Abstract
To explore the pathogenic mechanism of diabetic gastropathy, we investigated differences in response to electrical field stimulation (EFS) of gastric muscles from diabetic and non-diabetic (control) patients. Gastric specimens were obtained from 34 patients and 45 controls who underwent gastrectomy for early gastric cancer. Using organ bath techniques, we examined peak and nadir values of contraction under EFS. To examine responses to purinergic and nitrergic inhibition without cholinergic innervation, atropine, MRS2500, and N-nitro-L-arginine (L-NNA) were added sequentially to the organ bath. Tetrodotoxin (TTX) was used to confirm that the responses to EFS were mediated via neural stimulation. In the absence of pharmacological agents, peak contraction amplitude was greater in non-diabetic controls compared to diabetics only in the distal longitudinal gastric muscles. However, the nadir was greater in controls than in patients in both proximal and distal gastric circular muscles. Addition of MRS2500 could not decrease the nadir in both controls and patients, both in the proximal and distal stomach. However, L-NNA completely reversed the relaxation. TTX had no further effect on nadir. In conclusion, impaired inhibitory nitrergic neural pathway in both proximal and distal stomach and impaired excitatory cholinergic neural pathway in the distal stomach may contribute to the pathogenic mechanism underlying diabetic gastropathy.
Introduction
Diabetes mellitus (DM) is associated with an increased prevalence of upper gastrointestinal symptoms. Symptoms attributable to gastroparesis are reported in 5 to 12% of patients with DM1,2. Gastroparesis is characterized by abnormal gastric function resulting in delayed gastric emptying3. Pathogenic mechanisms proposed to underlie delayed gastric emptying in DM include autonomic neuropathy, loss of neuronal nitric oxide synthase (nNOS) expression, loss of interstitial cells of Cajal (ICC), low level of antioxidant heme oxygenase-1, and loss of CD206-positive anti-inflammatory macrophages4–15.
Loss of nNOS expression and loss of ICC are the most consistent findings in diabetic gastroparesis16–18. Loss of nNOS itself may not lead to a development of delayed gastric emptying as sildenafil does not improve gastric emptying in patients with diabetic gastroparesis19. In streptozotocin-induced diabetic rats, nitrergic gastric relaxation correlates better with the active dimeric form of nNOS rather than absolute nNOS levels20. Thus, post-translational modification may be important. Loss of ICC correlates with development of delayed gastric emptying in humans with diabetic gastroparesis as well as in animal models6,17,18,21,22. In a retrospective study using paraffin-embedded gastric specimens, decreased expression of nNOS and substance P (SP) was accompanied by loss of ICC levels in patients with DM6. Gastroparesis Clinical Research Consortium study using prospectively collected specimens also reported that loss of ICC is associated with delayed gastric emptying17. Immune cells also play a role in the development of diabetic gastroparesis. CD206-positive HO-1 expressing M2 macrophages show a protective effect against diabetic gastroparesis in mice14. A recent human study also demonstrates a correlation between ICC and CD206-positive anti-inflammatory macrophage numbers suggesting that loss of ICC may be the result of loss of the macrophage subtype15.
The studies mentioned above have focused on cellular abnormalities. However, gastric emptying relies on coordinated actions of the proximal and distal stomach, which requires the interplay of the nervous system, smooth muscle, ICCs, and immune cells. Little has been studied on the changes of gastric smooth muscle contractility according to the region of the stomach. In our previous study, we reported that acetylcholine has varying effects on human gastric contractions according to the stomach region23. Based on these observations, we investigated whether DM would affect the contractility of the human stomach with regional differences24. Comparison of spontaneous gastric muscle strip contractions between diabetic patients and control subjects has shown significant differences between them. The diabetic gastric muscle has higher basal tone in the distal stomach than in control muscle, lower frequency of contraction in the distal stomach, and less acetylcholine-induced positive inotropic effect in the proximal stomach. These changes of contractility of diabetic stomach may play a role in pathogenesis of diabetic gastroparesis. To further characterize the contractility of diabetic stomach, we investigated differences in response to electrical field stimulation (EFS) of human gastric muscles between diabetic patients and control subjects.
Results
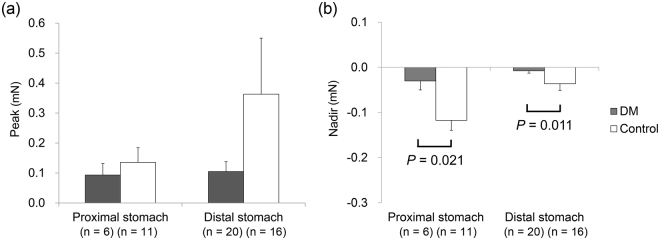
EFS-induced responses in circular muscle strips
Figure 1 shows EFS-induced response of the gastric circular muscle strips in the control state. The peak did not differ between diabetic patients and control subjects in both the proximal and distal stomach. However, the nadir was greater in control subjects than in diabetic patients in both the proximal and distal stomach (−0.12 ± 0.02 mN vs. −0.03 ± 0.02 mN, p = 0.021 and −0.04 ± 0.01 mN vs. −0.01 ± 0.01 mN, p = 0.011, respectively).
Figure 1.
Electrical field stimulation (EFS)-induced response of gastric circular muscle strips in the control state: (a) The peak did not differ between diabetic patients and control subjects. (b) The nadir was greater in control subjects than in diabetic patients.
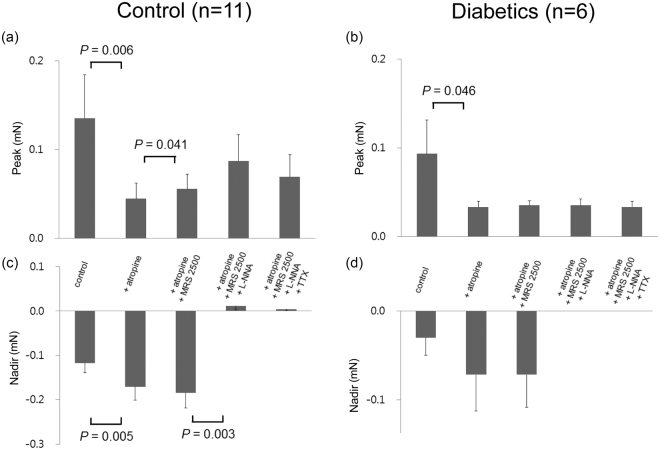
Figure 2 shows EFS-induced response of the proximal gastric circular muscle strips after serial administration of atropine (a muscarinic antagonist, 1 µM), N-nitro-L-arginine (L-NNA, a NO synthase inhibitor, 100 µM), MRS2500 (a purinergic P2Y1 antagonist, 1 µM), and tetrodotoxin (TTX, 1 µM). When atropine was added, the peak was decreased due to inhibition of contraction in both the control subjects and diabetic patients from 0.14 ± 0.05 mN to 0.04 ± 0.02 mN (p = 0.006) and 0.09 ± 0.04 mN to 0.03 ± 0.01 mN (p = 0.046), respectively. Except for the addition of MRS2500, which increased the peak in the control subjects from 0.05 ± 0.02 mN to 0.06 ± 0.02 mN (p = 0.041), addition of MRS2500, L-NNA, and TTX had no significant effect on the peak in both the control subjects and diabetic patients. Atropine also increased the nadir by inhibiting contraction in the control subjects from −0.12 ± 0.02 mN to −0.17 ± 0.30 mN (p = 0.005). Addition of MRS2500 had no effect on the nadir in both the control subjects and diabetic patients. However, L-NNA decreased the nadir by abolishing relaxation in the control subjects from −0.18 ± 0.03 mN to 0.01 ± 0.01 mN (p = 0.003). Also, in the diabetic patients, L-NNA decreased the nadir from −0.07 ± 0.04 mN to 0.00 ± 0.00 mN with marginal statistical significance (p = 0.080). TTX had no further effect on the nadir in both the control subjects and diabetic patients.
Figure 2.
Electrical field stimulation (EFS)-induced response of proximal gastric circular muscle strips after serial administration of atropine, MRS2500, N-nitro-L-arginine (L-NNA), and tetrodotoxin (TTX). (a) Atropine decreased the peak and MRS2500 increased the peak in the control subjects. (b) Atropine decreased the peak in diabetic patients. (c) Atropine increased the nadir and L-NNA abolished relaxation in the control subjects. (d) Also in the diabetic patients, L-NNA decreased the nadir with marginal statistical significance (p = 0.080). The Wilcoxon signed-rank test was used to evaluate the effects of each drug by compare values to the previous one.
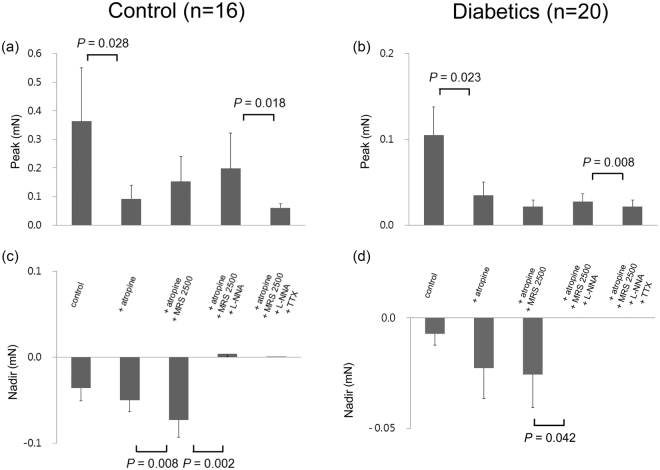
Figure 3 shows EFS-induced response of the distal gastric circular muscle strips after serial administration of atropine, L-NNA, MRS2500, and TTX. When atropine was added, the peak was decreased due to inhibition of contraction in both the control subjects and diabetic patients from 0.36 ± 0.19 mN to 0.09 ± 0.05 mN (p = 0.028) and 0.11 ± 0.03 mN to 0.03 ± 0.02 mN (p = 0.023), respectively. Addition of MRS2500 and L-NNA had no significant effect on the peak in both the control subjects and diabetic patients. However, addition of TTX decreased the peak in the control subjects and diabetic patients from 0.20 ± 0.12 mN to 0.06 ± 0.02 mN (p = 0.018) and 0.03 ± 0.01 mN to 0.02 ± 0.01 mN (p = 0.008), respectively. Addition of MRS2500 increased the nadir from −0.05 ± 0.01 mN to −0.07 ± 0.02 mN (p = 0.008) in the control subjects but did not have the same effect in diabetic patients. However, L-NNA decreased the nadir by abolishing relaxation in both the control subjects and diabetic patients from −0.07 ± 0.02 mN to 0.00 ± 0.00 mN (p = 0.002) and −0.03 ± 0.02 mN to 0.00 ± 0.00 mN (p = 0.042), respectively. TTX had no further effect on the nadir in both the control subjects and diabetic patients.
Figure 3.
Electrical field stimulation (EFS)-induced response of distal gastric circular muscle strips after serial administration of atropine, MRS2500, N-nitro-L-arginine (L-NNA), and tetrodotoxin (TTX). (a and b) Atropine decreased the peak and TTX decreased the peak further in both the control subjects and diabetic patients. (c) MRS2500 increased the nadir but L-NNA abolished relaxation in the control subjects. (d) Also in the diabetic patients, L-NNA abolished relaxation. The Wilcoxon signed-rank test was used to evaluate the effects of each drug by compare values to the previous one.
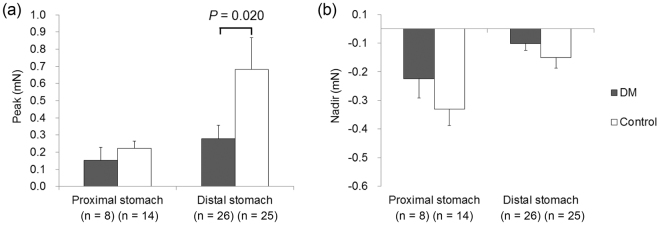
EFS-induced responses in the longitudinal muscle strips
Figure 4 shows EFS-induced response of the gastric longitudinal muscle strips in the control state. The peak did not differ between diabetic patients and control subjects in the proximal stomach but was greater in control subjects than in diabetic patients in the distal stomach (0.68 ± 0.18 vs. 0.28 ± 0.08, p = 0.020). However, the nadir did not differ between diabetic patients and control subjects in both the proximal and distal stomach.
Figure 4.
Electrical field stimulation (EFS)-induced response of gastric longitudinal muscle strips in the control state. (a) The peak did not differ between diabetic patients and control subjects in the proximal stomach but was greater in control subjects than in diabetic patients in the distal stomach. (b) The nadir did not differ between diabetic patients and control subjects in both the proximal and distal stomach.
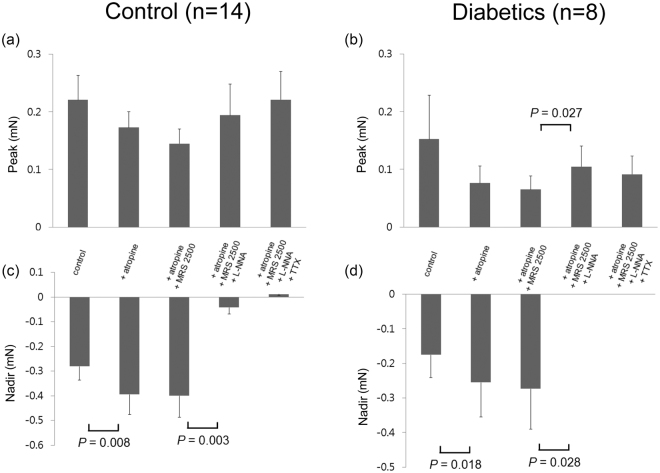
Figure 5 shows EFS-induced response of the proximal gastric longitudinal muscle strips after serial administration of atropine, L-NNA, MRS2500, and TTX. Except for the addition of L-NNA, which increased the peak in the diabetic patients from 0.07 ± 0.02 mN to 0.11 ± 0.04 mN (p = 0.027), addition of atropine, MRS2500, L-NNA, and TTX had no significant effect on the peak in both the control subjects and diabetic patients. Atropine increased the nadir by inhibiting contraction in both the control subjects and diabetic patients from −0.28 ± 0.06 mN to −0.40 ± 0.08 mN (p = 0.008) and −0.18 ± 0.07 mN to −0.26 ± 0.10 mN (p = 0.018), respectively. Addition of MRS2500 had no effect on the nadir in both the control subjects and diabetic patients. However, L-NNA decreased the nadir by abolishing relaxation in both the control subjects and diabetic patients from −0.40 ± 0.09 mN to −0.04 ± 0.03 mN (p = 0.003) and −0.27 ± 0.12 mN to 0.00 ± 0.00 mN (p = 0.028), respectively. TTX had no further effect on the peak in both the control subjects and diabetic patients.
Figure 5.
Electrical field stimulation (EFS)-induced response of the proximal gastric longitudinal muscle strips after serial administration of atropine, MRS2500, N-nitro-L-arginine (L-NNA), and tetrodotoxin (TTX). (a) No significant effects of serial administration of drugs in the control subjects. (b) L-NNA increased the peak in the diabetic patients. (c) Atropine increased the nadir but L-NNA abolished relaxation. (d) Also in the diabetic patients, atropine increased the nadir but L-NNA abolished relaxation. The Wilcoxon signed-rank test was used to evaluate the effects of each drug by compare values to the previous one.
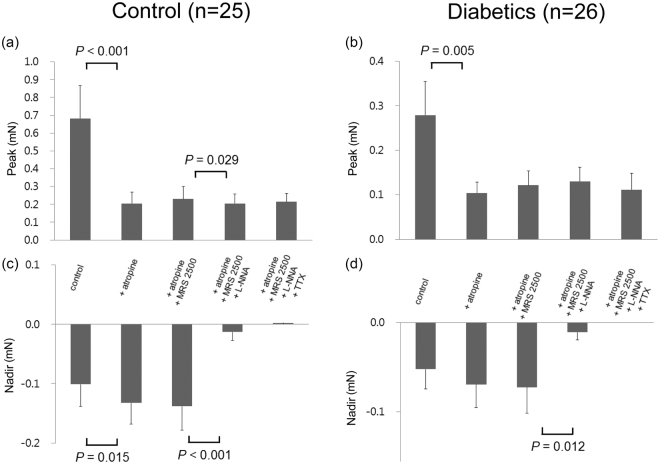
Figure 6 shows EFS-induced response of the distal gastric longitudinal muscle strips after serial administration of atropine, L-NNA, MRS2500, and TTX. When atropine was added, the peak was decreased due to inhibition of contraction in both the control subjects and diabetic patients from 0.68 ± 0.18 mN to 0.21 ± 0.06 mN (p < 0.001) and 0.28 ± 0.08 mN to 0.10 ± 0.02 mN (p = 0.005), respectively. Except for the addition of L-NNA, which decreased the peak in the control subjects from 0.23 ± 0.07 mN to 0.21 ± 0.05 mN (p = 0.029), addition of MRS2500, L-NNA, and TTX had no significant effect on the peak in both the control subjects and diabetic patients. Atropine also increased the nadir by inhibiting contraction in the control subjects from −0.10 ± 0.04 mN to −0.13 ± 0.04 mN (p = 0.015). Addition of MRS2500 had no effect on the nadir in both the control subjects and diabetic patients. However, L-NNA decreased the nadir by abolishing relaxation in both the control subjects and diabetic patients from −0.14 ± 0.04 mN to −0.01 ± 0.01 mN (p < 0.001) and −0.07 ± 0.03 mN to −0.01 ± 0.01 mN (p = 0.012), respectively. TTX had no further effect on the nadir in both the control subjects and diabetic patients.
Figure 6.
Electrical field stimulation (EFS)-induced response of distal gastric longitudinal muscle strips after serial administration of atropine, MRS2500, N-nitro-L-arginine (L-NNA), and tetrodotoxin (TTX). (a) Atropine and L-NNA decreased the peak in the control subjects. (b) Atropine decreased the peak in the diabetic patients. (c) Atropine increased the nadir but L-NNA abolished relaxation in the control subjects. (d) Also in diabetic patients, L-NNA abolished relaxation. The Wilcoxon signed-rank test was used to evaluate the effects of each drug by compare values to the previous one.
Discussion
Gastric dysmotility associated with DM causes considerable morbidity including gastroparesis as its most severe form1,2,25,26. Gastroparesis not only diminishes quality of life but also increases health-care costs27,28. Although understanding the pathogenesis of diabetic gastroparesis at a cellular level has been improved in the past decade, little has been studied on the changes of gastric muscle contractility in humans with DM. In our previous human studies, we demonstrated that acetylcholine has different effects on gastric muscle contractility by the stomach region and DM affects the spontaneous gastric muscle contractility with regional differences23,24. To further characterize the change of gastric muscle contractility in a diabetic condition, we investigated differences in response to EFS of human gastric muscles between patients with DM and control subjects.
In our experiments, EFS of the human gastric muscle strips elicited muscle relaxation. In the control state, the nadir was greater in control subjects than in diabetic patients in both the proximal and distal gastric circular muscle strips, but not in the longitudinal muscle strips. These observations indicate that the diabetic stomach has impaired relaxation especially in the circular muscle layer. The different degree of response between the gastric circular and longitudinal muscle strips is not thought to be due to the small sample size of the longitudinal sample because more strips were obtained from the longitudinal muscle. In the canine stomach, density of nerve fibers was higher in the circular muscle than in the longitudinal muscle, and inhibitory nitrergic nerves constituted a substantial fraction of the enteric nervous system29. NO and nNOS have been consistently observed to be decreased in animal models and in humans with diabetic gastroparesis. Decreased expression of nNOS in the myenteric plexus of gastric of streptozotocin-diabetic rats, and gastric relaxation is hampered mainly by impaired nNOS expression in the gastric myenteric plexus of spontaneously diabetic rats16,30. Iwasaki et al. reported loss of nNOS-positive neurons in patients with severe DM, along with loss of ICCs6. Taken together, impaired nitrergic neural pathway may contribute to the development of diabetic dysmotility.
To investigate responses to the inhibition of purinergic and nitrergic pathways without cholinergic innervation, MRS2500, and L-NNA were added sequentially to the organ bath in the presence of atropine, and EFS was performed. Addition of MRS2500 could not decrease the nadir. However, L-NNA completely reversed the relaxation by inhibiting nitrergic pathway in both the control subjects and diabetic patients. Although the effect was not statistically significant in the proximal circular muscle strips from the diabetic patients, it might be due to the small sample size (n = 6). Addition of TTX confirms that the EFS-induced relaxation was neurally mediated. These observations indicate that the human gastric relaxation is mainly mediated by nitrergic pathway.
Several neurotransmitters have been suggested to be released by inhibitory neurons, including NO31–34, vasoactive intestinal polypeptide35–38, and adenosine triphosphate39,40. From animal studies, conflicting data exist regarding whether NO predominantly mediates the relaxation41–43, or whether NO and vasoactive intestinal polypeptide act as co-transmitters44–47. However, NO is considered the major contributor in the non-adrenergic, non-cholinergic relaxation of the human stomach48–51, which is consistent with our findings in the present study. Pasricha et al. reported that decreased HO-2 immunoreactivity in the stomach of patient with poorly controlled diabetes7. HO, the enzyme that gives rise to carbon monoxide, known to regulate neurotransmission and smooth muscle membrane potential52,53. The authors suggested that combined loss of both inhibitory molecules may cause a profound disturbance of gastric physiology like gastroparesis7. In the control state, the peak was greater in control subjects than in diabetic patients in the distal gastric longitudinal muscle strips. The peak was decreased by the addition of atropine, and sequential addition of MRS2500, L-NNA, and TTX had no further effect on the peak. These observations indicate that the excitatory neural pathway, largely mediated by the cholinergic pathway, is also impaired in the diabetic distal stomach. Indeed, decreased expression of nNOS and SP accompanied by reduced ICC density was observed in the distal stomach of diabetics patients6. However, further studies are necessary to confirm our results.
The present study had some limitations. The clinical data of diabetic patients were limited, and diabetic gastropathy was not confirmed in them. In a population-based cohort study, the cumulative proportions developing gastroparesis over a 10-year period were 5.2% in type 1 DM, 1.0% in type 2 DM, and 0.2% in controls26. However, the prevalence of delayed gastric emptying in patients with diabetes has been reported to be between 28% and 65%54,55. In addition, a half of patients of diabetes have upper gastrointestinal symptoms2,25. Considering the long mean duration of disease (10.9 year) in our diabetic subjects, the observed differences in response to EFS of gastric muscles from diabetic and non-diabetic patients may contribute to the pathogenic mechanisms underlying diabetic gastropathy. Secondly, a majority of the diabetic patients had type 2 DM, and the sample size is rather small to be analyzed in terms of the differences in the stomach region and muscle layer. Nevertheless, to our knowledge, this is the first study comparing the response to EFS in normal and diabetic human stomach muscle. Therefore, our results may be of great importance for understanding the pathophysiology of diabetic gastropathy. In summary, diabetic patients have an impaired inhibitory nitrergic neural pathway in both the proximal and distal stomach and impaired excitatory cholinergic pathway in the distal stomach; these alterations may be the pathogenic mechanism of diabetic gastropathy.
Materials and Methods
Subjects and tissues
Gastric specimens were obtained from 34 diabetic patients (10 women, 24 men; mean age, 67.6 ± 6.3 [SD] years) and 45 control subjects (15 women, 30 men; mean age, 60.4 ± 11.9 years) who underwent gastrectomy for early gastric cancer at Samsung Medical Center, Seoul, Korea. The majority of diabetic patients (97%) had type 2 DM. The mean duration of DM and presence of glycated hemoglobin was 10.9 ± 7.1 years and 6.9% ± 0.9%, respectively. Control subjects did not have a history of DM. None of the control subjects had fasting serum glucose levels over 126 mg dL−1 or was using insulin or oral anti-hyperglycemic agents. No diffuse infiltrative type of gastric cancer was included in this study. None of the diabetic patients and control subjects had pre-operative radiotherapy, irritable bowel syndrome, or neurological disorders. They had no GI disease other than gastric cancer.
Shortly after gastrectomy, gastric muscle strips were excised from areas free of macroscopic evidence of cancer infiltration. The areas where the gastric tissues were removed from were mapped by the performing surgeon into the gastric fundus, corpus, or antrum. The surgeon was instructed regarding mapping of the exact gastric areas prior to the procedure5. The fundus was designated as the proximal stomach and the corpus and antrum as the distal stomach. Fourteen (6 circular and 8 longitudinal) gastric muscle strips from the proximal stomach and 46 (20 circular and 26 longitudinal) from the distal stomach were obtained in diabetic patients and 25 (11 circular and 14 longitudinal) from the proximal stomach and 41 (16 circular and 25 longitudinal) from the distal stomach were obtained in control subjects.
The excised tissues were collected in cold Krebs-Ringer bicarbonate (KRB) solution and transported to laboratory within 10 min after collection. KRB solution had the following composition (in mM): 120.4 NaCl, 5.9 KCl, 1.2 MgCl2, 15.5 NaHCO3, 1.2 KH2PO4, 11.5 dextrose, and 2.5 CaCl2. Tissues were pinned to the base of a Sylgard silicone elastomer (Dow Corning, Midland, MI) dish. The mucosa was removed by sharp dissection. After the mucosa was removed, thin strips of tissues were cut by use of parallel scalpel blades mounted on a scalpel handle. The final strips cut parallel to the muscle fibers measured 2 mm × 10 mm. The muscle strips were isolated and attached to a fixed mount and to a Fort 10 isometric strain gauge (UC3-GOULD Instruments, Paris, France; FT03-GFASS, Warwick, RI). The muscle strips were immersed in organ baths maintained at 37 ± 0.5 °C with oxygenated KRB solution. The pH of the KRB solution was 7.3–7.4 when bubbled with 97% O2-3% CO2 at 37 ± 0.5 °C. This preparation process was performed within 30 min after tissue collection.
The study protocol was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board at Samsung Medical Center, Seoul, Korea. All subjects provided written informed consent before inclusion in the study.
Organ chamber experiments
Experiments were performed in vitro using strips of the human gastric muscle, and their mechanical activity was recorded as changes in isometric force. These experiments were conducted using standard organ bath techniques, as previously described in another study by our group5. The sample strips were equilibrated in the organ baths, which were continuously perfused with oxygenated KRB solution, for 60 mins. Based on our preliminary study (data not shown), all experiments were performed with an optimal degree of passive tension, which was 0.7 g. Changes in tension due to relaxation or contraction of the muscles were recorded through an analog-to-digital board to a computer (Chart5-ADInstruments, Bella Vista, NSW, Australia). Experiments were performed after basal tone was stabilized. Basal tone did not change through the entire experiment with repeated stimulations. Actual peak amplitudes were measured with adjusted baseline using Clampfit software (Molecular Devices, pClamp version 10, Sunnyvale, CA). The lowest value of stabilized spontaneous phasic contractions was defined as baseline (zero point). EFS-induced responses were measured with reference to the baseline. EFS (0.3 ms in trains of 10 Hz for 20 s, 150 V) was applied via two platinum ring electrodes attached to each strip. The electrodes were connected to a GRASS S88 (GRASS Instruments, Quincy, MA) stimulator.
Protocols and measurements
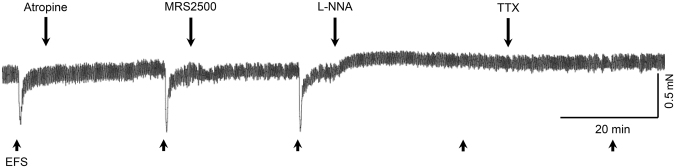
We examined EFS-induced responses for the peak (the highest value) and nadir (the lowest value). The peak and nadir of both circular and longitudinal muscle strips were measured during the first 1 minute after the initiation of EFS (Fig. 7) in control state and after administration of atropine, MRS2500, and N-nitro-L-arginine, which were added in a sequential order to the organ bath (Fig. 8). Then, tetrodotoxin was used to confirm that the responses to EFS were mediated via neural stimulation. The muscle strips were sequentially perfused with each drug for 20 min after EFS and were allowed a recovery time of 5 min.
Figure 7.
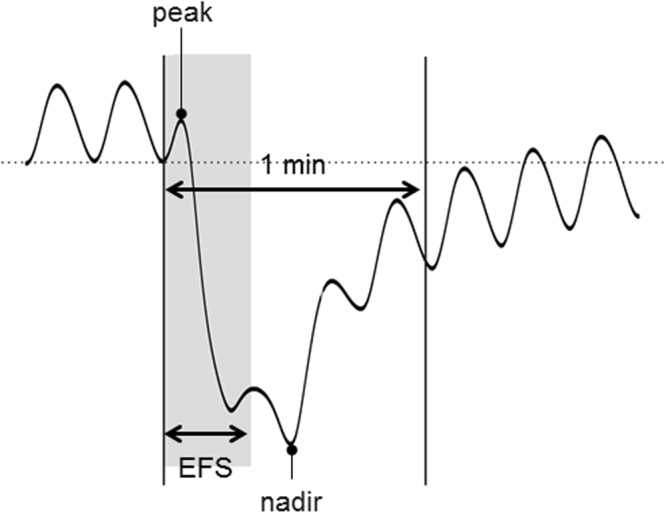
Peak and nadir of the response induced by electrical field stimulation (EFS) of human gastric muscle. Peak is the highest value, while nadir stands for the lowest value during the first 1 minute after the initiation of EFS.
Figure 8.
Typical tracing of electrical field stimulation (EFS)-induced response in gastric circular muscle strips with serial administration of atropine, MRS2500, N-nitro-L-arginine (L-NNA), and tetrodotoxin (TTX). Note the reduction of the relaxation by L-NNA.
Drugs and solutions
Atropine (Sigma Aldrich), MRS2500 (TOCRIS bioscience), L-NNA (Sigma Aldrich), and TTX (Alomone Labs) were used. Atropine, MRS2500, and TTX were dissolved in distilled water, while L-NNA was dissolved in 1 M hydrochloric acid. The stock concentration of L-NNA was 100 mM.
Statistical analysis
Statistical analyses were conducted using SPSS version 21 (SPSS IBM, NY, USA). Experimental data are shown as mean ± SE. Mann-Whitney U-test was used to compare responses to EFS between control subjects and diabetic patients. Wilcoxon signed ranks test was used to evaluate changes in peak and nadir of EFS-induced contractile responses after sequential exposure to drugs. A two-sided P value < 0.05 was taken as statistically significant.
Author Contributions
Guarantor of the article: Poong-Lyul Rhee. Yang Won Min contributed to data analysis and wrote the paper. Eun-Ju Ko and Ji-Yeon Lee performed laboratory experiments. Poong-Lyul Rhee designed and coordinated the study, contributed to data interpretation and edited the manuscript. All authors approved the final version of the manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Maleki D, et al. Gastrointestinal tract symptoms among persons with diabetes mellitus in the community. Archives of internal medicine. 2000;160:2808–2816. doi: 10.1001/archinte.160.18.2808. [DOI] [PubMed] [Google Scholar]
- 2.Bytzer P, et al. Prevalence of gastrointestinal symptoms associated with diabetes mellitus: a population-based survey of 15,000 adults. Archives of internal medicine. 2001;161:1989–1996. doi: 10.1001/archinte.161.16.1989. [DOI] [PubMed] [Google Scholar]
- 3.Camilleri, M., Bharucha, A. E. & Farrugia, G. Epidemiology, mechanisms, and management of diabetic gastroparesis. Clin Gastroenterol Hepatol9, 5–12; quiz e17 (2011). [DOI] [PMC free article] [PubMed]
- 4.Kashyap P, Farrugia G. Diabetic gastroparesis: what we have learned and had to unlearn in the past 5 years. Gut. 2010;59:1716–1726. doi: 10.1136/gut.2009.199703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sinn DH, et al. Regional differences of the effects of acetylcholine in the human gastric circular muscle. American journal of physiology. Gastrointestinal and liver physiology. 2010;299:G1198–1203. doi: 10.1152/ajpgi.00523.2009. [DOI] [PubMed] [Google Scholar]
- 6.Iwasaki H, et al. A deficiency of gastric interstitial cells of Cajal accompanied by decreased expression of neuronal nitric oxide synthase and substance P in patients with type 2 diabetes mellitus. J Gastroenterol. 2006;41:1076–1087. doi: 10.1007/s00535-006-1909-8. [DOI] [PubMed] [Google Scholar]
- 7.Pasricha PJ, et al. Changes in the gastric enteric nervous system and muscle: a case report on two patients with diabetic gastroparesis. BMC Gastroenterol. 2008;8:21. doi: 10.1186/1471-230X-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park KS, et al. Characterization of smooth muscle, enteric nerve, interstitial cells of Cajal, and fibroblast-like cells in the gastric musculature of patients with diabetes mellitus. World J Gastroenterol. 2016;22:10131–10139. doi: 10.3748/wjg.v22.i46.10131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim ER, et al. The clue of Interstitial Cell of Cajalopathy (ICCpathy) in human diabetic gastropathy: the ultrastructural and electrical clues of ICCpathy in human diabetic gastropathy. Exp Toxicol Pathol. 2012;64:521–526. doi: 10.1016/j.etp.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 10.Mazzone A, et al. Altered expression of Ano1 variants in human diabetic gastroparesis. J Biol Chem. 2011;286:13393–13403. doi: 10.1074/jbc.M110.196089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Grady G, et al. Abnormal initiation and conduction of slow-wave activity in gastroparesis, defined by high-resolution electrical mapping. Gastroenterology. 2012;143:589–598 e583. doi: 10.1053/j.gastro.2012.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yamamoto T, et al. Disturbed gastrointestinal motility and decreased interstitial cells of Cajal in diabetic db/db mice. J Gastroenterol Hepatol. 2008;23:660–667. doi: 10.1111/j.1440-1746.2008.05326.x. [DOI] [PubMed] [Google Scholar]
- 13.Ordog T, Takayama I, Cheung WK, Ward SM, Sanders KM. Remodeling of networks of interstitial cells of Cajal in a murine model of diabetic gastroparesis. Diabetes. 2000;49:1731–1739. doi: 10.2337/diabetes.49.10.1731. [DOI] [PubMed] [Google Scholar]
- 14.Choi KM, et al. Heme oxygenase-1 protects interstitial cells of Cajal from oxidative stress and reverses diabetic gastroparesis. Gastroenterology. 2008;135(2055–2064):2064 e2051–2052. doi: 10.1053/j.gastro.2008.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grover, M. et al. Diabetic and idiopathic gastroparesis is associated with loss of CD206-positive macrophages in the gastric antrum. Neurogastroenterology and motility: the official journal of the European Gastrointestinal Motility Society29 (2017). [DOI] [PMC free article] [PubMed]
- 16.Takahashi T, Nakamura K, Itoh H, Sima AA, Owyang C. Impaired expression of nitric oxide synthase in the gastric myenteric plexus of spontaneously diabetic rats. Gastroenterology. 1997;113:1535–1544. doi: 10.1053/gast.1997.v113.pm9352855. [DOI] [PubMed] [Google Scholar]
- 17.Grover M, et al. Clinical-histological associations in gastroparesis: results from the Gastroparesis Clinical Research Consortium. Neurogastroenterology and motility: the official journal of the European Gastrointestinal Motility Society. 2012;24(531–539):e249. doi: 10.1111/j.1365-2982.2012.01894.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang XY, Huizinga JD, Diamond J, Liu LW. Loss of intramuscular and submuscular interstitial cells of Cajal and associated enteric nerves is related to decreased gastric emptying in streptozotocin-induced diabetes. Neurogastroenterology and motility: the official journal of the European Gastrointestinal Motility Society. 2009;21:1095–e1092. doi: 10.1111/j.1365-2982.2009.01336.x. [DOI] [PubMed] [Google Scholar]
- 19.Dishy V, et al. The effect of sildenafil on gastric emptying in patients with end-stage renal failure and symptoms of gastroparesis. Clin Pharmacol Ther. 2004;76:281–286. doi: 10.1016/j.clpt.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 20.Gangula PR, Maner WL, Micci MA, Garfield RE, Pasricha PJ. Diabetes induces sex-dependent changes in neuronal nitric oxide synthase dimerization and function in the rat gastric antrum. American journal of physiology. Gastrointestinal and liver physiology. 2007;292:G725–733. doi: 10.1152/ajpgi.00406.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.He CL, et al. Loss of interstitial cells of cajal and inhibitory innervation in insulin-dependent diabetes. Gastroenterology. 2001;121:427–434. doi: 10.1053/gast.2001.26264. [DOI] [PubMed] [Google Scholar]
- 22.Moraveji S, et al. Depleted interstitial cells of Cajal and fibrosis in the pylorus: Novel features of gastroparesis. Neurogastroenterology and motility: the official journal of the European Gastrointestinal Motility Society. 2016;28:1048–1054. doi: 10.1111/nmo.12806. [DOI] [PubMed] [Google Scholar]
- 23.Min YW, et al. Impairment of the proximal to distal tonic gradient in the human diabetic stomach. Neurogastroenterology and motility: the official journal of the European Gastrointestinal Motility Society. 2014;26:229–236. doi: 10.1111/nmo.12253. [DOI] [PubMed] [Google Scholar]
- 24.Kassander P. Asymptomatic gastric retention in diabetics (gastroparesis diabeticorum) Annals of internal medicine. 1958;48:797–812. doi: 10.7326/0003-4819-48-4-797. [DOI] [PubMed] [Google Scholar]
- 25.Ricci JA, et al. Upper gastrointestinal symptoms in a U.S. national sample of adults with diabetes. Scandinavian journal of gastroenterology. 2000;35:152–159. doi: 10.1080/003655200750024317. [DOI] [PubMed] [Google Scholar]
- 26.Choung RS, et al. Risk of gastroparesis in subjects with type 1 and 2 diabetes in the general population. The American journal of gastroenterology. 2012;107:82–88. doi: 10.1038/ajg.2011.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jung HK, et al. The incidence, prevalence, and outcomes of patients with gastroparesis in Olmsted County, Minnesota, from 1996 to 2006. Gastroenterology. 2009;136:1225–1233. doi: 10.1053/j.gastro.2008.12.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Keshavarzian A, Iber FL, Vaeth J. Gastric emptying in patients with insulin-requiring diabetes mellitus. The American journal of gastroenterology. 1987;82:29–35. [PubMed] [Google Scholar]
- 29.Musara C, Vaillant C. Immunohistochemical studies of the enteric nervous system and interstitial cells of Cajal in the canine stomach. The Onderstepoort journal of veterinary research. 2013;80:518. doi: 10.4102/ojvr.v80i1.518. [DOI] [PubMed] [Google Scholar]
- 30.Wrzos HF, Cruz A, Polavarapu R, Shearer D, Ouyang A. Nitric oxide synthase (NOS) expression in the myenteric plexus of streptozotocin-diabetic rats. Digestive diseases and sciences. 1997;42:2106–2110. doi: 10.1023/A:1018830820537. [DOI] [PubMed] [Google Scholar]
- 31.Toda N, Herman AG. Gastrointestinal function regulation by nitrergic efferent nerves. Pharmacological reviews. 2005;57:315–338. doi: 10.1124/pr.57.3.4. [DOI] [PubMed] [Google Scholar]
- 32.Bult H, et al. Nitric oxide as an inhibitory non-adrenergic non-cholinergic neurotransmitter. Nature. 1990;345:346–347. doi: 10.1038/345346a0. [DOI] [PubMed] [Google Scholar]
- 33.Rand MJ. Nitrergic transmission: nitric oxide as a mediator of non-adrenergic, non-cholinergic neuro-effector transmission. Clinical and experimental pharmacology & physiology. 1992;19:147–169. doi: 10.1111/j.1440-1681.1992.tb00433.x. [DOI] [PubMed] [Google Scholar]
- 34.Baccari MC, Calamai F. Modulation of nitrergic relaxant responses by peptides in the mouse gastric fundus. Regulatory peptides. 2001;98:27–32. doi: 10.1016/S0167-0115(00)00225-1. [DOI] [PubMed] [Google Scholar]
- 35.Fahrenkrug J. Transmitter role of vasoactive intestinal peptide. Pharmacology & toxicology. 1993;72:354–363. doi: 10.1111/j.1600-0773.1993.tb01344.x. [DOI] [PubMed] [Google Scholar]
- 36.Shuttleworth CW, Keef KD. Roles of peptides in enteric neuromuscular transmission. Regulatory peptides. 1995;56:101–120. doi: 10.1016/0167-0115(95)00013-2. [DOI] [PubMed] [Google Scholar]
- 37.Curro D, De Marco T, Preziosi P. Involvement of peptide histidine isoleucine in non-adrenergic non-cholinergic relaxation of the rat gastric fundus induced by high-frequency neuronal firing. Naunyn-Schmiedeberg’s archives of pharmacology. 2002;366:578–586. doi: 10.1007/s00210-002-0633-z. [DOI] [PubMed] [Google Scholar]
- 38.Curro D, De Marco T, Preziosi P. Evidence for an apamin-sensitive, but not purinergic, component in the nonadrenergic noncholinergic relaxation of the rat gastric fundus. British journal of pharmacology. 2004;143:785–793. doi: 10.1038/sj.bjp.0705993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Burnstock G. The non-adrenergic non-cholinergic nervous system. Archives internationales de pharmacodynamie et de therapie. 1986;280:1–15. [PubMed] [Google Scholar]
- 40.Burnstock G, Satchell DG, Smythe A. A comparison of the excitatory and inhibitory effects of non-adrenergic, non-cholinergic nerve stimulation and exogenously applied ATP on a variety of smooth muscle preparations from different vertebrate species. British journal of pharmacology. 1972;46:234–242. doi: 10.1111/j.1476-5381.1972.tb06868.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Desai KM, Sessa WC, Vane JR. Involvement of nitric oxide in the reflex relaxation of the stomach to accommodate food or fluid. Nature. 1991;351:477–479. doi: 10.1038/351477a0. [DOI] [PubMed] [Google Scholar]
- 42.Desai KM, Warner TD, Bishop AE, Polak JM, Vane JR. Nitric oxide, and not vasoactive intestinal peptide, as the main neurotransmitter of vagally induced relaxation of the guinea pig stomach. British journal of pharmacology. 1994;113:1197–1202. doi: 10.1111/j.1476-5381.1994.tb17124.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lefebvre RA, Baert E, Barbier AJ. Influence of NG-nitro-L-arginine on non-adrenergic non-cholinergic relaxation in the guinea-pig gastric fundus. British journal of pharmacology. 1992;106:173–179. doi: 10.1111/j.1476-5381.1992.tb14311.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Boeckxstaens GE, et al. Evidence for a differential release of nitric oxide and vasoactive intestinal polypeptide by nonadrenergic noncholinergic nerves in the rat gastric fundus. Archives internationales de pharmacodynamie et de therapie. 1992;318:107–115. [PubMed] [Google Scholar]
- 45.D’Amato M, Curro D, Montuschi P. Evidence for dual components in the non-adrenergic non-cholinergic relaxation in the rat gastric fundus: role of endogenous nitric oxide and vasoactive intestinal polypeptide. Journal of the autonomic nervous system. 1992;37:175–186. doi: 10.1016/0165-1838(92)90039-J. [DOI] [PubMed] [Google Scholar]
- 46.Lefebvre RA, Smits GJ, Timmermans JP. Study of NO and VIP as non-adrenergic non-cholinergic neurotransmitters in the pig gastric fundus. British journal of pharmacology. 1995;116:2017–2026. doi: 10.1111/j.1476-5381.1995.tb16406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li CG, Rand MJ. Nitric oxide and vasoactive intestinal polypeptide mediate non-adrenergic, non-cholinergic inhibitory transmission to smooth muscle of the rat gastric fundus. European journal of pharmacology. 1990;191:303–309. doi: 10.1016/0014-2999(90)94162-Q. [DOI] [PubMed] [Google Scholar]
- 48.Tonini M, et al. Role of nitric oxide- and vasoactive intestinal polypeptide-containing neurones in human gastric fundus strip relaxations. British journal of pharmacology. 2000;129:12–20. doi: 10.1038/sj.bjp.0702977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Andrews CN, et al. Nitrergic contribution to gastric relaxation induced by glucagon-like peptide-1 (GLP-1) in healthy adults. American journal of physiology. Gastrointestinal and liver physiology. 2007;292:G1359–1365. doi: 10.1152/ajpgi.00403.2006. [DOI] [PubMed] [Google Scholar]
- 50.Tack J, Demedts I, Meulemans A, Schuurkes J, Janssens J. Role of nitric oxide in the gastric accommodation reflex and in meal induced satiety in humans. Gut. 2002;51:219–224. doi: 10.1136/gut.51.2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kuiken SD, Vergeer M, Heisterkamp SH, Tytgat GN, Boeckxstaens GE. Role of nitric oxide in gastric motor and sensory functions in healthy subjects. Gut. 2002;51:212–218. doi: 10.1136/gut.51.2.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Xue L, et al. Carbon monoxide and nitric oxide as coneurotransmitters in the enteric nervous system: evidence from genomic deletion of biosynthetic enzymes. Proc Natl Acad Sci USA. 2000;97:1851–1855. doi: 10.1073/pnas.97.4.1851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Farrugia G, et al. A major role for carbon monoxide as an endogenous hyperpolarizing factor in the gastrointestinal tract. Proc Natl Acad Sci USA. 2003;100:8567–8570. doi: 10.1073/pnas.1431233100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Samsom M, et al. Prevalence of delayed gastric emptying in diabetic patients and relationship to dyspeptic symptoms: a prospective study in unselected diabetic patients. Diabetes Care. 2003;26:3116–3122. doi: 10.2337/diacare.26.11.3116. [DOI] [PubMed] [Google Scholar]
- 55.Jones KL, et al. Predictors of delayed gastric emptying in diabetes. Diabetes Care. 2001;24:1264–1269. doi: 10.2337/diacare.24.7.1264. [DOI] [PubMed] [Google Scholar]