Abstract
Background
The identification of coronary artery calcification (CAC) detected coincidentally on chest CT exams could assist in cardiovascular risk assessment but may not be reported consistently on clinical studies. Cardiovascular risk factor stratification is important to predict short term cardiac events during cancer therapy and long term cardiac event free survival in cancer patients. We sought to determine the prevalence of CAC and clinical reporting rates in a cohort of cancer patients at high risk of cancer therapy related cardiac events.
Methods
408 Breast cancer patients who were referred to a cardiac oncology clinic were screened. Inclusion criteria included having had a CT chest and the absence of known coronary disease. Among those screened 263 patients were included in the study.
Results
CAC was identified in 70 patients (26%). CAC was reported in 18% of studies. The reporting rates of CAC increased with the extent of coronary calcification (p < 0.01) and increased during the period of the study (p < 0.05).
Conclusions
CAC was commonly detected on chest CT studies in this observational study of breast cancer patients at high risk of cardiac oncology events. The presence of CAC was often not reported clinically but reporting rates have increased over time. Recent SCCT/STR guidelines recommend reporting the presence of CAC on routine chest CT scans in recognition of the importance of CAC as a predictor of cardiovascular events. Reporting of CAC on chest CTs may help to further risk stratify breast cancer patients and improve cardiovascular outcomes in this vulnerable population.
Keywords: Cardiac oncology, Coronary calcification and chest CT
1. Introduction
Coronary Arterial calcification (CAC) denotes the presence of atherosclerosis and is a powerful predictor of cardiovascular events [1,2]. CAC may be detected co-incidentally on non-gated thoracic computed tomography (CT) studies [[3], [4], [5], [6], [7]]. Chest CT scans are performed in breast cancer patients as part of cancer staging, radiotherapy planning or to investigate clinical conditions that arise during cancer therapy [8]. Until recently there has been no consensus as to how to report arterial calcification on such studies [9]. In light of this, and since the focus of chest CT requests is often to look for non-cardiovascular findings, the presence of CAC may be under reported [[9], [10], [11]].
In breast cancer patients detection of atherosclerosis is of particular importance. This reflects the fact that cardiovascular disease is the leading cause of death in early stage breast cancer [12]. It acknowledges that in the past, cardiovascular risks may have been less aggressively managed in cancer patients [13,14]. As a result pre-chemotherapy cardiovascular screening has recently been recommended in three independent cardiac oncology guidelines [[15], [16], [17]]. Cardiac oncology guidelines also recognize that there is an increased cardiotoxicity risk from chemotherapy experienced by breast cancer patients in the presence of co-existing cardiac disease or cardiovascular risks such as hypertension and diabetes [[15], [16], [17]]. Thus, in not reporting CAC, the possibility of detecting an important short-term determinant from cancer therapy or long-term predictor of atherosclerotic events is potentially over looked.
To examine how often non-gated chest CT reports identified CAC in breast cancer patients we sought to study a population in whom CAC reporting might impact short and long term cardiovascular outcomes. We therefore choose to study breast cancer patients from a cardiac oncology clinic. The prevalence of CAC would be expected to higher in this population in comparison to an unselected population of breast cancer sufferers since cardiac oncology patients were either at risk or had already experienced cardiac complications.
2. Methods
The study was approved by the local research ethics board.
2.1. Study sample
From 2009 to 2017, a total of 408 consecutive breast cancer patients, who were referred to the cardio-oncology clinic at the Ottawa General Hospital, were included in the study. Of the 408 patients, 269 patients had undergone prior non-ECG gated Chest CT, 263 fulfilled the inclusion criteria (a history of breast cancer, prior non-ECG gated CT chest and no documented coronary artery disease or peripheral vascular disease.)
2.2. Clinical demographics
Patient cardiovascular risk factors, cardiac history and cancer history were obtained from a comprehensive review of the electronic medical records. A history of coronary artery disease was present if patients self-reported these at the cardio- oncology clinic or if evident on the medical chart [14].
2.3. Image acquisition
CT scans were performed on commercially available multi-detector CTs with methods as previously described [10]. Briefly, images were non-ECG gated thoracic CT scans with or without contrast enhancement as clinically indicated [8,18]. Soft tissue kernel slice-thickness images ranged from 1.0–5.0 mm and were acquired using Aquillon 16-, 64-, 320-detector (Toshiba Canada Medical Systems Limited, Markham, Ontario); Lightspeed Plus 16- and Lightspeed 64-detector (General Electric Healthcare, Mississauga, Ontario,) and Definition Flash dual source 64 × 2-detector Siemens Medical Solutions Canada, Oakville, Ontario). CT exams were initially reported in the clinical setting by a radiologist. All CT studies were subsequently reviewed for the study purposes without additional processing using patient archiving and communication system (PACS) software (McKesson Radiology 12.3, McKesson Canada, Mississauga, Ontario).
2.4. Coronary artery calcification (CAC)
CAC was identified and quantified using visual ordinal scoring system as previously described [3,19]. Briefly calcium in the left main, left anterior descending artery, left circumflex and right coronary arteries was categorized as absent (0) or present. If present the degree of calcification (1–3, or) was classified as mild (1) if <1/3 of the length of the entire artery contained calcification (CAC = 1), moderate if 1/3–2/3 (CAC = 2) and severe if >2/3 of the artery showed calcification (CAC = 3). The final score was the sum of the individual artery scores from 0 to 12. Patients were divided into 4 subgroups based on their final scores: 0, 1–3, 4–5 and 6–12. These scores have been reported to correspond to Agatston scores of 0, 1–100, 101–400 and >400 as previously described [19].
2.5. Thoracic arterial calcification
Non coronary arterial calcification (NCC) in the aorta, brachio-cephalic, subclavian, or carotid arteries was classified as present or absent.
2.6. CT imaging reports
Reports from the CT chest studies were obtained from the patient's electronic medical records. The time and date of study in terms of standard working hours (7 am–7 pm) and on call hours (7 pm–7 am) were recorded. For the purposes of the study weekday and weekend work times were not treated differently. The interpreting radiologist was classified as cardiac or non-cardiac based on their individual training and clinical practice during working hours.
2.7. Statistical analysis
Associations between the clinical reporting of non-coronary arterial calcification or CAC and a) the extent of coronary calcification, b) time of CT study (working versus on call hours), c) year of CT study, d) reading radiologists (cardiac versus non cardiac) were assessed as categorical and ordinal variables as appropriate using Chi Squared tests. The year of CT study was divided into 4 groups for this analysis. The groups were divide into quartiles by total number of CT scans performed (2002–2009 (65 studies), 2009–2011 (66 scans), 2011–2013 (66 scans) and 2013–2016 (66 scans). Linearity between the frequency of CAC or NCC reporting and the extent of CAC or year of CT study were assessed using Pearson's Chi Square test. Data were analyzed using IBM SPSS 24 statistics for Windows (Armonk, NY: IBM Corp). Statistical significance was defined as p < 0.05.
3. Results
3.1. Demographics
A total of 263 of 408 breast cancer patients at the cardiac oncology clinic met the inclusion criteria (Table 1). The majority of our sample were female (98.5%) and the median age was 60 years old. The most common indication for chest CT was cancer staging (87.5%) followed by investigation for pulmonary pathology (including pneumonia, chronic obstructive lung disease) (5.3%) and chest pains (3.4%). Reasons for referral to the cardiac oncology clinic were reduced left ventricular ejection fraction (51.3%), arrhythmia (11.4%), dyspnea (5.7%), and chest pain (7.6%) (Table 1). 75.7% of patients had received anthracycline containing chemotherapy regimens and 64.6% of patients received trastuzumab.
Table 1.
Patient's characteristics.
| Patient's characteristics, n = 263 | ||
|---|---|---|
| Category | Frequency (%) | |
| Gender | Female | 259 (98.5) |
| Age (mean ± SD) | 59.5 ± 11.6 | |
| Cardiovascular risk factors | Hypertension | 95 (36.1) |
| Diabetes | 38 (14.4) | |
| Smoking | 105 (39.9) | |
| Obesity | 71 (27.0) | |
| Family history of coronary disease | 34 (12.9) | |
| Peripheral vascular disease | 11 (4.2) | |
| Dyslipidemia | 74 (28.1) | |
| Cardiac oncology referral | Low ejection fraction | 135 (51.3) |
| Palpitations/arrhythmia | 20 (7.6) | |
| Chest pain | 20 (7.6) | |
| Dyspnea | 15 (5.7) | |
| Atrial fibrillation | 10 (3.8) | |
| Other | 63 (24.0) | |
| Reason for chest CT | Cancer staging | 230 (87.5) |
| Pulmonary pathology | 14 (5.3) | |
| Chest pain | 9 (3.4) | |
| Pre-operative assessment | 10 (3.8) |
3.2. Coronary artery calcification
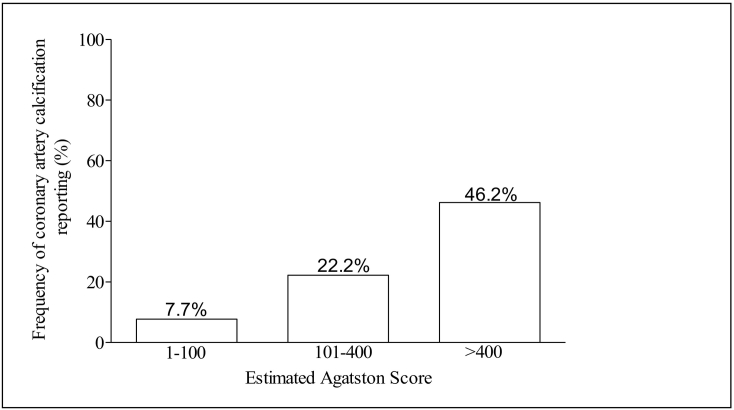
CAC was identified in 70 patients (26.2%) patients (Table 2). The most common artery to be involved was the LAD (22.9%) followed by the RCA(15.6%), LCx(14.3%) and LM(10.3%). The distribution of estimated Agatston scores were: 55.7% with a score between 1 and 100; 25.7% with a score between 101 and 400 and 18.6% with a score > 400.
Table 2.
Coronary artery calcification: frequency, extent and clinical reporting.
| Extent of coronary artery calcification (CAC) |
||
|---|---|---|
| Estimated Agatston Score | Number of patients | Frequency of CAC clinical reporting (%) |
| 0 | 193 | – |
| 1–100 | 39 | 7.7 |
| 101–400 | 18 | 22.2 |
| >400 | 13 | 46.2 |
3.3. Non coronary arterial calcification (NCC)
NCC was detected in 154 (58.6%) of CT studies, this was most commonly seen in the aorta (97.3%).
3.4. Clinical reporting of coronary artery calcification
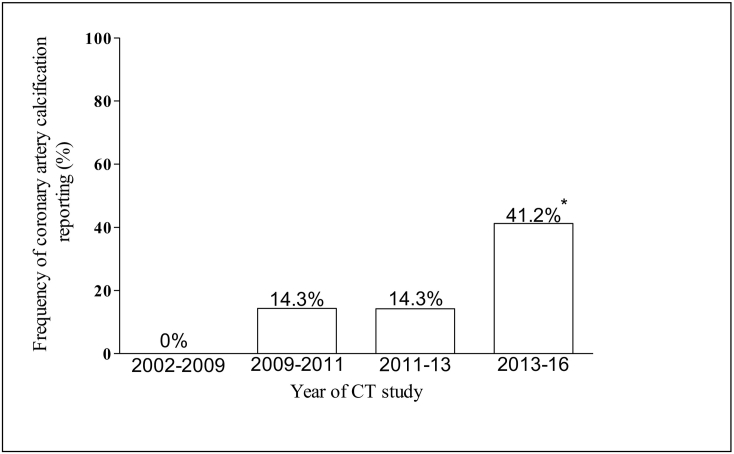
Reporting of coronary artery calcification was present on the clinical report of 13/70 (18.6%) of CT reports. Frequency of clinical reporting was associated with increasing CAC extent as measured by ordinal calcium scoring (Fig. 1, p < 0.0001, Pearson Chi Square 69.09). Temporal analysis of CAC reporting rates demonstrated an increase over the study period (Pearson's Chi-Square 8.73, p = 0.033). In the period from 2009 to 2011, 14.3% of CT scans with coronary calcium were reported clinically compared to 41.2% in the period 2013–2016 (Fig. 2). There was no association between the radiologist type (cardiac versus non cardiac) and the frequency of CAC reporting (Chi square statistic 1.98, p = 0.159). The time of the CT scan performance (working versus on call hours) did not appear to impact the frequency of CAC reporting (Chi square statistic 0.01, p = 0.914).
Fig. 1.
Relationship of Clinical Reporting with the Extent of CAC.
Legend: A positive linear relationship was demonstrated between the extent of CAC and CAC reporting rates (*p < 0.01).
Fig. 2.
The Temporal Relationship of CAC Reporting Rates.
Legend: A positive linear relationship was identified over the period of study and CAC reporting rates (*p < 0.05).
3.5. The rate of non-coronary arterial calcification reporting
NCC was clinically reported in (16, 10.4%) of cases. A similar analysis to CAC was performed for non-coronary vascular calcifications. The frequency of NCC reporting was associated with increasing CAC extent (Pearson's Chi Square statistic 58.63, p < 0.0001). Temporal analysis of NCC reporting rates demonstrated no change in reporting rates over the study period. Between 2009 and 201, clinical reports recorded NCC in 11.1% of CT scans with NCC versus 11.9% between 2013 and 2016 (Pearson's Chi Square statistic 6.149, p = 0.105). No significant relationships were found between the rate of reporting and the time of the CT acquisition (Chi-square statistic 3.45 p = 0.06) or the radiologist type (Chi Square statistic 0.79 p = 0.373).
4. Discussion
This single center retrospective observational study highlights the potential utility of using CT chest data to identify coronary and non-coronary arterial calcification in breast cancer patients at risk of cardiovascular events. We identified arterial calcification in 59% of 263 breast cancer patients attending a cardiac-oncology clinic who had a chest CT. We demonstrated low rates of clinical reporting of coronary or non-coronary arterial calcification (18.6% and 10.4% respectively) and noted that the rate of clinical reporting of CAC has increased in recent years.
By referral to a cardiac oncology clinic, the breast cancer patients evaluated in this study already had been established as high-risk for cancer therapy related cardiac dysfunction (CTRCD). National and international guidelines for the prevention of CTRCD recommend attention to cardiovascular risk factor stratification and optimization to prevent cardiovascular events [[15], [16], [17]]. The presence of CT chest data on 263/408 (64.5%) of the subjects screened indicates the potential utility of this available information to help further risk stratify patients for CTRCD.
In comparison to our study cohort, prior data has indicated a similar prevalence of coronary calcification in a population of breast cancer patients [8]. Coronary artery calcification was detected in 24% of subjects undergoing chest CT for radiotherapy planning [8]. Others have investigated the prevalence of arterial calcification on chest CT data performed as part of a lung screening program [[4], [5], [6], [7],20]. In 584 participants of a lung cancer screening trial, coronary arterial calcification was seen in 76% of patients [21]. The greater prevalence of CAC in this population could reflect the gender, age, or risk factor differences of the cohort studied in comparison to our data. Others have considered the relationship between CAC and extra coronary calcification (ECC) detected on chest CT in lung cancer screening studies. Using a visual estimate of the presence, severity and extent of ECC and CAC, correlation was noted between ECC and CAC (R = 0.515 p < 0.001) [4].
The prognostic utility of CAC and NCC detected by chest CT has also been considered in a lung cancer screening populations [5]. Increasing CAC and thoracic aortic calcification (TAC) was associated with all-cause mortality (p = 0.01 and p = 0.001 for CAC and TAC respectively) and cardiovascular events (p < 0.001 and 0.03 for TAC and CAC respectively). CAC was found to be a stronger predictor than TAC of all cause death and CV events. TAC was however a stronger predictor of non-cardiac CV events [5]. The value of CAC to predict clinical outcomes was also seen in 3559 male current or former smokers who underwent a CT chest scan as part a lung cancer screening program [20]. CAC was associated with increased risk of both fatal and non-fatal cardiovascular events over a median follow up of 2.9 years. The detection of extensive CAC (Agatston >400) in this population was associated with an increased hazard ratio of 12.58 (95% CI 5.42–29.16) in comparison to patients with no coronary calcification [20].
4.1. Clinical reporting of arterial calcification
In the current study CAC was reported in 18.6% and NCC in 10.4% of chest CT scans. Uretsky et al. reviewed 204 chest CT studies at their institution in patients without known CAD [10]. 108/204 (53%) of scans were found to have CAC when reviewed. CAC was reported clinically in only 68.4% of those with CAC (74/108 cases). Others have documented reporting rates of CAC on chest CTs of 44% [9].
Until recently there has not been guidelines, position statements or consensus for universal practice regarding the reporting of incidental CAC on chest CT exams [10]. The Society of Cardiovascular Computer Tomography (SCCT) and Society of Thoracic Radiology (STR) have however recently produced joint guidelines recommending the reporting of CAC on non-contrast, non-cardiac, chest CT studies [3]. They recommend reporting CAC on every scan: not just on those likely to be candidates for CAC screening. Scoring recommendations are also made by the guideline committees. They indicate that either visual estimate, ordinal scoring or Agatston techniques could be used depending on the availability of technologies and resources within the individual sites. The guidelines also acknowledge that for the reporting of CAC to have an impact clinically the CAC score should be linked to a risk classification system such as that provided by linking Agatston score to the age, gender and ethnicity associated population percentile for CAC [22].
The SCCT/STR guidelines are less prescriptive with regard to the reporting of NCC. The reporting of thoracic aortic calcification presence and extent was given a IIb recommendation at the time the guidelines were written. The absence of a class I recommendation was attributed to the lack of evidence for NCC to have prognostic utility [3]. The static nature of NCC reporting rates during the period of the present study may reflect this pragmatic approach and further data is awaited to help define the importance of NCC.
4.2. Factors affecting clinical reporting of CAC
Whether the chest CT was performed during the day or at night did not influence reporting rates, neither did the current practice of the radiologist (cardiac versus non cardiac). CAC extent positively increased CAC reporting rates. Despite this however in 77% of patients with estimated Agatston scores >400, coronary calcium was not declared on their clinical reports. CAC clinical reporting rates improved over time: 41.2% of studies with CAC were reported in 2013–2016 versus 0% in the years prior to and including 2009. During the study period the increased frequency of CAC reporting parallels the growing literature evidence of the value of CAC quantification, on non-gated chest CT, as a valid cardiovascular event/risk predictor.
4.3. Limitations
This was a retrospective observational study in a single center. As a single center study it may not represent more widespread clinical practice. We note that in the more recent years there was an observed increase in the reporting rates of coronary calcification. This may be more representative of current practice. Guidelines for the reporting of coronary calcium in non-gated CT studies have now emerged that may improve the rates of reporting in more contemporary practice and a prospective review could be considered [3]. The CT scans studied were from breast cancer patients attending a cardiac oncology referral clinic. It is possible that the rates of arterial calcification in our population might not be representative of a general breast cancer population. Original descriptions of coronary calcium scoring utilized a 3 mm section thickness [3]. Our study was a real world study utilizing chest CT studies that a employed a range of section widths. Others have demonstrated that the sensitivity of CAC detection may be reduced with wider (5 mm) in comparison to narrower sections (1 mm) although the specificity is reportedly well maintained at 90% across the section width employed in our study [23]. It is possible therefore that CAC determined from 5 mm sections may be underestimated and a more accurate estimation of Agatston score might be achieved by using <5 mm sections [19].
5. Conclusions
The importance of identifying incidental arterial calcification on chest CT scans is to highlight potential cardiovascular risk. This is relevant in the general population undergoing chest CT studies for chest pathologies as recognized by the recent SCCT/STR guidelines [3]. Arterial calcification is of particular importance in oncology patients where CAC is expected to be more prevalent and in whom cardiotoxic therapy may be under consideration [24,25]. The current study highlights the frequency of CAC in breast cancer patients and indicates that in a real world setting reporting rates have improved. It is hoped that clinical use of this information might improve cardiovascular outcomes in breast cancer patients.
Funding
This project was funded by a University of Ottawa Faculty of Medicine Mach-Gaensslen Foundation of Canada Award.
References
- 1.Hecht H.S. Coronary artery calcium scanning: past, present, and future. JACC Cardiovasc. Imaging. May 2015;8(5):579–596. doi: 10.1016/j.jcmg.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 2.Bos D., Leening M.J., Kavousi M. Comparison of atherosclerotic calcification in major vessel beds on the risk of all-cause and cause-specific mortality: the Rotterdam study. Circ. Cardiovasc. Imaging. December 2015;8(12) doi: 10.1161/CIRCIMAGING.115.003843. [DOI] [PubMed] [Google Scholar]
- 3.Hecht H.S., Cronin P., Blaha M.J. 2016 SCCT/STR guidelines for coronary artery calcium scoring of noncontrast noncardiac chest CT scans: a report of the Society of Cardiovascular Computed Tomography and Society of thoracic radiology. J. Thorac. Imaging. September 2017;32(5):W54–W66. doi: 10.1097/RTI.0000000000000287. [DOI] [PubMed] [Google Scholar]
- 4.Dirrichs T., Penzkofer T., Reinartz S.D., Kraus T., Mahnken A.H., Kuhl C.K. Extracoronary thoracic and coronary artery calcifications on chest CT for lung cancer screening: association with established cardiovascular risk factors - the “CT-Risk” trial. Acad. Radiol. July 2015;22(7):880–889. doi: 10.1016/j.acra.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 5.Jacobs P.C., Prokop M., van der Graaf Y. Comparing coronary artery calcium and thoracic aorta calcium for prediction of all-cause mortality and cardiovascular events on low-dose non-gated computed tomography in a high-risk population of heavy smokers. Atherosclerosis. 2010 April;209(2):455–462. doi: 10.1016/j.atherosclerosis.2009.09.031. [DOI] [PubMed] [Google Scholar]
- 6.Jacobs P.C., Gondrie M.J., van der Graaf Y. Coronary artery calcium can predict all-cause mortality and cardiovascular events on low-dose CT screening for lung cancer. AJR Am. J. Roentgenol. March 2012;198(3):505–511. doi: 10.2214/AJR.10.5577. [DOI] [PubMed] [Google Scholar]
- 7.Jairam P.M., de Jong P.A., Mali W.P., Gondrie M.J., Jacobs P.C., van der Graaf Y. Age and sex based reference values for incidental coronary artery and thoracic aorta calcifications on routine clinical chest CT: a powerful tool to appreciate available imaging findings. Atherosclerosis. August 2012;235(2):546–553. doi: 10.1016/j.atherosclerosis.2014.05.949. [DOI] [PubMed] [Google Scholar]
- 8.Gernaat S.A., Isgum I., de Vos B.D. Automatic coronary artery calcium scoring on radiotherapy planning CT scans of breast cancer patients: reproducibility and association with traditional cardiovascular risk factors. PLoS One. 2016;11(12) doi: 10.1371/journal.pone.0167925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams K.A., Sr., Kim J.T., Holohan K.M. Frequency of unrecognized, unreported, or underreported coronary artery and cardiovascular calcification on noncardiac chest CT. J. Cardiovasc. Comput. Tomogr. May 2013;7(3):167–172. doi: 10.1016/j.jcct.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 10.Uretsky S., Chokshi N., Kobrinski T. The interplay of physician awareness and reporting of incidentally found coronary artery calcium on the clinical management of patients who underwent noncontrast chest computed tomography. Am. J. Cardiol. 2015 June 1;115(11):1513–1517. doi: 10.1016/j.amjcard.2015.02.051. [DOI] [PubMed] [Google Scholar]
- 11.Kirsch J., Martinez F., Lopez D., Novaro G.M., Asher C.R. National trends among radiologists in reporting coronary artery calcium in non-gated chest computed tomography. Int. J. Card. Imaging. 2017 February;33(2):251–257. doi: 10.1007/s10554-016-0986-x. [DOI] [PubMed] [Google Scholar]
- 12.Patnaik J.L., Byers T., DiGuiseppi C., Dabelea D., Denberg T.D. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: a retrospective cohort study. Breast Cancer Res. June 20 2011;13(3):R64. doi: 10.1186/bcr2901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bhatia N., Lenihan D., Sawyer D.B., Lenneman C.G. Getting the SCOOP-survey of cardiovascular outcomes from oncology patients during survivorship. Am J Med Sci. 2016 June;351(6):570–575. doi: 10.1016/j.amjms.2016.01.025. [DOI] [PubMed] [Google Scholar]
- 14.Shum K., Solivan A., Parto P., Polin N., Jahangir E. Cardiovascular risk and Level of statin use among women with breast cancer in a cardio-oncology clinic. Ochsner J. 2016;16(3):217–224. [PMC free article] [PubMed] [Google Scholar]
- 15.Virani S.A., Dent S., Brezden-Masley C. Canadian cardiovascular society guidelines for evaluation and Management of Cardiovascular Complications of cancer therapy. Can. J. Cardiol. 2016 July;32(7):831–841. doi: 10.1016/j.cjca.2016.02.078. [DOI] [PubMed] [Google Scholar]
- 16.Armenian S.H., Lacchetti C., Barac A. Prevention and monitoring of cardiac dysfunction in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J. Clin. Oncol. March 10 2017;35(8):893–911. doi: 10.1200/JCO.2016.70.5400. [DOI] [PubMed] [Google Scholar]
- 17.Zamorano J.L., Lancellotti P., Rodriguez M.D. 2016 ESC position paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for practice guidelines: the task force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC) Eur. J. Heart Fail. January 2017;19(1):9–42. doi: 10.1002/ejhf.654. [DOI] [PubMed] [Google Scholar]
- 18.Gayed I.W., Raslan O.A., Bhosale P.R., Perrier N.D., Wei W., Gladish G. Significant coronary calcification detected using contrast-enhanced computed tomography: is it an indication for further investigation? Clin. Nucl. Med. June 2010;35(6):404–408. doi: 10.1097/RLU.0b013e3181db4ad6. [DOI] [PubMed] [Google Scholar]
- 19.Azour L., Kadoch M.A., Ward T.J., Eber C.D., Jacobi A.H. Estimation of cardiovascular risk on routine chest CT: ordinal coronary artery calcium scoring as an accurate predictor of Agatston score ranges. J. Cardiovasc. Comput. Tomogr. January 2017;11(1):8–15. doi: 10.1016/j.jcct.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 20.Takx R.A., Isgum I., Willemink M.J. Quantification of coronary artery calcium in nongated CT to predict cardiovascular events in male lung cancer screening participants: results of the NELSON study. J. Cardiovasc. Comput. Tomogr. January 2015;9(1):50–57. doi: 10.1016/j.jcct.2014.11.006. [DOI] [PubMed] [Google Scholar]
- 21.Jacobs P.C., Isgum I., Gondrie M.J. Coronary artery calcification scoring in low-dose ungated CT screening for lung cancer: interscan agreement. AJR Am. J. Roentgenol. May 2010;194(5):1244–1249. doi: 10.2214/AJR.09.3047. [DOI] [PubMed] [Google Scholar]
- 22.McClelland R.L., Chung H., Detrano R., Post W., Kronmal R.A. Distribution of coronary artery calcium by race, gender, and age: results from the multi-ethnic study of atherosclerosis (MESA) Circulation. January 3 2006;113(1):30–37. doi: 10.1161/CIRCULATIONAHA.105.580696. [DOI] [PubMed] [Google Scholar]
- 23.Kim S.M., Chung M.J., Lee K.S., Choe Y.H., Yi C.A., Choe B.K. Coronary calcium screening using low-dose lung cancer screening: effectiveness of MDCT with retrospective reconstruction. AJR Am. J. Roentgenol. April 2008;190(4):917–922. doi: 10.2214/AJR.07.2979. [DOI] [PubMed] [Google Scholar]
- 24.Mast M.E., Heijenbrok M.W., Petoukhova A.L., Scholten A.N., Schreur J.H., Struikmans H. Preradiotherapy calcium scores of the coronary arteries in a cohort of women with early-stage breast cancer: a comparison with a cohort of healthy women. Int. J. Radiat. Oncol. Biol. Phys. July 1 2012;83(3):853–858. doi: 10.1016/j.ijrobp.2011.08.012. [DOI] [PubMed] [Google Scholar]
- 25.Whitlock M.C., Yeboah J., Burke G.L., Chen H., Klepin H.D., Hundley W.G. Cancer and its association with the development of coronary artery calcification: an assessment from the multi-ethnic study of atherosclerosis. J. Am. Heart Assoc. November 9 2015;4(11) doi: 10.1161/JAHA.115.002533. [DOI] [PMC free article] [PubMed] [Google Scholar]