Abstract
Background
Recent epidemiological studies have suggested inverse associations between vitamin D status and metabolic diseases including type 2 diabetes (T2DM). The aim of this study was to examine whether a higher serum 25-hydroxyvitamin D (25(OH)D) was associated with a more favorable glucose homeostasis among adults without diabetes in Southwest China.
Methods
Serum 25(OH)D concentration was measured in a cross-sectional sample of 1514 adults without diabetes aged 25–65 years recruited from Southwest China. Indices describing glucose homeostasis included fasting plasma glucose (FPG), fasting insulin, glycated hemoglobin (HbA1c), the homeostatic model assessment 2-insulin resistance (HOMA2-IR) and odds of pre-diabetes. Data were analyzed by multivariable-adjusted regression models.
Results
The average serum 25(OH)D was 22.66 ng/ml, and percentages of vitamin D deficiency [25(OH)D < 20 ng/ml], insufficiency [20 ≤ 25(OH)D ≤ 30 ng/ml] were 47.6 and 32.2%, respectively. Serum 25(OH)D was inversely associated with fasting insulin (P = 0.0007), HbA1c (P = 0.0001) and HOMA2-IR (P = 0.0007), but not with FPG, after adjusting for age, gender, monthly personal income, smoking status, energy intake, moderate-to-vigorous physical activity (MVPA) and waist circumference (WC). Compared with the lowest 25(OH)D tertile, the odds ratio for pre-diabetes in the highest tertile was 0.68 (95%CI: 0.47-0.99) after adjustment for cofounders. In the following stratified analyses according to weight status, we only observed this inverse association between serum 25(OH)D and pre-diabetes in overweight or obese adults (n = 629, P = 0.047), but not in their counterparts with BMI < 24 kg/m2.
Conclusions
Our results advocate that a higher serum 25(OH)D level is associated with decreased risk of impairment of glucose homeostasis among adults without diabetes in Southwest China. Further studies are warranted to determine the role of vitamin D in glucose homeostasis.
Electronic supplementary material
The online version of this article (10.1186/s12902-018-0252-4) contains supplementary material, which is available to authorized users.
Keywords: Vitamin D, Glucose homeostasis, Pre-diabetes, Adult
Background
Over the past decades, the prevalence of type 2 diabetes (T2DM) among Chinese adults has increased from 2.5% in 1994 [1] to 11.6% in 2013 [2]. Additionally, almost half of the adult population had pre-diabetes [2], a major risk factor for the development of T2DM [3].
It is becoming clear that vitamin D status is related to cancer [4], multiple sclerosis [5], cardiovascular disease [6], and diabetes [7–9], besides its role in the modulation of calcium absorption and bone metabolism. Moreover, Vitamin D deficiency has now recognized as a worldwide concern [10]. Zhen et al. [11]. reported that northwest Chinese adults exhibit high prevalence (75.2%) of vitamin D deficiency [25(OH)D < 20 ng/mL].
The associations between vitamin D and factors involved in glucose homeostasis have drawn a great deal of attention recently. 25-hydroxyvitamin D (25(OH)D), the sum of both 25(OH)D2 and 25(OH)D3, is a generally accepted biomarker of vitamin D status. Several observational studies have reported that serum 25(OH)D is negatively associated with fasting plasma glucose (FPG) and insulin among western populations [12–15]. In addition, patients with T2DM had lower serum 25(OH)D compared to control subjects without diabetes [16]. Notably, vitamin D metabolism and its nutritional status were found to differ by ethnicity [8], nonetheless evidence from Asian populations is limited. Available data from China report that 25(OH)D is negatively associated with insulin resistance in patients with T2DM [17], while studies conducted among participants without diabetes are much less [18]. Besides, existing studies mainly focus on the relation of vitamin D with partial indicators (e.g. FPG or insulin) which can not cover the general status of glucose homeostasis.
Therefore, using data from a representative study among Chinese adults without diabetes, we investigated whether a higher serum 25(OH)D was associated with a more favorable glucose homeostasis (a. relative lower level of FPG, fasting insulin, HbA1c and HOMA2-IR within their normal ranges; b. lower odds of pre-diabetes). Furthermore, our results may highlight the importance of improving vitamin D status in the general population.
Methods
Study population
We used data from an ongoing population-based prospective study conducted in Southwest China initiated in September 2013, which aimed to investigate the health impact of nutritional and lifestyle factors on the development of several chronic diseases, as described elsewhere [19]. Using a cluster random sampling design stratified by urban and rural locations, a representative sample of civilian aged 25–65 years was recruited from the general population in Chengdu, Southwest China. The participants were invited to the study center for interviews. Generally, each visit included anthropometric measurements, medical examinations, questionnaires and face-to-face interviews by trained investigators about nutrition-related behaviors, lifestyles and social status. However, the following participants were excluded from the study: a) if they had major organ diseases, including heart, liver or kidney disease; b) if they had mental diseases; c) if they were taking hormone-based drugs and other medicines that affect blood glucose and lipids; or d) if they were pregnant or lactating women. The study was approved by the Ethics Committee of Sichuan University, and all participants provided written informed consent.
For the reason that serum 25(OH)D concentration was not measured in 2013 and 2014, eligible data in the present analysis were identified from the baseline survey conducted from March to October, 2015. Participants in survey 2013-2014 did not differ in gender, age, location and educational status from those who were included in our study.
Laboratory methods
All participants were requested to have an overnight fast of at least 10 h. Peripheral venous blood samples were centrifuged, aliquoted and stored at − 80 °C until measurement. 25(OH)D, calcium2+ and insulin were assayed from serum samples, while plasma samples were used to measure the concentrations of FPG. Finally, HbA1c was quantified from resolved erythrocytes. Serum 25(OH)D was measured using high-performance liquid chromatography (Agilent 1260 HPLC, Shanghai, China) and the intra-assay Coefficient of Variation (CV) was less than 5%. Vitamin D nutritional status was assessed as “deficiency” (< 20 ng/ml), “insufficiency” (20-30 ng/ml) or “sufficiency” (> 30 ng/ml) [20]. Serum calcium2+, which is closely related to serum 25(OH)D, was measured by automatic biochemistry analyzer. Serum insulin was assayed with chemiluminescence enzyme immunoassay within 4 h, and the intra-assay CV was 2.4%. Plasma glucose was measured by hexokinase assay on blood collected into fluoridated EDTA tubes within 2 h with an intra-assay CV of 2.5%. HbA1c was quantified with high-performance liquid chromatography (Bio-Rad D10 automatic analyzer, Shanghai, China) (intra-assay CV: 1.1%) at the clinical laboratory center in Chengdu, which was certified by the National Glycohemoglobin Standardization Program. Finally, the insulin resistance index (HOMA2-IR) was calculated using updated homeostasis model assessment methods (http://www.dtu.ox.ac.uk/homacalculator/) according to the Wallace formula [21].
Anthropometric measurements
Anthropometric measurements were performed by trained medical workers according to the standard procedures [22], with the participants dressed in underwear only, barefoot, and women’s hair uncovered. Waist circumference (WC) was measured without clothes midway between the lower rib margin and iliac crest, to the nearest 0.1 cm, after inhalation and exhalation, using inelasticity tape. Height and weight were measured to the nearest 0.1 kg and 0.1 cm, respectively, with an ultrasonic meter (Weight and Height Instrument DHM-30, China). Weight, height and WC were each averaged based on two measurements. Body mass index (BMI) was calculated as weight (kg) divided by height squared (m2) and was categorized as underweight (BMI < 18.5 kg/m2), normal weight (18.5 kg/m2 ≤ BMI < 24 kg/m2), overweight (24 kg/m2 ≤ BMI < 28 kg/m2), or obese (BMI ≥ 28 kg/m2) using the standard of Working Group on Obesity in China [23].
Definition of pre-diabetes
Pre-diabetes, based on glycaemic parameters above normal but below diabetes thresholds, is a high risk state for diabetes [24]. In our study, it was defined using the updated classification and diagnosis of diabetes of American Diabetes Association [3] as presentation of one or more of the following results: a) HbA1c of 5.7-6.4%; b) Fasting blood glucose of 100-125 mg/dl (5.6-6.9 mmol/L).
Other covariates
Information on socio-demographic characteristics, lifestyle, dietary intake, and other potential confounders were collected by interviewer-administered questionnaires in a face-to-face interview.
For the present analysis, we assessed socio-demographic factors potentially associated with serum 25(OH)D level and glucose homeostasis, which included gender, age (years), education level (≤ 6, 6~ 12, or > 12 years of schooling), occupation (mental worker, physical worker, retired or unemployed) [25] and monthly personal income (≤ 1800 Yuan, 1800~ 3200 Yuan, or > 3200 Yuan) [26]. We also collected data on lifestyle, including smoking status (current smokers, ex-smokers and non-smokers), sleeping and stress, and physical activities. To quantify the intensity of physical activities, the energy cost of moderate-to-vigorous physical activity (MVPA) was measured in metabolic equivalents-hours per week (MET-hours/week) [27].
Dietary data were collected on two random days within a 10-day period by trained investigators using a validated 24-h dietary recall [19]. Participants were asked to recall all foods and beverages they consumed and the corresponding timing. Dietary intake data from 24-h dietary recall were converted into energy using the continuously updated in-house nutrient database based on China Food Composition 2009 [28]. And in this analysis, total energy intake for each participant was calculated as individual means of two-day 24-h dietary recall in kcal/day. Alcohol beverage consumption (cups/d) and coffee consumption (cups/wk) were accessed by food frequency questionnaire.
In addition, season of blood drawn (spring: March to May, summer: June to August; autumn: September to November; winter: December to February) was recorded.
Statistical analysis
All statistical analyses were performed with SAS software (SAS, version 9.3, 2011, SAS Institute Inc., Cary, NC, USA.). A P value < 0.05 was considered statistically significant, except for interaction tests, where P < 0.1 was considered significant. Normality of all continuous variables was examined using normal probability plots and the Kolmogorov-Smirnov test. Given their non-normality, all continuous variables were presented as median (25th percentile, 75th percentile). As the initial analysis indicated no interaction between gender and relations of serum 25(OH)D with FPG, HbA1c, insulin levels, HOMA2-IR (range of P-value: 0.4–0.9), we pooled the sample in the follow-up analyses.
We cross-classified the study sample into categories of tertiles (T1-T3) of serum 25(OH)D to examine the distribution of baseline parameters. We tested differences in proportions using Student t-tests for normally-distributed continuous variables, the Wilcoxon rank-sum for non-normally distributed continuous variables and the Chi-square test for categorical variables, respectively.
To investigate the associations of serum 25(OH)D with glucose homeostasis, multivariable linear generalized regression models (PROC GLM in SAS) were performed. Serum 25(OH)D was defined as the independent variable in separate models. Glucose homeostasis including fasting insulin, FPG, HbA1c and HOMA2-IR were dependent variables in separate models. The independent and dependent variables that enter the linear regression models were non-normally distributed continuous variables. To improve the fitting effect of the models, log-transformed values of insulin, FPG, HbA1c and HOMA2-IR were used in the models.
In the basic models, the correlation analyses between serum 25(OH)D and glucose homeostasis (insulin, FPG, HbA1c, HOMA2-IR) were carried out first. In a further analysis, the following variables potentially affecting these associations were added: gender, age (years), educational level (≤ 6 years, 6~ 12 years, or > 12 years of theoretical education), monthly personal income (≤ 1800 Yuan, 1800~ 3200 Yuan, or > 3200 Yuan), occupation (mental worker, physical worker, retired or unemployed), smoking status (current smokers, ex-smokers and non-smokers), MVPA (MET-hour/week), total energy intake (kcal/d), alcohol beverage consumption (cups/d), coffee consumption (cups/wk), serum calcium2+ (mmol/L), season of blood drawn (spring, summer, autumn and winter) and WC (cm) or BMI (kg/m2). Each variable was initially considered separately, and variables that had their own independent significant effect in the basic models or that substantially modified the association of serum 25(OH)D with each variable of glucose homeostasis were included in the multivariate analyses. Thus, age, gender, monthly personal income, smoking status and season of blood drawn were retained in model A. In a further step, we additionally adjusted for MVPA and energy intake (model B). WC was checked as a potential confounder in model C. The adjusted means were the least-squares means predicted by the model when the other variables were held at their mean values. Then the least-squares means and 95% confidence interval (95%CI) computed by the linear models were back transformed and then presented in the results.
Finally, multivariate logistic regression analyses were used to determine the association of serum 25(OH)D with the odds of pre-diabetes. To enhance comparability, models were constructed in analogy to the multivariable linear regression analyses. To explore interaction of weight status on this association, we divided the participants into two groups according to their weight status (overweight or not) and performed stratified analyses. Estimates are presented as odds ratios (ORs) with 95% CI.
Results
A total of 1710 adults (654 men and 1056 women) had their blood drawn, completing the anthropometric measurements and questionnaires initially in 2015. We excluded individuals who had already been diagnosed with diabetes mellitus (n = 166) and adults who had taken vitamin D supplements, calcitriol or calcium (n = 21). Furthermore, participants who had missing value on anthropometric or biological data, or information on relevant covariates were excluded (n = 9). Therefore, this analysis was based on a final sample of 1514 participants (Fig. 1).
Fig. 1.
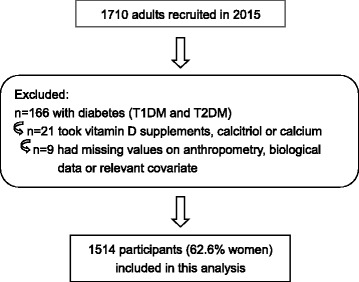
Flowchart for the study sample
General characteristics of the study sample are presented in Table 1. Participants (62.6% women) included in the present analysis had a mean age of 48.74 years. The average serum 25(OH)D concentration was 22.66 ng/ml, and percentages of vitamin D deficiency and insufficiency were 47.6 and 32.2%, respectively. Almost 65.2% of the participants had pre-diabetes (Additional file 1: Table S1), and the prevalence of overweight or obesity was 41.5% in our study sample.
Table 1.
Characteristicsa of study sample by gender (n = 1514)
| Characteristics | Total | Male | Female |
|---|---|---|---|
| n (%) | 1514 (100.0) | 566 (37.4) | 948 (62.6) |
| Age (yrs) | 51.5 (37.9, 60.6) | 46.7 (32.2, 60.4) | 53.2 (42.1, 60.6) |
| Serum 25(OH) D (ng/ml) | 20.7 (15.2, 27.9) | 19.7 (14.6, 25.1) | 21.8 (15.7, 29.9) |
| Pre-diabetesb (n (%)) | 987 (65.2) | 383 (67.7) | 604 (63.7) |
| Blood parameters | |||
| Fasting plasma glucose (mmol/L) | 5.20 (5.51, 5.85) | 5.58 (5.28, 5.89) | 5.46 (5.16, 5.84) |
| Fasting insulin (μIU/mL) | 6.40 (4.13, 10.13) | 6.70 (3.95, 10.00) | 6.30 (4.20, 10.20) |
| HbA1c (%) | 5.50 (5.20, 5.80) | 5.50 (5.20, 5.80) | 5.60 (5.30, 5.80) |
| HOMA2-IRc | 0.87 (0.55, 1.35) | 0.89 (0.52, 1.34) | 0.84 (0.59, 1.37) |
| Serum calcium2+ (mmol/L) | 2.42 (2.33, 2.51) | 2.45 (2.36, 2.55) | 2.40 (2.32, 2.50) |
| Anthropometric parameters | |||
| Overweightd (n (%)) | 629 (41.5) | 288 (50.9) | 341 (35.9) |
| Overweighte (n (%)) | 442 (29.2) | 212 (37.5) | 230 (24.3) |
| Body mass index (kg/m2) | 23.2 (21.0, 25.4) | 24.1 (21.9, 26.1) | 22.7 (20.8, 25.0) |
| Waist circumference (cm) | 84.1 (77.5, 91.0) | 86.4 (80.5, 92.4) | 82.5 (76.0, 89.1) |
| Social-demographic data | |||
| High education levelf (n (%)) | 676 (44.7) | 311 (55.0) | 365 (38.5) |
| High monthly personal incomeg (n (%)) | 576 (38.0) | 319 (56.4) | 257 (27.1) |
| Mental workerh(n (%)) | 510 (33.7) | 204 (36.0) | 306 (32.3) |
| Lifestyles | |||
| Smoking status (current, n (%)) | 217 (14.4) | 192 (33.9) | 25 (2.6) |
| MVPA (MET-hour/week)i | 95.4 (60.6, 144.3) | 78.5 (49.5, 122.1) | 105.8 (69.5, 155.5) |
| Total energy intake (kcal/d) | 1552.2 (1251.3, 1886.9) | 1808.9 (1494.0, 2141.5) | 1409.3 (1167.1, 1705.4) |
| Season of blood drawn (summerj, n (%)) | 372 (24.6) | 142 (25.1) | 230 (24.3) |
aValues are median (25th percentile, 75th percentile) for non-normally-distributed continuous variables and n (%) for categorical variables
bPre-diabetes was defined using the updated classification and diagnosis of diabetes of American Diabetes Association (ADA) [3]
cHOMA2-IR, Homeostasis model assessment 2-insulin resistance, calculated by Wallace Formula [21]
dBody mass index ≥24.0 kg/m2 [23]
eBody mass index ≥25.0 kg/m2 [48]
fAt least 12 years of school education
gMonthly personal income at least ≥3200 CNY (Chinese Yuan), which is moderate level among the general population in Southwest China [26]
hMental worker includes professional and technical personnel (teacher/policeman/doctor etc), legislator & administrator, businessman and student [25]
iMVPA: moderate-to-vigorous physical activity (MET-hour/week) [27]. MET: Metabolic equivalent
jSummer in Southwest China is from June to August generally
Across 25(OH)D tertiles, participants in higher serum 25(OH)D tertiles had significantly lower fasting insulin, HOMA2-IR, serum calcium2+ and monthly personal income, in addition, they were more likely to have their blood drawn in summer and to engage in more physical activities than those in lower tertiles of serum 25(OH)D concentration. The differences in the associations (Vitamin D and glucose homeostasis) between the three proposed groups were not statistically significant in regard to FPG or HbA1c and several other variables. (Table 2).
Table 2.
Characteristics of study sample by tertiles of serum 25(OH)D (n = 1514)a
| Tertiles of serum 25(OH)D (ng/ml) | P | |||
|---|---|---|---|---|
| Tertile 1 12.6 (9.5, 15.1)b |
Tertile 2 20.6 (18.6, 23.1)b |
Tertile 3 31.9 (27.9, 38.9)b |
||
| n (%) | 504 (33.3) | 505 (33.4) | 505 (33.4) | – |
| Age (yrs) | 58.9 (47.0, 64.9) | 47.8 (34.9, 57.9) | 57.7 (49.5, 62.2) | < 0.0001 |
| Male (n (%)) | 203 (40.3) | 222 (44.0) | 141 (27.9) | 0.0001 |
| Pre-diabetesc (n (%)) | 323 (64.1) | 334 (66.1) | 330 (65.4) | 0.847 |
| Blood parameters | ||||
| Fasting plasma glucose (mmol/L) | 5.51 (5.22, 5.82) | 5.51 (5.17,5.84) | 5.49 (5.20, 5.90) | 0.929 |
| Fasting insulin (μIU/mL) | 7.00 (4.40, 10.86) | 6.50 (4.20, 10.40) | 5.80 (3.90, 9.35) | 0.014 |
| HbA1c (%) | 5.50 (5.20, 5.80) | 5.50 (5.20, 5.80) | 5.60 (5.30, 5.80) | 0.483 |
| HOMA2-IRd | 0.95 (0.59, 1.45) | 0.87 (0.56, 1.39) | 0.78 (0.52, 1.26) | 0.018 |
| Serum calcium2+ (mmol/L) | 2.44 (2.36, 2.52) | 2.43 (2.33, 2.51) | 2.40 (2.30, 2.50) | 0.006 |
| Anthropometric parameters | ||||
| Overweighte (n (%)) | 208 (41.2) | 202 (40.1) | 219 (43.3) | 0.707 |
| Overweightf (n (%)) | 146 (29.0) | 138 (27.4) | 158 (31.3) | 0.566 |
| Body mass index (kg/m2) | 22.9 (20.9, 25.3) | 23.3 (21.1, 25.2) | 23.4 (21.1, 25.6) | 0.372 |
| Waist circumference (cm) | 83.5 (77.4, 89.8) | 84.1 (77.3, 90.0) | 84.7 (78.1, 92.2) | 0.119 |
| Social-demographic data | ||||
| High education levelg (n (%)) | 237 (47.0) | 243 (48.1) | 196 (38.8) | 0.042 |
| High monthly personal incomeh (n (%)) | 201 (39.9) | 197 (39.0) | 178 (35.3) | 0.0005 |
| Mental workeri (n (%)) | 188 (37.3) | 196 (38.8) | 126 (25.0) | < 0.0001 |
| Lifestyles | ||||
| Smoking status (current, n (%)) | 72 (14.3) | 79 (15.6) | 66 (13.1) | 0.539 |
| MVPA (MET-hour/week)j | 90.0 (54.6, 139.4) | 89.24 (58.3, 137.4) | 105.90 (66.6, 153.5) | 0.019 |
| Total energy intake (kcal/d) | 1563.3 (1250.7, 1884.8) | 1575.7 (1261.0, 1963.3) | 1530.0 (1232.6, 1839.8) | 0.361 |
| Seasonk (summer, n (%)) | 84 (16.7) | 138 (27.3) | 150 (29.7) | < 0.0001 |
aValues are median (25th percentile, 75th percentile) for non-normally-distributed continuous variables and n (%) for categorical variables. For non-normally distributed data, Kruskal-Wallis test was used to test the differences of the parameters among the tertiles of 25(OH)D, and for categorical variables, chi-square test were used
bValues are median (25th percentile, 75th percentile) in tertiles of vitamin D (ng/ml)
cPre-diabetes was defined using the updated classification and diagnosis of diabetes of American Diabetes Association (ADA) [3]
dHOMA2-IR, Homeostasis model assessment 2-insulin resistance, calculated by Wallace Formula [21]
eBody mass index ≥24.0 kg/m2 [23]
fBody mass index ≥25.0 kg/m2 [48]
gAt least 12 years of school education
hMonthly personal income at least ≥3200 CNY (Chinese Yuan), which is moderate level among the general population in Southwest China [26]
iMental worker includes professional and technical personnel (teacher/policeman/doctor etc), legislator & administrator, businessman and student [25]
jMVPA: moderate-to-vigorous physical activity (MET-hour/week) [27]. MET: Metabolic equivalent
kSummer in Southwest China is from June to August generally
The associations of tertiles of Vitamin D with glucose homeostasis are shown in Table 3. Multiple linear regression analysis showed that serum 25(OH)D concentration was inversely related to fasting insulin (P = 0.016), HbA1c (P = 0.0003) and HOMA2-IR (P = 0.016) in these non-diabetic participants after adjustment for age, gender, monthly personal income, smoking status and season of blood drawn (model A), while association between vitamin D and FPG was not statistically significant (P > 0.05, after adjusting for confounders mentioned above). Further adjusting for MVPA, energy intake (model B), or including additional adjustment for WC (model C) did not materially change these inverse associations. Adults in the highest serum 25(OH)D concentration tertile had 12.4% lower fasting insulin (P = 0.0007), 2.2% lower HbA1c (P = 0.0001) and 12.3% lower HOMA2-IR (P = 0.0007) than those in the lowest tertile.
Table 3.
Multiple linear regression least-squares means and 95% confidence interval for the association of tertiles of serum 25(OH)D (ng/ml) with glucose homeostasis (n = 1514)a
| Tertiles of serum 25(OH)D (ng/ml) | P for trend | |||
|---|---|---|---|---|
| Tertile 1 12.6 (9.5, 15.1)b |
Tertile 2 20.6 (18.6, 23.1)b |
Tertile 3 31.9 (27.9, 38.9)b |
||
| Fasting insulin (μIU/mL) | ||||
| Model Ac | 8.36 (7.59, 9.12) | 8.00 (7.25, 8.75) | 7.47 (6.68, 8.26) | 0.016 |
| Model Bd | 8.35 (7.58, 9.12) | 7.98 (7.23, 8.73) | 7.45 (6.66, 8.24) | 0.015 |
| Model Ce | 8.00 (7.31, 8.70) | 7.63 (6.95, 8.31) | 7.01 (6.29, 7.73) | 0.0007 |
| Fasting plasma glucose(mmol/L) | ||||
| Model Ac | 5.56 (5.48, 5.64) | 5.55 (5.47, 5.63) | 5.52 (5.44, 5.61) | 0.331 |
| Model Bd | 5.56 (5.48, 5.64) | 5.55 (5.47, 5.63) | 5.52 (5.43, 5.60) | 0.291 |
| Model Ce | 5.55 (5.47, 6.63) | 5.53 (5.46, 5.61) | 5.50 (5.42, 5.58) | 0.197 |
| HbA1c (%) | ||||
| Model Ac | 5.57 (5.51, 5.63) | 5.53 (5.46, 5.59) | 5.46 (5.40, 5.52) | 0.0003 |
| Model Bd | 5.57 (5.51, 5.63) | 5.52 (5.46, 5.82) | 5.45 (5.39, 5.52) | 0.0002 |
| Model Ce | 5.57 (5.50, 5.63) | 5.52 (5.46, 5.58) | 5.45 (5.39, 5.51) | 0.0001 |
| HOMA2-IR | ||||
| Model Ac | 1.11 (1.01, 1.21) | 1.06 (0.97, 1.16) | 0.99 (0.89, 1.10) | 0.016 |
| Model Bd | 1.11 (1.01, 1.21) | 1.06 (0.96, 1.16) | 0.99 (0.89, 1.10) | 0.015 |
| Model Ce | 1.06 (0.97, 1.16) | 1.02 (0.93, 1.10) | 0.93 (0.84, 1.03) | 0.0007 |
aValues are models least-squares means and 95% confidence interval. Linear trends (P for trend) were obtained with vitamin D concentrations as continuous variables;
bValues are median (25th percentile, 75th percentile) in tertiles of Vitamin D (ng/ml);
cModel A: adjusted for age, gender, monthly personal income, smoking status and season of blood drawn;
dModel B: additionally adjusted for MVPA and energy intake;
eModel C: additionally adjusted for waist circumference
Table 4 outlines the association of tertiles of Vitamin D with the odds of pre-diabetes. A significantly 32% lower odds of pre-diabetes was observed for adults in the highest tertile of serum 25(OH)D (OR: 0.68, 95%CI: 0.47-0.99) compared with those in the lowest tertile after adjustment for potential confounders. We further discovered an interaction of weight status on this association (P = 0.06). In stratified analyses, overweight individuals in the highest tertile of serum 25(OH)D had lowest risk of pre-diabetes (P = 0.047), but not in individuals with BMI < 24 kg/m2. To compare these results with western adults, we conducted a sensitivity analysis using the criteria of World Health Organization to define overweight and observed similar result patterns (Additional file 2: Table S2).
Table 4.
Multiple logistic regression odds ratio (OR) and 95% confidence interval (CI) for the association of tertiles of serum 25(OH)D (ng/ml) with pre-diabetesa
| OR (95%CI) | P for trend | |||
|---|---|---|---|---|
| Pre-diabetesc (yes or no) | Tertile 1 12.6 (9.5, 15.1)b |
Tertile 2 20.6 (18.6, 23.1)b |
Tertile 3 31.9 (27.9, 38.9)b |
|
| Total (n = 1514) | ||||
| Model Ad | 1.00 | 1.07 (0.75, 1.52) | 0.70 (0.48, 1.01) | 0.056 |
| Model Be | 1.00 | 1.07 (0.74, 1.52) | 0.69 (0.47, 0.99) | 0.049 |
| Model Cf | 1.00 | 1.06 (0.74, 1.52) | 0.68 (0.47, 0.99) | 0.046 |
| BMI < 24 kg/m2 (n = 885) | ||||
| Model Ad | 1.00 | 1.32 (0.84, 2.08) | 0.86 (0.53, 1.38) | 0.182 |
| Model Be | 1.00 | 1.36 (0.87, 2.14) | 0.86 (0.53, 1.39) | 0.153 |
| BMI ≥ 24 kg/m2 (n = 629) | ||||
| Model Ad | 1.00 | 0.68 (0.36, 1.27) | 0.45 (0.24, 0.85) | 0.052 |
| Model Be | 1.00 | 0.65 (0.34, 1.22) | 0.45 (0.23, 0.84) | 0.047 |
aValues are odds ratio and 95% confidence interval. Linear trends (P for trend) were obtained with vitamin D concentrations as continuous variables;
bValues are median (25th percentile, 75th percentile) of in tertiles of Vitamin D (ng/ml);
cUsing the Classification and Diagnosis of diabetes of American Diabetes Association to classify pre-diabetes [3];
dModel A: adjusted for age, gender, average personal income per month, smoking status and season of blood drawn;
eModel B: additionally adjusted for MVPA and energy intake;
fModel C: additionally adjusted for waist circumference
Discussion
This study suggests that a higher vitamin D level was associated with a more favorable glucose homeostasis among non-diabetic adults in Southwest China. Moreover, a poor vitamin D status was significantly related with an increased risk of pre-diabetes especially in overweight or obese adults.
As indicated in previous studies [8, 12, 13], our findings suggested inverse associations of serum 25(OH)D with fasting insulin and insulin resistance. Of note, superior than the traditional assessment of HOMA1-IR, our study used HOMA2-IR to assess insulin resistance [29, 30]. The underlying mechanisms that may explain these associations have not been well understood, many possibilities being raised: a) vitamin D appears to exert effects on pancreatic β-cells secretory function and insulin sensitivity through direct modulation of gene expression via vitamin D receptors (VDRs) or regulation of calcium influx [31, 32]; b) VDR gene polymorphisms have been recently suggested to associate with variation in insulin secretion [33, 34]; and c) insufficient vitamin D usually results in increased serum parathyroid hormone which in turn has been found to be related to impaired glucose tolerance and decreased insulin sensitivity in healthy adults [35].
Serum 25(OH)D in the present study was shown to be negatively associated with HbA1c, the longer-term marker of glycemic status, which was in line with a cross-sectional population-based survey from National Health and Nutrition Examination Survey (NHANES) 2003-2006 [36]. Liu et al. [12] reported an inverse association between serum 25(OH)D and FPG as well, whereas we did not observe that. One reason for the divergence might be that FPG is a short-term indicator of glycemic status susceptible to participants’ diet and emotion at specific times. Moreover, evidence has suggested the decrease in HbA1c with increasing 25(OH)D was the steepest in levels < 65 nmol/L (26 ng/ml), with some small decreases with further increases [37]. In this scenario, the relative poorer vitamin D status of our study sample may lead to a more overt relation of serum 25(OH)D with HbA1c rather than with FPG.
In this study, low vitamin D status was associated with increased risk of pre-diabetes. Consistent relationships have been found among non-diabetic U.S. adults, using data from NHANES III [38, 39], as well as Kuwait adults [40]. In addition, above results suggest that vitamin D deficiency has important effects on insulin resistance and impaired β-cell function, which are the two critical factors that drive the development of T2DM. Remarkably, in the following stratified analyses, we only observed the association between serum 25(OH)D and pre-diabetes among overweight or obese adults. Hypponen et al. [37] reported that obesity played an important role in the relation between serum 25(OH)D and glucose homeostasis. To some extent, our results were in agreement with the previous findings that overweight or obese adults had poorer vitamin D status [41, 42]. Nevertheless, another cross-sectional study among elder Brazilians indicated there was no association between 25(OH)D levels and pre-diabetes [43] due partly to their small sample size. Considering the higher prevalence of pre-diabetes among Chinese, a stage in the disease continuum where diabetes prevention has been shown to be effective [44, 45], identification and treatment of pre-diabetic individuals are therefore crucial.
In the meanwhile, our data indicated that vitamin D deficiency was fairly common in our study sample with an average age of 48.74 years (the prevalence of vitamin D deficiency or insufficiency was 79.8%), which was lower than another study focused on Chinese adults aged 50-70 years (93.6%, 2009) [46] perhaps owing to the fact that aging is associated with reduced capacity to produce vitamin D [20]. Notably, prevalence in this study was substantially higher than those observed among US population in 2009-2010 (64%) [47], which may lie in that fewer vitamin D fortified foods are available in China. Our results suggest that vitamin D deficiency might be universal in the general population in China and relevant measures might be taken to improve vitamin D status of Chinese adults.
Several limitations of our study merit consideration. Owing to the cross-sectional nature of the study design, a cause-effect relationship between serum 25(OH)D and glucose homeostasis cannot be inferred. The present study was completed within a relatively long period, from March to October, 2015, which may increase the seasonal variation in the biomarkers. However, data from the Ely Study (Cambridgeshire, U.K.) [13] and NHANES 2001-2006 [14] suggested that the associations between 25(OH)D and glucose homeostasis were independent of season. Finally, our analysis has excluded diabetic participants, many of whom were men due to the higher prevalence of diabetes in men than women among Chinese populations, generating an imbalanced sex proportion which could have potentially biased our results. Nonetheless, initial analysis indicated no interaction between gender and serum 25(OH)D, and we have adjusted gender in the multiple regression analyses. Furthermore, participants in the present analysis have been shown to be comparable to age-matched adults in the general population in Southwest China on sociodemographic and lifestyle characteristics [26].
Notwithstanding the limitations mentioned above, the present study had following strengths. Serum 25(OH)D allowed for objective measurement of vitamin D status rather than relying on self-reported vitamin D intake or sunlight exposure, which circumvented the recall bias. In addition, our analyses took into account many potential covariates that might confound the observed associations. Finally, we investigated participants aged 25-65 years with a range of quantitative indicators of glucose homeostasis (including FPG, fasting insulin, HbA1c and HOMA2-IR), providing more comprehensive results than the previous studies.
Conclusions
In conclusion, we have demonstrated inverse associations of serum 25(OH)D concentration with glucose homeostasis in Southwest Chinese adults without diabetes. Prospective studies and clinical trials are needed to confirm our findings.
Additional files
Table S1. The diagnosis of pre-diabetes (n = 1514). (DOCX 16 kb)
Table S2. Multiple logistic regression odds ratio (OR) and 95% confidence interval (CI) for the association of tertiles of serum 25(OH)D (ng/ml) with pre-diabetes1 (DOCX 18 kb)
Acknowledgements
All the participants in our study are gratefully acknowledged. We also thank the staff of the Department of Nutrition, Food Safety, and Toxicology for organizing this study and all the laboratorians involved in our study for providing technical support.
Funding
This study was supported by research grant from the National Nature Science Foundation of China (No.81472976). The funding agencies had no role in the design of study, data collection and analysis, or presentation of the results.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- 25(OH)D
25-hydroxyvitamin D
- BMI
Body mass index
- CV
Coefficient of Variation
- FPG
Fasting plasma glucose
- HbA1c
Glycated hemoglobin
- HOMA2-IR
The homeostatic model assessment 2-insulin resistance
- MVPA
Moderate-to-vigorous physical activity
- NHANES
National Health and Nutrition Examination Survey
- OGTT
Oral glucose tolerance test
- T2DM
Type 2 diabetes mellitus
- VDRs
Vitamin D receptors
- WC
Waist circumference
Authors’ contributions
GC conceived the project and designed the study. DL conducted the analysis and wrote the manuscript. HW revised the manuscript critically for laboratory technique content. HX provided critical input on the calculation of physical activity. JZ and MC researched data. YG provided critical input on earlier versions of the manuscript. All authors had final approval of the final manuscript as submitted.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Sichuan University, and all participants provided written informed consent.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12902-018-0252-4) contains supplementary material, which is available to authorized users.
Contributor Information
Danting Li, Email: ldtsea@126.com.
Haoche Wei, Email: maria2588@sina.cn.
Hongmei Xue, Email: xhmei_1109@163.com.
Jieyi Zhang, Email: hx_zhangjieyi@qq.com.
Mengxue Chen, Email: iman1207@qq.com.
Yunhui Gong, Email: yunhuigong@126.com.
Guo Cheng, Phone: +86-28-85502220, Email: ehw_cheng@126.com.
References
- 1.Pan X-R, Liu J, Yang W-Y, Li G-W. Prevalence of diabetes and its risk factors in China, 1994. Diabetes Care. 1997;20(11):1664–1669. doi: 10.2337/diacare.20.11.1664. [DOI] [PubMed] [Google Scholar]
- 2.Xu Y, Wang L, He J, Bi Y, Li M, Wang T, et al. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310(9):948–959. doi: 10.1001/jama.2013.168118. [DOI] [PubMed] [Google Scholar]
- 3.American Diabetes A Classification and diagnosis of diabetes. Diabetes Care. 2016;39(Suppl 1):S13–S22. doi: 10.2337/dc16-er09. [DOI] [PubMed] [Google Scholar]
- 4.van der Rhee H, Coebergh JW, de Vries E. Sunlight, vitamin D and the prevention of cancer: a systematic review of epidemiological studies. Eur J Cancer Prev. 2009;18(6):458–475. doi: 10.1097/CEJ.0b013e32832f9bb1. [DOI] [PubMed] [Google Scholar]
- 5.Munger KL, Levin LI, Hollis BW, Howard NS, Ascherio A. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA. 2006;296(23):2832–2838. doi: 10.1001/jama.296.23.2832. [DOI] [PubMed] [Google Scholar]
- 6.Wang TJ, Pencina MJ, Booth SL, Jacques PF, Ingelsson E, Lanier K, et al. Vitamin D deficiency and risk of cardiovascular disease. Circulation. 2008;117(4):503–511. doi: 10.1161/CIRCULATIONAHA.107.706127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Daghri NM, Al-Attas OS, Alokail MS, Alkharfy KM, Yakout SM, Aljohani NJ, et al. Lower vitamin D status is more common among Saudi adults with diabetes mellitus type 1 than in non-diabetics. BMC Public Health. 2014;14(1):1–5. doi: 10.1186/1471-2458-14-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scragg R, Sowers M, Bell C. Serum 25-hydroxyvitamin D, diabetes, and ethnicity in the third national health and nutrition examination survey. Diabetes Care. 2004;27(12):134–139. doi: 10.2337/diacare.27.12.2813. [DOI] [PubMed] [Google Scholar]
- 9.Pittas AG, Sun Q, Manson JE, Dawson-Hughes B, Hu FB. Plasma 25-hydroxyvitamin D concentration and risk of incident type 2 diabetes in women. Diabetes Care. 2010;33(9):2021–2023. doi: 10.2337/dc10-0790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–281. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 11.Zhen D, Liu L, Guan C, Zhao N, Tang X. High prevalence of vitamin D deficiency among middle-aged and elderly individuals in northwestern China: its relationship to osteoporosis and lifestyle factors. Bone. 2015;71:1–6. doi: 10.1016/j.bone.2014.09.024. [DOI] [PubMed] [Google Scholar]
- 12.Liu E, Meigs JB, Pittas AG, McKeown NM, Economos CD, Booth SL, et al. Plasma 25-hydroxyvitamin d is associated with markers of the insulin resistant phenotype in nondiabetic adults. J Nutr. 2009;139(2):329–334. doi: 10.3945/jn.108.093831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Forouhi NG, Luan J, Cooper A, Boucher BJ, Wareham NJ. Baseline serum 25-hydroxy vitamin d is predictive of future glycemic status and insulin resistance: the Medical Research Council Ely prospective study 1990-2000. Diabetes. 2008;57(10):2619–2625. doi: 10.2337/db08-0593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ford ES, Zhao G, Tsai J, Li C. Associations between concentrations of vitamin D and concentrations of insulin, glucose, and HbA1c among adolescents in the United States. Diabetes Care. 2011;34(3):646–648. doi: 10.2337/dc10-1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chiu KC, Chu A, Go VLW, Saad MF. Hypovitaminosis D is associated with insulin resistance and dysfunction. Amer J Clin Nutr. 2004;79(5):820–825. doi: 10.1093/ajcn/79.5.820. [DOI] [PubMed] [Google Scholar]
- 16.Scragg R, Holdaway I, Singh V, et al. Serum 25-hydroxyvitamin D3 levels decreased in impaired glucose tolerance and diabetes mellitus [J] Diabetes Res Clin Pract. 1995;27(3):181–188. doi: 10.1016/0168-8227(95)01040-K. [DOI] [PubMed] [Google Scholar]
- 17.Zhang J, Ye J, Guo G, et al. Vitamin D status is negatively correlated with insulin resistance in Chinese type 2 diabetes:[J] Int J Endocrinol. 2016;2016(5):1–7. doi: 10.1155/2016/1794894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lin D, Wang C, Ma H, et al. The study of serum vitamin D and insulin resistance in Chinese populations with normal glucose tolerance [J] Int J Endocrinol. 2014;2014(2014):870235. doi: 10.1155/2014/870235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guo C, Xue H, Jiao L, et al. Relevance of the dietary glycemic index, glycemic load and genetic predisposition for the glucose homeostasis of Chinese adults without diabetes [J] Sci Rep. 2017;7(1):400. doi: 10.1038/s41598-017-00453-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holick MF. Vitamin D status: measurement, interpretation, and clinical application. Ann Epidemiol. 2009;19(2):73–78. doi: 10.1016/j.annepidem.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wallace TM, Levy JC, Matthew DR. Use and abuse of HOMA modeling. Diabetes Care. 2004;27(6):1487–1495. doi: 10.2337/diacare.27.6.1487. [DOI] [PubMed] [Google Scholar]
- 22.Group CSCaHR . Reports on the physical fitness and health research of chinese school students. Beijing: Higher Education Press; 2010. [Google Scholar]
- 23.Working Group on Obesity in China Guidelines for prevention and control of overweight and obesity in Chinese adults. Acta Nutrimenta Sinica. 2004;26(1):1–4. [Google Scholar]
- 24.Tabák AG, Herder C, Rathmann W, Brunner EJ, Kivimäki M. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379(9833):2279–2290. doi: 10.1016/S0140-6736(12)60283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Elias P, Birch M. SOC2010: revision of the standard occupational classification. Labour Gaz. 2010;4(7):48–55. [Google Scholar]
- 26.Statistical Bureau of Sichuan, NBS Survey Officie in Sichuan . SiChuan statistical yearbook. Beijing: China Statistic Press; 2015. [Google Scholar]
- 27.Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR, Jr, Tudor-Locke C, et al. 2011 Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 28.Yuexin Y, Guangya W, Xingchang P. China food conposition: Peking University Medical Press. 2009. [Google Scholar]
- 29.Hermans MP, Levy JC, Morris RJ, Turner RC. Comparison of tests of β-cell function across a range of glucose tolerance from normal to diabetes. Diabetes. 1999;48:1779–1786. doi: 10.2337/diabetes.48.9.1779. [DOI] [PubMed] [Google Scholar]
- 30.Hermans MP, Levy JC, Morris RJ, Turner RC. Comparison of insulin sensitivity tests across a range, of glucose tolerance from normal to diabetes. Diabetologia. 1999;42(6):678–687. doi: 10.1007/s001250051215. [DOI] [PubMed] [Google Scholar]
- 31.Tai K, Need AG, Horowitz M, Chapman IM. Vitamin D, glucose, insulin, and insulin sensitivity. Nutrition. 2008;24(3):279–285. doi: 10.1016/j.nut.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 32.Pittas AG, Lau J, Hu FB, Dawson-Hughes B. The role of vitamin D and calcium in type 2 diabetes. A systematic review and meta-analysis. J Clin Endocrinol Metab. 2007;92(6):2017–2029. doi: 10.1210/jc.2007-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reis JP, von Muhlen D, Miller ER., 3rd Relation of 25-hydroxyvitamin D and parathyroid hormone levels with metabolic syndrome among US adults. Eur J Endocrinol. 2008;159(1):41–48. doi: 10.1530/EJE-08-0072. [DOI] [PubMed] [Google Scholar]
- 34.Hypponen E, Boucher BJ, Berry DJ, Power C. 25-hydroxyvitamin D, IGF-1, and metabolic syndrome at 45 years of age: a cross-sectional study in the 1958 British birth cohort. Diabetes. 2008;57(2):298–305. doi: 10.2337/db07-1122. [DOI] [PubMed] [Google Scholar]
- 35.Lee DM, Rutter MK, O'Neill TW, Boonen S, Vanderschueren D, Bouillon R, et al. Vitamin D, parathyroid hormone and the metabolic syndrome in middle-aged and older European men. Eur J Endocrinol. 2009;161(6):947–954. doi: 10.1530/EJE-09-0496. [DOI] [PubMed] [Google Scholar]
- 36.Kositsawat J, Freeman VL, Gerber BS, Geraci S. Association of A1C levels with vitamin D status in U.S. adults: data from the national health and nutrition examination survey. Diabetes Care. 2010;33(6):1236–1238. doi: 10.2337/dc09-2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hypponen E, Power C. Vitamin D status and glucose homeostasis in the 1958 British birth cohort: the role of obesity. Diabetes Care. 2006;29(10):2244–2246. doi: 10.2337/dc06-0946. [DOI] [PubMed] [Google Scholar]
- 38.Shankar A, Sabanayagam C, Kalidindi S. Serum 25-Hydroxyvitamin D levels and prediabetes among subjects free of diabetes. Diabetes Care. 2011;34(5):1114–1119. doi: 10.2337/dc10-1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gupta AK, Brashear MM, Johnson WD. Prediabetes and prehypertension in healthy adults are associated with low vitamin D levels. Diabetes Care. 2011;34(3):658–660. doi: 10.2337/dc10-1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang FF, Hooti SA, Rao A, Jahmah NA, Saltzman E, Ausman LM. Low level of serum vitamin D is associated with elevated fasting glucose and prediabetes in Kuwait adults. FASEB J. 2013;27(1):lb376. doi: 10.1096/fj.12-215491. [DOI] [Google Scholar]
- 41.Gonzalez L, Ramos-Trautmann G, Diaz-Luquis GM, Perez CM, Palacios C. Vitamin D status is inversely associated with obesity in a clinic-based sample in Puerto Rico. Nutr Res. 2015;35(4):287–293. doi: 10.1016/j.nutres.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang Y, Zhang X, Wang F, Zhang W, Wang C, Yu C, et al. The relationship between obesity indices and serum vitamin D levels in Chinese adults from urban settings. Asia Pac J Clin Nutr. 2016;25(2):333–339. doi: 10.6133/apjcn.2016.25.2.15. [DOI] [PubMed] [Google Scholar]
- 43.Giorelli GV, Matos LN, Saado A, Soibelman VL, Dias CB. No association between 25-hydroxyvitamin D levels and prediabetes in Brazilian patients. A cross-sectional study. Sao Paulo Med J. 2015;133(2):73–77. doi: 10.1590/1516-3180.2013.7180005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Knowler WC, Bar-rett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.American Diabetes A Standards of medical care in diabetes--2010. Diabetes Care. 2010;33(Suppl 1):S11–S61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lu L, Yu Z, Pan A, Hu FB, Franco OH, Li H, et al. Plasma 25-hydroxyvitamin D concentration and metabolic syndrome among middle-aged and elderly Chinese individuals. Diabetes Care. 2009;32(7):1278–1283. doi: 10.2337/dc09-0209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schleicher RL, Sternberg MR, Lacher DA, Sempos CT, Looker AC, Durazo-Arvizu RA, et al. The vitamin D status of the US population from 1988 to 2010 using standardized serum concentrations of 25-hydroxyvitamin D shows recent modest increases. Amer J Clin Nutr. 2016;104(2):454–461. doi: 10.3945/ajcn.115.127985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pi-Sunyer F, Becker D, Bouchard C, Carleton R, Colditz G. Executive summary of the clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. Arch Intern Med. 1998;158(17):1855–1867. doi: 10.1001/archinte.158.17.1855. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. The diagnosis of pre-diabetes (n = 1514). (DOCX 16 kb)
Table S2. Multiple logistic regression odds ratio (OR) and 95% confidence interval (CI) for the association of tertiles of serum 25(OH)D (ng/ml) with pre-diabetes1 (DOCX 18 kb)
Data Availability Statement
All data generated or analyzed during this study are included in this published article.


