Abstract
The use of computed tomography (CT) has increased dramatically over the past several decades and has resulted in a concurrent increase in medical exposure to ionizing radiation. Several recent studies have examined the link between medical radiation and the risk of cancer, especially in children. The cancer risk associated medical exposure has not been definitively confirmed. However, we have to reduce unwarranted medical radiation exposure in pediatric patients. Justification and optimization are of great importance in order to minimize these risks, and the standardization of CT usage is essential. However, in Japan no clinical guidelines for the use of CT have been commonly agreed upon, especially in children. Furthermore, the CT-associated radiation exposure in Japan varies widely among the different facilities. Further studies based on a nationwide survey in Japan will be required in order to establish simple and useful clinical guidelines.
Keywords: CT, medical exposure, cancer risk, justification, optimization, children
INTRODUCTION
Computed tomography (CT) is a valuable and medically beneficial imaging technology; its use is increasing in all industrial countries, where it is replacing conventional X-ray studies. The number of CT scanners per million people in Japan was the highest among developed countries according to the data from the Organisation for Economic Cooperation and Development (OECD) [1]. However, the patient is exposed to considerably high doses of ionizing radiation when undergoing CT. For example, a chest CT scan typically delivers more than one hundred times the radiation dose of a chest X-ray [2, 3]. Furthermore, the radiation exposure from CT has also increased due to rapid scanning and multiphase examinations. Radiological imaging is associated with some risk of adverse effects. The risk of cancer induction through CT scans has recently received special attention. In particular, children are assumed to have a higher risk of developing cancer due to radiosensitivity, the relatively higher doses that are absorbed because of their smaller bodies, and because of their long lifespan after the radiation exposure. Some recent epidemiological studies have indicated that the risk of cancer was increased in children who underwent CT at relatively low doses [4–6]. Pearce et al. revealed increased leukemia and brain cancer risk in pediatric patients who had previously received CT. Mathews et al. found increased various cancer risks in pediatric patients who had been exposed to CT using a large database. However, considering the effect of confounding by indication, those results are subject to further analysis, and the effects of low-dose radiation are still unclear. At any rate, it is important to reduce the potential risk of cancer associated with CT exposure, and to draw attention to the justification of exposure and the optimization of radiation protection. Unlike other countries, such as Germany, the USA and the UK, Japan does not have clinical guidelines for the use of CT, especially in the pediatric field. We assessed the patterns of CT practice in Japan. Recognizing the patterns of CT studies is very important for standardizing the pediatric CT practice worldwide. We would like to emphasize methods by which unnecessary medical radiation exposure can be reduced in pediatric patients.
THE CANCER RISKS ASSOCIATED WITH CT EXPOSURE
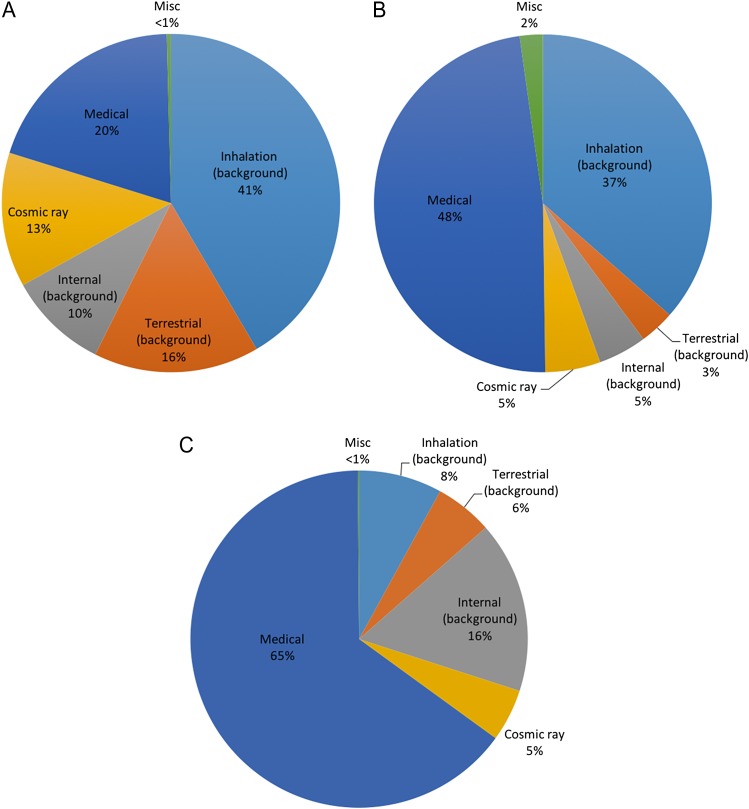
There are various sources of public radiation, including natural sources (e.g. internal inhalation, ingestion, external cosmic rays, and terrestrial sources), medical radiation, occupational radiation, nuclear power, and nuclear weapons. According to the United Nations Scientific Committee on the Effect of Atomic Radiation (UNSCEAR) 2008 report [7], ~20% of the public radiation burden is due to medical radiation. However, in comparison with the worldwide average, medical radiation accounts for a higher percentage of the public radiation burden in both the USA (~50%) [8] and Japan (>60%) [9] (Fig. 1). The use of medical radiation is associated with some risks.
Fig. 1.
A comparison of the sources of public radiation worldwide (UNSCEAR 2008) [7], in the USA (2009) [8] and Japan (2011) [9]. (A) UNSCEAR in 2008. (B) USA in 2009. (C) Japan in 2011. All of the sources that account for <1% of the total radiation burden (i.e. occupational radiation, nuclear power, and nuclear weapons) are labeled ‘Misc’. The frequency of medical radiation in the USA and Japan was higher than that in UNSCEAR.
Ionizing radiation is a well-established risk factor for cancer [10], and the risk in children is higher than that in adults due to the radiosensitivity of their growing and developing organs and tissues. Furthermore, their longer post-exposure life expectancy increases the lifetime risks of developing radiation-induced malignancies in comparison with adults [11, 12].
Recently, several studies have examined the link between medical radiation and the risk of cancer, especially in children.
In 2001, Brenner et al. estimated the risks of radiation-induced fatal cancer from pediatric CT examinations [4]. The estimated lifetime increase in the cancer mortality risk attributable to the radiation exposure from a CT scan in a 1-year-old are 0.18% and 0.07% for the abdomen and head, respectively. In other words, among the ~600 000 abdominal and head CT examinations performed each year for children in the USA, roughly 500 individuals might die from cancer attributable to CT radiation.
A more recent study performed by Pearce et al. [5] was the first to show an increased incidence of leukemia and brain cancer in children and adolescents who had received CT. In this retrospective cohort study of 178 604 patients who underwent a CT scan between 1985 and 2002 in various hospitals in the UK, the authors reported excess rates of leukemia and brain cancer. The average follow-up period was a little under 10 years. They estimated that one excess case of leukemia and one excess case of brain cancer would occur per 10 000 head CT scans. They showed significant associations between the estimated radiation doses provided by CT scans to the red bone marrow and brain and the subsequent incidence of leukemia and brain tumors.
Similar increases or projected risks in leukemia, brain, and other solid cancers were reported in the USA [13], Taiwan [14] and Australia [6].
Methews et al. estimated the increased cancer risk directly by comparing the cancer incidence in over 680 000 children and adolescents exposed to CT scans in a comparison cohort of over 10 million unexposed persons of similar age [6]. Cancer incidence in CT-exposed patients was increased by 24% in comparison with that in unexposed individuals after accounting for age, sex and year of birth [incidence rate ratio (IRR) 1.24]. The IRR was greater for persons exposed at younger ages. There was an excess of 608 cancers among the CT-exposed patients (brain, n = 147; other solid, n = 356; leukemia or myelodysplasia, n = 48; and other lymphoid, n = 57). The authors showed a dose–response relationship, with the IRR increasing by 0.16 for each additional CT scan.
Boice reviewed the literature on radiation epidemiology and recent pediatric CT studies and noted a critical problem: the reasons why the examinations were performed were not known, and these reasons were the probable cause of the subsequent cancer diagnosis [15]. This is ‘confounding by indication’ (or ‘reverse causation’), which is a major bias that frequently contaminates study populations [16]. Thus, these studies must be interpreted very carefully because analyzing the risk of medical radiation is very difficult. The cancer risk associated with CT exposure has not yet been definitively confirmed. To clarify this issue, a detailed analysis of the purpose of CT studies should be performed and the risks and benefits of radiological imaging should be determined, especially in children.
THE NUMBER OF CT SCANNERS AND PEDIATRIC CT EXAMINATIONS IN JAPAN AND OTHER COUNTRIES
Computed tomography (CT) is an essential diagnostic tool in modern medicine. The use of CT is dramatically increasing in all industrial countries, including Japan, because of technical advances [7].
Berrington de Gonzalez and Darby compared the cancer risk from medical exposure between several developed countries [17]. They concluded that Japan had the highest attributable risks, with 3.2% of the cumulative risk of cancer attributable to diagnostic X-rays. They used the average frequency for all health-care level 1 countries in the main calculations because no data were available for the annual frequency of CT examinations in Japan. Despite this, the higher rates of X-ray examination in Japan in comparison with those in other countries might have influenced the cancer risk.
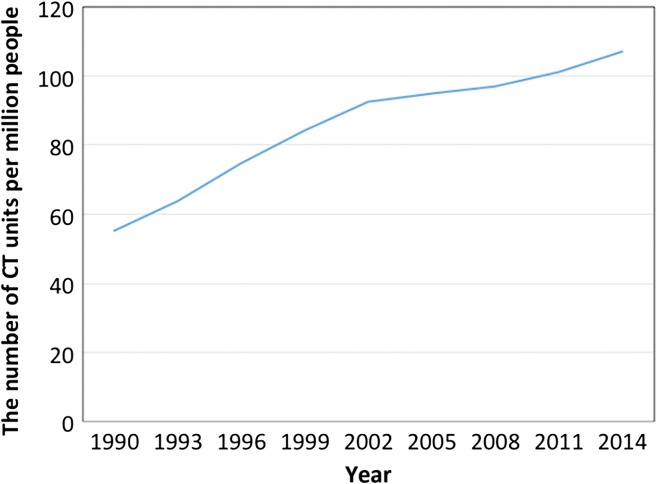
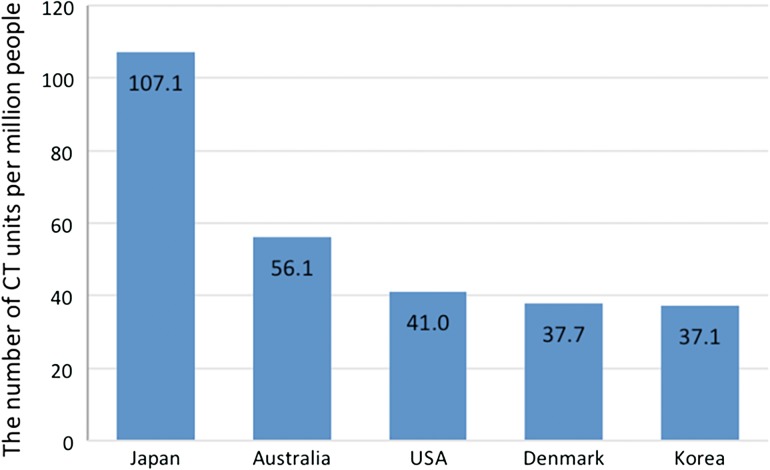
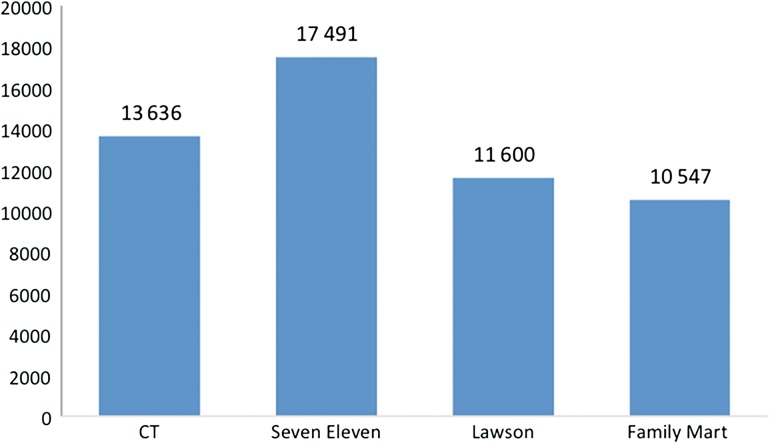
A report from the UNSCEAR in 2000 stated that there were 64 CT scanners per million people in Japan [18]. Nishizawa et al. conducted a nationwide survey in 2000 and concluded that there were 87.8 CT units per million people in Japan [19]. Based on the data from the Organisation for Economic Cooperation and Development (OECD), the number of CT units per million people is gradually increasing (Fig. 2) [1]. In 2014, the number of CT units per million people was 107.1, which was the highest among developed countries (Fig. 3). In the same year, a total of 13 636 medical facilities possessed CT scanners, which is equivalent to the number of convenience stores in Japan [20–22] (Fig. 4).
Fig. 2.
The number of CT units per million people in Japan from 1990 to 2014. The number has increased year by year.
Fig. 3.
The number of CT units per million people in different countries (data for 2014). There were 107.1 CT units per million people in Japan, which was the highest number among the developed countries.
Fig. 4.
A comparison of the number of CT scanners in Japan, and several convenience stores. The number of CT scanners was similar to the number of convenience stores in Japan.
On the contrary, the number of procedures for both total CT and pediatric CT is lower in Japan than in the USA [23]. In 2006, the number of total CT procedures per thousand people was 166 in Japan and 207 in the USA. Similarly, the number of pediatric CT procedures per thousand people was 32–34 in Japan and 76–94 in the USA. In 2005, there were 64–78 pediatric CT procedures per CT unit in Japan, and 460–590 in the USA; thus, the number of procedures per CT unit in the USA was approximately seven times higher than that in Japan. Furthermore, the number of CT examinations in pediatric patients has not increased in Japan, whereas an increase has been seen in the USA.
Nishizawa estimated—based on a nationwide survey of Japan that was performed in 2000—that 1.14 million CT examinations were performed annually for patients of 0–14 years of age [19]. Miyazaki estimated that 1.22 million pediatric CT examinations were performed for children of 0–15 years of age in 2003 [24]. Ono estimated that approximately 580 000 and 600 000 CT scans were performed for pediatric patients in 2005 and 2006, respectively [23].
A COMPARISON OF PEDIATRIC CT BETWEEN JAPAN AND GERMANY
Recognition of the patterns in CT studies is important, not only for resolving the abovementioned issue of ‘confounding by indication’, but also for standardizing pediatric CT practices worldwide. For this purpose, we are the first to assess the pediatric CT practice patterns in Japan (Nagasaki University Hospital and Fukushima Medical University Hospital) and to compare the patterns with the German data (Mainz University Medical Center) [25]. All pediatric patients between 0 and 14 years of age who underwent a CT examination during 2008 to 2010 were included in this study. We investigated the number of CT examinations, the time of the examination and the indication. The indications were classified into several categories, which included tumor-related examinations, trauma, congenital/other typical childhood diseases, and general examination regions (‘cranium’, ‘spine’, ‘thorax’ and ‘abdomen’).
The mean number of CT examinations per patient was 1.79 in Japanese hospitals, and 1.63 in the German hospital. The overall frequency of CT examinations in Japanese university hospitals did not differ significantly from that in the German hospital. However, differences were detected in the age distribution of the examined patients and the indications for CT. The proportion of patients of <5 years of age in Japan was significantly higher than that in Germany. The mean age in the Japanese hospitals (5.5 years) was significantly lower than that in the German hospital (7.7 years). Almost 20% of the pediatric CT examinations involved children younger than 12 months of age at the Japanese hospitals (both Nagasaki and Fukushima). In contrast, in the German hospital, fewer CT examinations were performed in patients younger than 12 months of age (2.2%).
At the Japanese hospitals, cranial indications were the most common indications for CT (42% of all CT scans), followed by tumor-related, trauma-related and abdominal indications. In comparison, trauma-related indications were the common indication for CT at the German hospital (34%), followed by cranial and tumor-related indications. The rates of cranial and abdominal CT scans at the Japanese hospitals were significantly higher in comparison with at the German hospital.
FUTURE PROSPECTS
Justification and optimization
Several studies have examined the link between medical radiation and the cancer risk. Although there is much uncertainty about the cancer risk from CT, it is reasonable to act on the assumption that there may be some risk [12, 26]. There are two principles for reducing the radiation dose from CT: justification and optimization. According to the principle of justification, the advantages of using ionizing radiation must outweigh the disadvantages. According to the principle of optimization, the radiation dose must be kept as low as is reasonably achievable/practicable (ALARA) [27].
The principle of justification is very important but also very difficult to evaluate, because it is difficult to measure quantitatively. Thus, studies on justification are very rare. However, the inappropriate use of medical radiation is a clear violation of the principle of justification, and should be reduced.
Prior consultation before CT examination is important for reducing the inappropriate or excessive use of imaging procedures. Pediatricians and radiologists should discuss whether CT is the best study to perform [28]. These discussions can provide an opportunity to share information, such as the number of imaging tests using ionizing radiation to which the patient has been exposed [12]. A conference on radiation protection for children could be a first step in educating referring physicians [29]. It would also be useful to produce risk communication materials and education materials for parents that aim to reduce the number of unnecessary CT examinations. A previous study revealed that one-third of all CT scans were not justified by medical need [30]. Slovis asked some pediatric radiologists about the percentage of head or body CT scans that they thought they could probably do without and found that the radiologists thought that up to 30% of studies were unnecessary or could be replaced with examinations that did not involve ionizing radiation [30]. If this is true, perhaps more than 1 million children per year could be being irradiated unnecessarily in the USA. This finding suggests that unnecessary irradiation may occur and that assessments of the justification in daily practice are far from perfect. We should investigate how useful the CT findings are in Japan.
The nuclear disaster at the Tokyo Electric Power Company Fukushima Daiichi Nuclear Power Plant on 11 March 2011 resulted in the release of a large amount of radioactive materials into the atmosphere. Yoshida et al. investigated the number and ratio of outpatients who underwent imaging examinations (e.g. CT, X-ray, MRI, US, etc.) at Fukushima Medical University hospital before and after the accident [31]. The number of outpatients of <10 years of age who underwent CT and X-ray examinations significantly decreased after the accident. On the other hand, a significant increase was observed in the ratio of outpatients of <10 years of age who underwent US. Since the accident, information on the relatively high radiation sensitivity of children has been widely distributed. Recently, Miyazaki also investigated the number of CT examinations at the main children’s hospital in Japan before and after the accident [32]. They found that the number was significantly reduced each year after the accident in comparison with the number in the year before the accident. These results suggest that public awareness of the radiation risk to children increased. Furthermore, from the viewpoint of justification, excess pediatric CT examinations might be avoided by doctors due to the recognition of the risks of radiation exposure. We hope that the increased awareness of radiation exposure has led to a turning point in Japanese pediatric radiology.
To ‘optimize’ medical radiation, it is very important to understand the quantitative data collected in relation to currently used devices as a starting point. In 2010, Tsushima et al. assessed the current situation of CT use in Japan [33]. They showed that there was very large variation in the levels of CT-associated radiation exposure among institutions. In particular, for lower abdominal CT, the radiation exposure ranged from 2.6 to 19 mSv. Many facilities use quality assessments, including consultation with a physician and assessments based on experience and the manufacturer’s recommendations [34].
Tsushima et al. emphasized the importance of the application of reference dose levels to further reduce such institutional differences. Also, the International Commission on Radiological Protection (ICRP) recommended the use of diagnostic reference levels (DRLs) in1996 [35]. However, DRLs were not set in Japan until 2015, when Takei et al. conducted a nationwide survey on radiation exposure during pediatric CT examinations and established the DRLs in Japan [36]. They found that the DLP (dose–length product) values for pediatric CT in Japan were higher in comparison with those of other countries [37–40]. We should organize a more extensive survey to collect dose data from a large cohort to establish empirical dose distributions for pediatric CT in Japan.
The automatic exposure-control option on the latest generation of scanners is also helping to reduce the CT-related radiation dose in individual patients [41]. The use of non-ionizing imaging techniques, such as ultrasonography (US) and magnetic resonance imaging (MRI), instead of CT is another approach that can be used to further reduce ionizing radiation exposure [41]. In cases of suspected appendicitis, the ACR (the American College of Radiology) recommends that ultrasonography or MRI should be performed instead of abdominal CT in pediatric patients. Another way to reduce the CT dose is to limit the number of phases. Multiple scans through the same body part can double or triple the radiation dose to the patient. A single pass is usually sufficient for diagnostic purposes in most cases in which CT scans are indicated for pediatric patients. The most effective way to reduce the population dose from CT is simply to decrease the number of CT studies. When a CT scan is justified by medical need, the associated risk is small relative to the diagnostic information that will be obtained [41].
In particular, we believe that justification is more important than optimization. To justify the usage of ionizing radiation, the benefits must outweigh the risks. However, little has been reported on the benefits of ionizing radiation. It is necessary to quantify the benefits and risks; however, this is very difficult to accomplish because the individuals that benefit from the use of ionizing radiation in medical practice and those that are put at risk by it are usually different.
What can we learn from the present state of radiation exposure from CT examinations in Japan and by comparing the use of CT among developed countries?
Yoshida et al. compared the use of pediatric CT between Japan (Nagasaki University Hospital and Fukushima Medical University Hospital) and Germany (Mainz University Medical Center). They found large differences in the frequencies of various indications for CT [25].
In Japan, the proportion of CT examinations involving pediatric patients was higher than that in Germany (5.1% vs 2.2%). The proportions of cranial and abdominal CT scans in Japan were significantly higher in comparison with those of Germany. These findings might indicate that CT is overused in Japan.
In Germany, specialized pediatric radiologists generally perform pediatric CT, whereas the CT examinations in Japan were conducted by general radiologists who did not specialize in pediatric radiology. Miyazaki et al. showed that, in Japan, the scanning parameters were determined by full-time radiologists in 40% of cases, and by CT technologists in 28% of cases [23]. This might partly explain the differences between Japan and Germany.
In Germany, the Radiation Protection Commission, together with clinical experts, has developed guidelines for diagnostic radiological procedures. Consequently, the low overall number of CT examinations at Mainz University Medical Center might reflect the effects of these guidelines. The American College of Radiology and the US Society for Pediatric Radiology have also produced recommendations and guidelines for pediatric CT use. Unlike other countries such as Germany, the USA and the UK, Japan does not have commonly agreed upon clinical guidelines for the use of ionizing radiation in diagnostic radiology. At the time of writing, there are no standardized clinical guidelines for pediatric CT in Japan. In 2016, the guidelines for medical imaging were published in Japan. In comparison with the 2013 guidelines, the 2016 guidelines included more content related to pediatric imaging.
From the viewpoint of ‘justification’, it is important to reduce inappropriate use and to standardize the usage of medical radiation. As shown in the comparison between the three Japanese University Hospitals, standardization has not been achieved in Japan. To resolve this situation, a nationwide survey on medical radiation usage should be conducted. Such a nationwide survey would also be important for ‘optimization’. A nationwide survey was only recently conducted to establish the Japanese DRLs; this is roughly 10 years behind other major developed countries and the details are still insufficient. A nationwide survey on how medical radiation is used, including the indications, consequences, and radiation dose, is necessary in order to establish standardized criteria for the appropriate use of medical radiation (for justification), and for establishing standardized imaging procedures and more detailed DRLs (for optimization).
ETHICS STATEMENT
Approvals for the study were obtained before the beginning of the study from the Ethics Committee of Nagasaki University Hospital (No. 10042553). The study was conducted in accordance with the guidelines set out in the Declaration of Helsinki. All the data used in this study were analyzed anonymously and securely protected under the supervision of the data protection officer of each hospital.
CONFLICT OF INTEREST
The authors have no conflicts of interest directly relevant to the content of this article.
FUNDING
This work was performed under institutional funds.
REFERENCES
- 1.Organisation for Economic Co-operation and Development (OECD). OECD.Stat http://stats.oecd.org/Index.aspx?DataSetCode=HEALTH_REAC (20 June 2017, date last accessed)
- 2. Linet MS, Kim KP, Rajaraman P. Children’s exposure to diagnostic medical radiation and cancer risk: epidemiologic and dosimetric considerations. Pediatr Radiol 2009;39:S4–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mettler FA Jr, Huda W, Yoshizumi TT et al. . Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology 2008;248:254–63. [DOI] [PubMed] [Google Scholar]
- 4. Brenner DJ, Bliston CD, Hall EJ et al. . Estimated risks of radiation-induced fatal cancer from pediatric CT. Am J Roentgenol 2001;176:289–96. [DOI] [PubMed] [Google Scholar]
- 5. Pearce MS, Salotti JA, Little MP et al. . Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 2012;380:499–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mathews JD, Forsythe AV, Brady Z et al. . Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ 2013;346:f2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) Sources and effects of ionizing radiation. UNSCEAR 2008 Report Volume 1, Annex A: Medical radiation exposures. New York, 2010.
- 8. Schauer DA, Linton OW. NCRP Report No. 160, ionizing radiation exposure of the population of the United States, medical exposure—are we doing less with more, and is there a role for health physicists? Health Phys 2009;97:1–5. [DOI] [PubMed] [Google Scholar]
- 9. NSRA Shinban Seikatsu Kankyu Houshasen (Kokumin senryou no santei), 2011 (in Japanese).
- 10. IARC Working Group Ionizing radiation, Part 1: X- and gamma (γ)-radiation, and neutrons In: IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, Vol. 75 Lyon: International Agency for Research on Cancer, 1999. [Google Scholar]
- 11. ICRP, Khong PL, Ringertz H, Donoghue V et al. . ICRP publication 121: radiological protection in paediatric diagnostic and interventional radiology. Ann ICRP 2013;42:1–63. [DOI] [PubMed] [Google Scholar]
- 12. Brody AS, Frush DP, Huda W et al. . Radiation risk to children from computed tomograpy. Pediatrics 2007;120:677–82. [DOI] [PubMed] [Google Scholar]
- 13. Miglioretti DL, Johnson E, Williams A et al. . The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr 2013;167:700–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Huang WY, Muo CH, Lin CY et al. . Paediatric head CT scan and subsequent risk of malignancy and benign brain tumour: a nation-wide population-based cohort study. Br J Cancer 2014;110:2354–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Boice JD., Jr Radiation epidemiology and recent paediatric computed tomography studies. Ann ICRP 2015;44:236–48. [DOI] [PubMed] [Google Scholar]
- 16. Kyriacou DN, Lewis RJ. Confounding by Indication in Clinical Research. JAMA 2016;316:1818–9. [DOI] [PubMed] [Google Scholar]
- 17. Berrington de González A, Darby S. Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet 2004;363:345–51. [DOI] [PubMed] [Google Scholar]
- 18. United Nations Scientific Committee on the Effect of Atomic Radiation (UNSCEAR) Sources and effects of ionizing radiation. UNSCEAR 2000 Report, 2000.
- 19. Nishizawa K, Matsumoto M, Iwai K et al. . Survey of CT practice in Japan and collective effective dose estimation. Nihon Igaku Hoshasen Gakkai Zasshi 2004;64:151–8. [PubMed] [Google Scholar]
- 20. Seven-eleven Japan Co. Ltd http://www.sej.co.jp/company/index.html (19 June 2017, date last accessed) (in Japanese).
- 21. Lawson http://www.lawson.co.jp/company/corporate/ (19 June 2017, date last accessed) (in Japanese).
- 22. FamilyMart http://www.family.co.jp/company.html (19 June 2017, date last accessed) (in Japanese).
- 23. Ono K, Yoshitake T, Hasegawa T et al. . Estimation of the number of CT procedures based on a nationwide survey in Japan. Health Phys 2011;100:491–6. [DOI] [PubMed] [Google Scholar]
- 24. Miyazaki O, Kitamura M, Masaki H et al. . Current practice of pediatric MDCT in Japan: survey results of demographics and age-based dose reduction. Nihon Igaku Hoshasen Gakkai Zasshi 2005;65:216–23. [PubMed] [Google Scholar]
- 25. Yoshida K, Krille L, Dreger S et al. . Pediatric computed tomography practice in Japanese university hospitals from 2008–2010: did it differ from German practice? J Radiat Res 2017;58:135–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rehani MM. I am confused about the cancer risks associated with CT: how can we summarize what is currently known? Am J Roentgenol 2015;205:W2–3. [DOI] [PubMed] [Google Scholar]
- 27. Kudo T, Ideguchi R. The effects of medical radiation: a few things nuclear cardiologists must know. Ann Nucl Cardiol 2015;1:35–42. [Google Scholar]
- 28. Linet MS, Kim KP, Rajaraman P. Children’s exposure to diagnostic medical radiation and cancer risk: epidemiologic and dosimetric considerations. Pediatr Radiol 2009;39:S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Strauss KJ, Goske MJ, Kaste SC et al. . Image gently: ten steps you can take to optimize image quality and lower CT dose for pediatric patients. Am J Roentgenol 2010;194:868–73. [DOI] [PubMed] [Google Scholar]
- 30. Slovis TL, Berdon WE. Panel discussion. Pediatr Radiol 2002;32:242–4. [Google Scholar]
- 31. Yoshida K, Hayashida N, Fukushima Y et al. . Changes in radiological imaging frequencies in children before and after the accident at the Fukushima Daiichi Nuclear Power Plant in Fukushima Prefecture, Japan. Jpn J Radiol 2015;33:619–26. [DOI] [PubMed] [Google Scholar]
- 32. Miyazaki O. Has pediatric CT practice in Japan changed since the Fukushima nuclear disaster? Pediatr Radiol 2015;45:1571–4. [DOI] [PubMed] [Google Scholar]
- 33. Tsushima Y, Taketomi-Takahashi A, Takei H et al. . Radiation exposure from CT examinations in Japan. BMC Med Imaging 2010;10:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Takei Y, Suzuki S, Miyazaki O et al. . Summary of a survey on radiation exposure during pediatric computed tomography examination in japan, focusing on the computed tomography examination environment. Nippon Hoshasen Gijutsu Gakkai Zasshi 2014;70:562–8. [DOI] [PubMed] [Google Scholar]
- 35. International Commission on Radiological Protection. Radiological protection and safety in medicine. ICRP Publication 73. Ann ICRP1996;26 (2). [PubMed]
- 36. Takei Y, Miyazaki O, Matsubara K et al. . Nationwide survey of radiation exposure during pediatric computed tomography examinations and proposal of age-based diagnostic reference levels for Japan. Pediatr Radiol 2016;46:280–5. [DOI] [PubMed] [Google Scholar]
- 37. Verdun FR, Gutierrez D, Vader JP et al. . CT radiation dose in children: a survey to establish age-based diagnostic reference levels in Switzerland. Eur Radiol 2008;18:1980–6. [DOI] [PubMed] [Google Scholar]
- 38. Kritsaneepaiboon S, Trinavarat P, Visrutaratna P. Survey of pediatric MDCT radiation dose from university hospitals in Thailand: a preliminary for national dose survey. Acta Radiol 2012;53:820–6. [DOI] [PubMed] [Google Scholar]
- 39. Vassileva J, Rehani MM, Applegate K et al. . IAEA survey of paediatric computed tomography practice in 40 countries in Asia, Europe, Latin America and Africa: procedures and protocols. Eur Radiol 2013;23:623–31. [DOI] [PubMed] [Google Scholar]
- 40. Brisse HJ, Aubert B. CT exposure from pediatric MDCT: results from the 2007–2008 SFIPP/ISRN survey. J Radiol 2009;90:207–15. [DOI] [PubMed] [Google Scholar]
- 41. Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med 2007;357:2277–84. [DOI] [PubMed] [Google Scholar]