Abstract
Work-related mental health impairment is recognized as a real problem in the context of helping responders, including health professionals, due to adverse health outcomes after a severe disaster. The Great East-Japan Earthquake, which occurred on 11 March 2011, was an unprecedented complex disaster that caused a nuclear accident at the Fukushima Daiichi Nuclear Power Plant (NPP). In addition to disaster stress and daily work, medical and health-care professionals, particularly nurses, provided counseling services to residents concerned about radiation health risks or mental health issues. This review focuses on the psychological aspects of the complex nuclear disaster, which was a combined artificial nuclear accident and natural disaster, and we investigated the psychological effects on hospital nurses associated with their experiences during the disaster. We looked at several investigations into the mental health of nurses after a nuclear disaster and in other situations. It was shown that mental health of nurses is impacted, not only after nuclear disasters but also in other circumstances. Furthermore, we noted the effects of extended periods of a heavy workload and daily life. Regarding anxiety about radiation exposure, nurses who had more knowledge of radiation tended to have better mental health, suggesting that education about the health risks of radiation exposure is important for health-care professionals. In summary, it is essential that nurses are provided with education about radiation exposure and its associated health risks, and also that there is a comprehensive approach to mental health care for nurses during the chronic phase of a disaster.
Keywords: resilience, radiation anxiety, Fukushima disaster, post-traumatic stress disorder, GHQ-12
INTRODUCTION
Exposure to disasters is common worldwide, and individuals severely exposed to disasters, particularly artificial disasters, may develop post-traumatic stress disorder (PTSD) or other mental disorders [1, 2]. Certain occupational factors and certain disaster characteristics are strongly associated with psychological distress among disaster responders [3–5]. The Great East-Japan Earthquake, accompanied by a huge Tsunami on 11 March 2011, was an unprecedented complex disaster that caused more than 18 000 deaths and missing people and was followed by the nuclear accident at the Fukushima Daiichi NPP [6]. The nuclear accident had a large negative impact, and rebuilding of the community of Fukushima has been notably slow over the past 6 years. Although it has been reported that the level of additional external and internal radiation exposure from this nuclear accident was much lower than the minimum dose level that causes direct negative health effects [7],the residents’ anxiety regarding radiation exposure and health risks is yet to be resolved [5]. A survey of public perception of radiation in Fukushima city conducted in May 2014 revealed that 70–80% of residents had experienced anxiety regarding the health risks of radiation exposure to themselves or their families following the nuclear accident [8]. It has been documented that the Three Mile Island NPP accident in the USA in 1979 and the Chernobyl nuclear accident in the former Soviet Union in 1986 significantly influenced the residents mentally [9]. The decommissioning work at the Fukushima Daiichi NPP is expected to continue for a long time, and, as for the Three Mile Island and the Chernobyl accidents, health-care workers, especially public health nurses and hospital nurses, are often asked by the residents about the health risks of the radiation exposure after the disaster [10]. At the same time, the health-care workers are also residents who have their own concerns regarding radiation exposure and the health risks to themselves and their families, which tends to be a mental burden for them. Although the role of nurses in providing mental health care for disaster victims has been extensively studied, the mental health of the nurses themselves in a disaster area has not been sufficiently considered [11–13]. As shown in Table 1, there are a few studies focusing on the mental health of nurses in disaster zones [3, 13–15]. In this review, we looked at the factors affecting mental health and the narrative stories describing resilience in nurses working in the face of disaster, also reviewing the mental health–related findings for residents who experienced the Fukushima disaster or similar disasters, such as atomic bomb.
Table 1.
Mental health risk of nurses during disasters evaluated by using GHQ-12 score
| Authors (year of pub) | Subjects | Number | GHQ-12 (av.) | GHQ-12 (SD) | Low-risk group (%) | High-risk group (%) |
|---|---|---|---|---|---|---|
| Suzuki et al. [14] (2004) | Nurses in 8 tertiary-care hospitals | 4279 | 5.42 | 3.29 | 31.2 | 68.8 |
| Nickell et al. [15] (2004) | Nurses in a tertiary-care hospital of SARS | 87 | a | a | 54.9 | 45.1 |
| Mattei et al. [3] (2017) | Nurses in an earthquake-stricken area | 173 | b | b | 47.5c | 52.5c |
| Nukui et al. [13] (2017) | Nurses in Fukushima | 730 | 3.96 | 3.27 | 54.4 | 45.6 |
The cut-off values of GHQ-12 for the low- and high- risk groups were <3 and >4, respectively. aNo description in the article. bDifferent scoring method. cPercentage of included nurses (n = 173), doctors (n = 77) and health-care assistants (n = 34). GHQ-12 scores did not differ significantly between nurses and doctors, or between nurses and health-care assistants.
NARRATIVE STORIES FROM NURSES DURING THE ACUTE PHASE OF THE COMPLEX DISASTER
The psychosocial issues among health-care workers during the acute phase of the Great East-Japan Earthquake and subsequent nuclear accident in the Fukushima prefecture have been described in several reports [16–20]. Naturally, these experiences were individual, and the factors affecting mental health were diverse, such as death of a close relative, losing a house in an earthquake or a tsunami, and/or being forced to evacuate. Meanwhile, some of the mental health factors were particular to nurses. In considering the mental health and resilience of nurses in the medium and long term, understanding of the experiences they underwent in the acute phase is important. Thus, we introduce the features and common aspects of the reported experiences below.
Case of a hospital in evacuation area
Although a hospital located close to the Fukushima Daiichi NPP was saved from destruction of the building by the earthquake or the tsunami, the patients and hospital staff shivered in the cold and shuddered with fear of aftershocks [16, 17]. Because patients with severe disease could not be moved, but had to remain in the hospital, hospital staff had to prepare for recurrence of tsunamis while treating emergency patients [16]. On the day after the disaster, evacuation instructions were given to residents within a 10-km radius of the nuclear power plant. There was no specific information as to why an evacuation was necessary, or where or how to evacuate; however, instructions to initiate evacuation had been given. Several people directly heard the sound of the explosion of the nuclear power plant [17]. When they became aware of the nuclear accident at the Fukushima Daiichi NPP, they felt even more anxious. The patients and hospital staff were forced to evacuate by separating into separate groups using relief buses and helicopters. Furthermore, they did not know where they would be evacuated to, and it took more than one week to confirm the safety of patients and hospital staff and also that of their families.
Case of a hospital 40–60 km from the Fukushima Daiichi NPP
Another hospital more than 40 km away from the nuclear power plant struggled to maintain its normal function due to patients experiencing strong anxiety or requiring medication with low or no supplies [16, 18]. Voluntary evacuation of the residents began 3 days after the explosion at the Fukushima Daiichi NPP and peaked after one week. Some nurses tried to go back to work, but their families strongly opposed them. A hospital more than 60 km away from the nuclear power plant was partially destroyed and tried to discharge the patients due to the frequent aftershocks [18]. The hospital accepted patients from the evacuation area. Nurses continued to work in three shifts around the clock, although they were having difficulty commuting because of a gasoline shortage. Another nurse in the non-evacuated area evacuated her children to another prefecture where relatives lived; however, she stayed back [18]. While she experienced a strong sense of guilt as a parent, she was firm in her decision based on her professional mission statement. Conversely, some nurses decided to temporarily evacuate the area with their families just after the nuclear accident occurred; they often found it difficult to return to work owing to feelings of guilt. Many suffered from the dilemma in deciding between their responsibilities as nurses and in securing their families’ relief. They felt a feeling of guilt, regardless of the choice they made.
Case of a core disaster hospital
At another core disaster hospital, they prepared setting beds at the entrance of the hospital to accept the emergency patients being transported [19, 20]. However, soon after the earthquake, the water supply was cut off, causing problems with dialysis, examinations, sterilization, and cooking by the hospital food service. Furthermore, information on the potential crisis at the nuclear power plant caused great unrest in the staff. Staff anxiety was further exacerbated because water and electric current supplies were cut off at home as well as at the hospital, and securing food and gasoline was difficult. They helped each other, bringing rice and other food from home wherever possible, and commuting by car-pooling. When the earthquake occurred, Disaster Medical Assistance Teams (DMATs) arrived at the affected hospitals from all over Japan. However, the DMATs withdrew 4 days after the earthquake from Fukushima prefecture owing to the possibility that the NPP accident has deteriorated. The DMAT withdrawals increased anxiety and fostered unease among the local staff [20]. The fact that a few medical teams continued their support as networks of radiation emergency medicine became a very valuable communication link in a time of crisis.
NUCLEAR DISASTER AND ANXIETY CONCERNING RADIATION EXPOSURE
Although the radiation exposure level in Fukushima was reported as much lower than that in the Hiroshima/Nagasaki Atomic Bombing and in Chernobyl [7], the psychosocial impacts have highlighted the similarities between these situations, including the health issues related to radiation health risk perception [6]. A significant association was observed between concerns regarding late effects of the atomic bomb radiation and mental health conditions in Nagasaki atomic bomb survivors [21]. While radiation cannot be felt through the five physical senses, atomic bomb survivors reported that they felt a flash of radiation [22]. They reported being often scared of the sounds of thunder and airplane flight and sometimes closed their eyes and turned the lights on and off because of their memory of flashing lights—all symptoms of suspected PTSD. If people had directly heard the explosive sounds of the nuclear power plant, it could be expected that they would be vulnerable to PTSD onset. Although relatively few people reported similar experiences after the 2011 nuclear accident, PTSD-like symptoms did seed to be more frequent even those without such experiences, indicating high-risk trauma had been experienced by >30% of residents, based on the results of the Fukushima Health Management Survey [23]. Furthermore, subjects with a high traumatic symptom score reportedly have a tendency toward poor mental health [24].
Nurses are prone to mental health problems, not only during disasters but also in daily work [25–27], suggesting that the problems can also be associated with job-related stress and burnout. Following the 2011 earthquake and nuclear disaster, staff shortage at hospitals (53% shortage of total staff and 52% shortage of nurses) reached a maximum within one month in disaster-affected areas [28]. In a survey targeting nurses working at a university hospital conducted 2 years after the disaster, several nurses had considered leaving their jobs because of ‘anxiety about life after the accident,’ ‘possible radiation health effects in children,’ and ‘anxiety about relationships with colleagues in the hospital’ [14]. In addition, in our survey [13], several nurses were also concerned about radiological contamination of foods, health effects on their children rather than on themselves, and evacuation requirements. Although they have some knowledge regarding radiation, some were anxious about the health risks of radiation exposure, whereas others were not, indicating that anxiety about radiation exposure varies widelyfrom person to person.
FEELINGS OF ISOLATION, DISCRIMINATION, AND HARMFUL RUMORS (FUHYOHIGAI)
A medical professional in this complex disaster reported having felt isolation and abandonment [19]. Feelings of isolation were also described during an infectious disease outbreak [29]. There are some common factors in relation to feelings of isolation found in medical staff involved in a radiation disaster and those involved in an outbreak, for example, seclusion with patients, protection clothing, and a risk perception of radioactive contamination or infection. Meanwhile, in the description of the Great Hanshin-Awaji Earthquake in 1995, feelings of isolation were greatly alleviated by the aid of supporters, relief supplies, and timely donations. Many disaster victims did not doubt that relief would be provided in due course, enabling them to remain relatively calm and relieved [30, 31]. In designated evacuation areas for disasters, especially nuclear disasters, business continuity around the area experiences physical damage as well as lack of human resources [6, 32]. In addition, the safety of dispatched staff needs to be ensured during disaster medical assistance; however, it is very important to support victims so that they do not feel abandoned during the emergency.
There have been cases of discrimination against people from Fukushima [33]. Similar discrimination has been reported in connection with other nuclear disasters and radiation accidents. Victims of a radiation accident in Goiania, Brazil, had to be issued certificates declaring them to be free of contamination because passengers refused to fly with contaminated persons aboard airplanes [34]. Such discrimination would strengthen the sense of isolation and desperation.
It has been reported that some atomic bomb survivors could not talk about their experience [22]. Many people who experienced the Fukushima complex disaster, similarly, did not talk about their experiences. Comments in responses to our questionnaire survey indicated that some hospital nurses could not talk about their anxiety, even to their families [13]. Nuclear disasters tend to cause disruption in families, workplaces, and local communities [35]. However, talking to each other about their shared experiences may contribute to alleviating mental distress [36]. In fact, many nurses wrote that they were able to overcome their mental distress with support from their superiors, colleagues, families and/or lovers.
An additional concern regarding damage to reputation, called ‘Fuhyohigai,’ was reported after the Fukushima disaster [35]. ‘Fuhyohigai’ refers to social and economic damage caused by an unfounded negative rumour spread by the media, causing decreased sales of local products, trade, and tourism. However, ‘Fuhyohigai’is not only an economic issue, but also applies to psychosocial problems and self-stigmatization [37]. For example, concerns about discrimination because of supposed dangerous levels of radiation exposure can lead a change in risk perception, stigmatization by others, and self-stigmatization. After the Fukushima complex disaster, some nurses wrote that they did not want to reveal their hometown and were concerned about the impact of the disaster on their daughter’s marriage [13]. Similar concerns were reported by atomic bomb survivors [35]. Fuhyohigai can easily occur, even if the risk is negligible after a nuclear accident, and can cause continued stigmatization.
COMPARISON IN SURVEYS ABOUT DISASTER-RELATED MENTAL HEALTH OF NURSES
Radiation disasters have a large impact on mental health. In a survey of atomic bomb survivors of Hiroshima or of Nagasaki who have been living in South Korea, conducted more than 60 years later, 30.3% of them were categorized as the high-risk group with respect to trauma response, and 48.1% of them were included in the higher risk group of the survey using the General Health Questionnaire-12 (GHQ-12) [38]. The effect on mental health was regarded as the most serious health effect after the Chernobyl nuclear accident, and residents who recognized radiation health risks made lifestyle changes, such as over-drinking, that affected not only their mental health but also their physical disorders [39].
A mental health and lifestyle survey for residents in the evacuation areas was conducted by the Fukushima Health Management Survey [23]. In this survey, the K6 score was used as an index of general mental health. The proportion of people at high risk of requiring support for depressed mood and anxiety was 14.6% in 2011, 11.7% in 2012 and 9.7% in 2014 [40], compared with ~7% in the evacuation areas in Miyagi and Iwate. Hence, mental health care in the evacuation area surrounding the nuclear accident is presumably needed [41]. Using the PTSD checklist (PCL) score as an index of the trauma response, 21.6% of participants required support in 2011, 17.4% in 2012, and 15.8% in 2014 [37], compared with 12.4% in a one-year survey of firefighters who responded to terrorist attacks in the USA [42]. Ben-Ezra et al. compared the reactions of hospital nurses (n = 34) and civilians (n = 39) after this disaster, using a brief questionnaire [43]. This preliminary study suggested that nurses had a lower level of PTSD symptoms, but higher self-rated health, life satisfaction, and perceived coping, and a similar level of fear about radiation to that of civilians. Sakuma et al. also reported that the prevalence of high general psychological distress (K6 score) was higher among medical workers [mostly hospital nurses (14.5%)] and municipality officers (14.9%) than among firefighters (2.6%) at about one year after the Great East-Japan Earthquake in the coast area of Miyagi prefecture affected by the tsunami [5].
We investigated the mental health of hospital nurses (n = 730) in the Fukushima prefecture 4 years after the radiation disaster [13]. Their mental health status was estimated using GHQ-12, and 45.6% of respondents scored above the GHQ-12 threshold point, indicating high emotional distress after the disaster. The mean GHQ-12 value was 3.96 (SD 3.27), the mode was 2, and the median was 3. This result was higher than the mean GHQ-12 value of 1.91 in a survey by a general corporation not affected by disaster [15]. However, the mean score and the proportion of the high-risk group were 5.42 and 68.8%, respectively, in nurses from eight Japanese tertiary care hospitals [27]. These results suggested that nursing is a stressful occupation, even in peacetime, compared with other occupations. Compared with other disasters, the mean GHQ-12 score was 3.6 in evacuees of the Niigata–Chuetsu Earthquake [44], and 45.1% of nurses who provided SARS medical care were in the high-risk group [45]. These data are summarized in Table 1. Nurses who have been exposed to extremely high stress after the Fukushima Daiichi NPP accident have the same level of mental health risk compared with that found previous studies, and it seems that the nurses acquired some resilience over the 4-year period after the disaster.
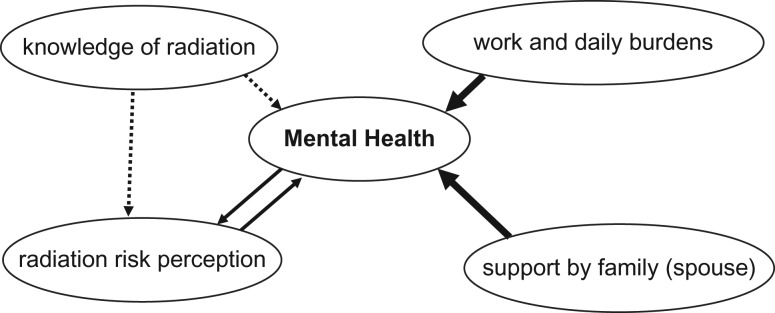
Subsequently, we analyzed the factors contributing to resilience—‘with spouse’ and ‘no increase of daily life burdens’ was significantly correlated with being in the low-risk group [13]. With regard to radiation risk perception, knowledge of radiation, and coping with anxiety, ‘Dread risk’ (feeling of fears), ‘Concern about effects on health,’ ‘Present work burdens,’ and ‘Present daily burdens’ were significantly positively correlated with the high-risk group, and ‘Known risk’ and ‘Controllability’ were significantly negatively correlated with the high-risk group. Among these, association with mental health issues was higher for work and daily burdens than was anxiety about radiation [13].
The correlation between radiation risk perception and mental health issues was also demonstrated in the residents by the Fukushima Health Management Survey [46, 47]. In addition, the greater the knowledge of radiation, the better the mental health observed. It is possible that increased knowledge regarding radiation will reduce anxiety of radiation, suggesting the importance of radiation health risk education for health-care professionals especially from the acute to subacute period of disasters [14, 37, 48]. During the chronic phase of a disaster, work and daily burdens were more influential on mental health than anxiety about radiation; hence, mental health care for nurses should be considered, independent of concerns of radiation (Fig. 1). It is particularly important to address the mental health care of nurses through comprehensive approaches during the chronic phase of a disaster.
Fig. 1.
Supposed association of factors affecting long-term mental health of nurses after the nuclear disaster. Bold arrow = strong effects, bi-directional arrow = correlation, dotted arrow = week influence.
CONCLUSIONS
In this narrative review, we mainly focused on the psychological effects on hospital nurses due to their experiences during the Fukushima complex disaster. We also looked at other investigations into the mental health of nurses. We concluded that it is essential that nurses are provided with education about radiation exposure and its associated health risks, and also that there is a comprehensive approach to mental health care for nurses during the chronic phase of a disaster.
ACKNOWLEDGEMENTS
We would like to thank Ms Suenaga, Dr Rokkaku, Prof. Yabe, the nursing staff and their managers for participating in our previous study [13].
FUNDING
This work was partially supported by the Program of the Network-type Joint Usage/Research Center for Radiation Disaster Medical Science Grant number KI28203 Fukushima Medical University.
REFERENCES
- 1. Farooqui M, Quadri SA, Suriya SS et al. . Posttraumatic stress disorder: a serious post-earthquake complication. Trends Psychiatry Psychother 2017;39:135–43. [DOI] [PubMed] [Google Scholar]
- 2. Neria Y, DiGrande L, Adams BG. Posttraumatic stress disorder following the September 11, 2001, terrorist attacks: a review of the literature among highly exposed populations. Am Psychol 2011;66:429–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mattei A, Fiasca F, Mazzei M et al. . Stress and burnout in health-care workers after the 2009 l’aquila earthquake: a cross-sectional observational study. Front Psychiatry 2017;8:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McVicar A. Workplace stress in nursing: a literature review. J Adv Nurs 2003;44:633–42. [DOI] [PubMed] [Google Scholar]
- 5. Sakuma A, Takahashi Y, Ueda I et al. . Post-traumatic stress disorder and depression prevalence and associated risk factors among local disaster relief and reconstruction workers fourteen months after the Great East Japan Earthquake: a cross-sectional study. BMC Psychiatry 2015;15:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hasegawa A, Tanigawa K, Ohtsuru A et al. . Health effects of radiation and other health problems in the aftermath of nuclear accidents, with an emphasis on Fukushima. Lancet 2015;386:479–88. [DOI] [PubMed] [Google Scholar]
- 7. United Nations Scientific Committee on the Effects of Atomic Radiation Sources and effects of ionizing radiation. Report to the General Assembly. Scientific annexes A: Levels and effects of radiation exposure due to the nuclear accident after the 2011 Great East Japan earthquake and tsunami. UNSCEAR 2013 Report Volume I New York: United Nations, 2013.
- 8. Results of ‘2nd Survey on Citizen Consciousness of Radiation’ Fukushima City Policy Promotion Department, implemented in May 2014 http://www.city.fukushima.fukushima.jp/skyodokocho/shise/kocho/anketo/kouchou12090501.html. (21 August 2017, date last accessed) (in Japanese).
- 9. Evelyn JB, Parkinson DK, Leslie OD. Long-term mental health consequences of the accident at Three Mile Island. Int J Ment Health 1990;19:48–50. [Google Scholar]
- 10. Goto A, Rudd RE, Lai AY et al. . Leveraging public health nurses for disaster risk communication in Fukushima City: a qualitative analysis of nurses’ written records of parenting counseling and peer discussions. BMC Health Serv Res 2014;14:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stangeland PA. Disaster nursing: a retrospective review. Crit Care Nurs Clin North Am 2010;22:421–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Turner SB. Resilience of nurses in the face of disaster. Disaster Med Public Health Prep 2015;9:601–4. [DOI] [PubMed] [Google Scholar]
- 13. Nukui H, Murakami M, Midorikawa S et al. . Mental health and related factors of hospital nurses: an investigation conducted 4 years after the Fukushima disaster. Asia Pac J Public Health 2017;29:161S–70S. [DOI] [PubMed] [Google Scholar]
- 14. Nakai H. Saigaigahontouniosottatoki—Hanshin Awaji Daishinsai 50 nichikannokiroku (When a disaster hit really—Hanshin Awaji Earthquake 50 days record). Tokyo: Misuzu Publishing, 2011. (in Japanese). [Google Scholar]
- 15. Urakawa K, Yokoyama K. Sense of coherence (SOC) may reduce the effects of occupational stress on mental health status among Japanese factory workers. Ind Health 2009;47:503–8. [DOI] [PubMed] [Google Scholar]
- 16. Yamasaki T. The Great East-Japan Earthquake Nursing Judgement and Action. Aichi: Nissoken Publishing, 2011. (in Japanese). [Google Scholar]
- 17. Maeda M. Difficulties of the staff working at Hibarigaoka Psychiatric Hospital in Minami-Soma. Jpn J Clin Psychiatry 2012;41:1183–91 (in Japanese). [Google Scholar]
- 18. Japanese Nursing Association Publishing Association Nurse’s East-Japan Great Earthquake Report Tokyo: Japanese Nursing Association, 2011. (in Japanese).
- 19. Fukushima Medical University Hospital Radiation Disaster Medical Center At the Forefront of the Radiation Disaster: Message From the Medical Staff Living in Fukushima. Tokyo: Life Science Publishing, 2013. (in Japanese). [Google Scholar]
- 20. Fukushima Medical University FUKUSHIMA Lives on the line. A Compendium of Reports from the 2011 Great East Japan Earthquake and Tsunami. Fukushima: Fukushima Medical University Publishing Association, 2012. [Google Scholar]
- 21. Honda S, Shibata Y, Mine M et al. . Mental health conditions among atomic bomb survivors in Nagasaki. Psychiatry Clin Neurosci 2002;56:575–83. [DOI] [PubMed] [Google Scholar]
- 22. Kim Y, Tsutsumi A, Izutsu T et al. . Persistent distress after psychological exposure to the Nagasaki atomic bomb explosion. Br J Psychiatry 2011;199:411–6. [DOI] [PubMed] [Google Scholar]
- 23. Yabe H, Suzuki Y, Mashiko H et al. . Psychological distress after the Great East Japan Earthquake and Fukushima Daiichi Nuclear Power Plant accident: results of a mental health and lifestyle survey through the Fukushima Health Management Survey in FY2011 and FY2012. Fukushima J Med Sci 2014;60:57–67. [DOI] [PubMed] [Google Scholar]
- 24. Yoshida K, Shinkawa T, Urata H et al. . Psychological distress of residents in Kawauchi village, Fukushima Prefecture after the accident at Fukushima Daiichi Nuclear Power Station: the Fukushima Health Management Survey. PeerJ 2016;4:e2353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jenkins R, Elliott P. Stressors, burnout and social support: nurses in acute mental health settings. J Adv Nurs 2004;48:622–31. [DOI] [PubMed] [Google Scholar]
- 26. Riding RJ, Wheeler HH. Occupational stress and cognitive style in nurses. Br J Nurs 1995;4:160–8. [DOI] [PubMed] [Google Scholar]
- 27. Suzuki K, Ohida T, Kaneita Y et al. . Mental health status, shift work, and occupational accidents among hospital nurses in Japan. J Occup Health 2004;46:448–54. [DOI] [PubMed] [Google Scholar]
- 28. Ochi S, Tsubokura M, Kato S et al. . Hospital staff shortage after the 2011 triple disaster in Fukushima, Japan—an earthquake, tsunamis, and nuclear power plant accident: a case of the Soso District. PLoS One 2016;11:e0164952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nakai H. Fukkounomichinakabade–Hanshinawajidaishinsaiichinennokiroku (In the midst of reconstruction road—Hanshin Awaji great earthquake record of one year). Tokyo: Misuzu Publishing, 2011. (in Japanese). [Google Scholar]
- 30. Sato Y, Hayashida N, Orita M et al. . Factors associated with nurses’ intention to leave their jobs after the Fukushima Daiichi Nuclear Power Plant accident. PLoS One 2015;10:e0122389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sim M. Psychological trauma of Middle East Respiratory Syndrome victims and bereaved families. Epidemiol Health 2016;38:e2016054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Morioka N, Tomio J, Seto T et al. . Trends in the geographic distribution of nursing staff before and after the Great East Japan Earthquake: a longitudinal study. Hum Resour Health 2015;13:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Haworth A. After Fukushima: Families on the Edge of Meltdown 2013. https://www.theguardian.com/environment/2013/feb/24/divorce-after-fukushima-nuclear-disaster (31 August 2017, date last accessed).
- 34. Petterson JS. Perception vs. reality of radiological impact: the Goiania model. Nucl Newsmag 1988;8:84–90. [Google Scholar]
- 35. Bromet EJ, Havenaar JM. Psychological and perceived health effects of the Chernobyl disaster: a 20-year review. Health Phys 2007;93:516–21. [DOI] [PubMed] [Google Scholar]
- 36. Knowles A. Resilience among Japanese atomic bomb survivors. Int Nurs Rev 2011;58:54–60. [DOI] [PubMed] [Google Scholar]
- 37. Ohtsuru A, Tanigawa K, Kumagai A et al. . Nuclear disasters and health: lessons learned, challenges, and proposals. Lancet 2015;386:489–97. [DOI] [PubMed] [Google Scholar]
- 38. Koshimato R, Nakane H, Kim H et al. . Mental health conditions in Korean atomic bomb survivors: a survey in Seoul. Acta Med Nagasaki 2011;56:53–8. [Google Scholar]
- 39. Bromet EJ. Mental health consequences of the Chernobyl disaster. J Radiol Prot 2012;32:N71–5. [DOI] [PubMed] [Google Scholar]
- 40. Report of the Fukushima Health Management Survey (revised version, 25 April, 2016). http://fmu-global.jp/download/report-of-the-fukushima-health-management-survey-in-english_revised-2/?wpdmdl=1914 (27 August 2017, date last accessed).
- 41. Kunii Y, Suzuki Y, Shiga T et al. . Severe psychological distress of evacuees in evacuation zone caused by the Fukushima Daiichi Nuclear Power Plant accident: the Fukushima Health Management Survey. PLoS One 2016;11:e0158821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Perrin MA, DiGrande L, Wheeler K et al. . Differences in PTSD prevalence and associated risk factors among World Trade Center disaster rescue and recovery workers. Am J Psychiatry 2007;164:1385–94. [DOI] [PubMed] [Google Scholar]
- 43. Ben-Ezra M, Palgi Y, Hamama-Raz Y et al. . Reactions to the 2011 Tōhoku earthquake and tsunami: a preliminary matching study comparing nurses and civilians. J Nerv Ment Dis 2013;201:534–6. [DOI] [PubMed] [Google Scholar]
- 44. Toyabe S, Shioiri T, Kobayashi K et al. . Factor structure of the General Health Questionnaire (GHQ-12) in subjects who had suffered from the 2004 Niigata–Chuetsu Earthquake in Japan: a community-based study. BMC Public Health 2007;7:175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Nickell LA, Crighton EJ, Tracy CS et al. . Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. CMAJ 2004;170:793–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Oe M, Maeda M, Nagai M et al. . Predictors of severe psychological distress trajectory after nuclear disaster: evidence from the Fukushima Health Management Survey. BMJ Open 2016;6:e013400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Suzuki Y, Yabe H, Yasumura S et al. . Psychological distress and the perception of radiation risks in Fukushima evacuees. Bull World Health Organ 2015;93:598–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Yasui K, Kimura Y, Kamiya K et al. . Academic responses to Fukushima disaster. Asia Pac J Public Health 2017;29:99S–109S. [DOI] [PubMed] [Google Scholar]