Abstract
Background
Problem-based learning (PBL) was introduced into Basic Medical Sciences early in the 1980s at Tribhuvan University (TU), Nepal, followed by other universities where didactic lecture method was still followed as the main teaching strategy. Despite gaining its popularity worldwide as integrated teaching learning method, PBL is not given importance in Nepal. This study aimed to assess the attitude and perceptions of undergraduate medical students regarding learning outcomes of PBL and to know their views about role and qualities of effective tutors for its successful implementation.
Methods
This descriptive study was based on a self-administered questionnaire. The first part of the questionnaire measured students’ perception and attitude toward benefits of PBL and the second part measured students’ perception about role of PBL tutor. Bachelor of Medicine and Bachelor of Surgery (MBBS) first year (2014/2015 academic year) students at Chitwan Medical College, TU, were asked to express their opinions about the importance of learning outcomes by rating each statement on a five-point Likert scale and the responses were combined into three categorical variables: “agree” (strongly agree plus agree), “neutral”, and “disagree” (strongly disagree plus disagree). Data were analyzed using SPSS version 21.0.
Results
Approximately 85.5% participants agreed that PBL is an interesting method of teaching learning. Most of them (86.7%) accepted that PBL is an interactive and a mutual learning method and improves self-directed learning (83.2%). Although 78% had recommended it better than lecture, many (54.2%) pointed it out as a time-consuming method. The participants were also highly rated (80.5%) to the statement - the tutor’s role in enhancing the constructive active learning and maintaining good intra-personal behavior.
Conclusion
Student’s attitude toward PBL was positive. They highly appreciated the roles of a tutor as facilitators and motivators for proper activities in PBL session. PBL sessions were considered effective in improving students professional knowledge and refining problem-solving and self-directed learning skills along with enriching teamwork experience.
Keywords: PBL, student’s perception, role of tutor, teaching learning method
Introduction
The problem-based learning (PBL) after its introduction in the McMaster University, Canada, in 1960s by Barrows has been adopted by many medical colleges around the globe, which helps the transformation of the medical curriculum from traditional teacher-centered to student-centered approach of learning in system-based integrated medical education.1 Its close affiliation with workplace collaboration and interdisciplinary learning contributed to its spread beyond the traditional realm of clinical education.2 Though PBL has become an integral component of medical curricula around the world, it is partially experienced in Nepal. In Nepal, PBL was introduced in Integrated Basic Medical Sciences early in 1980s in the curriculum of Institute of Medicine (IOM), Tribhuvan University (TU), followed by BP Koirala Institute of Health Sciences (BPKIHS) in 1998, Kathmandu University School of Medical Sciences (KUSMS) and its affiliated colleges in 2011, and Patan Academy of Heath Sciences (PAHS) in 2011.3 BPKIHS, PAHS, and KU have put a step forward toward implementation of PBL as hybrid curriculum, however, its successful adoption into the curriculum is still in the process of development.
In BPKIHS, 12 PBL themes, each of one-week duration with seven-jump process, were organized during the course of the two years of phase one of the Bachelor of Medicine and Bachelor of Surgery (MBBS) course. In addition, the cardiovascular system is completed with four PBL themes. In this, the Basic Science subjects are integrated around an organ system and interfaced with clinical disciplines. It is estimated that 20%–25% of the MBBS curriculum is covered by the PBL method.3,4
In KUSMS, approximately 40 PBL cases are exercised by the basic science medical students. It is estimated that each PBL case involves an average of 12 hours, which amounts to a total of ~490 case hours, which is estimated to be about 25% of actual learning time by PBL method.3,4
In PAHS, a total of 33 cases are covered in the first year and 33 in the second year. All the basic science and the clinical science teachers are involved. Here the MBBS course duration is not only longer by six months but they also use the PBL method to teach the whole curriculum. They call it “Case based learning”. To get to this point, they have had regular input with some faculty from outside the country, that from Calgary being just one of those involved. However, there is more involvement of clinical faculty than non-medicals. In Nepal, BPKIHS and Patan Academy of Health Sciences have been active in transforming the teaching learning strategy using PBL.3–5
TU-affiliated medical colleges still follow didactic lecture methods as the main teaching learning strategy. In IOM (TU), though initially two cases of PBL were discussed for each of the two years of MBBS, this figure was reduced to one case per year over the course of one week.4,5
IOM, TU-affiliated colleges
At KIST, the curriculum followed is of TU and so the current practice is to have one PBL problem per year discussed over the course of one week.4,5
In Chitwan Medical College (CMC), the PBL sessions are started with conjunction with lectures, the latter covering the portion of the syllabus not covered through PBL. It is introduced to MBBS students in their basic science phase, but PBL is not being introduced in other courses at CMC, such as Dental and Nursing sciences. The PBL practice starts with a trigger on the first day followed by required resource and self-study sessions related to the PBL and discussions on second day. At the completion of case on the fourth day, MCQs type of quiz is held to check for participation of students. The pattern of tutorial, self-study, and resource session follows till end with a final presentation by students and end of topic on the sixth day. In order to acquaint the students for the PBL, an orientation session on PBL is provided to MBBS first year and second year students before initiating PBL. The orientation introduces the concept of PBL to the students and attempts to make them understand seven-jump process of PBL and to make them aware about the role of students and tutors to organize PBL. All basic science teaching faculty takes part in the tutoring of PBL sessions. The senior professors are, however, not obligated to do PBL sessions and their participation is voluntary. Ten groups of 10–12 students go through PBL under the guidance of ten tutors. All tutors either have previous experience of conducting PBL sessions or have participated in a workshop on PBL held at teacher’s training program in CMC. We have plan of building up library of PBL themes for use in the course. This is partly to ensure interest in the students. The numbers of PBL cases per system that we intend to use during two years of basic sciences of MBBS are still not confirmed.
There are firm advocates for utilizing PBL in the medical colleges of Nepal. In the same time, there are many who would like to stick to the traditional methods saying that PBL is not in extensive use. This could be reason why PBL practice is not prioritized as a main teaching learning strategy in TU-affiliated medical colleges, though TU is the pioneer in introducing PBL in Nepal.6
CMC was the second among the TU-IOM-affiliated colleges in introducing PBL. We have started with one PBL case in both first and second year MBBS course. Therefore, student’s perception about PBL is an important aspect to measure the strength of its implementation. Many studies have reported a positive impact of PBL on the learning process. PBL enhances student’s performance in many ways, including increasing knowledge horizon and retention, better understanding of basic sciences topics, integration of basic and clinical sciences, and improvement of problem-solving skills.7 In addition, it contributes to the early growth of professionalism by developing interpersonal and communication skills, presentation skills, promotes self-directed learning, and enhances students’ enthusiasm and motivation.8
For the effectiveness of PBL, the tutor and tutoring are among the most important factors influencing the PBL strategy, as tutors play a central role in facilitating PBL tutorials and help students to achieve their learning objectives.9 The perception of undergraduate medical students regarding the qualities of tutoring and effectiveness of tutor is of remarkable importance.10 However, a few studies regarding student’s perception of the PBL session indicated controversy in their findings. In Malaysia, a study by Emerald et al showed that PBL was time-consuming, and can be substituted by other instructional methods.11 Students will remember more content if brief activities are introduced in the lecture, and in order to emphasize and maintain students individual responsibility, the entire course need not be team based.12 Newman concluded that the limited high-quality evidence available from existing reviews does not provide robust evidence about the effectiveness of different kinds of PBL in different contexts.13
Therefore, a student’s impression of the PBL session remains controversial at different places. Thus, at the very introductory level of PBL in CMC, this study was conducted to explore the attitude and perceptions of undergraduate medical students regarding learning outcomes of PBL and sought their views about the role of tutors and qualities of effective tutors.
Methods
This descriptive study, conducted at CMC, Nepal, was based on an anonymous self-administered questionnaire on perceptions of PBL.9,10 The data were collected from medical undergraduate students of first year MBBS of 2014–2015 academic year. All students (n=113) of MBBS first year were included in this study. The questionnaire was developed in light of the stated objectives and purposes of the study. Methodologies of some relevant published researches were reviewed, and relevant questions that could investigate the objectives of the study in our setup and population were selected to be utilized in the questionnaire.14–16
The questionnaire was divided into 2 parts: first part containing 12 statements and second part containing 11 statements, measuring the students’ perception and attitude toward the benefits of PBL sessions and the students’ perception about the role of tutor in the process of conducting PBL, respectively. Students were asked to express their opinions about the importance of these learning outcomes by rating each learning outcomes on a five-point Likert scale as following: 1) strongly disagree, 2) disagree, 3) neutral, 4) agree, and 5) strongly agree. Pilot study was conducted on 20 students to increase validity of questionnaire. The internal consistency of all 23 items was measured by Cronbach’s alpha reliability test and showed a value of 0.88 (χ2=1783.7, p=0.001).
All participants (n=113) had completed the questionnaires completely; therefore, 100% of samples were included for data analysis. Data were coded and entered into Microsoft Excel software and analyzed using SPSS version 21.0 (IBM Corporation, Armonk, NY, USA). The five-point Likert scale responses were combined into three different categorical variables: “agree” (strongly agree plus agree), “neutral”, and “disagree” (strongly disagree plus disagree) since the summed up related items emphasize the score for a group of statements.17
Descriptive analysis was done to summarize information by calculating the number and percent for categorical variables. All the participants were informed of the objectives of the study, and information on the items in the questionnaire was clearly explained before the commencement of study. Study participants were made aware that the collected data were intended for publication and presentation. Written informed consent was taken from the participants before distribution of questionnaires. The proposal of this study was reviewed and approved by the Institutional Review Committee of Chitwan Medical College (CMC-IRC), Nepal.
Results
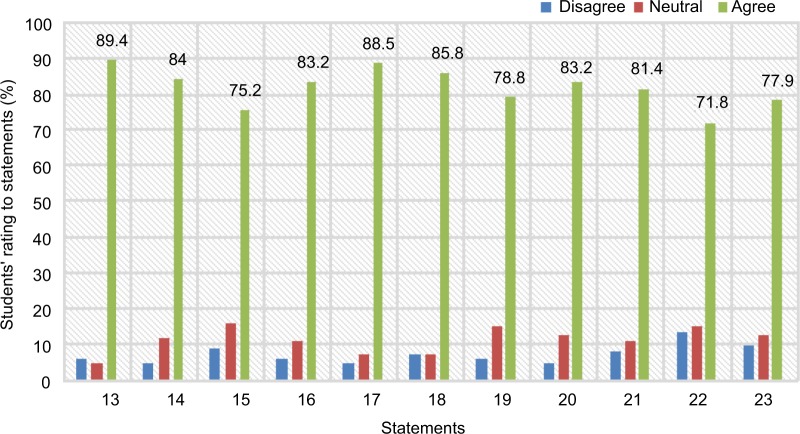
One hundred thirteen undergraduate medical students (male 73% and female 27%) participated in this study. Average age of the participants was 18.84±0.98 (17–20) years. No sex-wise difference in responses to the statements was observed. Overall perception and attitude of students toward PBL (Table 1) and about the role of tutors involved in the PBL sessions (Figure 1) was positive. Ninety seven percent of the students stated that PBL is an interesting method of teaching and learning, whereas only 7% disagreed. About 89% cited that focus on common medical problems was the reason of their interest in this method. Eighty seven percent students reported that they enjoyed cooperative group learning of PBL. Most of them (89.4%) realized that learning issues generated during the group discussion was the stimulus for the group discussion and self-directed learning. High percentage (84%) of them agreed to the statement that discussion in the tutorial group determined to a large extent what they would like to study. Although majority of students (61.9%) rated that they studied to a large extent independently from the learning issues generated, this percentage was comparably less than that for other statements. About 50% students reported that this approach had taken less time than conventional lecture in learning the course objectives, while remaining 50% of participants had inclined their thoughts that it was a relatively more time-consuming method. In this study, there was appreciable rating for the tutors too. More than 80% of students reported that tutors stimulated them for constructive/active, contextual and self-directed learning by encouraging their discussions and rewarding them with appropriate feedback on both individual basis and group basis (Figure 1).
Table 1.
Perceptions and attitude of undergraduate medical students toward PBL (n=113).
| S.N. | Statements | Disagree | Neutral | Agree | Mean±SD |
|---|---|---|---|---|---|
| 1. | I have found the PBL course interesting. | 7 (6.2%) | 9 (8%) | 97 (85.8%) | 4.12±0.86 |
| 2. | I have found that focusing the course on common medical problems has made the course seem more relevant to my interests. | 6 (5.3%) | 6 (5.3%) | 101(89.4%) | 4.30±0.80 |
| 3. | Working in groups means learning from one another. | 3 (2.7%) | 12 (10.6%) | 98 (86.7%) | 4.30±0.80 |
| 4. | I have understood the applied aspects of the course better than if it had been lectured in the conventional way. | 12 (10.6%) | 23 (20.4%) | 78 (69.1%) | 3.82±0.97 |
| 5. | This approach has taken less time than conventional lecture in learning the course objectives. | 20 (17.7%) | 31 (27.4%) | 62 (54.8%) | 3.49±1.05 |
| 6. | The discussion in the tutorial group determines to a large extent what I will study. | 3 (2.7%) | 15 (13.3%) | 95 (84%) | 4.02±0.70 |
| 7. | The tutorial group discussion is an important stimulus for my learning activities during self-study. | 2 (1.8%) | 17 (15%) | 94 (83.2%) | 4.13±0.76 |
| 8. | The learning issues generated are the most important starting point for my learning activities during self-study. | 5 (4.4%) | 21 (18.6%) | 87 (77%) | 4.03±0.85 |
| 9. | I study to a large extent independently from the learning issues generated. | 14 (12.4%) | 29 (25.7%) | 70 (61.9%) | 3.78±1.02 |
| 10. | Tutors have stimulated my learning activities. | 8 (7.1%) | 14 (12.4%) | 91 (80.5%) | 4.05±0.88 |
| 11. | In general, tutors stimulate students to make use of different sources of information. | 5 (4.5%) | 13 (11.5%) | 95 (89.6%) | 4.20±0.87 |
| 12. | In general, tutors have an important influence on the selection of learning issues. | 9 (8%) | 16 (14.2%) | 88 (77.8%) | 3.98±0.95 |
Abbreviation: PBL, problem-based learning.
Figure 1.
Students’ perception about the role of tutor in PBL (n=113).
Notes: Constructive/active learning: the tutor stimulated us to summarize what we had learnt in our own words (13); the tutor stimulated us to search for links between issues discussed in the tutorial group (14); the tutor stimulated us to understand underlying mechanisms/theories (15). Self-directed learning: the tutor stimulated us to generate clear learning issues by ourselves (16); the tutor stimulated us to search for various resources by ourselves (17). Contextual learning: the tutor stimulated us to apply knowledge to the discussed problem (18); the tutor stimulated us to apply knowledge to other situations/problems (19). Collaborative learning: the tutor stimulated us to give constructive feedback about our group work (20); the tutor stimulated us to evaluate group co-operation regularly (21). Intra-personal behavior as tutor: the tutor had a clear picture about his/her strengths/weaknesses as a tutor (22); the tutor was clearly motivated to fulfill their role as a tutor (23).
Abbreviation: PBL, problem-based learning.
Discussion
PBL has been introduced in many medical universities around the globe, and the medical educationists are in the way of establishing its existence in response to a set of perceived problems in medical education. These problems include emphasis on fact memorization over problem-solving skills, limited direct orientation of basic science education to clinical career, and the need to develop habits of lifelong learning.18 Students’ perception and attitude about PBL has become the bottom line for its success in gaining popularity among the medical universities. Our study revealed that PBL was very interesting for majority of students (97%) who participated in the PBL sessions. They also highlighted that focusing the course on common medical problems made the course more relevant to their interests. Moreover, the reason for their aroused interests toward the PBL sessions could be due to the well-designed PBL scenarios, which help cultivate the students’ interest in their profession from the very beginning of their career. Medical educationists have worked on the fact that to increase students’ interests, the selection of problem scenario for PBL should be moderately challenging linking the topic to the learner and should be very relevant to the profession.19 Students in our study realized that they understood the applied aspects of the course better than if it had been lectured in the conventional way. Moreover, most of them reported that the PBL sessions helped to apprehend basic medical sciences concepts and increase their performance in cognitive and psychomotor domains. Our study showed that PBL sessions imparted better knowledge, skills, and behavior; previous studies support this finding.20,21
In contrast to this, Khan et al mentioned that knowledge and attitudes of medical students were better in students who were trained through lecture-based learning compared to students who studied using PBL method.22 Students in this study pointed that working in groups meant that they learned from each other. They also agreed to the statement that the tutorial group discussion was an important stimulus for their learning activities during self-study. Their discussion in the tutorial group determined to a large extent what they would want to study. The learning issues generated were the most important starting point for their learning activities during self-study. Overall attitude of students was very positive toward the learning, especially cooperative learning in the group, during PBL tutorial session. Our findings are supported by the report of Nandi et al pointing that students, in PBL, had very congenial and fearless environment during discussion with own friends that is lacking in teacher-centered methods.23 This had positive psychological impact on students creating a healthy learning environment that was “more stimulating and more humane” than did in conventional method.23 PBL improves teaching and learning process because it focuses more on developing students as self-directed learners compared to traditional lectures that encourage students to be spoon-fed by lecturers.24
This could be the reason for the development of positive perception and attitude about PBL in students that favored them to study to a large extent independently from the learning issues generated in the discussion.
Participants of our study showed very courteous attitude toward the faculties involved as tutors in PBL sessions. Students reported that tutors were acting like catalyst during discussion and they played very crucial roles in maintaining the group dynamics and harmony. They also helped in finding the learning issues in a very constructive way and behaved as guide but not like the sage on the stage as they do in the lecture method of teaching learning. Like this, several studies revealed that the students had more contact time with faculty than students who engaged in the traditional teaching learning.25,26 The tutors are the facilitators in PBL but not the disseminators of information as in lecture method.27
In this study, students also highly appreciated the tutors as they stimulated them for constructive and self-directed learning to search for links between issues generated in discussion and to understand underlying mechanisms/theories. Tutors highly encouraged them to solve applied clinical problems with creative thinking by applying the knowledge acquired by collaborative and self-directed learning during PBL. This is in line with the previous report mentioning that one of the prime roles of a PBL tutor is to facilitate the PBL process by keeping the group focused on tasks and guiding the students to achieve their goals.28 Tutors who are skilled in group dynamics are evaluated more highly than those who are not so skilled.28,29 In our study, students reported that tutors evaluated them on both individual basis and group basis and encouraged them by giving very constructive feedback that certainly motivated them to perform better and better on each passing day of PBL session. During the process of PBL, tutors play an essential role in facilitating and efficiently structuring tutorials to enable students to construct individual cognitive networks, and have a significant impact on students’ performance in subsequent assessments.30
Overall perception of students toward PBL and about the role of tutors involved in the PBL sessions was very positive, with the exception being some students (50%) perceiving PBL as a time-consuming method, which is also supported by Telang.31
Conclusion
This study highlighted the perspectives of students’ internal feeling toward PBL, with findings that PBL was interesting to them and it had a great contribution in improving the knowledge horizon and learning skills and developing interpersonal, communication, and presentation skills. They also highly appreciated the roles of tutor as facilitators and motivators for proper activities in PBL tutorial session. However, the small sample size data may be the limitation of this study in satisfying the full potential statistically. Similar studies can be conducted in other medical colleges of Nepal, which could certainly help in introducing PBL as a method of learning.
Acknowledgments
The authors would like to thank all the students who participated in this study.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Barrows HS. Problem-based learning in medicine and beyond: a brief overview. In: Wilkerson L, Gilselaers H, editors. Bringing Problem-based Learning to Higher Education: Theory and Practice. San Fran-cisco, CA: Jossey Bass Inc; 1996. [Google Scholar]
- 2.Yew EH, Schmidt HG. Evidence for constructive, self-regulatory, and collaborative processes in problem-based learning. Adv Health Sci Educ Theory Pract. 2009;14(2):251–273. doi: 10.1007/s10459-008-9105-7. [DOI] [PubMed] [Google Scholar]
- 3.Dixit H, Sharma SC. The MBBS Programme in Nepal. J Nepal Med Assoc. 2002;41:341–58. [Google Scholar]
- 4.Pradhan B, Ranjit E, Ghimire MR, Dixit H. History of problem based learning in Nepal and experiences at Kathmandu Medical College. J Kathmandu Med Coll. 2012;1(1):37–44. [Google Scholar]
- 5.Jane in Nepal: Contrasting PBL Tutor Training at PAHS (Nepal) and at the IMP (Canada). Blog.
- 6.Pant DS. Experiences from the Institute of Medicine, Tribhuvan University on introducing Problem Based Learning (PBL) in an organ system based integrated curriculum. J Nep Med Assoc. 2000;39:232–239. [Google Scholar]
- 7.Rakhudu MA, Amaize A, Useh U, Maselesele M. Inter and intra professional collaboration in the implementation of problem based learning in nursing education: lesson for South Africa. Life Sci J. 2012;9(4):344–353. [Google Scholar]
- 8.Azer SA. Interactions between students and tutor in problem-based learning: the significance of deep learning. Kaohsiung J Med Sci. 2009;25(5):240–249. doi: 10.1016/S1607-551X(09)70068-3. [DOI] [PubMed] [Google Scholar]
- 9.Wood SJ, Woywodt A, Pugh M, Sampson I, Madhavi P. Twelve tips to revitalize problem based learning. Med Teach. 2014;17:1–7. doi: 10.3109/0142159X.2014.975192. [DOI] [PubMed] [Google Scholar]
- 10.Al Haqwi AI. Learning outcomes and tutoring in problem based-learning: how do undergraduate medical students perceive them? Int J Health Sci (Qassim) 2014;8(2):125–132. doi: 10.12816/0006078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Emerald NM, Aung PP, Han TZ, et al. Students’ perception of problem based learning conducted in phase1 medical program, UCSI University, Malaysia. South East Asian J Med Educ. 2013;7:45–48. [Google Scholar]
- 12.Al-Naggar RA, Bobryshev YV. Acceptance of Problem Based Learning among Medical Students. J Community Med Health Educ. 2012;2(5):146. [Google Scholar]
- 13.Newman M. A pilot systematic review and meta-analysis on the effectiveness of problem-based learning. [Accessed December 12, 2005]. Available from: http://www.ltsn-01.ac.uk/docs/pbl_report.pdf.
- 14.Dolmans DH, Ginns P. A short questionnaire to evaluate the effectiveness of tutors in PBL: validity and reliability. Med Teach. 2005;27(6):534–538. doi: 10.1080/01421590500136477. [DOI] [PubMed] [Google Scholar]
- 15.Carolyn G, Caroline M. A PBL evaluation toolkit: Building the evidence-base to understand effective practices. Procedia Soc Behav Sci. 2012;47:1686–1691. [Google Scholar]
- 16.Al-Drees AA, Khalil MS, Irshad M, Abdulghani HM. Students’ perception towards the problem based learning tutorial session in a system-based hybrid curriculum. Saudi Med J. 2015;36(3):341–348. doi: 10.15537/smj.2015.3.10216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bertram D. Likert Scale—Topic report CPSC-681. [Accessed February 21, 2018]. Available from: http://pages.cpsc.ucalgary.ca/~saul/wiki/uploads/CPSC681/topic-dane-likert.doc.
- 18.Saalu L, Abraham A, Aina W. Quantitative evaluation of third year medical students’ perception and satisfaction from problem based learning in anatomy: a pilot study of the introduction of problem based learning into the traditional didactic medical curriculum in Nigeria. Educ Res Rev. 2010;5:193–200. [Google Scholar]
- 19.Hung W. The 3C3R model: a conceptual framework for designing problems in PBL. IJPBL. 2006;1(1):55–77. [Google Scholar]
- 20.Hudec R, Tisonova J, Bozekova L, Wawruch M, Kriska M, Kristova V. Modified problem-based learning in pharmacology. Bratisl Lek Listy. 2009;110(11):732–735. [PubMed] [Google Scholar]
- 21.Alper A. Attitudes towards problem-based learning in a New Turkish Medical Curriculum. World Appl Sci J. 2008;6:830–836. [Google Scholar]
- 22.Khan H, Khawaja MR, Waheed A, Rauf MA, Fatmi Z. Knowledge and attitudes about health research amongst a group of Pakistani medical students. BMC Med Educ. 2006;6:54. doi: 10.1186/1472-6920-6-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nandi PL, Chan JN, Chan CP, Chan P, Chan PL. Undergraduate medical education: comparison of problem-based learning and conventional teaching. Hong Kong Med J. 2000;6(3):301–306. [PubMed] [Google Scholar]
- 24.Albanese MA, Mitchell S. Problem-based learning: a review of literature on its outcomes and implementation issues. Acad Med. 1993;68(1):52–81. doi: 10.1097/00001888-199301000-00012. [DOI] [PubMed] [Google Scholar]
- 25.Hwang SY, Kim MJ. A comparison of problem-based learning and lecture-based learning in an adult health nursing course. Nurse Educ Today. 2006;26(4):315–321. doi: 10.1016/j.nedt.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 26.Chan LC. The role of a PBL tutor: a personal perspective. Kaohsiung J Med Sci. 2008;24(Suppl 3):S34–S38. doi: 10.1016/s1607-551x(08)70092-5. [DOI] [PubMed] [Google Scholar]
- 27.Othman SY, Shalaby SA. Students’ perception and acceptance of problem-based learning approach in critical care nursing practice. Presented at: Scientific Cooperations International Workshops on Medical Topics; June 7–8; 2014; Ankara, Turkey. [Google Scholar]
- 28.Azer SA. Challenges facing PBL tutors: 12 tips for successful group facilitation. Med Teach. 2005;27(8):676–681. doi: 10.1080/01421590500313001. [DOI] [PubMed] [Google Scholar]
- 29.Bowman D, Hughes P. Emotional responses of tutors and students in problem based learning: lessons for staff and development. Med Educ. 2005;39(2):145–153. doi: 10.1111/j.1365-2929.2004.02064.x. [DOI] [PubMed] [Google Scholar]
- 30.Bosse HM, Huwendiek S, Skelin S, Kirschfink M, Nikendei C. Interactive film scenes for tutor training in problem-based learning (PBL): dealing with difficult situations. BMC Med Educ. 2010;10:52. doi: 10.1186/1472-6920-10-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Telang A. Problem-based learning in health professions education: an overview. Arch Med Health Sci. 2014;2:243–246. [Google Scholar]