Abstract
This is a review of the recent literature of the various factors that affect patellar tracking following total knee arthroplasty (TKA).
Patellar tracking principally depends on the pre-existing patellar tracking and the rotational alignment of the femoral and tibial implants, but the detailed movements depend on the patellar shape. The latter means that the patellar kinematics of any implanted TKA does not return to normal.
Laboratory cadaveric studies use normal knees and non-activity-based testing conditions and so may not translate into clinical findings.
The recent literature has not added anything significant to change established clinical practice in achieving satisfactory patellar tracking following TKA.
Cite this article: EFORT Open Rev 2018;3:106-113. DOI: 10.1302/2058-5241.3.170036.
Keywords: femoral rotation, implant alignment, patellar kinematics, review, total knee arthroplasty
Introduction
Historically, problems with the patella have accounted for half of the poor outcomes from total knee arthroplasty (TKA).1 This was in the early days when there was no trochlear extension to the femoral component and before ‘patellar-friendly’ implant designs. Nowadays the debate persists about whether the patella should or should not be replaced. Revision of primary TKA for patellofemoral pain accounts for 0.5% of all revisions.2 There are also risks of extensor mechanism rupture. However, the major error to avoid is post-operative patellar maltracking. The debate still rages about how to avoid post-operative anterior knee pain. This review will mainly concentrate on avoiding maltracking. It begs the question whether maltracking per se leads to anterior knee pain. Since the patella has six degrees of freedom then, in theory, it can maltrack in any one of them. The term ‘maltracking’ is inexact. For the purposes of this review it is defined as the centre of the patella displacing to a non-physiological position during knee movement. It should be understood that, in the normal knee during sports activities, the position of the patella within the trochlea depends on the degree of knee flexion, the position of the foot if on the ground, and the relative pull of the different components of the quadriceps muscle. The path of the patella from full extension to full flexion is therefore not fixed. Passive movements of the knee do not show the full medial and lateral displacement of the patella within the groove that occurs during flexion and rotation of the tibia with respect to the femur in activity and subjected to muscle forces. In practice the principal reason for patellar maltracking following TKA is malrotation of the femoral and/or tibial components. Table 1 summarizes the factors that affect patellar tracking in TKA.
Table 1.
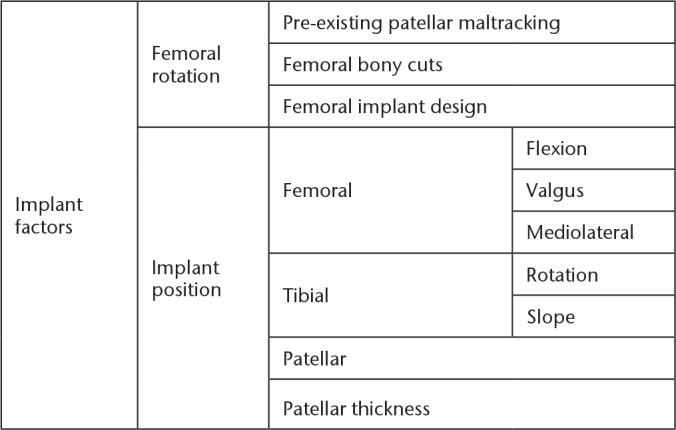
Factors that may affect patellar tracking in total knee arthroplasty
Information that has been gained from cadaveric studies is undertaken on normal, i.e. non-arthritic, knees, and therefore only gives an indication of the biomechanical behaviour of the knee in very controlled conditions. It is the reason that laboratory findings may not match clinical outcomes.3 This review looks at the recent publications on this subject to indicate current thoughts.
Factors that affect patellar tracking
Patellofemoral tracking in the normal knee centralizes the different quadriceps muscle bellies when the patella moves along the groove.3 This improves the efficiency of the extension forces. Data on patellar biomechanics have been collected by describing the tracking, the muscle forces and the retropatellar contact pressure, as well as the shear forces. The rotation of the limb at both the femur and tibia is also understood to play an important role. In theory, if the patella is tracking laterally, either the groove can be placed under the patella by a rotational osteotomy in the native knee and external rotation of the femoral implant in the TKA, or the soft tissue envelope around the patella can be rotated to bring the patella over the groove by proximal and/or distal realignment procedures. In TKA the objective of obtaining correct patellar tracking is to optimize the position of the patella for extensor efficiency whilst maintaining a stable tibiofemoral joint. This has been well described in a previous instructional lecture.4
Implant factors
Femoral rotation: pre-existing patellar maltracking
The mainstream view is that any pre-existing maltracking of the patella should be corrected either before or during a TKA.5 However, Oh et al6 performed a TKA but without relocating the patella in a patient with an inherited dysplasia. This may be a reasonable choice in low-demand patients but is probably inappropriate with a patient with more physical demands. The surgical management of the chronic dislocation requires a full workup including the relevant radiology. The main point is to check on the femoral anteversion and tibial torsion to decide whether a rotational osteotomy of either bone is needed, or whether any rotational abnormality can be corrected by rotating the implants. If a tibial tubercle medialization is considered necessary, it can be included in the surgical approach. Chronic patellar dislocation is always associated with a tight lateral retinaculum so there should be a low threshold to performing a lateral release, noting that a quadricepsplasty may also be needed.7
Femoral rotation: femoral bony cuts
External rotation
The most important factor for post-operative patellar tracking is the rotation of the femur based on the posterior condylar cuts (Fig. 1); the more externally rotated the implant, the less risk there is for lateral patellar maltracking. However, this must not be at the expense of tibiofemoral alignment and stability.4
Fig. 1.
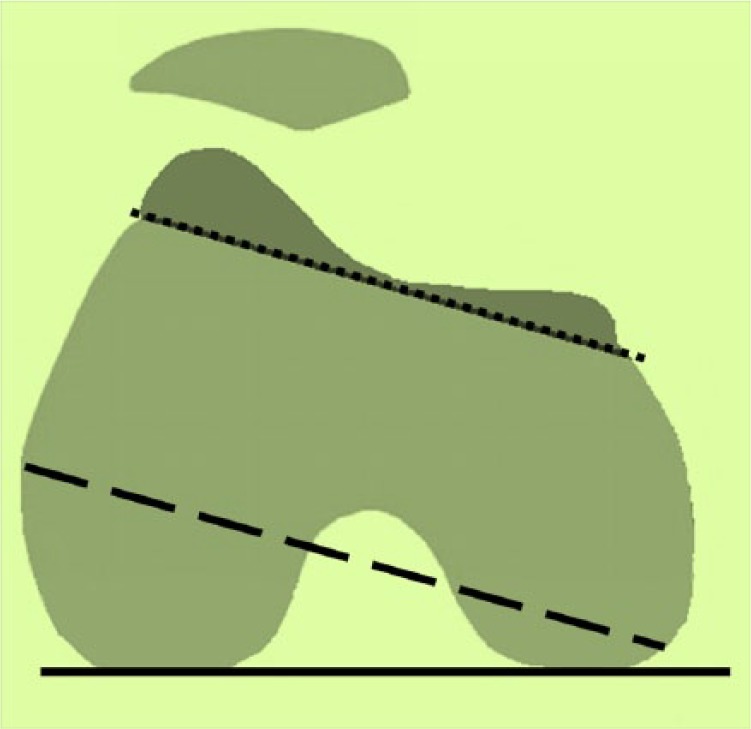
Diagram showing the posterior condylar axis (continuous line) and an asymmetric cut (dashed line), which results in an internally rotated anterior femoral cut and lateral patellar displacement.
Cadaveric studies
A number of cadaveric studies have been undertaken recently to assess patellar tracking and the effects of femoral component rotation.8,9 Colwell Jr et al8 have developed a computer model, initially validated with cadaveric knees,9 to look at the effect of a rotating platform to see if this would reduce the effects of femoral component malrotation. The cadaveric study used the Scorpio CR (Stryker Orthopaedics, Mahwah, NJ, USA) TKA. The femoral component was malrotated at ± 3°. They had found that with a fixed-bearing implant, internal rotation of the femoral component caused a corresponding (and unsurprising) tibiofemoral internal rotation, whereas external rotation resulted in the opposite direction. External rotation of the femoral component also resulted in a 2.5 mm lateral shift of the patella and an increased patellofemoral lateral peak shear by 19 N. Using a rotating bearing reduced this to 7 N, but did not improve patellar kinematics and emphasized the importance of achieving the correct femoral rotation. The conclusion was that computer modelling was a useful tool in the preclinical evaluation of new implants.
Merican et al,10 from the Amis Laboratory, in a study of eight cadaveric knees looked at the effect of femoral implant rotation during active extension on both tibiofemoral and patellofemoral kinematics with the Genesis II (Smith & Nephew, Memphis, TN, USA) TKA. They had two test conditions: the standard 3° external rotation, and ± 5° from this. They emphasized that the kinematics of both compartments were different from normal. In the tibiofemoral joint the screw-home mechanism was reversed. In the patellofemoral joint the patella was displaced medially in flexion by 6 mm, and tilted more laterally by 7° in extension. External rotation of the femoral component worsened the tilt by 4°. They noted that addressing an abnormality in one degree of freedom created an abnormality in another. They concluded that it is inadvisable to correct patellar lateral maltracking by externally rotating the femoral component as this would then adversely affect tibiofemoral kinematics.
Ghosh et al,11 again from the Amis Laboratory, looked at the effects on the medial and lateral retinaculum of malrotation of the femoral component in TKA with the same set-up as Merican et al,10 and presumably with the same cadaveric knees. Again, the implant was rotated internally and externally by 5°. In external rotation the medial patellofemoral ligament (MPFL) lengthened between 90° and 0° since it is attached to bone, but had no effect on the transverse fibres of the lateral retinaculum which is attached to the iliotibial tract.
Clinical studies
Terashima et al12 undertook what was essentially a biomechanical study, but intra-operatively on patients. They used a cohort of 30 patients undergoing a rotating platform PFC Sigma (Depuy, Warsaw, IN, USA) TKA and inserted a Flexiforce pressure sensor (Nitta Co Ltd, Osaka, Japan) which is an ultrathin (100 lm) force transducer that was embedded between the resection surface of the patellar trial component and a metal plate affixed to the bony cut surface of the patella. The contact stress from 0° extension to maximum flexion was measured to obtain the patellofemoral maximum stress. The maximum values of the lateral medial patellar shift were garnered using the Vector Vision 1.61 navigation system (Brain Lab, Heimstetten, Germany) in kinematic mode. They found that the patellofemoral contact stress did not correlate with the sagittal and coronal alignment of the femoral component or the patellar tracking. Only the rotational alignment of the femoral component was correlated with patellofemoral contact stress, which decreased as the femoral component rotated more externally. It should be noted that the experimental conditions exclude the effect of muscle forces, any changes in limb rotation and any effects of planting the foot.
A study by Heesterbeck et al13 reported a prospective cohort study in 49 patients undergoing a primary TKA using CT-free navigation and a balanced gap technique and a total condylar fixed-bearing cruciate-retaining implant (Mathys Ltd, Bettlach, Switzerland). Femoral rotation was referenced off the posterior condyles. The aim of the study was to measure the lateral tilt of the patella and patellar displacement. At 2 years follow-up they found the external femoral rotation varied from –3° to +12° and did not predict the post-operative patellar tilt or displacement. The pre-operative patellar position correlated with the post-operative one, but not the femoral implant rotation as defined by the balanced gap technique. It should be emphasized that patellar tilt and displacement in extension reveals little about the dynamic path of the patella during knee motion.
A recent systematic review14 looked at the outcomes of rotational alignment with patient-specific instrumentation (PSI) in TKA. The review covered publications between 2000 and 2014. Six randomized controlled trials were selected with 444 knees reported that fitted the inclusion criteria. These trials did not specifically look at patellar tracking, but it was inferred that with correct femoral component rotation the tracking would be normal. The review favoured PSI over conventional techniques for defining femoral implant rotation.
Femoral rotation: femoral implant design
Cadaveric studies
A cadaveric study of six knees looked at whether trochlear design would affect patellar tracking.15 Comparison was made between a symmetrical femoral prosthesis (Kinemax, Stryker, Mahwah, NJ, USA) and a modern asymmetrical one (Triathlon, Stryker, Mahwah, NJ, USA) where there was a more prominent proximal-lateral lip and the groove aligned proximolaterally to distomedially to see the effect on patellar tracking. They found no difference between either design, both of which showed significant differences in lateral displacement stability of the patella and, near extension, the patellae tilted laterally by about 6° and flexed by 8° compared to normal. The conclusion was that the femoral implant design with respect to the trochlea had no effect.
Another study of five cadaveric knees looked at four different conditions: normal knee with patella replaced, cruciate-retaining, condylar-stabilizing, and posterior-stabilized TKAs using the Stryker Triathlon design.16 The study measured the patellofemoral pressure, patellar offset, and patellar tilt. The patellofemoral pressure in the normal knee remained less than 5 N for the full range of motion, while the patellofemoral pressure in TKA knees increased to more than 8 N at 120° knee flexion. No significant difference in patellofemoral pressure was observed between the three types of TKA. No significant difference in patellar offset was noted in the TKA groups but the normal knee patellar offset decreased with increasing knee flexion angles. The amount of lateral patellar tilt in the normal knee was significantly larger than the TKA knees in the full range of motion. The study also showed that differences in implant design did not significantly affect patellar tracking.
Implant position: femoral
Femoral component flexion
Femoral implant flexion is illustrated in Figure 2.
Fig. 2.
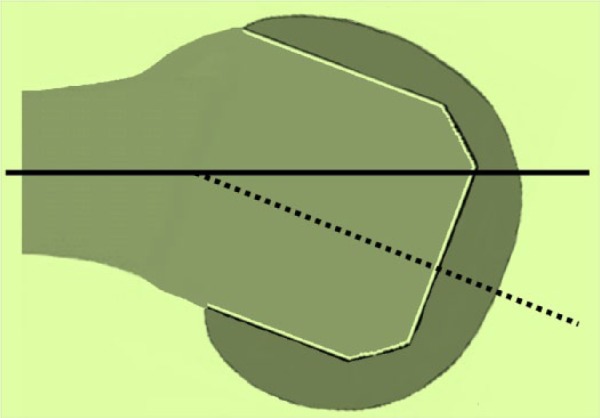
Diagram showing the anatomical axis (continuous line) and the equivalent axis (dotted line) for the femoral implant, which is flexed.
Cadaveric studies
Keshmiri et al17 conducted a laboratory-based study of 10 intact lower limbs using a fixed-bearing cruciate-retaining Sigma PFC (DePuy, Warsaw, IN, USA) TKA. They measured pre- and post-implantation patellar tracking using the BrainLab (Feldkirchen, Germany). Six knees were aligned at 5° flexion of the femoral component and four at 0° (the jigging system has a built-in 3° external rotation). They found that in the 5° flexion group as well as in the 0° flexion group, the patellae shifted more laterally at all flexion angles. They also tilted medially from 50° to 90° of flexion, in the opposite direction, compared to the pre-operative knee. Sagittal component alignment from 0° to 5° for the femur and with a 1° increase in posterior tibial component slope resulted in a patellar lateral shift of 17 mm. In contrast, the patellar epicondylar distance, rotation and tilt were not significantly influenced. Sagittal component alignment in TKA has a major impact on patellar kinematics.
Clinical studies
In a study that pre-dated their laboratory work, Keshmiri et al,18 using the same prosthesis and navigation system (fixed-bearing cruciate-retaining Sigma PFC TKA and BrainLab) looked at a cohort of 40 patients undergoing primary TKA. They measured the pre- and post-implantation patellar tracking between 30° and 90° knee flexion (0° to 30° were excluded because of absent muscle tone) intra-operatively. Both absolute and relative values for patellar mediolateral shift, axial tilt, and coronal rotation were collected. They found that sagittal component alignment, but not rotational component alignment, had a statistically significant influence on patellar kinematics. There were major differences in patellar kinematics between the pre-operative arthritic knee and the knee after TKA with more lateral shift and tilt up to 60° knee flexion. They concluded that combined sagittal component alignment, in particular, appeared to have a major effect on patellar kinematics. It should be noted that they reported: ‘at 90° of flexion, a change in femoral component flexion of 1° in combination with a change in tibial posterior slope of 1° increases the difference (pre-operative–post-operative) in epicondylar distance by about 1.5 mm (0.6 mm +0.8 mm). Therefore, the post-operative value for epicondylar distance would be reduced by about 1.5 mm. This effect is slightly reduced at flexion angles of 75° or less’.18 It can be questioned whether these values are clinically relevant. The study does not show the changes that happen within an individual knee, nor do we know how a normal knee compares to an implanted one.
Femoral component valgus
An illustration of the femoral implant in valgus is given in Figure 3.
Fig. 3.
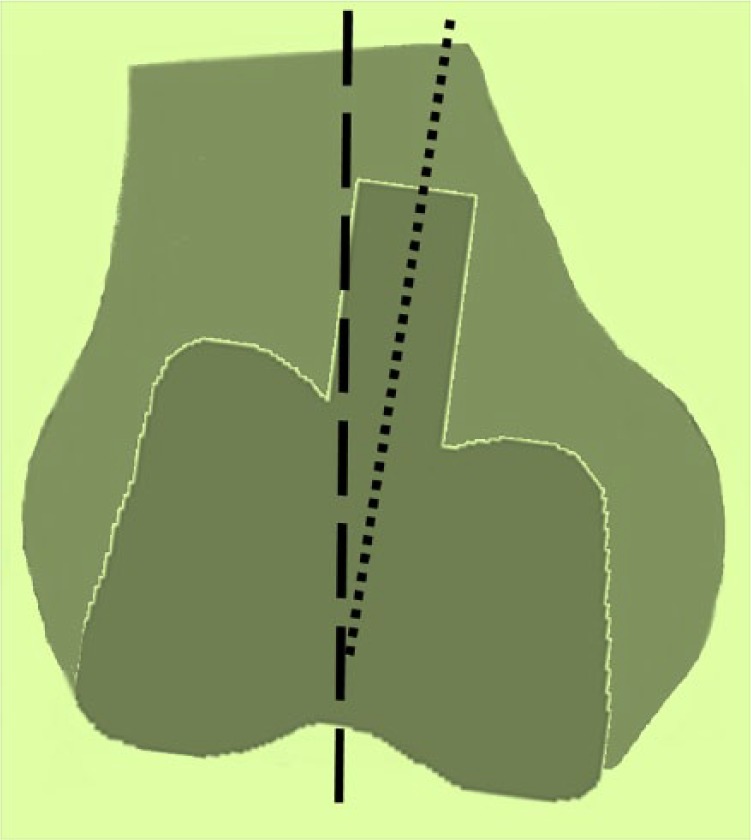
Diagram showing the mechanical axis (dashed line) and the equivalent axis (dotted line) for the femoral implant which is in valgus.
Clinical study
Slevin et al19 reported on a study involving 64 knees in 62 patients who underwent TKA without patellar resurfacing. The implant type was not reported. They assessed the loading of the patella using Spect-CT and were interested in the positional factors that affected this. Scans were taken at 12 and 24 months post-implantation. Femoral component position was found to range from –5° to +5° in the coronal plane where 0° was in the line of the anatomical axis. They found that with the femoral component only a valgus position was associated with increased loading of the lateral areas of the patella as measured by bone tracer uptake. No association was found with sagittal or rotational alignment. The lateral uptake reflects the lateral tracking of the patella in a valgus-aligned knee but could also reflect trochlear morphology. Interestingly, although they recorded Knee Society Scores and reported the mean and standard deviation, they did not perform correlations with their bone tracer uptake findings. It would be very interesting to know whether high bone tracer uptake is associated with anterior knee pain, or not.
Femoral component mediolateral
An illustration of a femoral implant which lies medially is given in Figure 4.
Fig. 4.
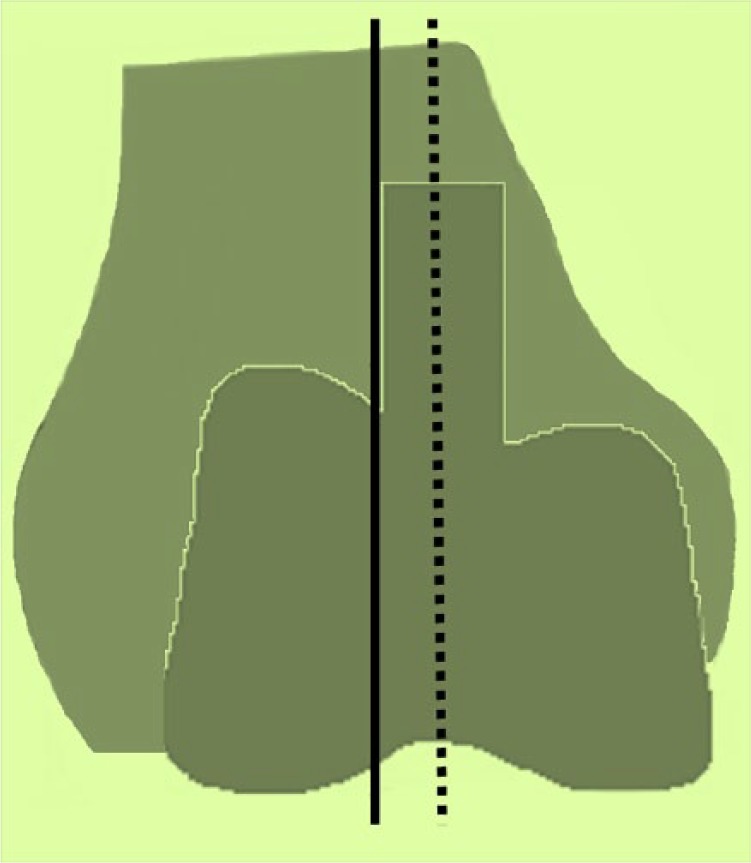
Diagram showing the mechanical axis (continuous line) and the same at the midpoint of the femoral implant which lies medially.
Clinical study
Van de Groes et al20 reported on a follow-up to a previous study of a cohort of 61 patients who had undergone a TKA. This had shown that the implant trochlea was medialized by a mean of 2.5 mm (range from −4 mm to +9 mm) with respect to the native groove. Van de Groes et al looked at the association of medialization of the femoral component and post-operative anterior knee pain. The TKA system used was the LCS rotating platform prosthesis (DePuy, Warsaw, IN, USA) in 21 patients and the PFC prosthesis (DePuy, Warsaw, IN, USA) in the other 40. Telephone follow-up of 40 patients was undertaken at a mean follow-up of 9 years. They concluded that a more medial position may result in a better post-operative outcome, which could probably be explained by the non-physiological lateral orientation of the trochlear groove in TKA designs.
Implant position: tibial
Rotation
Cadaveric studies
The rotational alignment of the tibial component is important as it has a direct effect on the tibial tubercle-trochlear groove (TTTG) distance (Fig. 5). Martin et al21 created CT reconstructions of 30 tibial specimens. They then modelled two types of symmetrical tibial implant and two different asymmetrical ones and used computer modelling to show that fitting the implant to maximize coverage of the bony surface risks malrotation. This is worse with symmetrical designs compared to asymmetrical ones. Rotational alignment of the tibial component is more important than bony coverage. However, as the authors acknowledge, all implants were aligned to the medial sixth of the tibial tubercle and therefore did not allow for surgical input into the alignment. I would also add that, especially in the varus knee with a large posteromedial osteophyte, the upper tibia can be matched to the tibial component after insertion, relaxing the medial ligament and improving knee flexion. However, the Keshmiri et al18 study reported above found no effect on patellar kinematics with tibial component rotation.
Fig. 5.
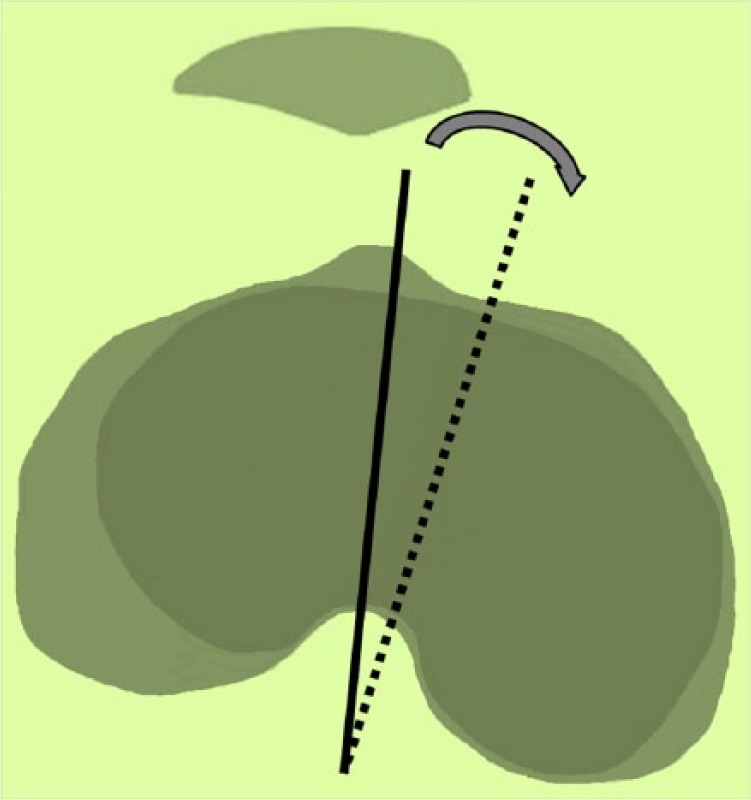
Diagram showing that rotating the implant (sagittal axis dotted line) internally (medially) relative to the tibia (sagittal axis continuous line) displaces the tibial tubercle laterally and consequently the patella as well.
Slevin et al19 also reported on the effects of tibial alignment on patellar stress in their study. They found no correlation between the bone tracer uptake in the patella and the TTTG distance.
Slope
Cadaveric studies
Slevin et al19 also reported no correlation between the bone tracer uptake in the patella and the coronal or sagittal alignment of the tibial component. Keshmiri et al18 also looked at the effect of the posterior slope of the tibia and found no effect on patellar mediolateral shift but a statistically significant difference in the epicondylar distance. Since this difference had a mean of 0.9 mm (95% CI 0.3 mm to 1.4 mm) it is unlikely that this is clinically relevant.
Implant position: patella
There have been no studies looking at differences in the superoinferior position of the patellar button on the cut patella surface. One study looked at the mediolateral position. Lee et al22 undertook a single-surgeon retrospective review from an original cohort of 426 knees (310 patients) and a study cohort of 177 knees (143 patients) who had undergone a mixture of primary TKAs: Scorpio NRG (Stryker, Mahwah, NJ, USA), Nexgen LPS (Zimmer,Warsaw, IN, USA), PFC Sigma (Johnson & Johnson, Raynham, MA, USA), and Optetrak (Exactech, Gainesville, Florida, USA). All-polyethylene, dome-shaped patellar components with three fixation lugs were used in all cases. Lee et al divided the cohort into two groups: those with the patella displaced from the median ridge by at least 3 mm (n = 34) and those where the two corresponded (n = 143). The two groups were similar demographically. At one year no differences were found between the two groups with respect to the Knee Society Score, Kujala score or range of knee motion. The position of the patellar component was measured from Merchant views and calculated from the width of the patella, comparing this to the pre-operative radiograph. This assumes that there was no effect on the width by the removal of any patellar osteophytes.
Patellar thickness
Cadaveric studies
Merican et al,23 in a study of eight cadaveric knees, looked at the effects of overstuffing the patella on patellofemoral kinematics in TKA. They used the Genesis II (Smith & Nephew, Memphis, TN, USA) implant and the Polaris optical system (Northern Digital Incorporated, Waterloo, Canada) with active optical trackers to obtain the kinematic data processed with Visual3D software (C-Motion Inc., Maryland, USA). They looked at the effect of the patellar thickness on patellar tracking from –2 mm to +4 mm at 2 mm increments. As the thickness increased so did the lateral patellar tilt. This could be corrected by a lateral retinacular release but this resulted in abnormal tibial external rotation. They also noted that inserting the femoral implant shifted the groove medially, but the thickness of the patella had no effect on the mediolateral patellar position. Perforce the patella was more anterior in extension, and distal at 90° flexion as the thickness increased. Bracey et al24 performed a similar study on 10 cadaveric knees but increased the patellar thickness. They found at +6 mm a significant increase in lateral patellar shift and tilt, and at +8 mm a decrease in knee flexion.
Clinical studies
In Slevin et al’s19 study, using Spect-CT also showed no association between patellar bone tracer uptake and patellar thickness and patellar height when the patella had not been resurfaced. Youm et al25 looked into whether patellar thickness would affect patellar tilt by adversely tightening the lateral retinaculum. Data were collected prospectively on 272 knees in 168 women. No explanation was given as to why men were excluded. This was a single-surgeon retrospective review. The implants used were of two different types of posterior stabilized total knee implant: the Triathlon (Stryker, Allendale, NJ, USA) in 146 knees, and the LCS (Low Contact Stress, Depuy, Warsaw, IN, USA). The patients were stratified into groups according to changes in patellar thickness measured intra-operatively with electronic callipers. The groups were:
A: Thinner by 1 mm or more (n = 30)
B: Equal or thinner by less than 1 mm (n = 45)
C: Thicker by 1 mm or less (n = 36)
D: Thicker by more than 1 mm (n = 35)
Tracking was assessed intra-operatively, and patellar tilt from Merchant’s view post-operatively at 2 weeks and 6 months. Patients with abnormal tracking intra-operatively underwent a lateral retinacular release. The button was placed centrally for mobile-bearing LCS implants, and medially for the Triathlon. The details of the lateral release rates for each system were not reported. The study found that there was an association with increased patellar tilt post-operatively only in Group D (post-operative thickness > 1 mm). The difference between the groups was 2° (6° to 8°), and pre- and post-operatively 1° (9° to 8°). The obvious conclusion is that the findings are statistically significant but clinically irrelevant.
Kim et al26 looked at the effect of the post-operative patellar thickness in patients presenting for a primary TKA who also had stiff knees from pre-operative fibrosis defined as pre-operative flexion against gravity < 100° under general anaesthesia. Eleven patients (11 knees) underwent a PCL-retaining primary TKA (PFC Sigma; DePuy Inc, Warsaw, IN, USA). To test the effect of patellar thickness four custom-made trial patellar implants were used as well as the standard trial, the former increasing by 2 mm (0 mm, 2 mm, 4 mm, 6 mm, 8 mm). The data from a previously studied cohort of 23 knees (23 patients) undergoing primary TKA without pre-operative fibrosis were used as a comparator. The effects on knee flexion and patellar tilt were assessed intra-operatively prior to implanting the definitive components. The medial patellar approached was clamped, and the tourniquet released during the testing. The two groups were similar demographically. Unsurprisingly, increasing the patellar thickness decreased knee flexion, and this effect was worse in the fibrotic group. There was also no observed effect on patellar tracking or tilt.
Conclusions
Functional patellar tracking in most primary TKAs is achieved by implanting the femoral and tibial components correctly. The recent literature has not really added anything that is useful for the practising clinician (Table 2). Previous maltracking is still thought to be best managed by correcting the maltracking prior to or during the operation. It is not sensible to over externally rotate the femoral component to correct the maltracking; this is likely to cause abnormal tibiofemoral kinematics. Work needs to be done to correlate laboratory findings of increased patellofemoral load/stress with anterior knee pain and patellar bone erosion (if not replaced) or patellar component wear and loosening. It is important to understand that the shape of the femur and patella is a major factor in the fine details of patellar tracking. Since no implant system reproduces this shape precisely for the individual patient, the patella will never track as per the native normal knee. It is clear that small differences in tracking are not clinically relevant.
Table 2.
Summary of findings of literature review on total knee arthroplasty (TKA) and factors affecting patellar tracking
| Factor | TKA tested | Findings | Clinical relevance | |
| Pre-existing patellar maltracking | None new | N/A | ||
| Femoral bony cuts | Scorpio Genesis II PFC Sigma RP Mathys TC |
No difference between MB & FB ↑ Femoral ER → abnormal TF kinematics ↑ Femoral ER → ↓ PF stress No effect on tilt or displacement by femoral rotation |
Interesting Avoid excessive femoral ER Not generalizable Not generalizable |
|
| Femoral implant design | Kinemax & Triathlon Triathlon CR/CS/PS |
No effect from change of trochlea No differences in patellar tracking or pressure between the three designs |
Interesting Interesting |
|
| Femoral | Flexion | PFC Sigma CR FB | Femoral flexion → lateral patellar shift | ? ↑ LR rates when implant flexed |
| Valgus | Not reported | Valgus → ↑ patellar stress | Interesting | |
| Mediolateral | LCS RP | Medial position had better outcome | Not generalizable | |
| Tibial | Rotation | Not reported | Maximizing coverage → internal rotation of tibial implant | Useful |
| Slope | Sigma CR FB | 1 mm change in epicondylar distance | No significant effect | |
| Patellar | Scorpio/ PFC Sigma/ Optetrak |
No difference in KSS scores at 1 year | Interesting | |
| Patellar thickness | Genesis II Not stated PFC Sigma |
↑ patellar tilt and shift at +6 mm ↓ knee flexion at +8 mm |
Unlikely to overstuff by 6 mm | |
Note. ER, external rotation; IR, internal rotation; MB, mobile bearing; FB, fixed bearing; CR, cruciate retaining; CS, condylar stabilized; PS, posterior stabilized; LR, lateral retinacular release; TF, tibiofemoral; N/A, not applicable; KSS, Knee Society Score; →, leads to.
Footnotes
ICMJE Conflict of interest statement: S. Donell declares royalties from Corin/Tornier, activity outside the submitted work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Brick GW, Scott RD. The patellofemoral component of total knee arthroplasty. Clin Orthop Relat Res 1988;231:163-178. [PubMed] [Google Scholar]
- 2. Khan M, Osman K, Green G, Haddad FS. The epidemiology of failure in total knee arthroplasty: avoiding your next revision. Bone Joint J 2016;98-B:105-112. [DOI] [PubMed] [Google Scholar]
- 3. Keshmiri A, Maderbacher G, Baier C, Zeman F, Grifka J, Springorum HR. Significant influence of rotational limb alignment parameters on patellar kinematics: an in vitro study. Knee Surg Sports Traumatol Arthrosc 2016;24:2407-2414. [DOI] [PubMed] [Google Scholar]
- 4. Victor J. Optimising position and stability in total knee arthroplasty. EFORT Open Rev 2017;2:215-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bullek DD, Scuderi GR, Insall JN. Management of the chronic irreducible patellar dislocation in total knee arthroplasty. J Arthroplasty 1996;11:339-345. [DOI] [PubMed] [Google Scholar]
- 6. Oh K-J, Yoon J-R, Yang J-H. Total knee arthroplasty in a pseudoachondroplastic dwarfism patient with bilateral patellar dislocation. Knee 2013;20:45-48. [DOI] [PubMed] [Google Scholar]
- 7. Dao Q, Chen DB, Scott RD. Proximal patellar quadricepsplasty realignment during total knee arthroplasty for irreducible congenital dislocation of the patella: a report of two cases. J Bone Joint Surg Am 2010;92:2457-2461. [DOI] [PubMed] [Google Scholar]
- 8. Colwell CW, Jr, Chen PC, D’Lima D. Extensor malalignment arising from femoral component malrotation in knee arthroplasty: effect of rotating-bearing. Clin Biomech (Bristol, Avon) 2011;26:52-57. [DOI] [PubMed] [Google Scholar]
- 9. Kessler O, Patil S, Colwell CW, Jr, D’Lima DD. The effect of femoral component malrotation on patellar biomechanics. J Biomech 2008;41:3332-3339. [DOI] [PubMed] [Google Scholar]
- 10. Merican AM, Ghosh KM, Iranpour F, Deehan DJ, Amis AA. The effect of femoral component rotation on the kinematics of the tibiofemoral and patellofemoral joints after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2011;19:1479-1487. [DOI] [PubMed] [Google Scholar]
- 11. Ghosh KM, Merican AM, Iranpour F, Deehan DJ, Andrew A, Amis AA. The effect of femoral component rotation on the extensor retinaculum of the knee. J Orthop Res 2010;28:1136-1141. [DOI] [PubMed] [Google Scholar]
- 12. Terashima T, Onodera T, Sawaguchi N, Kasahara Y, Majima T. External rotation of the femoral component decreases patellofemoral contact stress in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2015;23:3266-3272. [DOI] [PubMed] [Google Scholar]
- 13. Heesterbeek PJC, Keijsers NL, Wymenga AB. Femoral component rotation after balanced gap total knee replacement is not a predictor for postoperative patella position. Knee Surg Sports Traumatol Arthrosc 2011;19:1131-1136. [DOI] [PubMed] [Google Scholar]
- 14. Mannan A, Smith TO. Favourable rotational alignment outcomes in PSI knee arthroplasty: a Level 1 systematic review and meta-analysis. Knee 2016;23:186-190. [DOI] [PubMed] [Google Scholar]
- 15. Stoddard JE, Deehan DJ, Bull AMJ, McCaskie AW, Amis AA. No difference in patellar tracking between symmetrical and asymmetrical femoral component designs in TKA. Knee Surg Sports Traumatol Arthrosc 2014;22:534-542. [DOI] [PubMed] [Google Scholar]
- 16. Tanikawa H, Tada M, Harato K, Okuma K, Nagura T. Influence of total knee arthroplasty on patellar kinematics and patellofemoral pressure. J Arthroplasty 2017;32:280-285. [DOI] [PubMed] [Google Scholar]
- 17. Keshmiri A, Springorum HR, Baier C, Zeman F, Grifka J, Maderbacher G. Changes in sagittal component alignment alters patellar kinematics in TKA: an in vitro study. Knee Surg Sports Traumatol Arthrosc 2016;24:823-829. [DOI] [PubMed] [Google Scholar]
- 18. Keshmiri A, Maderbacher G, Baier C, et al. The influence of component alignment on patellar kinematics in total knee arthroplasty. Acta Orthop 2015;86:444-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Slevin O, Schmid F, Schiapparelli FF, Rasch H, Amsler F, Hirschmann MT. Coronal femoral TKA position significantly influences in vivo patellar loading in unresurfaced patellae after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2017;25:3605-3610. [DOI] [PubMed] [Google Scholar]
- 20. van de Groes SAW, Koëter S, de Waal Malefijt M, Verdonschot N. Effect of medial-lateral malpositioning of the femoral component in total knee arthroplasty on anterior knee pain at greater than 8 years of follow-up. Knee 2014;21:1258-1262. [DOI] [PubMed] [Google Scholar]
- 21. Martin S, Saurez A, Ismaily S, Ashfaq K, Noble P, Incavo SJ. Maximizing tibial coverage is detrimental to proper rotational alignment. Clin Orthop Relat Res 2014;472:121-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lee RH, Jeong HW, Lee JK, Choi CH. Should the position of the patellar component replicate the vertical median ridge of the native patella? Knee 2017;24:82-90. [DOI] [PubMed] [Google Scholar]
- 23. Merican AM, Ghosh KM, Baena FRY, Deehan DJ, Amis AA. Patellar thickness and lateral retinacular release affects patellofemoral kinematics in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2014;22:526-533. [DOI] [PubMed] [Google Scholar]
- 24. Bracey DN, Brown ML, Beard HR, et al. Effects of patellofemoral overstuffing on knee flexion and patellar kinematics following total knee arthroplasty: a cadaveric study. Int Orthop 2015;39:1715-1722. [DOI] [PubMed] [Google Scholar]
- 25. Youm Y-S, Cho W-S, Woo J-H, Kim B-K. The effect of patellar thickness changes on patellar tilt in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2010;18:923-927. [DOI] [PubMed] [Google Scholar]
- 26. Kim AD, Shah VM, Scott RD. The effect of patellar thickness on intraoperative knee flexion and patellar tracking in patients with arthrofibrosis undergoing total knee arthroplasty. J Arthroplasty 2016;31:1011-1015. [DOI] [PubMed] [Google Scholar]


