Abstract
Background
Childhood obesity preventive interventions should promote a healthy diet and physical activity at home and school. This study aims to describe a school-based childhood obesity preventive programme (POIBA Project) targeting 8-to-12- year-olds.
Design and methods
Evaluation study of a school-based intervention with a pre-post quasi-experimental design and a comparison group. Schools from disadvantaged neighbourhoods are oversampled. The intervention consists of 9 sessions, including 58 activities of a total duration between 9 and 13 hours, and the booster intervention of 2 sessions with 8 activities lasting 3 or 4 hours. They are multilevel (individual, family and school) and multicomponent (classroom, physical activity and family). Data are collected through anthropometric measurements, physical fitness tests and lifestyle surveys before and after the intervention and the booster intervention. In the intervention group, families complete two questionnaires about their children’s eating habits and physical activity. The outcome variable is the cumulative incidence rate of obesity, obtained from body mass index values and body fat assessed by triceps skinfold thickness. The independent variables are socio-demographic, contextual, eating habits, food frequency, intensity of physical activity and use of new technologies.
Expected impact for public health
It is essential to implement preventive interventions at early ages and to follow its effects over time. Interventions involving diet and physical activity are the most common, being the most effective setting the school. The POIBA Project intervenes in both the school and family setting and focuses on the most disadvantaged groups, in which obesity is most pronounced and difficult to prevent.
Significance for public health.
Overweight and obesity are a major public health concern that predispose affected individuals to the development of chronic diseases. Of importance, obesity is more common among disadvantaged neighbourhoods and it is precisely these environments that have the lowest involvement in preventive interventions. Consequently, it is very important to target these populations when designing an intervention. This study will provide an evaluated childhood obesity intervention which includes the perspective of gender and social inequalities. In addition, a sustainability plan has been developed for the intervention. It is planned that, in the near future, the intervention and its reinforcement are part of the set of health educational programmes offered by the Agència de Salut Pública de Barcelona (Spain) to schools, with funding both the cost of the training and the materials borne by the Agència.
Key words: School-based intervention programme, Evaluation, Lifestyle, Eating habits, Physical activity
Introduction
Overweight and obesity are a major public health concern characterised by an increase in body fat. Overweight or obese children are more likely to remain obese in adulthood and to have cardiovascular disease at younger ages.1
In the last few decades, the prevalence of overweight and obesity has steadily increased in most developed countries. A study in 6- to 9-year-olds from 12 European countries participating in the European Childhood Obesity Surveillance Initiative (COSI) of the World Health Organisation (WHO) concluded that the prevalence of overweight (including obesity) ranged from 19.3% to 49% in boys and from 18.4% to 42.5% in girls, depending on the country. For obesity, the prevalence ranged from 6.0% to 26.6% in boys and from 4.6% to 17.3% in girls. These data show a north-south pattern with the highest prevalence of obesity in southern European countries.2
Spain has one of the highest prevalence of overweight and obesity in Europe. The enKid study3 found that, among 2- to 24- year-old, 12.4% were overweight and 13.9% were obese in 2000, while a more recent study in 20124 showed that, among 8- to 17- year-olds, 26.0% were overweight and 12.6% were obese.
The causes of overweight and obesity are multifactorial, with multiple complex determinants. The main social factors supported by evidence are having a disadvantaged socioeconomic status (SES), and belonging to an immigrant or a single-parent family.5 Genetic and family factors such as maternal overweight during pregnancy5 and not having been breastfeed play an important role in the development of childhood obesity.6 Additionally, notable lifestyle-related determinants are those linked to eating habits, unhealthy food, low physical activity,7 excessive screen time (which encourages a sedentary lifestyle)8 and fewer hours of sleep.
Body mass index (BMI) is a measure of the association between weight and size, which varies depending on age and gender and is considered the main indicator of weight problems. BMIbased definitions of overweight and obesity are clear in adults but controversial in children. In Spain, the curves and tables of the Orbegozo Foundation9 have been used in clinical practice. In recent years, the WHO has encouraged the use of the z-scores,10 which are based on standard deviations (SD). Nevertheless, some authors argue that body fat distribution, measured by skinfold thickness, may be a more sensitive and simpler obesity indicator in children aged 6 to 10 years.11
A Cochrane systematic review on interventions for preventing obesity in children showed that the most effective interventions are those addressed to children aged 6 to12 years old and most of them are based on theories of behaviour change and developed at school. Most interventions include content related to diet (88%) or programs related to physical activity (88%) and almost 100% apply content on healthy lifestyle. In addition, evidence is needed on the long-term effects of these interventions, beyond three years, as well as on knowing the impact of each component on multifactor interventions.12
There are few studies on the prevalence of childhood obesity in Spanish and Catalan child population with representative samples. 3,4,13 Additionally, none of these studies deepens in the differences between advantaged and disadvantaged populations. Therefore, the childhood obesity prevention programme in Barcelona (POIBA Project) aims to determine the true prevalence of the problem and to devise solutions. The conceptual framework of the project is based on Dahlgren and Whitehead’s 1991 model of social determinants.14 Likewise, the POIBA Project includes a school-based intervention, in which most determinants are those relating to lifestyles, addressing mainly those of behavioural kind. The aim of this paper is to describe in detail the methodology of the POIBA project and the intervention designed in its framework.
Objectives
General objective of the project POIBA
The childhood obesity prevention programme in Barcelona (POIBA Project) aims to design and evaluate the effectiveness of a multilevel (individual, family and school level) and multicomponent (classroom, physical activity and family) intervention to prevent overweight and obesity among 8- to 12-year-olds. The project includes the perspective of gender and social inequalities.
Specific objectives
The specific objectives are the following ones:
To design an obesity preventive intervention that would improve diet-related attitudes and skills, increase physical activity, reduce screen time, and increase hours of sleep.
To design and validate an ad hoc questionnaire to gather information on food, sedentariness and physical activity and other data related to overweight and obesity.
To identify the prevalence of overweight and obesity by means of BMI calculation and body fat measurement (triceps skinfold thickness).
To assess the effectiveness of the intervention according to the characteristics of the pupils, their families and schools.
To study the homogeneity of the effect of the intervention in subpopulations of schools in low SES neighbourhoods and subpopulations of immigrant families.
Hypothesis
The main hypothesis of this study is that the incidence of obesity measured by BMI and body fat (triceps skinfold) in pupils in the Intervention Group (IG) will be significantly lower compared with that in pupils in the Comparison Group (CG).
Other hypotheses are that the intervention will: i) improve their diet, increase their physical activity, reduce screen time (TV, computer and video games) and increase hours of sleep. ii) Improve parents’ and children’s attitudes towards diet, sedentariness and lack of physical exercise, as well as increase the consumption of healthy food and the practice of physical exercise in children directly. iii) Reduce exposure to obesogenic environments by increasing the frequency of visits to healthy eating establishments and the practice of physical exercise made by children. iv) Achieve similar effects in different student subgroups, regardless of SES or birth country.
Design and Methods
Study design
It is an evaluation study of an intervention with a pre-post quasi-experimental design with a comparison group. Effects of the intervention in a group of schoolchildren, the Intervention Group, are compared with another group not exposed to the intervention, the Comparison Group.
Study population and setting
The study involves 4139 pupils from 104 schools in Barcelona aged 8-9 years at baseline, of which 3624 were enrolled in the study (a non-response rate of 12.4%). The main causes of non-participation were parental refusal to allow their children to participate in the study and pupil absence from the classroom at the time of data collection.
Among the 10 districts of the city, 4 of them were conveniently assigned to the IG and the other 6 to the CG, in order to oversample the schools located in disadvantaged neighbourhoods. Once it was decided which districts of the city would be part of the IG and which of the CG, the schools located in those districts were randomly selected. The IG was composed of 1633 children in 47 schools (75 classrooms). In this group, half the schoolchildren attend schools located in disadvantaged neighbourhoods. The CG was composed of 1991 children attending 57 schools (97 classrooms) where, similar to the IG, half of the schools were randomly selected from disadvantaged neighbourhoods, to achieve comparability between the IG and the CG. The composition of the sample at different stages of the project is shown in Figure 1. SES was measured according to the Gross Disposable Household Income (GDHI),15 an ecological indicator that measures the average family purchasing power for each neighbourhood; neighbourhoods with a GDHI ≥85 are considered to be advantaged and those <85 to be disadvantaged. The sample was stratified according to the SES of the neighbourhood of the school, its ownership (state or subsidised) and the size or number of year 4 primary school classrooms. The schools were randomly selected following the same distribution of these strata for schoolchildren in the city. Others schools belonging to the same SES and type of school replaced those that refused to participate in the study.
Figure 1.
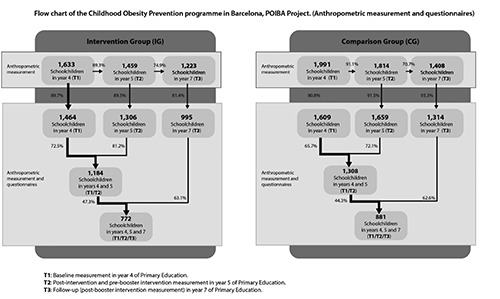
Flow chart of the Childhood Obesity Prevention programme in Barcelona (POIBA Project).
The project begun in January 2009, when pupils were 8-9 years old, and it is planned to follow-up the students until they are 17-18 years old.
Ethics approval
The project has been evaluated and approved by the Clinical Research Ethics Committee of Parc de Salut Mar (CEIC-Parc Salut Mar), reference number 2009/3470/l.
During the study, national and international guidelines are followed (codes of professional ethics, the Helsinki Declaration of 1964 and subsequent revisions). Additionally, the Spanish law on data confidentiality was observed (Law 15/1999 of 13 December on Personal Data Protection). Parents provided signed consent for their children to participate in the project. All information is protected by using data management and information storage procedures.
Sample size calculation and final study sample
A sample size of 2450 schoolchildren allows detection of a 3- point decrease in the prevalence of obesity (for example, a reduction in prevalence from 10.4% to 7.4%) with an alpha error of 5 (error type I of 0.05) and statistical power of 80 (type II of 0.20 error), assuming 15% of losses between the initial examination and the post-intervention. In the analysis, the intraclass correlation involving group sampling will be taken into account. A total of 40 schools and 100 classrooms in each group were required to obtain 2450 schoolchildren in each group. Other factors influencing school selection were the type of school (state or subsidised) and the size or number of year 4 primary school classrooms. Therefore, the required study sample size was 4900 students, with 2450 students in each group (40 schools, 100 classrooms).
In practice, the schools enrolled in the study have a total of 4139 schoolchildren because, in some strata, the schools refused to participate and the possibilities of replacing them were exhausted. Of these 4139 students, 3624 participate in the study, representing a non-participation rate of 12.4%.
Procedure
Study development
A pilot study was conducted in 92 children aged between 9 and 10 years attending year 5 in two schools of Terrassa (Catalonia, Spain).
Intervention
The global intervention We grow up healthy was developed by taking into consideration the characteristics and specific needs of people with low SES and from immigrant communities. The intervention is multilevel (individual, family and school) and multicomponent (classroom, physical activity and family) and is addressed to year 5 pupils.16 The main contents are those related to promoting a healthy diet and proper energy balance, the practice of at least 60 minutes of physical activity daily, a maximum of 2 hours screen time and a minimum of 9 hours of sleep per night. A detailed description of the intervention is shown in Table 1.
Table 1.
Components of the childhood obesity prevention programme (POIBA) intervention.
| Level of intervention | Type of intervention | Contents | Preventive activities | Techniques | Materials |
|---|---|---|---|---|---|
| Individual | We grow up healthy (Classroom intervention) | 3 modules with the following contents: - Module 1: Growth: weight and height. Body image assessment - Module 2: Food and nutrition: digestion, food groups, nutrients and their functions, food pyramid and proper breakfast - Module 3: Physical activity and rest; summary and synthesis of the intervention |
- Module 1: 2 sessions (15 activities) - Module 2: 5 sessions (31 activities) - Module 3: 2 sessions (12 activities) |
Lectures; Active teaching (questions and answers); Discussion | Teacher’s guide; Pupil’s notebook; Family booklet; Digital platform “Edu Natura” (Module 2); Interactive video game Menja’t el coco” (Module 3) |
| We move to grow up healthy (Physical activity intervention) | 3 content blocks to meet the recommendation of ≥6 hours of physical activity per week: - School: assurance of ≥2 hours/week of physical education in the curriculum - Extracurricular: promotion of ≥2 hours/week of activities outside school; register of activities (including sports competitions); funding of activities for families with economic difficulties - Leisure time: promotion of ≥2 hours/week participation in recreational activities at weekends |
- Block 1: (1 activity) - Block 2: (3 activities) - Block 3: (1 activity) ≥6 hours/week (school, extracurricular and leisure time) |
Information on physical education; Discussion; Register of activities | Teacher’s guide for physical education teachers; Physical activity register; Physical fitness register | |
| Family | A plan for change (workshop) | Family involvement in: - workshop on food and physical activity (1.5 hours) - activities from the family booklet (7 activities) - 3 activities on the digital platform Edu Natura |
1 workshop 10 activities | Explanation in the workshops | 5 suitcases of activities for the workshop; Sheet “A plan for change”; Family booklet |
| School | Set of actions including: - Review of the content of the school menu - Improving the availability of healthy food in the canteen - Promoting the opening of playgrounds |
3 activities | Revision; Didactic information | Informative documents |
Individual level
The classroom intervention is implemented in the classroom throughout the school year by a teacher previously trained by staff at the Agència de Salut Pública de Barcelona. The sessions are divided into three work modules, consisting of 58 activities distributed into nine teaching sessions with an overall duration of between 9 and 13 hours. The sessions last between 55 and 110 minutes. Each module presents activities for the classroom and the family environment. The first module consists of two sessions and focuses on personal growth and body image, the second module consists of five sessions on diet (food and nutrition) and the third is composed of two sessions on physical activity and rest. In the case of immigrant families, the specific needs taken into consideration have to do mainly with their eating habits. In the design of these activities cultural diversity was taken into account so that schoolchildren belonging to immigrant communities could be represented. Thus, as an example, the breakfast session included foods consumed by other cultures such as Arabic bread in the case of cereals or papaya and mango in the case of fruits (Table 1).
The physical activity intervention is applied by physical education teachers with the support of the Agència de Salut Pública de Barcelona. It seeks to intensify physical activity during school hours, after school and in leisure time among pupils. The project funds extracurricular activities to those pupils whose families have economic difficulties. These activities were chosen by each beneficiary family based on the children’s preferences, with the most popular being soccer, basketball and swimming.
Family level
Families collaborate by carrying out some activities from the family booklet and participating in a workshop which aimes to provide families with skills and strategies to achieve a healthy, full and balanced diet and to improve their sleep hygiene. The workshop is held at the school premises in parallel with the intervention. The estimated duration is 1.5 hours. At the end of the workshop, parents and children have to agree on which aspect of diet or physical activity they will attempt to improve.
School level
A set of actions in the school are implemented in parallel with the intervention to achieve a healthier environment such as reviewing the school menu, increasing the availability of healthy food in the canteen and promoting the opening of playgrounds.
Booster intervention
A reinforcement of the multilevel and multicomponent intervention, We grow up more healthy, is carried out 2 years later when the pupils are enrolled in year 7 of primary school, aged 11 to 12 years old16. The contents follow the same line as the intervention, strengthening the work previously developed with pupils on improvement in the family diet and increase physical activity at weekends (Table 2).
Table 2.
Components of the childhood obesity prevention programme (POIBA) booster intervention.
| Level of intervention | Type of intervention | Contents | Preventive activities | Techniques | Materials |
|---|---|---|---|---|---|
| Individual | We grow up more healthy (Classroom booster intervention) | 2 sessions with the following contents: - Session 1: Remember the food pyramid - Session 2: A balanced diet 1 session with the following contents: - Session 3: Register of the physical activity taken and rest during 1 month (week and weekend); Information about sporting events on the weekend |
8 activities 3 activities; ≥6 hours/week exercise (school, extracurricular and leisure time) | Didactic teaching; Active teaching (questions and answers); Discussion Information on physical education; Discussion; Register of activities | Teaching guide; Pupil’s notebook; Family booklet Teacher’s guide for physical education teachers; Physical activity and rest register; Physical fitness register; Set of sports equipment; Reward for attending sports events at weekends |
| Family | Let’s get active at the weekend (Physical activity booster intervention) | Family involvement in: - A workshop on improvements in meals and weekend physical activity (1 hour) - Attendance at ≥ 4 events on weekends |
1 workshop 4 activities | Explanation in the Workshops; Didactic information | Teaching material for the workshop; Family booklet; Information sheet on sports events |
| School | Let’s improve family health (Workshop) | Set of actions including: - Review of the content of the school menu - Increasing the availability of healthy food in the canteen - Promoting playground opening - Promoting the opening of playgrounds |
3 activities | Revision; Information | Informative documents |
Individual level
The classroom booster intervention is implemented by the teacher. It consists of eight activities distributed in two teaching sessions, with a scheduled duration of between 3 and 4 hours of class. The first session is a refresher of the contents of the previous intervention on the food pyramid. The second session aimes to introduce in detail the concept of portions of food groups and the distribution of servings in a balanced diet for a whole week.
The physical activity booster intervention is implemented by physical education teachers as a single session comprising three activities in the physical education schedule. It consists of recording the physical activity taken by each pupil in 1 month, both during the week and at the weekend. Pupils whose families have financial difficulties receive subsidies for extracurricular physical activity.
Family level
Family involvement in the booster intervention basically focuses on the workshop, carried out at the school in parallel with the booster intervention. Families attend together with their children to the workshop, which lasts 1 hour. The objective of the workshop is to negotiate and agree on improvements at meals and physical activity at the weekend.
School level
These actions are a continuation of those initiated in the intervention.
Data collection
A series of measures are included in the study in both the IG and CG. To avoid problems due to seasonality, the measurements are carried out at the same time of year. Figure 2 shows the evaluative design of the project, the pilot test, the intervention and the booster intervention. An alpha numeric code is created for each pupil.
Figure 2.
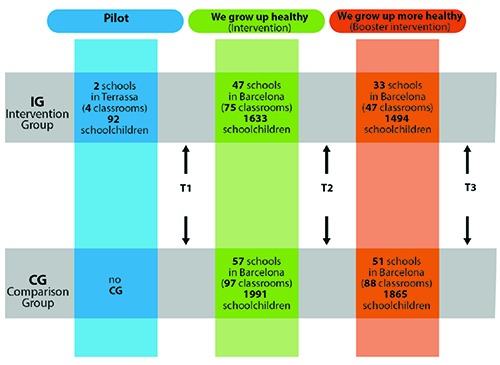
Evaluative design of the POIBA Project.
Procedure with schoolchildren
Baseline measurement (T1): Between April and June 2011, year 4 of primary education (8-9 years old).
Post-intervention and pre-booster intervention measurement (T2): Between April and June 2012, year 5 of primary education (9-10 years old).
Follow-up (post-booster intervention measurement) (T3): Between April and June 2014, year 7 of secundary education (11-12 years).
Long-term follow-up: T4: Between November and December 2016, year 9 of secondary education (13-14 years old). T5: Between November and Decembrer 2020, year 13 of secondary education (17-18 years old).
Currently the project has completed the data collection of the long-term follow-up T4.
The measurements and the information sources are described below.
Anthropometric measurements
Objective data (weight, size, triceps skinfold thickness and waist and hip circumference) are measured in the classroom by trained personnel from the Agència de Salut Pública de Barcelona, with prior informed consent from the families. This allowe BMI and triceps skinfold thickness calculation, as well as data collection on overweight and obesity.
Behavioural determinants of overweight and obesity
he independent variables of the study are those related to knowledge, attitudes and behaviours regarding diet and nutrition, physical activity, a sedentary lifestyle and sleep duration. These variables are collected through two validated self-administered computerised questionnaires.16 POIBA-How do we eat? consists of 74 questions gathering information about food frequency and eating habits. The POIBA-How do we move? questionnaire consists of 39 questions collecting information on physical activity and use of new technologies. Both questionnaires elicits sociodemographic information.
Measurement of physical fitness
An adaptation of the Eurofit battery is used for children aged between 8 and 10 years, which was designed with the advice of experts in the field. The battery consists of six tests, three of which were adapted instead of including the original tests. The adapted tests are 20 metre shuttle run test (Beep test), vertical jump and displacement in zig-zag with a ball.
Although most of the Eurofit tests are valid for pupils aged 11- to 12-year-olds, they have also been adapted because this population is in the lower age limit of the Eurofit battery application. The adjusted tests are adapted abdominals exercises and trunk forward flexion.
Parental procedure
The families of the pupils in the IG complete two self-administered questionnaires during the T1 period. POIBA-How do our children eat? collects information on food consumption and eating habits and POIBA-How do our children move? gathers information on school extracurricular activities, leisure time activities and sleep duration.
It was not possible to survey the families beyond T1 due to feasibility problems. Therefore, in the project we will have information about the families at the beginning, which will allow us to know the baseline point. The evolution of family habits throughout the project will be collected by schoolchildren questionnaires, who at the age of 8-12 years are a reflection of their family habits.
School procedure
Information regarding the school environment is collected through a self-report completed by school staff and another by the professional who reviews the school menu.
Variables
Outcome variables
The outcome variables are the cumulative incidence rate (CIR) and the prevalence of overweight and obesity. The CIR is defined as the change in the percentage of children with childhood overweight or obesity between baseline and follow-up. It is constructed from the values of BMI and triceps skinfold thickness. BMI is calculated based on weight and height and according to age and gender, following the WHO z-score definitions,10 which are based on standard deviations (SD). In addition, data on triceps skinfold thickness are calculated according to percentiles of the National Health and Nutrition Examination Survey (NHANES) of the Centers for Disease Control and Prevention (CDC).17
Independent variables
The independent variables are obtained from questionnaires and physical fitness tests.
Both questionnaires collect individual sociodemographic variables and contextual variables. POIBA-How do we eat? collects variables related to eating habits and food frequency. Information on physical activity in school, after school and in free time and use of new technologies is collected through the POIBA-How do we move? questionnaire. The variables gathered by the physical fitness examination are those relating to the results obtained by the schoolchildren in the six tests that composed the batteries.
Data analysis
A descriptive and bivariate analysis will be conducted between the independent and dependent variables. Chi-square Pearson contrasts will be used to observe relationships among the variables studied, with significance set at 5%. The Cohen test will be used to indicate the standardised effect size. Bivariate logistic regression models will be calculated between overweight and obesity and social determinants and lifestyle, obtaining odds ratios and 95% confidence intervals. A multivariate logistic regression model will be adjusted with the significant variables in the bivariate analysis. The possible interactions in the model will be taken into account. A generalised estimating equation will be used to estimate the parameters of a generalised linear model with a possible unknown correlation between outcomes. Finally, multilevel models are appropriate for research designs that organise data for participants at more than one level (i.e., nested data). The units of analysis will be individuals (at a lower level) who are nested within contextual/aggregate units (at a higher level). All analyses will be stratified by sex. Data will be analysed using the statistical packages SPSS v.13 and Stata/SE v.13.1.
Discussion
Obesity has become one of the main public health problems in Spain, because it affects a high percentage of our child and adult population.2-4 This problem is most prevalent among disadvantaged and immigrant populations. Because childhood and adolescent obesity is a predictor of adult obesity, preventive interventions should be implemented at an early age. Most interventions addressed to children younger than 10 years are school-based. In 2006, Flynn et al. reviewed the actions that can be carried out in childhood and youth to reduce obesity and associated chronic diseases. 18 Among these activities, the most common were those related to food education and the practice of physical activity, the school being the main setting to achieve a positive impact. The design of the POIBA Project is in line with these guidelines. This project is a school-based childhood obesity prevention programme that aims to provide children and their families with the knowledge, skills and means necessary to make healthy life choices in terms of food, physical activity, rest and screen viewing.
Defining overweight and obesity is more difficult in the child than in the adult population. This is due to the difficulty of establishing clear criteria for the paediatric age group to classify persons as overweight or obese based on BMI, which is the main indicator of weight problems, since BMI cannot distinguish between lean and fat body mass. Consequently, some authors argue that distribution of body fat is a more sensitive indicator than BMI for determining body fatness in children and adolescents, for monitoring obesity in children and for predicting high adult body fatness.11 The percentage of body fat can be calculated based on the height, weight and thickness measurements of four skinfolds (biceps, triceps, subscapular and suprailiac).19 If only one skinfold can be measured, it is recommended to use the triceps skinfold.11 Thus, in the POIBA Project, the triceps skinfold measurement is also carried out, since its measurement is feasible and relatively inexpensive.
Some school-based childhood obesity preventive interventions, in which an improvement of the unhealthy habits has been shown, have been carried out in our country20 and Europe21 previously. The contribution of the POIBA Project intervention to these studies is based on the fact that it is a multilevel and multi-component intervention addressed to children from 8 to 12 years old, which allows to involve in the activities not only the children but also their families and the school community.
Our study has several methodological limitations. Those concerning the intervention include the difficulties arising from the absence of a regular education schedule for health in school. Nevertheless, about one third of the school population of the cohort born in 2002 participate in the study. Even though randomisation is not an essential criterion in evaluative studies, one of the possible evaluation drawbacks could be that the CG and the IG could not be randomised because there had been contamination between groups. However, to minimise this effect, the schools were randomly selected and stratified by the main confounding factors and the cluster-randomization was taken into account in the sample size calculation. Information bias is common in self-reported questionnaires but both questionnaires have been previously validated. Finally, because this is a follow-up study, another possible limitation could be data matching attrition but this has been minimised to 25% to 30%.
A major strength of the study is that it is the first to obtain data on overweight, obesity and its main determinants in children in a large sample of the city of Barcelona. Additionally, this study is part of a broader project that will address the prevention of childhood obesity in preschool and primary schoolchildren, addressing individual, family, school and community components, following them until the adolescence. Another important strength is that a sustainability plan has been developed for the intervention.
Expected impact on public health
Prevention of childhood obesity is one of the main aims in current health policies due to its increased prevalence in our environment. The POIBA Project focuses on education on nutrition and physical activity, the latter being the critical intervention in programmes for the prevention and reduction of childhood obesity. This project focuses specifically on the most disadvantaged groups, which are most at risk and which receive the least support. It also intervenes in the family and school environment. Thus, the current project, based on theoretical design models and especially focused on reducing inequalities through economically sustainable and feasible actions, could become a local and national model for preventive intervention.
Acknowledgements
The authors would like to thank the schools for their collaboration in the project, the staff of the Terrassa City Council Department of Community Health for their strong involvement in the pilot study, the nurses of the Community Health Department of the Agència de Salut Pública de Barcelona who established contacts with the schools and are involved in the body composition examinations. Finally, the authors are grateful to the Technogym Company for allowing us to use the accelerometers necessary for the study free of charge.
Funding Statement
Funding: the study has been partially funded by the Fondo de Investigación Sanitaria (PI09/02259), of the Carlos III Health Institute (Ministry of Economy and Competitiveness, Spanish Government) and by the Agència de Salut Pública de Barcelona. Font Vella and Danone Companies have paid for copies of some materials. The funding bodies have no role in the design of the study and collection, analysis, interpretation of data and writing the manuscript.
References
- 1.World Health Organization. Childhood overweight and obesity. Press Centre. 2012. http://www.who.int/dietphysicalactivity/childhood/en/ . Accessed 7 Mar 2016. [Google Scholar]
- 2.Wijnhoven TM, van Raaij JM, Spinelli A, et al. WHO European Childhood Obesity Surveillance Initiative 2008: weight, height and body mass index in 6-9-year-old children. Pediatr Obes 2013;8:79-97. [DOI] [PubMed] [Google Scholar]
- 3.Serra Majem L, Ribas Barba L, Aranceta Bartrina J, et al. Obesidad infantil y juvenil en España. Resultados del estudio enKid (1998-2000). Med Clin (Barc) 2003;121:725-32. [DOI] [PubMed] [Google Scholar]
- 4.Sánchez-Cruz JJ, Jiménez-Moleón JJ, Fernández-Quesada S, Sánchez MJ. Prevalencia de obesidad infantil y juvenil en España en 2012. Rev Esp Cardiol 2013;66:371-6. [DOI] [PubMed] [Google Scholar]
- 5.Moens E, Braet C, Bosmans G, Rosseel Y. Unfavourable family characteristics and their associations with childhood obesity: A cross-sectional study. Eur Eat Disord Rev 2009;17:315-23. [DOI] [PubMed] [Google Scholar]
- 6.Sanders RH, Han A, Baker JS, Cobley S. Childhood obesity and its physical and psychological co-morbidities: a systematic review of Australian children and adolescents. Eur J Pediatr 2015;174:715-46. [DOI] [PubMed] [Google Scholar]
- 7.Román-Viñas B, Serra-Majem L, Ribas-Barba L, Pérez-Rodrigo C. Actividad física en la población infantil y juvenil española en el tiempo libre. Estudio enKid (1998-2000). Apunts Medicina de l’esport 2006:151:86-94. [Google Scholar]
- 8.de Jong E, Visscher TL, HiraSing RA, et al. Association between TV viewing, computer use and overweight, determinants and competing activities of screen time in 4- to 13-yearold children. Int J Obes (Lond) 2013;37:47-53. [DOI] [PubMed] [Google Scholar]
- 9.Hernández M, Castellet K, Narvaiza JL, et al. Curvas y tablas de crecimiento. Instituto sobre Crecimiento y Desarrollo Fundación F. Orbegozo. Madrid: Editorial Garsi, 1988. [Google Scholar]
- 10.World Health Organization. Growth reference 5-19 years. 2013. http://www.who.int/growthref/who2007_bmi_for_age/en/ Accessed 28 Jul 2017. [Google Scholar]
- 11.Nooyens AC, Koppes LL, Visscher TL, et al. Adolescent skinfold thickness is a better predictor of high body fatness in adults than is body mass index: the Amsterdam Growth and Health Longitudinal Study. Am J Clin Nutr 2007;85:1533-9. [DOI] [PubMed] [Google Scholar]
- 12.Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2011;12. [DOI] [PubMed] [Google Scholar]
- 13.NAOS Strategy. Results of the ALADINO study. AECOSAN. Ministerio de Sanidad, Política Social e Igualdad, 2014. [Google Scholar]
- 14.Dahlgren G, Whitehead M. (1991). Policies and strategies to promote equity in health. Stockholm: Institute for Futures Studies. [Google Scholar]
- 15.Barcelona Economia. Indicadors economics de Barcelona i de la regió metropolitana 2009:79-87. [Google Scholar]
- 16.Agència de Salut Pública de Barcelona. POIBA project. Available from: http://www.aspb.cat/poiba/. Accessed 28 Jul 2017. [Google Scholar]
- 17.Fryar CD, Gu Q, Ogden CL. Anthropometric reference data for children and adults: United States, 2007-2010. National Center for Health Statistics. Vital Health Stat 2012;11. [PubMed] [Google Scholar]
- 18.Flynn MA, McNeil DA, Maloff B, et al. Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with best practice recommendations. Obes Rev 2006;7:7-66. [DOI] [PubMed] [Google Scholar]
- 19.Lohman TG, Hingle M, Going SB. Body composition in children. Pediatr Exerc Sci 2013;25:573-90. [DOI] [PubMed] [Google Scholar]
- 20.Tarro L, Llauradó E, Moriña D, et al. Follow-up of a healthy lifestyle education program (the Educació en Alimentació Study): 2 years after cessation of intervention. J Adolesc Health 2014;55:782-9. [DOI] [PubMed] [Google Scholar]
- 21.De Bourdeaudhuij I, Verbestel V, De Henauw S, et al. Behavioural effects of a community-oriented setting-based intervention for prevention of childhood obesity in eight European countries. Obes Rev 2015;16:30-40. [DOI] [PubMed] [Google Scholar]


