung-Delgado K, Guillen-Bravo S, Revilla-Montag A, Bernabe-Ortiz A. Mortality among MDR-TB cases: comparison with drug-susceptible tuberculosis and associated factors. PLoS One. 2015;10(3):e0119332. doi: 10.1371/journal.pone.0119332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.de Faria Gomes NM, et al. Differences between Risk Factors Associated with Tuberculosis Treatment Abandonment and Mortality. Pulm Med. 2015;2015:546106. doi: 10.1155/2015/546106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pepper DJ, Schomaker M, Wilkinson RJ, de AV, Maartens G. Independent predictors of tuberculosis mortality in a high HIV prevalence setting: a retrospective cohort study. AIDS Res Ther. 2015;12:35. doi: 10.1186/s12981-015-0076-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feng JY, et al. Initial presentations predict mortality in pulmonary tuberculosis patients–a prospective observational study. PLoS One. 2011;6(9):e23715. doi: 10.1371/journal.pone.0023715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lin CH, et al. Tuberculosis mortality: patient characteristics and causes. BMC Infect Dis. 2014;14:5. doi: 10.1186/1471-2334-14-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pina JM, et al. [Excess mortality due to tuberculosis and factors associated to death in and annual cohort of patients diagnosed of tuberculosis] Rev Clin Esp. 2006;206(11):560–565. doi: 10.1016/S0014-2565(06)72897-1. [DOI] [PubMed] [Google Scholar]
- 27.Almeida CP, et al. Predictors of in-hospital mortality among patients with pulmonary tuberculosis: a protocol of systematic review and meta-analysis of observational studies. BMJ Open. 2016;6(11):e011957. doi: 10.1136/bmjopen-2016-011957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 29.Wells G. A. et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomised studies in meta-analyses. Ottawa Hospital Research Institute. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (2016).
- 30.Rucker G, Schwarzer G, Carpenter JR, Schumacher M. Undue reliance on I(2) in assessing heterogeneity may mislead. BMC Med Res Methodol. 2008;8:79. doi: 10.1186/1471-2288-8-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 32.Atkins D, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guyatt GH, et al. GRADE guidelines: 4. Rating the quality of evidence–study limitations (risk of bias). J Clin Epidemiol. 2011;64(4):407–415. doi: 10.1016/j.jclinepi.2010.07.017. [DOI] [PubMed] [Google Scholar]
- 34.Guyatt GH, et al. GRADE guidelines 6. Rating the quality of evidence–imprecision. J Clin Epidemiol. 2011;64(12):1283–1293. doi: 10.1016/j.jclinepi.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 35.Guyatt GH, et al. GRADE guidelines: 7. Rating the quality of evidence–inconsistency. J Clin Epidemiol. 2011;64(12):1294–1302. doi: 10.1016/j.jclinepi.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 36.Guyatt GH, et al. GRADE guidelines: 5. Rating the quality of evidence–publication bias. J Clin Epidemiol. 2011;64(12):1277–1282. doi: 10.1016/j.jclinepi.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 37.Erbes R, et al. Characteristics and outcome of patients with active pulmonary tuberculosis requiring intensive care. Eur Respir J. 2006;27(6):1223–1228. doi: 10.1183/09031936.06.00088105. [DOI] [PubMed] [Google Scholar]
- 38.Horita N, et al. Development and validation of a tuberculosis prognostic score for smear-positive in-patients in Japan. Int J Tuberc Lung Dis. 2013;17(1):54–60. doi: 10.5588/ijtld.12.0476. [DOI] [PubMed] [Google Scholar]
- 39.Kim CW, et al. Risk factors related with mortality in patient with pulmonary tuberculosis. Tuberc Respir Dis (Seoul) 2012;73(1):38–47. doi: 10.4046/trd.2012.73.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee PL, et al. Patient mortality of active pulmonary tuberculosis requiring mechanical ventilation. Eur Respir J. 2003;22(1):141–147. doi: 10.1183/09031936.03.00038703. [DOI] [PubMed] [Google Scholar]
- 41.Lin SM, et al. Predictive factors for mortality among non-HIV-infected patients with pulmonary tuberculosis and respiratory failure. Int J Tuberc Lung Dis. 2009;13(3):335–340. [PubMed] [Google Scholar]
- 42.Okamura K, et al. Hypoalbuminemia and lymphocytopenia are predictive risk factors for in-hospital mortality in patients with tuberculosis. Intern Med. 2013;52(4):439–444. doi: 10.2169/internalmedicine.52.8158. [DOI] [PubMed] [Google Scholar]
- 43.Ryu YJ, et al. Prognostic factors in pulmonary tuberculosis requiring mechanical ventilation for acute respiratory failure. Respirology. 2007;12(3):406–411. doi: 10.1111/j.1440-1843.2006.01007.x. [DOI] [PubMed] [Google Scholar]
- 44.Sun J, Fang K, Ren DH, Sheng XL. [A study of the prognostic factors associated with mortality in critically ill patients with tuberculous] Zhonghua Jie He He Hu Xi Za Zhi. 2011;34(1):39–42. [PubMed] [Google Scholar]
- 45.Who. World Health Organization. Global Tuberculosis Programme. A framework for effective tuberculosis control. WHO/TB/94. 179. Geneva, Switzerland. Available at: www.who.int (1994).
- 46.Kamboj M, Sepkowitz KA. The risk of tuberculosis in patients with cancer. Clin Infect Dis. 2006;42(11):1592–1595. doi: 10.1086/503917. [DOI] [PubMed] [Google Scholar]
- 47.Kim HR, et al. Solid-organ malignancy as a risk factor for tuberculosis. Respirology. 2008;13(3):413–419. doi: 10.1111/j.1440-1843.2008.01282.x. [DOI] [PubMed] [Google Scholar]
- 48.Silva FA, Matos JO, de QMF, Nucci M. Risk factors for and attributable mortality from tuberculosis in patients with hematologic malignances. Haematologica. 2005;90(8):1110–1115. [PubMed] [Google Scholar]
- 49.Balabanova Y, et al. The Directly Observed Therapy Short-Course (DOTS) strategy in Samara Oblast, Russian Federation. Respir Res. 2006;7:44. doi: 10.1186/1465-9921-7-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dewan PK, et al. Risk factors for death during tuberculosis treatment in Orel, Russia. Int J Tuberc Lung Dis. 2004;8(5):598–602. [PubMed] [Google Scholar]
- 51.Naalsund A, Heldal E, Johansen B, Kongerud J, Boe J. Deaths from pulmonary tuberculosis in a low-incidence country. J Intern Med. 1994;236(2):137–142. doi: 10.1111/j.1365-2796.1994.tb01275.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.