Abstract
Psychological aspects of a person, such as the personal value and belief systems, cognition and emotion, form the basis of human health behaviors, which, in turn, influence self-management, self-efficacy, quality of life, disease control and clinical outcomes in people with chronic diseases such as diabetes mellitus. However, psychological, psychosocial and behavioral interventions aimed at these groups of patients have yielded inconsistent effects in terms of clinical outcomes in clinical trials. This might have been due to differing conceptualization of health behavioral theories and models in the interventions. Assimilating different theories of human behavior, this narrative review attempts to demonstrate the potential modulatory effects of intrinsic values on cognitive and affective health-directed interventions. Interventions that utilize modification of cognition alone via education or that focuses on both cognitive and emotional levels are hardly adequate to initiate health-seeking behavior and much less to sustain them. People who are aware of their own personal values and purpose in life would be more motivated to practice good health-related behavior and persevere in them.
Keywords: behavioral medicine, psychological theory, long-term care, diabetes care, self-management, self-efficacy, chronic diseases
Introduction
Diabetes mellitus and other non-communicable chronic diseases (e.g., cancers, ischemic heart disease, stroke, COPD and asthma) demand an acceptance of change in one’s life’s prospects and adherence to unceasingly progressive treatment regimens.1 Non-communicable chronic diseases were the leading causes of death (72.3%) and diabetes mellitus recorded an increase in years of life lost due to premature mortality globally in 2016, when other causes decreased significantly.2 The most common type of diabetes mellitus is type 2 diabetes mellitus, accounting for >90% of all diabetes cases, and it was the sixth leading cause of disability in 2015.3 Diabetes mellitus has long been a global epidemic with about one-third of a billion of the world’s population now living with diabetes,4 and it is projected to increase to 642 million people by the year 2040.5 By the end of 2015, diabetes mellitus was estimated to have caused 5 million deaths and between USD 673–1,197 billion was spent in annual health care.5
People with diabetes mellitus suffer from other chronic diseases as comorbidities or complications such as hypertension, dyslipidemia, cardiovascular diseases (coronary heart disease, cerebrovascular disease and peripheral arterial disease), nephropathy, retinopathy and neuropathy. The complications are a result of suboptimal control of blood glucose, blood pressure and lipids,6,7 and negative moods.8–10 Type 2 diabetes mellitus increases the risk of death from cardiovascular diseases up to four times compared to people who do not have cardiovascular disease.11 Early, optimal and appropriate control of these diseases and their risk factors could prevent poor clinical outcomes12–16 not only in terms of mortality, but also the morbidity related to these illnesses.17,18 It has been shown that well-integrated health systems with improved management of risk factors, advancements in clinical decision-making support, patient education and disease management substantially reduce both mortality and the incidence of cardiovascular outcomes among people with diabetes mellitus compared to the general population.19–22
Even when different genetic and environmental factors23 are accounted for and the latest advanced and efficacious therapies are used by competent therapists,24–27 the outcomes of preventive or curative therapies for diabetes mellitus still depend on the patient’s adherence to the prescribed treatments and therapeutic lifestyle recommendations.28–31 Notwithstanding the influence that the family, social, economic and political environments have on personal health goals and behaviors;32–35 the quality of health systems36,37 and physician–patient communication in clinical consultations may also influence health behaviors and affect disease control.38,39 Nevertheless, health-seeking behavior and diabetes self-management are very much dependent on the understanding and thinking, feeling and attitudes at a personal level.40–43 Patients’ contribution to the variance in glycemic control (HbA1c) was found to be as inordinately high as 98%.44 Published data often show that poor adherence to medication, appointments, screening tests, diet, exercise and poor health behaviors were between 30% and 40%.29,45 Proportion of people with diabetes mellitus who achieved treatment targets for HbA1c <7.0% (<53 mmol/mol) was at best about 40%, blood pressure <140/90 mmHg was 80% and low-density lipoprotein cholesterol was 60%.31,46–48 The causes for these nonadherent behaviors and persistent suboptimal disease control in people with diabetes mellitus are multiple.49–51 Psychological, psychosocial and behavioral interventions aimed at this group of patients in clinical trials have yielded inconsistent effects in clinical outcomes.52 This may have been due to differing or insufficient conceptualization of health behavioral theories and models in the interventions.52,53 This article attempts to provide a narrative review of psychological approaches and interventions that influence human health behaviors, specifically those that can bring about desirable behavioral adjustment or change in adults with chronic diseases in general and diabetes mellitus in particular. Sustainability of such psychological programs is also briefly discussed.
Materials and methods
We conducted searches of multiple databases (MEDLINE® via PubMed®, Embase®, Cochrane Register of Controlled trials, CINAHL [EBSCO], PsycINFO) using terms for emotion, cognition, human/health behavior, psychosocial and psychological aspects in diabetes care in English literatures, including but not limited to MeSH terms for health behaviors, emotional disorders and psychological interventions. Outcomes were not confined to objective disease control. We obtained additional articles from systematic reviews, reference lists of pertinent studies and editorials. We compiled a narrative synthesis of findings, highlighting underlying theories, mechanisms and interactions of the different and essential psychological aspects of people that might explain health behavior in chronic diseases and diabetes mellitus. It is a sequel to our earlier review on the basic aspects of health psychology in effecting behavioral change.53 Focus was given to underlying concepts and theories of human health behaviors, and was less on the approaches or delivery methods, and health care systems or policy changes. We provide a brief overview of important considerations to sustain psychological programs and services at health care facilities.
Psychological interventions for behavioral adjustments and self-management
Underlying psychological mechanisms are determining factors of health behaviors, self-efficacy, successful self-management and quality of life in people with diabetes mellitus.53–66 The extent and quality of evidence seemed to vary depending on the type of chronic disease, behavior and outcome targeted, but evidence indicates that theory-driven psychological interventions are likely to result in behavioral change and good outcomes.67,68 However, there are inconsistent effects of psychological, psychosocial and behavioral interventions on the clinical outcome parameters such as depressive symptoms, diabetes distress, self-efficacy, self-care, quality of life and disease control. This might be due to different application and conceptualization of health psychology besides differing approaches in clinical trials.58,59,69–71 In the following paragraphs, we assimilate the commonly held concepts, theories 53 and perspectives of health psychology72 in patient-centered empowerment/intervention strategies73,74 and put forth a hypothesis that reliable interventions in supporting patient’s self-management may have to start from exploring personal value systems (purpose) in life.75,76
Earlier reviews77–79 and current guidelines80,81 have recognized the essential necessity of taking into account a patient’s personal and valued goals in order to formulate personalized custom-made approaches that promote execution of health-seeking behaviors. Rasmussen et al provided an informative review of the hierarchical goals in affecting action-behavior from the perspective of self-regulation and readjustment of unattainable goal. This is important in the pursue of a valued goal without sacrificing quality of life.82 We have begun to see clinical trials evaluating life goals or preferences in people with chronic diseases.83–85 Acquiring competency in goal setting and pursuit could potentially enable a person’s successful adaptation to life with diabetes and complement health-promoting behaviors that, in turn, lead to enhanced quality of life.86 Psychological interventions at the level of the personal value system and life purpose would enhance resilience through improved understanding and health literacy, increasing motivation and ability in using existing social networks around oneself for better illness self-management.87,88 Moreover, this type of intervention is consistent with the principle of “to begin with the end in mind”,89 which will be further expounded below.
Behavioral theories and concepts
Undisputedly, knowledge and understanding of disease entities are important cognitive processes that can influence health behaviors. Some of the most commonly cited models for health behavior focus on cognitive constructs such as attitudes, beliefs and expectations (related to outcomes, self-belief or what other people might think) and examples of such models include the “Health Belief Model”,90 “Theory of Reasoned Action and Planned Behavior”,91 “Protection Motivation Theory”,92 “Social Cognitive Theory”,93 “Self-regulation”,94,95 “Relapse Prevention Model”96 and others (Table 1). In fact, all these models have cognitive and affective (emotional) components, and most recognize emotions as being the enabler and catalyst of learning in the process that leads to motivation, self-efficacy and behavioral/intentional change. Emotional constructs such as human abilities have been reported to be another important skill that is essential in social functioning, interpersonal relationships and pro-health behaviors.97,98 This emotional skill is measured as emotional intelligence improves the life and health of a person through facilitation of accurate reasoning, thought process, self- perception and interpersonal relationships. Some of the important and common concepts of psychological aspects in effecting a behavioral change had been presented in our earlier review.53
Table 1.
Key elements of the common and important health behavior concepts
| Key developer or health behavior concepts | Key elements |
|---|---|
| Gonzalez et al99 | Diabetes self-management behaviors may be influenced by three psychosocial domains: 1. Knowledge, beliefs and related cognitive constructs 2. Emotional distress and well-being 3. Behavioral skills and coping Socioeconomic status, cultural beliefs and norms are important context for the above patient-level constructs |
| Empowerment100 | Empowerment is seen as a goal and as a means (process, method, approach) that consists of or leads to an increase in the: 1. Control of an individual’s (or community’s) own health 2. Ability to control their life 3. Ability to change the world Empowerment as a goal requires knowledge, consciousness raising, skills development, self-esteem, self-confidence or self-efficacy, ability, autonomy and freedom. The idea that empowerment is an approach suggests that the individual or group should take responsibility themselves for the change process, instead of relying on health care professionals |
| Mindfulness101 | Mindfulness involves intentionally bringing one’s attention to the internal (such as bodily sensations, thoughts and emotions) and external (such as sights, smells and sounds) experiences at the present moment with an attitude of nonjudgmental acceptance (not evaluated as good or bad, true or false, healthy or sick, important or trivial). It aims to detach or decenter one’s thoughts, including statements such as “thoughts are not facts” and “I am not my thoughts.” This decentered approach is also applied to emotions and bodily sensations |
| Self-Determination Theory (autonomy)102 | The theory posits that internalization of motivations (or self-regulation) is an active activity and it occurs to satisfy three innate needs: 1. Autonomy (free will and self-rule) 2. Competence (self-efficacy) 3. Relatedness (secure and supportive interpersonal relationships) Satisfaction of these psychological needs is necessary for successful integration (development), psychological and physical health and well-being |
| Theory of Planned Behavior103 | The theory of planned behavior is an extension of the theory of reasoned action. It emphasizes cognitive processing of information and decision making in goal-directed health behaviors. Affect and emotions serve as background factors that influence intentions and behaviors. Performance of a behavior is a joint function of: 1. Intention to perform a given behavior. Determinants of intentions: • Attitude toward the behavior • Subjective norm-perceived social pressure to perform or not to perform the behavior • Perceived ease or difficulty of performing the behavior – willpower 2. Salient information or beliefs relevant to the behavior: • Behavioral beliefs • Normative beliefs • Control beliefs |
| Moser et al104 | Self-management processes in people with T2DM: 1. Off-course (short term) – in facing with health problems caused by diabetes, becoming aware, reasoning, deciding, acting and evaluating 2. Daily activities (long term) – adhering, adapting and acting routinely 3. Preventive (long term) – experiencing, learning, being cautious and putting into practice Self-management is deeply embedded in one’s unique life situation; it is perceived as an important dimension of personal autonomy which requires competency. These processes are interwoven, recurring and complex. Support from health care providers and family caregivers is necessary |
| Lorig and Holman41 | Self-management behavior of five core skills: 1. Problem solving 2. Decision making 3. Resource utilization 4. Patient–health care provider partnership 5. Taking action |
| Corbin and Strauss105 | Self-management framework of three tasks: 1. Medical management – adhering to medication and recommended lifestyle change 2. Behavioral/role management – changes in social roles or routines as an adaptation to illness 3. Emotional management |
| Social Cognitive Theory (previously known as Social Learning Theory)106 | Behavior is determined by expectancies and incentives. Expectancies consist of: 1. Expectancies about environmental cues (beliefs about how events are connected – about what leads to what) 2. Outcome expectation 3. Efficacy expectation (self-efficacy) Incentive or reinforcement is defined as the value of a particular object or outcome. Behavior is also regulated by the (possible) consequences Cognitive behavioral therapy applies the principles of social cognitive theory in changing human behaviors. Directive and action-oriented approaches are used to help a person to become aware of own dysfunctional thoughts and actions. Strategies such as self-monitoring, problem solving, goal setting, contingency management, cognitive restructuring, social support, stimulus control, stress management and relapse prevention are skills that are taught to the participants |
| Health Belief Model106,107 | Health behavior depends on simultaneous occurrence of three factors: 1. Sufficient motivation 2. Perceived threat 3. Perceived benefit and perceived barriers in following health recommendation |
| Protection Motivation Theory and Self-efficacy Theory108 | A possible general model of attitude change. The probability of a threat’s occurrence (fear appeal) initiates cognitive appraisal of its severity and believing in possession of an effective coping response (self-efficacy expectancy); both have positive effects on attitudes and intentions to adopt a recommended preventive health behavior. Four basic components: 1. Outcome expectancy – current behavior 2. Outcome expectancy – alternative behavior 3. Self-efficacy (for the alternative behavior) 4. The relative value of the different sets of outcomes Two decision-making strategies that people use when confronted with a fear appeal: 1. A precaution strategy (a response is not necessary) 2. A hyperdefensiveness strategy (the danger cannot be avoided) A shift to positive emphasis/outcomes was argued to be possible with little modification of the basic components of the theory |
Abbreviation: T2DM, type 2 diabetes mellitus.
The psychological framework
It is clear from the preceding discussion on health behavior theories and models that health behavioral adjustment or change will involve modifications of personal value systems, cognition and emotions. A personal value system consists of valued goals that provide a purpose for living,109 which, consciously or unconsciously, are the strength and essence of living; losing these may end up giving up on living and life. When valued goals are congruent with healthful belief systems in terms of knowledge and attitudes toward an illness, these can help to frame or reframe nonthreatening illness perception.110,111 Consequently, a new behavior can be formed or an existing behavior can be successfully maintained through proactive coping, physiological adaptation and psychological habituation, leading to resilient health-promoting behaviors that transcend the gene–environmental interdependence throughout the lifespan.112
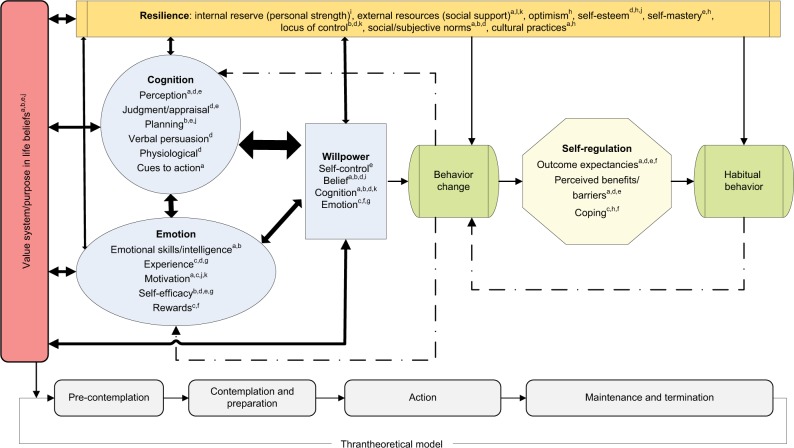
Value systems and the purpose of life have always been related to religious faith or spirituality110 and their effects on physical and psychological health are believed to be the result of healthier behaviors as required in the religious teachings, greater social support and having hope that rests on the ultimate or absolute being.113–115 Given the underlying importance of value systems and the sense of purpose in life, and the importance of cognition and emotion in human behaviors, the assimilation of these concepts produces a value-based, emotion-focused educational psychological framework in effecting behavioral change (Figure 1). This psychological framework also maps well with the stages of change proposed in the transtheoretical model of health behavior change:116 pre-contemplation ↔ cognition; contemplation and preparation ↔ emotion/motivation; action ↔ self-efficacy; maintenance and termination ↔ resilience/value.
Figure 1.
Value–cognition–emotion psychological framework.
Note: aHealth Belief Model; bTheory of Reasoned Action and Planned Behavior; cProtection Motivation Theory; dSocial Cognitive Theory; eSelf-regulation; fRelapse Prevention Model; gSelf-efficacy; hResilience; iValue System; jWillpower; kSelf-Determination Theory.
Possible psychological mechanisms of the value-based, emotion-focused education
The first step in exploring a person’s value system is to appeal to the motives for change in regard to a variety of health behaviors. Invariably, it demands a verdict from the person on whether a new or current behavior is either “right” or “wrong”, and thus warranting maintenance or change. An awareness of this value system by both the person and the treating physician will provide a clear perspective and direction in clinical consultation, both qualitatively and quantitatively, of what the person needs to know, to change, to do and to maintain. An assessment of a person’s pursuit of health as a goal in relation to other goals of life will be helpful in gauging willingness to expend effort toward the same. Considering good health as a prerequisite and foundation to achieve other purposes in life would greatly facilitate learning, health literacy and decision making (cognition),49,117 motivation (emotion) and maintenance of healthy lifestyles (self-efficacy), even in the face of life events and challenges (resilience).118 Thus, the awareness of a person’s values and belief systems with respect to his/her life purpose is important for three specific reasons: 1) to modify perception of the immediate environment; 2) to identify modifiable unhealthy coping styles such as turning to alcohol, increase smoking and so on and 3) to identify the unique internal and external resources available for improving the quality of life and disease control.119
This type of psychological intervention may be helpful for people who say “It is not that I don’t know what and how to take care of myself but it is just that I don’t want to do it” (value problem), compared to people who say “It is not that I don’t know what and how to take care of myself but I’m just not able/can’t manage to do it” (emotion/motivation problem) or “I don’t know what and how to take care of myself ” (cognition problem). A mixture of these problems, rather than discrete characterization of values problems, emotion/motivation problems or cognition problems, is believed to be present in most people. Despite this, psychological interventions that address an individual’s unique value system separately, besides exploring the possible cause(s) of resistance to pro-health behaviors could help the person to overcome the psychological barriers to healthful behaviors, especially when facing with multiple behavioral choices. This form of intervention is similar to the motivational interviewing as proposed by Hettema et al.120 The use of motivational interviewing to induce health-related behavior change is well documented,121,122 and has at its basis resolving cognitive dissonance between one’s values and one’s behaviors, such that this dissonance would provide a motivating force to overcome the inertia toward pro-health behaviors. The stronger the awareness of the dissonance, the more likely the person will resolve the dissonance by changing their behaviors to be congruent to their unique values and purpose, or vice versa. This step would help people to come to terms with, and be informed of, their behavioral choices. In some instances, the presence of multiple valued goals in the person may be conflicting to each other such that they compete for limited inner reserves, and this could minimize the motivation toward a certain desired behavior. Thus, alignment, synchronization and/or conglomeration of these personal values are necessary before an effective motivation could be generated. Since a personal value is personal and subjected to the demands of immediate circumstances, it is possible that this personal value system is not a pro-healthy behavior at times,50 or it may not agree with another person’s wants and wishes. However, a personal value that agrees with the universal “good” and “bad” health behaviors prevails and presides in long term.
On the subject of emotions being a driving force to modify behavior, emotional training could provide the necessary emotional skills for people to recognize the emotional information in daily events, and thus gaining insights and energy to effectively managing emotions in themselves and in others toward facilitating productive relationships with self and others, and leading to healthful behaviors. Technical knowledge and skills would then be more effectively learned, retained and applied in the form of new behaviors. The preceding discussion suggests why interventions that work at the cognitive level alone (e.g., educational in nature) were often inadequate for truly forming or altering a behavior, and lesser so in maintaining the required behavior.123 Even an intervention at both cognitive and emotional levels may initiate a change in behavior, albeit transiently. Based on the review of human health behavioral theories and concepts, we believe that people who have come to terms with their own values/life purpose would have a more profound understanding about themselves, a meaningful feeling about life and a stronger intention to realize their valued goals in life. This could potentially lead to a greater insight into one’s value system, a realignment of cognition, emotion and a new behavior consistent with the realized value system. From another perspective, equipped with sufficient motivation (emotional intelligence) and appropriate knowledge about what and how to behave, an adjustment or a change would lead to a new behavior. This is believed to be a real and meaningful change in a person as compared to the psychological interventions of health-related nudges124 and behavioral economics125,126 that modify the environmental cues and financial incentives to exert or induce a behavioral change, respectively. Regular reinforcement of the upheld values, emotional skills and knowledge is, however, necessary for continuity of the desired behaviors. From a social support perspective, involving the person’s spouse or significant others increases the effectiveness of an intervention by serving as an informed companion to support and remind the person.127 Thus, initiating a lasting behavior (resilience and self-efficacy)53 is more effective when its foundational elements, namely, the personal value system/purpose in life53 is assessed and addressed, surpassing the effects of the personal past achievement in social and occupational domains.118
Service and program sustainability
Having psychological and behavioral change services for people with chronic diseases such as diabetes mellitus requires efforts to sustain the services. The sheer burden of diabetes mellitus and its related comorbidities and complications, disease chronicity and treatment complexity demand a sustained support for people with diabetes mellitus. Moreover, a person with diabetes mellitus visits their primary care provider on average four times per year, with an average consultation taking about 20 minutes.128 This equates to people with diabetes mellitus spending <1% of their lifetime with their doctors and the health care team. However, the successful implementation of such a service requires cooperation on the part of participants to attend the scheduled sessions.129 To help in this aspect, the program could be individualized and delivered in its separate simpler sufficient parts to certain types of people, depending on their particular needs such as knowledge, emotional skills or goal setting, or learning about providing social supports by the significant others.80 This would make the program more accessible and feasible to more people and their significant others. Additionally, ongoing feedback from the participants and input from the community that is served by the clinics would help to make the program more person centered, culturally relevant, with participant-identified needs, as well as supported by the family of the participants and the local community.80
At the clinic level, limitations in terms of logistics and human resources may be barriers to the sustainability of such services. Many smaller or resource-constrained health facilities may face challenges to conduct programs due to facility or staff constraints. Institutional change may also be required to have a functional, and even a dedicated unit, such as a Noncommunicable Disease Unit, staffed by at least one diabetes educator/nurse and one doctor. Service sustainability can also be gained from seeking ongoing input from valued staff and health care providers. This may promote quality and mutual understanding, and enhance participants’ referral and utilization. Better organizational or administrative arrangements, such as defining and documenting a mission statement and goals on providing effective programs, will assist in the service continued support and update.80
Higher-level stakeholders’ involvement in ongoing planning processes will also improve sustainability of the service through sharing of ideas, quality improvement, measurable outcomes, achievement and positive feedback from the community.80 It is equally important that the administration validates the efforts of their staff and acknowledge appropriate recognition of such services.130 Consequently, nurses and doctors conducting the program can experience lesser or no clashes with other clinic duties or with other colleagues. To further improve the sustainability of the service at the clinic, a quality coordinator can be designated to ensure implementation of the program and oversee the overall services including evidence-based practice, service design, evaluation and continuous quality improvement.130
Conclusion
Approaching people with chronic diseases such as diabetes mellitus from the vantage point of their personal value systems and emotional skills besides knowledge does not trade off medical professionalism and commitment to health advancement. On the contrary, this approach is in agreement with the principles of evidence-based medicine, where the personal values and preference of patients are recognized in the formulation of their own treatment plan131 and the dynamic definition of health132 as “the ability to adapt and self-manage in the face of social, physical, and emotional challenges.”
It may be evident from this review that habitual healthful behaviors arise from successful self-regulation and resilience. Successful forming of a new behavior depends on a strong willpower that is fueled by adequate cognizance (understanding and reasoning) and emotional intelligence (motivation and self-efficacy). These become effective when the behavior is highly valued and in line with the purpose of life of the person. Interventional programs and services should consider including all the components in the value–cognition–emotion psychological framework, probably in different appropriate proportions, through culturally appropriate manners in different health care settings, and for people at different illness stages and phases of life. Outcomes and targets of psychological interventions should primarily be psychological measurements and health behaviors and secondarily be the biomarkers of disease control as measured by the laboratory. Both are important and supportive of the notions of holistic care and biopsychosocial models of medicine.
Acknowledgments
We acknowledge Prof Dr Guy EHM Rutten and Asst Prof Dr Rimke C Vos for reading and commenting on some parts of the article. We thank Universiti Putra Malaysia and the Ministry of Higher Education Malaysia for sponsoring the PhD study of BHC, which made possible this work.
Footnotes
Author contributions
BHC wrote the first draft. All authors contributed toward data analysis, further drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Chan JC, Luk AO. Diabetes: a cinderella subject we can’t afford to ignore. PLoS Med. 2016;13(7):e1002068. doi: 10.1371/journal.pmed.1002068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2016 Causes of Death Collaborators Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2015 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94(3):311–321. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 5.International Diabetes Federation . IDF Diabetes Atlas. Brussels, Belgium: International Diabetes Federation; 2015. [Google Scholar]
- 6.Jermendy G. Vascular memory: can we broaden the concept of the metabolic memory? Cardiovasc Diabetol. 2012;11(1):44. doi: 10.1186/1475-2840-11-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Konig M, Lamos EM, Stein SA, Davis SN. An insight into the recent diabetes trials: what is the best approach to prevent macrovascular and microvascular complications? Curr Diabetes Rev. 2013;9(5):371–381. doi: 10.2174/15733998113099990077. [DOI] [PubMed] [Google Scholar]
- 8.Kim D, Kubzansky LD, Baccarelli A, et al. Psychological factors and DNA methylation of genes related to immune/inflammatory system markers: the VA Normative Aging Study. BMJ Open. 2016;6(1):e009790. doi: 10.1136/bmjopen-2015-009790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laake JP, Stahl D, Amiel SA, et al. The association between depressive symptoms and systemic inflammation in people with type 2 diabetes: findings from the South London Diabetes Study. Diabetes Care. 2014;37(8):2186–2192. doi: 10.2337/dc13-2522. [DOI] [PubMed] [Google Scholar]
- 10.Dalsgaard EM, Vestergaard M, Skriver MV, et al. Psychological distress, cardiovascular complications and mortality among people with screen-detected type 2 diabetes: follow-up of the ADDITION-Denmark trial. Diabetologia. 2014;57(4):710–717. doi: 10.1007/s00125-014-3165-4. [DOI] [PubMed] [Google Scholar]
- 11.Stamler J, Vaccaro O, Neaton JD, Wentworth D. Diabetes, other risk factors, and 12-year cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care. 1993;16(2):434–444. doi: 10.2337/diacare.16.2.434. [DOI] [PubMed] [Google Scholar]
- 12.Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348(5):383–393. doi: 10.1056/NEJMoa021778. [DOI] [PubMed] [Google Scholar]
- 13.Dailey G. Early and intensive therapy for management of hyperglycemia and cardiovascular risk factors in patients with type 2 diabetes. Clin Ther. 2011;33(6):665–678. doi: 10.1016/j.clinthera.2011.04.025. [DOI] [PubMed] [Google Scholar]
- 14.Goto A, Arah OA, Goto M, Terauchi Y, Noda M. Severe hypoglycaemia and cardiovascular disease: systematic review and meta-analysis with bias analysis. BMJ. 2013;347:f4533. doi: 10.1136/bmj.f4533. [DOI] [PubMed] [Google Scholar]
- 15.Boussageon R, Bejan-Angoulvant T, Saadatian-Elahi M, et al. Effect of intensive glucose lowering treatment on all cause mortality, cardiovascular death, and microvascular events in type 2 diabetes: meta-analysis of randomised controlled trials. BMJ. 2011;343:d4169. doi: 10.1136/bmj.d4169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu H, Xu MJ, Zou DJ, Han QJ, Hu X. Intensive glycemic control and macrovascular events in type 2 diabetes mellitus: a meta-analysis of randomized controlled trials. Chin Med J (Engl) 2010;123(20):2908–2913. [PubMed] [Google Scholar]
- 17.DeJean D, Giacomini M, Vanstone M, Brundisini F. Patient experiences of depression and anxiety with chronic disease: a systematic review and qualitative meta-synthesis. Ont Health Technol Assess Ser. 2013;13(16):1–33. [PMC free article] [PubMed] [Google Scholar]
- 18.Nicolucci A, Kovacs Burns K, Holt RI, et al. DAWN2 Study Group Diabetes Attitudes, Wishes and Needs second study (DAWN2): cross-national benchmarking of diabetes-related psychosocial outcomes for people with diabetes. Diabet Med. 2013;30(7):767–777. doi: 10.1111/dme.12245. [DOI] [PubMed] [Google Scholar]
- 19.Rawshani A, Rawshani A, Franzén S, et al. Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med. 2017;376(15):1407–1418. doi: 10.1056/NEJMoa1608664. [DOI] [PubMed] [Google Scholar]
- 20.Herman WH, Ye W, Griffin SJ, et al. Early detection and treatment of type 2 diabetes reduce cardiovascular morbidity and mortality: a simulation of the results of the Anglo-Danish-Dutch Study of Intensive Treatment in People With Screen-Detected Diabetes in Primary Care (ADDITION-Europe) Diabetes Care. 2015;38(8):1449–1455. doi: 10.2337/dc14-2459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gregg EW, Li Y, Wang J, et al. Changes in diabetes-related complications in the United States, 1990–2010. N Engl J Med. 2014;370(16):1514–1523. doi: 10.1056/NEJMoa1310799. [DOI] [PubMed] [Google Scholar]
- 22.Booth GL, Kapral MK, Fung K, Tu JV. Recent trends in cardiovascular complications among men and women with and without diabetes. Diabetes Care. 2006;29(1):32–37. doi: 10.2337/diacare.29.01.06.dc05-0776. [DOI] [PubMed] [Google Scholar]
- 23.Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. Lancet. 2017;389(10085):2239–2251. doi: 10.1016/S0140-6736(17)30058-2. [DOI] [PubMed] [Google Scholar]
- 24.Naranjo D, Tanenbaum ML, Iturralde E, Hood KK. Diabetes technology: uptake, outcomes, barriers, and the intersection with distress. J Diabetes Sci Technol. 2016;10(4):852–858. doi: 10.1177/1932296816650900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hadjiconstantinou M, Byrne J, Bodicoat DH, et al. Do web-based interventions improve well-being in type 2 diabetes? A systematic review and meta-analysis. J Med Internet Res. 2016;18(10):e270. doi: 10.2196/jmir.5991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pal K, Eastwood SV, Michie S, et al. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2013;3:Cd008776. doi: 10.1002/14651858.CD008776.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lutfey KE, Wishner WJ. Beyond “compliance” is “adherence”. Improving the prospect of diabetes care. Diabetes Care. 1999;22(4):635–639. doi: 10.2337/diacare.22.4.635. [DOI] [PubMed] [Google Scholar]
- 28.Messina J, Campbell S, Morris R, Eyles E, Sanders C. A narrative systematic review of factors affecting diabetes prevention in primary care settings. PLoS One. 2017;12(5):e0177699. doi: 10.1371/journal.pone.0177699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cramer JA, Benedict A, Muszbek N, Keskinaslan A, Khan ZM. The significance of compliance and persistence in the treatment of diabetes, hypertension and dyslipidaemia: a review. Int J Clin Pract. 2008;62(1):76–87. doi: 10.1111/j.1742-1241.2007.01630.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aghili R, Polonsky WH, Valojerdi AE, et al. Type 2 diabetes: model of factors associated with glycemic control. Can J Diabetes. 2016;40(5):424–430. doi: 10.1016/j.jcjd.2016.02.014. [DOI] [PubMed] [Google Scholar]
- 31.Edelman SV, Polonsky WH. Type 2 diabetes in the real world: the elusive nature of glycemic control. Diabetes Care. 2017;40(11):1425–1432. doi: 10.2337/dc16-1974. [DOI] [PubMed] [Google Scholar]
- 32.Carlin A, Perchoux C, Puggina A, et al. A life course examination of the physical environmental determinants of physical activity behaviour: a “Determinants of Diet and Physical Activity” (DEDIPAC) umbrella systematic literature review. PLoS One. 2017;12(8):e0182083. doi: 10.1371/journal.pone.0182083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Coleman MT, Pasternak RH. Effective strategies for behavior change. Prim Care. 2012;39(2):281–305. doi: 10.1016/j.pop.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 34.Hu FB. Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care. 2011;34(6):1249–1257. doi: 10.2337/dc11-0442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jacob S, Serrano-Gil M. Engaging and empowering patients to manage their type 2 diabetes, Part II: initiatives for success. Adv Ther. 2010;27(10):665–680. doi: 10.1007/s12325-010-0071-0. [DOI] [PubMed] [Google Scholar]
- 36.Dwamena F, Holmes-Rovner M, Gaulden CM, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev. 2012;12:CD003267. doi: 10.1002/14651858.CD003267.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Renders CM, Valk GD, Griffin S, Wagner EH, Eijk JT, Assendelft WJ. Interventions to improve the management of diabetes mellitus in primary care, outpatient and community settings. Cochrane Database Syst Rev. 2000;(4):CD001481. doi: 10.1002/14651858.CD001481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alden DL, Friend J, Lee PY, et al. Who decides: me or we? Family involvement in medical decision making in Eastern and Western Countries. Med Decis Making. 2018;38(1):14–25. doi: 10.1177/0272989X17715628. [DOI] [PubMed] [Google Scholar]
- 39.Low LL, Tong SF, Low WY. Selection of treatment strategies among patients with type 2 diabetes mellitus in Malaysia: a grounded theory approach. PLoS One. 2016;11(1):e0147127. doi: 10.1371/journal.pone.0147127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schulman-Green D, Jaser S, Martin F, et al. Processes of self-management in chronic illness. J Nurs Scholarsh. 2012;44(2):136–144. doi: 10.1111/j.1547-5069.2012.01444.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 42.Cortis C, Puggina A, Pesce C, et al. Psychological determinants of physical activity across the life course: a “DEterminants of DIet and Physical Activity” (DEDIPAC) umbrella systematic literature review. PLoS One. 2017;12(8):e0182709. doi: 10.1371/journal.pone.0182709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Broadbent E, Wilkes C, Koschwanez H, Weinman J, Norton S, Petrie KJ. A systematic review and meta-analysis of the brief illness perception questionnaire. Psychol Health. 2015;30(11):1361–1385. doi: 10.1080/08870446.2015.1070851. [DOI] [PubMed] [Google Scholar]
- 44.Tuerk PW, Mueller M, Egede LE. Estimating physician effects on glycemic control in the treatment of diabetes: methods, effects sizes, and implications for treatment policy. Diabetes Care. 2008;31(5):869–873. doi: 10.2337/dc07-1662. [DOI] [PubMed] [Google Scholar]
- 45.DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42(3):200–209. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- 46.Feisul MI, Azmi SE, editors. National Diabetes Registry Report, 2009–2012. Vol. 1. Kuala Lumpur: Non-Communicable Disease Section, Disease Control Division, Department of Public Health; 2013. [Google Scholar]
- 47.Guðbjörnsdóttir S, Eliasson B, Cederholm J, Zethelius B, Ann-Marie S, Samuelsson P. Swedish National Diabetes Register Annual Report 2013. Gothenburg, Sweden: Centre of Registers, Region Västra Götaland; 2014. [Google Scholar]
- 48.National Diabetes Audit . National Diabetes Audit – 2015–2016: Report 1, Care Processes and Treatment Targets. England and Wales: Healthcare Quality Improvement Partnership, National Diabetes Audit; 2017. [Google Scholar]
- 49.Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Barriers to diabetes management: patient and provider factors. Diabetes Res Clin Pract. 2011;93(1):1–9. doi: 10.1016/j.diabres.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 50.Kodolitsch YV, Bernhardt AM, Kölbel T, Detter C, Reichenspurner H, Debus ES. Maximizing therapeutic success: the key concepts of individualized medical strategy (IMS) Cogent Med. 2015;2:1109742. [Google Scholar]
- 51.Luo X, Liu T, Yuan X, et al. Factors influencing self-management in Chinese adults with type 2 diabetes: a systematic review and meta-analysis. Int J Environ Res Public Health. 2015;12(9):11304–11327. doi: 10.3390/ijerph120911304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Patnode CD, Evans CV, Senger CA, Redmond N, Lin JS. Behavioral Counseling to Promote a Healthful Diet and Physical Activity for Cardiovascular Disease Prevention in Adults Without Known Cardiovascular Disease Risk Factors: Updated Systematic Review for the US Preventive Services Task Force. Rockville, MD, USA: Agency for Healthcare Research and Quality; 2017. US. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews. [PubMed] [Google Scholar]
- 53.Chew BH, Shariff-Ghazali S, Fernandez A. Psychological aspects of diabetes care: effecting behavioral change in patients. World J Diabetes. 2014;5(6):796–808. doi: 10.4239/wjd.v5.i6.796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Powers MA, Bardsley J, Cypress M, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Care. 2015;38(7):1372–1382. doi: 10.2337/dc15-0730. [DOI] [PubMed] [Google Scholar]
- 55.Sturt J, Taylor H, Docherty A, Dale J, Louise T. A psychological approach to providing self-management education for people with type 2 diabetes: the diabetes manual. BMC Fam Pract. 2006;7(1):70. doi: 10.1186/1471-2296-7-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Robertson SM, Stanley MA, Cully JA, Naik AD. Positive emotional health and diabetes care: concepts, measurement, and clinical implications. Psychosomatics. 2012;53(1):1–12. doi: 10.1016/j.psym.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 57.Robertson SM, Amspoker AB, Cully JA, Ross EL, Naik AD. Affective symptoms and change in diabetes self-efficacy and glycaemic control. Diabet Med. 2013;30(5):e189–e196. doi: 10.1111/dme.12146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Harkness E, Macdonald W, Valderas J, Coventry P, Gask L, Bower P. Identifying psychosocial interventions that improve both physical and mental health in patients with diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33(4):926–930. doi: 10.2337/dc09-1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Baumeister H, Hutter N, Bengel J. Psychological and pharmacological interventions for depression in patients with diabetes mellitus and depression. Cochrane Database Syst Rev. 2012;12:CD008381. doi: 10.1002/14651858.CD008381.pub2. [DOI] [PubMed] [Google Scholar]
- 60.Brierley S, Eiser C, Johnson B, Young V, Heller S. Psychological interventions for young people with type 1 diabetes: a metaanalysis. Diabet Med. 2013;30:177–178. doi: 10.1111/j.1464-5491.2012.03721.x. [DOI] [PubMed] [Google Scholar]
- 61.Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005;(2):CD003417. doi: 10.1002/14651858.CD003417.pub2. [DOI] [PubMed] [Google Scholar]
- 62.Duke SA, Colagiuri S, Colagiuri R. Individual patient education for people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2009;(1):CD005268. doi: 10.1002/14651858.CD005268.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Franek J. Self-management support interventions for persons with chronic disease: an evidence-based analysis. Ont Health Technol Assess Ser. 2013;13(9):1–60. [PMC free article] [PubMed] [Google Scholar]
- 64.Pal K, Eastwood SV, Michie S, et al. Computer-based interventions to improve self-management in adults with type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2014;37(6):1759–1766. doi: 10.2337/dc13-1386. [DOI] [PubMed] [Google Scholar]
- 65.van Dam HA, van der Horst FG, Knoops L, Ryckman RM, Crebolder HF, van den Borne BH. Social support in diabetes: a systematic review of controlled intervention studies. Patient Educ Couns. 2005;59(1):1–12. doi: 10.1016/j.pec.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 66.Winkley K, Ismail K, Landau S, Eisler I. Psychological interventions to improve glycaemic control in patients with type 1 diabetes: systematic review and meta-analysis of randomised controlled trials. BMJ. 2006;333(7558):65. doi: 10.1136/bmj.38874.652569.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhao FF, Suhonen R, Koskinen S, Leino-Kilpi H. Theory-based self-management educational interventions on patients with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. J Adv Nurs. 2017;73(4):812–833. doi: 10.1111/jan.13163. [DOI] [PubMed] [Google Scholar]
- 68.Barley E, Lawson V. Using health psychology to help patients: theories of behaviour change. Br J Nurs. 2016;25(16):924–927. doi: 10.12968/bjon.2016.25.16.924. [DOI] [PubMed] [Google Scholar]
- 69.Ismail K, Winkley K, Rabe-Hesketh S. Systematic review and meta-analysis of randomised controlled trials of psychological interventions to improve glycaemic control in patients with type 2 diabetes. Lancet. 2004;363(9421):1589–1597. doi: 10.1016/S0140-6736(04)16202-8. [DOI] [PubMed] [Google Scholar]
- 70.Sturt J, Dennick K, Hessler D, Hunter BM, Oliver J, Fisher L. Effective interventions for reducing diabetes distress: systematic review and meta-analysis. Int Diab Nurs. 2015;12(2):40–55. [Google Scholar]
- 71.Chew BH, Vos RC, Metzendorf MI, Scholten RJ, Rutten GE. Psychological interventions for diabetes-related distress in adults with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2017;9:CD011469. doi: 10.1002/14651858.CD011469.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Riekert KA, Ockene JK, Pbert L, editors. The Handbook of Health Behavior Change. 4th ed. New York: Springer Publishing Company; 2013. [Google Scholar]
- 73.Serrano-Gil M, Jacob S. Engaging and empowering patients to manage their type 2 diabetes, part I: a knowledge, attitude, and practice gap? Adv Ther. 2010;27(6):321–333. doi: 10.1007/s12325-010-0034-5. [DOI] [PubMed] [Google Scholar]
- 74.Funnell MM, Tang TS, Anderson RM. From DSME to DSMS: developing empowerment-based diabetes self-management support. Diab Spectr. 2007;20(4):221–226. [Google Scholar]
- 75.Lynch CP, Hernandez-Tejada MA, Strom JL, Egede LE. Association between spirituality and depression in adults with type 2 diabetes. Diabetes Educ. 2012;38(3):427–435. doi: 10.1177/0145721712440335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rasmussen NH, Smith SA, Maxson JA, et al. Association of HbA1c with emotion regulation, intolerance of uncertainty, and purpose in life in type 2 diabetes mellitus. Prim Care Diabetes. 2013;7(3):213–221. doi: 10.1016/j.pcd.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 77.Grimaldi A. How to help the patient motivate himself? Diabetes Metab. 2012;38(Suppl 3):S59–S64. doi: 10.1016/S1262-3636(12)71536-7. [DOI] [PubMed] [Google Scholar]
- 78.Ahola AJ, Groop PH. Barriers to self-management of diabetes. Diabet Med. 2013;30(4):413–420. doi: 10.1111/dme.12105. [DOI] [PubMed] [Google Scholar]
- 79.Rothman AJ. Initiatives to motivate change: a review of theory and practice and their implications for older adults. In: Carstensen LL, Hartel CR, editors. When I’m 64. Washington, DC, USA: National Academies Press; 2006. [PubMed] [Google Scholar]
- 80.Beck J, Greenwood DA, Blanton L, et al. National standards for diabetes self-management education and support. Diabetes Care. 2017;2017;40(10):1409–1419. doi: 10.2337/dci17-0025. [DOI] [PubMed] [Google Scholar]
- 81.Scottish Intercollegiate Guidelines Network . Management of Diabetes: A National Clinical Guideline. Guideline No 116. Edinburgh: Healthcare Improvement Scotland; 2010. [Google Scholar]
- 82.Rasmussen HN, Wrosch C, Scheier MF, Carver CS. Self-regulation processes and health: the importance of optimism and goal adjustment. J Pers. 2006;74(6):1721–1747. doi: 10.1111/j.1467-6494.2006.00426.x. [DOI] [PubMed] [Google Scholar]
- 83.Arends RY, Bode C, Taal E, Van de Laar MA. The role of goal management for successful adaptation to arthritis. Patient Educ Couns. 2013;93(1):130–138. doi: 10.1016/j.pec.2013.04.022. [DOI] [PubMed] [Google Scholar]
- 84.Zhang Y, Tikkinen KA, Agoritsas T, et al. Patients’ values and preferences of the expected efficacy of hip arthroscopy for osteoarthritis: a protocol for a multinational structured interview-based study combined with a randomised survey on the optimal amount of information to elicit preferences. BMJ Open. 2014;4(10):e005536. doi: 10.1136/bmjopen-2014-005536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chew BH, Vos RC, Shariff Ghazali S, et al. The effectiveness of a value-based EMOtion-cognition-focused educational programme to reduce diabetes-related distress in Malay adults with type 2 diabetes (VEMOFIT): study protocol for a cluster randomised controlled trial. BMC Endocr Disord. 2017;17(1):22. doi: 10.1186/s12902-017-0172-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Stuifbergen AK, Morris M, Jung JH, Pierini D, Morgan S. Benefits of wellness interventions for persons with chronic and disabling conditions: a review of the evidence. Disabil Health J. 2010;3(3):133–145. doi: 10.1016/j.dhjo.2009.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bailey SC, Brega AG, Crutchfield TM, et al. Update on health literacy and diabetes. Diabetes Educ. 2014;40(5):581–604. doi: 10.1177/0145721714540220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cavanaugh K, Wallston KA, Gebretsadik T, et al. Addressing literacy and numeracy to improve diabetes care: two randomized controlled trials. Diabetes Care. 2009;32(12):2149–2155. doi: 10.2337/dc09-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Covey SR. The 7 Habits of Highly Effective People. New York: Simon & Schuster; 2013. [Google Scholar]
- 90.Rosenstock IM. Why people use health services. Milbank Mem Fund Q. 1966;44((3):Suppl):94–127. [PubMed] [Google Scholar]
- 91.Ajzen I. The theory of planned behaviour: reactions and reflections. Psychol Health. 2011;26(9):1113–1127. doi: 10.1080/08870446.2011.613995. [DOI] [PubMed] [Google Scholar]
- 92.Rogers RW. A protection motivation theory of fear appeals and attitude change1. J Psychol. 1975;91(1):93–114. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- 93.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. 2001;52(1):1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 94.Clark NM, Gong M, Kaciroti N. A model of self-regulation for control of chronic disease. Health Educ Behav. 2001;28(6):769–782. doi: 10.1177/109019810102800608. [DOI] [PubMed] [Google Scholar]
- 95.de Ridder Denise, de Wit John., editors. Self-Regulation in Health Behavior. West Sussex, England: John Wiley & Sons; 2006. [Google Scholar]
- 96.Hendershot CS, Witkiewitz K, George WH, Marlatt GA. Relapse prevention for addictive behaviors. Subst Abuse Treat Prev Policy. 2011;6:17. doi: 10.1186/1747-597X-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mayer JD, Roberts RD, Barsade SG. Human abilities: emotional intelligence. Annu Rev Psychol. 2007;59(1):507–536. doi: 10.1146/annurev.psych.59.103006.093646. [DOI] [PubMed] [Google Scholar]
- 98.Abraham R. Emotional competence as antecedent to performance: a contingency framework. Genet Soc Gen Psychol Monogr. 2004;130(2):117–143. doi: 10.3200/MONO.130.2.117-145. [DOI] [PubMed] [Google Scholar]
- 99.Gonzalez JS, Tanenbaum ML, Commissariat PV. Psychosocial factors in medication adherence and diabetes self-management: implications for research and practice. Am Psychol. 2016;71(7):539–551. doi: 10.1037/a0040388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tengland PA. Empowerment: a conceptual discussion. Health Care Anal. 2008;16(2):77–96. doi: 10.1007/s10728-007-0067-3. [DOI] [PubMed] [Google Scholar]
- 101.Baer RA. Mindfulness training as a clinical intervention: a conceptual and empirical review. Clin Psychol Science Pract. 2003;10(2):125–143. [Google Scholar]
- 102.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 103.Ajzen I. The theory of planned behavior. Theories Cogn Self Regul. 1991;50(2):179–211. [Google Scholar]
- 104.Moser A, van der Bruggen H, Widdershoven G, Spreeuwenberg C. Self-management of type 2 diabetes mellitus: a qualitative investigation from the perspective of participants in a nurse-led, shared-care programme in the Netherlands. BMC Public Health. 2008;8:91. doi: 10.1186/1471-2458-8-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Corbin JM, Strauss A. Unending Work and Care: Managing Chronic Illness at Home (Jossey Bass Social and Behavioral Science Series) San Francisco, CA: Jossey-Bass; 1988. [Google Scholar]
- 106.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. 1988;15(2):175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 107.Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 108.Maddux JE, Rogers RW. Protection motivation and self-efficacy: a revised theory of fear appeals and attitude change. J Exp Soc Psychol. 1983;19(5):469–479. [Google Scholar]
- 109.Scheier MF, Wrosch C, Baum A, et al. The life engagement test: assessing purpose in life. J Behav Med. 2006;29(3):291–298. doi: 10.1007/s10865-005-9044-1. [DOI] [PubMed] [Google Scholar]
- 110.Myers DG. The funds, friends, and faith of happy people. Am Psychol. 2000;55(1):56–67. doi: 10.1037//0003-066x.55.1.56. [DOI] [PubMed] [Google Scholar]
- 111.Petrie KJ, Jago LA, Devcich DA. The role of illness perceptions in patients with medical conditions. Curr Opin Psychiatry. 2007;20(2):163–167. doi: 10.1097/YCO.0b013e328014a871. [DOI] [PubMed] [Google Scholar]
- 112.Aspinwall LG. The psychology of future-oriented thinking: from achievement to proactive coping, adaptation, and aging. Motiv Emotion. 2005;29(4):203–235. [Google Scholar]
- 113.McCullough ME, Willoughby BL. Religion, self-regulation, and self-control: associations, explanations, and implications. Psychol Bull. 2009;135(1):69–93. doi: 10.1037/a0014213. [DOI] [PubMed] [Google Scholar]
- 114.Newlin K, Melkus GD, Tappen R, Chyun D, Koenig HG. Relationships of religion and spirituality to glycemic control in Black women with type 2 diabetes. Nurs Res. 2008;57(5):331–339. doi: 10.1097/01.NNR.0000313497.10154.66. [DOI] [PubMed] [Google Scholar]
- 115.Okun MA, Stock WA. Correlates and components of subjective well-being among the elderly. J Appl Gerontol. 1987;6(1):95–112. [Google Scholar]
- 116.Prochaska JO, DiClemente CC. Self change processes, self efficacy and decisional balance across five stages of smoking cessation. Prog Clin Biol Res. 1984;156:131–140. [PubMed] [Google Scholar]
- 117.Lee YK, Low WY, Ng CJ. Exploring patient values in medical decision making: a qualitative study. PLoS One. 2013;8(11):e80051. doi: 10.1371/journal.pone.0080051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Mertens VC, Bosma H, Groffen DA, van Eijk JT. Good friends, high income or resilience? What matters most for elderly patients? Eur J Public Health. 2012;22(5):666–671. doi: 10.1093/eurpub/ckr104. [DOI] [PubMed] [Google Scholar]
- 119.Rose M, Fliege H, Hildebrandt M, Schirop T, Klapp BF. The network of psychological variables in patients with diabetes and their importance for quality of life and metabolic control. Diabetes Care. 2002;25(1):35–42. doi: 10.2337/diacare.25.1.35. [DOI] [PubMed] [Google Scholar]
- 120.Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- 121.Rubak S, Sandbæk A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55(513):305–312. [PMC free article] [PubMed] [Google Scholar]
- 122.Treasure J. Motivational interviewing. Adv Psychiatr Treat. 2004;10(5):331–337. [Google Scholar]
- 123.Sperl-Hillen J, Beaton S, Fernandes O, et al. Are benefits from diabetes self-management education sustained? Am J Manag Care. 2013;19(2):104–112. [PubMed] [Google Scholar]
- 124.Marteau TM. Changing minds about changing behaviour. Lancet. 2018;391(10116):116–117. doi: 10.1016/S0140-6736(17)33324-X. [DOI] [PubMed] [Google Scholar]
- 125.Volpp KG, Pauly MV, Loewenstein G, Bangsberg D. P4P4P: an agenda for research on pay-for-performance for patients. Health Aff (Mill-wood) 2009;28(1):206–214. doi: 10.1377/hlthaff.28.1.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Reed DD, Niileksela CR, Kaplan BA. Behavioral economics: a tutorial for behavior analysts in practice. Behav Anal Pract. 2013;6(1):34–54. doi: 10.1007/BF03391790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Rintala TM, Jaatinen P, Paavilainen E, Astedt-Kurki P. Interrelation between adult persons with diabetes and their family: a systematic review of the literature. J Fam Nurs. 2013;19(1):3–28. doi: 10.1177/1074840712471899. [DOI] [PubMed] [Google Scholar]
- 128.Ahmad BA, Khairatul K, Farnaza A. An assessment of patient waiting and consultation time in a primary healthcare clinic. Malays Fam Physician. 2017;12(1):14–21. [PMC free article] [PubMed] [Google Scholar]
- 129.Swerissen H, Crisp BR. The sustainability of health promotion interventions for different levels of social organization. Health Promot Int. 2004;19(1):123–130. doi: 10.1093/heapro/dah113. [DOI] [PubMed] [Google Scholar]
- 130.Gruen RL, Elliott JH, Nolan ML, et al. Sustainability science: an integrated approach for health-programme planning. Lancet. 2008;372(9649):1579–1589. doi: 10.1016/S0140-6736(08)61659-1. [DOI] [PubMed] [Google Scholar]
- 131.Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312(7023):71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Huber M, Knottnerus JA, Green L, et al. How should we define health? BMJ. 2011;343:d4163. doi: 10.1136/bmj.d4163. [DOI] [PubMed] [Google Scholar]