Abstract
Background
The NHS Health Check Programme was launched in England in 2009, offering a vascular risk assessment to people aged 40–74 years without established disease. Socio-economic deprivation is associated with higher risk of cardiovascular disease and lower uptake of screening. We evaluated the potential impact of a community-based health check service that sought to address health inequalities through the involvement of lay health trainers.
Methods
Key stakeholder discussions (n = 20), secondary analysis of client monitoring data (n = 774) and patient experience questionnaires (n = 181).
Results
The health check programme was perceived as an effective way of engaging people in conversations about their health. More than half (57.6%) of clients were aged under 50 years and a similar proportion (60.5%) were from socio-economically deprived areas. Only 32.7% from the least affluent areas completed a full health check in comparison with 44.4% from more affluent areas. Eligible men were more likely than eligible women to complete a health check (59.4 versus 33.8%).
Conclusions
A community-based, health trainer-led approach may add value by offering an acceptable alternative to health checks delivered in primary care settings. The service appeared to be particularly successful in engaging men and younger age groups. However, there exists the potential for intervention-generated inequalities.
Keywords: circulatory disease, public health, screening
Background
Cardiovascular disease (CVD) is the leading cause of death in the UK and socio-economic deprivation is associated with higher risk of cardiovascular mortality. Tackling CVD, coupled with action to reduce health inequalities, is therefore a key priority for improving health. In 2008, the Department of Health in England established a national CVD prevention strategy—the NHS Health Check Programme—and implementation began in April 2009.1 A primary care-based vascular risk assessment is offered to anyone aged 40–74 years without established CVD, diabetes, kidney disease or dementia, relying on the assumption that the excluded groups already receive optimal risk management through other care pathways.2 Patients identified as having preclinical symptoms of disease are referred for formal diagnosis and enter established care pathways. The remainder of the population is managed within the programme, either with a brief lifestyle intervention or signposting to local services for more intensive intervention. The setting of the health check is flexible, as long as the minimum quality criteria are met.3 Most are carried out in general practice, but additional community-based services (e.g. in pharmacies) are increasingly provided to improve coverage.
If there is universal uptake, the NHS Health Check Programme could prevent 9500 cardiovascular events (myocardial infarctions and strokes) and 2000 deaths each year.1 The programme is also predicted to be cost-effective, with an estimated cost of £3000 per quality-adjusted life-year.4 However, strategies to identify and manage CVD risk have never been implemented on this scale, and estimates of effectiveness and cost-effectiveness rely on modelling studies.4,5 Concerns have been raised regarding the level of uptake of the health checks and subsequent lifestyle interventions. Department of Health cost-effectiveness modelling assumes a 75% uptake but a similar programme in Wales reported response rates of 29%, with even fewer attending for follow-up.4,6 In general, response rates for screening programmes are low in areas of socio-economic deprivation and therefore there exists the potential to widen health inequalities. However, modelling studies suggest the NHS Health Check Programme could be cost-effective if targeted at high-risk groups.5,7 Community-based approaches might be used to engage with these groups, thereby relieving some of the pressure on primary care. Robust evaluation of these approaches is required to assess the reach of the programme and determine whether it is likely to reduce or exacerbate inequalities.
The present study had two aims: (i) to determine the feasibility, acceptability and uptake of a community-based NHS health check service delivered by non-clinicians and (ii) to explore the likely impact of the service in terms of health improvement and a reduction in health inequalities.
Methods
Setting
The study was conducted in County Durham, UK, which has a population of 510 804.8 Almost half of the county's population lives in relatively deprived areas and premature mortality rates for the ‘biggest killers’ (heart disease, cancer and stroke) are worse locally than for England as a whole.9 NHS Health Checks have been delivered in general practices across Durham since 2009, with an annual target of 24 000 checks based on an eligible population of 120 000 and a target of 20% per year (health checks are repeated every 5 years). However, implementation across the county was variable and many practices consistently failed to meet their quarterly targets.10 A health trainer-led community health check (CHC) service was implemented in 2011 by County Durham and Darlington NHS Foundation Trust. The remit of the CHC service involved offering health checks in the community, with a view to engaging a wider cross section of the population and particularly those who may not access clinical health services. The service was designed to add value by building on the proven succcess of lay health trainers in engaging with people from socio-economically disadvantaged communities and supporting lifestyle change.11,12 To reinforce the broader, non-clinical focus and facilitate engagement, a ‘mini health MOT’ was devised and offered opportunistically to anyone aged 16 years or over in various community settings (e.g. workplaces, colleges, libraries and children's centres). This involved taking the person's weight, height [to calculate body mass index (BMI)] and blood pressure, as well as asking key screening questions. Those found to be eligible for a full health check were invited to a separate appointment, where their waist circumference and cholesterol level (via pinprick blood testing) were measured and the results were explained. The health trainers also provided brief advice and signposted to lifestyle services, where appropriate.
Study design
A pragmatic formative evaluation, combining analysis of routine monitoring data with key stakeholder consultation. The design was decided in collaboration between the researchers and service leads, in light of the limited resources and timescales.
Participant recruitment
The CHC service leads, health trainers and commissioners of the countywide NHS Health Check Programme were invited to take part in the evaluation. Other stakeholders were recruited using a purposive sampling approach in order to develop variation and maximize the possibilities of obtaining leads for additional data.13 A list of workplaces, community organizations, primary care and public health staff was developed based on suggestions from the service leads and their existing links with these teams. The risks of bias were felt to be counter-balanced by the need to access those who were aware of the CHC service and willing to participate in its evaluation. Information packs setting out the purpose of the evaluation and what participation would involve were distributed by email or post. Those who were willing to take part were asked to contact the evaluation team and those who did not respond within two weeks were sent one reminder. Recruitment continued until all relevant stakeholder groups were represented.
Data collection
Semi-structured interviews (n = 11) were used to gather key stakeholder perspectives on the CHC service, in terms of what had worked well and what could be improved. The interviews were conducted either at the participant's workplace or by telephone, according to their preference. A focus group with all members of the CHC health trainer team (n = 5) explored their experiences of implementing and delivering the service. This method was felt to be appropriate for use with staff working as a team.14 The interviews and focus group were audio-recorded, with participants' informed consent, and transcribed verbatim. Due to time restrictions, other local health trainers were asked to complete an H-diagram. This is a tool that combines attributes of SWOT analysis with those of ranking exercises and helps individuals to record their views in a non-threatening, open but structured way.15 Health trainers (n = 4) completed the H-diagram in their own time and returned it to the evaluation team by post.
Quantitative monitoring data from the first six months of CHC service delivery ( January to June 2012) were also examined. Client age, gender, ethnicity, postcode, BMI and blood pressure were gathered using the mini MOT (n = 774). These details were then entered onto a Microsoft Excel spreadsheet by a secretary within the NHS Foundation Trust, along with details of whether the client was eligible for an NHS health check (n = 239) or had been signposted to their GP or appropriate lifestyle services. The same information was recorded for those who returned for a health check (n = 101), plus waist circumference, cholesterol level and CVD risk score (calculated using specialized software). The results of the health check were entered onto a laptop computer in the community, then uploaded and processed by an external company, Health Diagnostics®, with quarterly reports submitted to the Foundation Trust. A final data source involved patient experience questionnaires (see Box 1) completed anonymously and voluntarily by clients following the mini MOT (n = 181); responses were entered onto Survey Monkey® by a secretary.
Box 1. Content of the patient experience questionnaire.
| How did you find out about the Mini Health MOT? |
| Told by health trainer |
| Told by Get Active |
| Told by partner, friend, relative, colleague |
| Information from work |
| Information leaflet |
| Advertisement in local community |
| Other, please state: |
| What made you decide to have a Mini Health MOT? |
| I was worried about my health |
| I don't get to see my doctor |
| I was encouraged by a family member or friend |
| The staff here told me about it when I came in |
| I take care of my health—this was an opportunity to have it checked out |
| It's more convenient than making an appointment with my doctor |
| Other, please state: |
| Following their Mini Health MOT, some people made the following statements about the staff who did their Mini Health MOT. Please tick the boxes that best indicate how far you agree or disagree with each statement: |
| The staff were friendly |
| The staff made me feel comfortable |
| The staff explained everything to me in an understandable way |
| I was given enough time to discuss any concerns |
| How satisfied were you with today's Mini Health MOT? |
| Would you recommend the Mini Health MOT to other people? |
| Are you: male/female? |
| What age group are you in? 39 and under/40–49/50–65/66–74/75+ |
Analysis
The interviews and focus group were audio recorded and transcribed verbatim, with all identifying information removed. The transcripts and H-diagrams were analysed using a thematic content approach, whereby each phrase is examined, coded according to the themes within it and considered in terms of its context in the discussion.16 Trustworthiness of data interpretation was addressed by having two members of the evaluation team independently analyse each transcript.17 The process took place manually to ensure the researchers' continued immersion in the data.
The Statistical Package for the Social Sciences (v.19) was used to process quantitative data from the NHS Foundation Trust monitoring database. Summary data obtained from the full health check and patient experience questionnaires were collated and examined using Microsoft Excel. Descriptive statistics were produced to highlight the baseline characteristics of the CHC client population and identify areas of unmet need.
Results
Client demographics
Of the 774 individuals who underwent a mini MOT between January and June 2012, 61.6% were women. However, among those who returned for a full health check, the sex ratio was almost equal (54 women and 47 men) (see Fig. 1). More than half (59.4%) of men found to be eligible for a health check went on to complete one with the CHC service, in comparison with around one-third (33.8%) of eligible women. Offering health checks in workplaces was felt to be a particularly successful strategy for engaging men, in terms of removing potential barriers to health screening:
Being a man myself, I know a lot of men typically will put off going to the doctors and things like that […] I think the fact that we're providing the onsite facility removes that excuse, if you like—for want of a better term—for a lot of people who say, ‘Well, oh, I'll go next week. Or I'll go at the weekend.’ When it's actually there, provided for them at work, be it in their lunch break or whether the employer gives the time, it does remove a barrier for a lot of people. (Stakeholder 10: workplace lead)
Fig. 1.
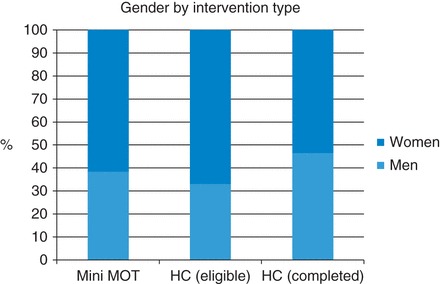
Gender by intervention type.
Health checks delivered within general practice were described as most appealing to women and patients aged 60 years and over. In contrast, the 40–49-age group constituted the largest proportion (56.0%) of those attending for a health check with the CHC service (see Fig. 2). Of the 53 individuals aged 60 years and over who were found to be eligible, 18 completed a full health check, equating to an attendance rate of 34.0%. However, 56 of the 94 eligible people aged 40–49 years completed a health check, equating to a 59.6% attendance rate.
Fig. 2.
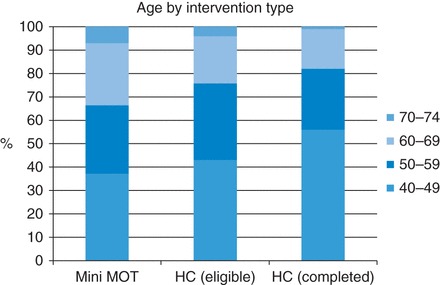
Age by intervention type.
Socio-economic status
The Index of Multiple Deprivation (IMD) 2007 was used to rank client postcodes based on national distributions of IMD and the ranks were then assigned to deprivation quintiles. This revealed that those living in the most deprived areas were more likely to engage with the CHC service than those living in less deprived areas. Almost two-thirds of mini MOT recipients (60.5%, 449 individuals) came from the first and second deprivation quintiles combined, compared with one-quarter (24.7%, 183 individuals) from the fourth and fifth quintiles. Stakeholders saw this as a key indicator of success for the CHC service, which had been commissioned to target ‘hard-to-reach’ populations:
What we were concerned with is that our most deprived communities weren't engaging in the health checks programme. So this idea of a community health checks programme was very much, kind of, let's try it. A little bit of a pilot. […] The health trainers were tasked more about trying to get into those areas where we don't really have any provision at the moment. (Stakeholder 3: commissioner)
Figure 3 compares the socio-economic status of mini health MOT recipients with those found to be eligible and returning for a full health check. It appears that health checks were more likely to be taken up by those from relatively affluent groups. Of the 52 clients from the most deprived quintile identified as being eligible, only 17 completed a health check. This represents an attendance rate of 32.7% in comparison with 44.4% for the more affluent groups.
Fig. 3.
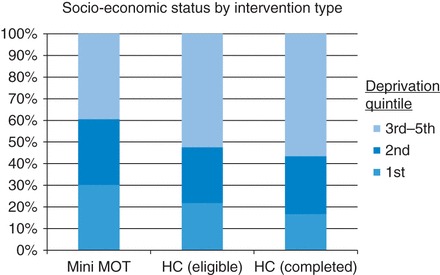
Socio-economic status by intervention type.
CVD risk and signposting
More than half of those who received a health check (58 of 101 individuals) were identified as having a low CVD risk score. Almost one-third (30 individuals) had a moderate score and a further 13 individuals had a high score. These proportions differed significantly by gender (see Fig. 4). A higher proportion of women were in the low-risk category (68.5%, compared with 44.7% for men), whereas men were twice as likely to be in the high-risk category (17.0%, compared with 9.3% for women). Gender is a key risk factor for CVD. However, it is possible that many women who were identified as low risk in the short-term had high risk of developing CVD later in life due to a combination of family history and lifestyle factors. A new calculator has since been introduced to assess CVD risk throughout an individual's lifetime.18
Fig. 4.
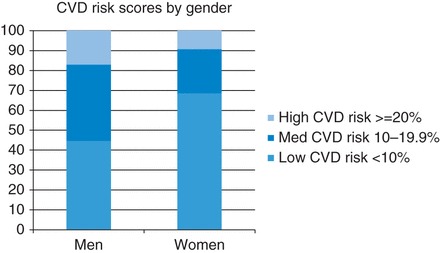
CVD risk scores by gender.
Those who received a full health check were more likely to be referred to a GP for advice than those who received a mini MOT (35.1% of clients in comparison with 22.2%), due to a greater level of health need among health check recipients. Other mini MOT recipients were referred for further support from a health trainer (10.6%), stop smoking services (2.7%), weight management (2.7%) or exercise on referral (1.8%). These figures were lower than expected, given that the CHC model was anticipated to increase the likelihood of clients being offered—and taking up the offer—of appropriate lifestyle advice and support:
The health trainers have this, kind of, unique role because of their translation of evidence and risk factors into a format that people would understand. So I think with the community programme, we will see more people going into lifestyle programmes—stop smoking, physical activity, weight management—as a result of having a health check. As opposed to those people having a health check done in general practice. (Stakeholder 8: commissioner)
User satisfaction
A total of 181 patient experience questionnaires were completed voluntarily and anonymously by clients following a mini health MOT. Most respondents agreed strongly that the staff were friendly (94.4%), made them feel comfortable (92.7%), explained things in a way that was understandable (93.9%) and gave them enough time to discuss any concerns (86.4%). In total, 99.4% of respondents stated that they were very or quite satisfied and the same figure said they would recommend the mini MOT to others. These results suggest a high level of satisfaction with the mini MOT approach. There was a general perception that the CHC service offered more than other health check providers in terms of the level of information provided:
That's what I've had a few people say—‘Oh, you don't get this kind of information at the GP’—because we sit and go through everything and the results with them. (Stakeholder 14: health trainer)
Two workplace leads had received a health check and spoke positively about their experiences (see Box 2). Health trainers also gave examples of clients identified as having very high blood pressure and requiring urgent referral to their GP. Overall, stakeholders perceived the CHC service to be successful in terms of engaging with at-risk groups and raising awareness of heart health locally.
Box 2. Feedback from workplace leads.
The fact that, you know, they came into work—it's just 15 min to go and it's, like, one-to-one and all the information that you got. Especially through to the final check when, you know, you get your own personalised print out and … I'm like the other colleagues who have never had a cholesterol test. And it's always at the back of your mind, you know, what if? I know with like a family history that there was a possibility—even though you feel you're fit and healthy and doing all the right things—I know that cholesterol is one of the things that you can't predict because of … All of the things that can affect it. So I … It was an opportunity for me to have that done. (Stakeholder 6—workplace lead)
I went for the initial screening. And I can't remember what the figures or the data was, but I suspect largely because of my age that I now had an entitlement to the … to the blood check and all of the other details. Interestingly enough, when I had the first check, then what it was indicating was that my BMI was higher than it needed to be. So it … Although I probably knew that I was overweight, it certainly made me think twice and as a result I made some changes. And there was advice given at the session which was very helpful. And then when I came to do the second check, obviously the things … The adjustments that I had been making had actually made a difference. So that was positive. And, I suppose, for me, I've managed to maintain that and sustain it. (Stakeholder 7—workplace lead)
Discussion
Main findings of this study
Our findings suggest that the CHC service model represents a potentially feasible strategy for increasing coverage of the NHS Health Check Programme. The model appeared to be most successful in terms of engaging with men, younger age groups and those living in socio-economically disadvantaged areas, i.e. individuals who may be less willing to take up the offer of a health check from another provider. It is well documented that men are less likely to make use of health care and health improvement services than women, for reasons including work-related issues and a lack of services specifically targeting men's health.19,20 Offering the CHC service through workplaces was perceived to be a particularly successful strategy. Participants found the health trainer-led approach to be an acceptable way of delivering screening and communicating CVD risk in local communities. The assumption that health trainers might be more successful than clinicians in encouraging people to access appropriate lifestyle services was not supported by the monitoring data, which may indicate a lack of signposting or poor recording of this activity.
What is already known on this topic
There is some evidence to support the use of similar lay-led health improvement programmes, particularly in increasing access to care amongst ‘hard-to-reach’ populations.21–24 One review found that, although lay health advisors were not cost-effective in promoting screening uptake in a UK context, they were successful in building social capital and demonstrating high degrees of acceptability.23 Evidence is scarce to support the idea that informing someone of their risk status will lead to behaviour changes, particularly in the longer term. A Cochrane Review found that general health checks conducted by clinicians in primary or secondary care settings did not reduce morbidity or mortality.25 In contrast, a systematic review of community-based CVD prevention programmes found small but consistent positive changes in overall CVD risk.26 Studies conducted in the UK27 and USA28 have found that ‘healthy heart’ interventions delivered by trained, non-clinical health educators can reduce health service utilization and medication usage, resulting in lower costs.
Much of the ongoing debate around health checks centres on whether universal or targeted approaches to CVD screening are more effective and cost-effective.29,30 A modelling study using Scottish survey data suggested that a targeted approach would be less costly than mass screening and identify up to 84% of high-risk individuals.7 However, a universal approach creates opportunities to engage with people at different levels of risk to influence their lifestyle choices.30 Growing evidence suggests that universal strategies can be cost-effective and are likely to be beneficial for health inequalities.2,29 The CHC service combines both approaches in an effort to achieve good coverage in groups who could potentially see the greatest benefit, which fits with the idea of ‘proportionate universalism’.31 However, the lower take-up rate of health checks amongst those from the most deprived areas suggests that this approach may be disproportionately attractive to more affluent individuals and therefore there remains a risk of intervention-generated inequalities.32
What this study adds
Uptake of NHS health checks remains a key concern. The CHC service was particularly successful in engaging those from less affluent communities at the mini MOT stage and it is important that efforts are made to retain these individuals to avoid widening the inequalities gap. Lower retention of women and older people need not be problematic if these individuals choose to receive a health check from a GP or pharmacist instead. Improved communication and data linkage between the various providers would facilitate monitoring of this situation and also help to avoid duplication of effort. Gender differences in the way that men and women respond to services and also in the way that CVD risk is calculated must be taken into account. It appears that delivering mini MOTs in community settings is a particularly successful way to engage women, while offering health checks in workplaces may remove some of the barriers that men experience in accessing health services.
Health checks alone are unlikely to be sufficient in terms of prompting people to change their lifestyles. The CHC service was commissioned in part to deliver lifestyle interventions to people identified as being at moderate risk of CVD. However, around two-thirds of clients were found to be at low or high risk. Efforts are needed to ensure these clients have access to appropriate support and also to ensure that anyone identified as high risk seeks advice from their GP. Health trainers and others involved in delivering health checks require appropriate training to communicate the level of risk without creating unnecessary anxiety or false reassurance. Rigorous process and outcome evaluations are required to determine the effectiveness, cost-effectiveness and equity of various health check providers. Our findings suggest that a health trainer-led, community-based approach to vascular risk assessment can be feasible and acceptable, but this needs to be evaluated on a larger scale.
Limitations of this study
This evaluation was based largely on information gathered by health trainers during routine practice. Limitations of secondary data analysis include concerns about the accuracy of data sources and how to deal with incomplete or inconclusive information.33 Rather than giving numeric values for BMI and blood pressure, the CHC service database used a yes/no response to indicate overweight or high blood pressure and the fields for recording signposting to lifestyle interventions were largely left blank. The lack of numeric data and likelihood of recording errors, particularly in relation to signposting, limited the analyses we were able to conduct. Furthermore, we were only provided with summary data from the full health checks and patient experience questionnaires, and therefore we were not able to conduct the statistical testing that individual level data would allow. Our analyses highlight the importance of linking mini MOT and health check data in order to identify particular groups that may be lost-to-follow-up.
We acknowledge that service users are a key group not represented in the qualitative element of this evaluation, although some feedback was gathered using the patient experience questionnaire. This work constitutes a pilot for larger scale evaluations that are likely to focus on the views, experiences and outcomes for service users. The relatively small sample size might also cause concern, even though credibility in qualitative research depends less on sample size than on the richness of the information gathered.34 By involving the CHC service leads in identifying potential participants, we are likely to have spoken only to individuals who were largely supportive of the service. However, use of a mixed-methods approach and sampling different groups of stakeholders enabled us to effectively capture a range of views and enhance the reliability of the evaluation.17 Trustworthiness of interpretation was addressed by having all members of the research team independently analyse the transcripts. An additional element of trustworthiness was achieved by feeding back our interpretations to the service leads for comments, as well as presenting interim findings at a national conference.
Ethics Approval
The evaluation received approval from Northumbria University Faculty of Health and Life Sciences research ethics sub-committee. A letter of access was obtained from County Durham and Darlington NHS Foundation Trust.
Authors' Contributions
S.V. wrote the initial draft of the manuscript, conceived the evaluation and led on data collection, analysis and interpretation of findings. S.M.C. and L.G. contributed to the evaluation design, data analysis and interpretation, and commented on drafts of the paper. L.G. also collected data.
Funding
This work was supported by Northumbria University through the Higher Education Innovation Fund (HEIF). At the time of conducting the evaluation, S.V. and S.M.C. were funded in part as members of Fuse, a UK Clinical Research Collaboration (UKCRC) Public Health Research Centre of Excellence. Funding from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council and the National Institute for Health Research (NIHR), under the auspices of UKCRC, is gratefully acknowledged. Views expressed are those of the authors and do not necessarily represent those of the above named funders.
Acknowledgements
We express our grateful thanks to the participants who gave up their time to take part in this evaluation. We acknowledge the support of colleagues from County Durham and Darlington NHS Foundation Trust, particularly Grace Wali, Kathy King and Lee Mack.
References
- 1. Department of Health. Putting Prevention First—Vascular Checks: Risk Assessment and Management. London: Department of Health, 2008. [Google Scholar]
- 2. Dalton A, Soljak M. The nationwide systematic prevention of cardiovascular disease. The UK's Health Check Programme. J Ambul Care Manage 2012;35(3):206–15. [DOI] [PubMed] [Google Scholar]
- 3. Department of Health. Putting Prevention First—Vascular Checks: Risk Assessment and Management—Next Steps Guidance for Primary Care Trusts. London: Department of Health, 2008. [Google Scholar]
- 4. Department of Health. Economic Modelling for Vascular Checks. London: Department of Health, 2008. [Google Scholar]
- 5. Khunti K. Unanswered questions over NHS health checks. BMJ 2011;342(5):316–8. [DOI] [PubMed] [Google Scholar]
- 6. Richardson G, Woerden H, Morgan L, et al. Healthy hearts—a community-based primary prevention programme to reduce coronary heart disease. BMC Cardiovasc Disord 2008;8:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lawson KD, Fenwick EA, Pell AC, et al. Comparison of mass and targeted screening strategies for cardiovascular risk: simulation of the effectiveness, cost-effectiveness and coverage using a cross-sectional survey of 3921 people. Heart 2010;96(3):208–12. [DOI] [PubMed] [Google Scholar]
- 8. Altogether Better Durham Area Action Partnership. 2012 Statistical Profile. County Durham & Area Action Partnerships. Durham, UK: Assistant Chief Executive's Office, Durham County Council, 2012. [Google Scholar]
- 9. Durham County Council, NHS County Durham. County Durham Joint Strategic Needs Assessment 2012. County Durham: Durham County Council & NHS County Durham, 2012. [Google Scholar]
- 10. Lavender M. Check4Life—a countywide approach. In: Paper Presented at: Check4Life Learning Network Inaugural Conference 2013, Durham, UK. [Google Scholar]
- 11. Wilkinson D, Sniehotta F, Michie S. Targeting those in need: baseline data from the first English National Health Service (NHS) Health Trainer Service. Psychol Health Med 2011;16(6):736–48. 1–13. [DOI] [PubMed] [Google Scholar]
- 12. Visram S, Clarke C, White M. Making and maintaining lifestyle changes with the support of a lay health advisor: longitudinal qualitative study of health trainer services in northern England. PLOS One 2014;9(5):e94749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lincoln Y, Guba E. Naturalistic Inquiry. Beverly Hills, CA: Sage, 1985. [Google Scholar]
- 14. Morgan D. Focus Groups as Qualitative Research, 2nd edn London: Sage, 1997. [Google Scholar]
- 15. O'Hara P. Enhancing Stakeholder Participation in National Forest Programmes. Tools for Practitioners. Rome: National Forest Programme Facility, Food and Agriculture Organization of the United Nations, 2009. [Google Scholar]
- 16. Boyatzis R. Transforming Qualitative Information: Thematic Analysis and Code Development. London: Sage, 1998. [Google Scholar]
- 17. Denzin NK. The Research Act: A Theoretical Introduction to Sociological Methods. New York: McGraw-Hill, 1978. [Google Scholar]
- 18. JBS3 Board. Joint British Societies’ consensus recommendations for the prevention of cardiovascular disease ( JBS3). Heart 2014;100:ii1–ii67. [DOI] [PubMed] [Google Scholar]
- 19. Bertakis K, Azari R, Helms J, et al. Gender differences in the utilization of health care services. J Fam Pract 2000;49(2):147–52. [PubMed] [Google Scholar]
- 20. Smith J, Braunack-Mayer A, Wittert G. What do we know about men's help-seeking and health service use? Med J Aust 2006;184(2):81–3. [DOI] [PubMed] [Google Scholar]
- 21. Andrews J, Felton G, Wewers M, et al. Use of community workers in research with ethnic minority women. J Nurs Scholarsh 2004;36(4):358–65. [DOI] [PubMed] [Google Scholar]
- 22. Swider S. Outcome effectiveness of community health workers: an integrative literature review. Public Health Nurs 2002;19(1):11–20. [DOI] [PubMed] [Google Scholar]
- 23. Carr S, Lhussier M, Forster N, et al. An evidence synthesis of qualitative and quantitative research on component intervention techniques, effectiveness, cost-effectiveness, equity and acceptability of different versions of health-related lifestyle advisor role in improving health. Health Technol Assess 2011;15(9):0–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lewin SA, Dick J, Pond P, et al. Lay health workers in primary and community health care (review). Cochrane Database Syst Rev 2005;(2): Art. No.: CD004015. [DOI] [PubMed] [Google Scholar]
- 25. Krogsboll L, Jorgensen K, Gronhoj C, et al. General health checks in adults for reducing morbidity and mortality from disease. The Cochrane Library 2012;(10):CD009009.pub009002. [DOI] [PubMed] [Google Scholar]
- 26. Pennant M, Davenport C, Bayliss S, et al. Community programs for the prevention of cardiovascular disease: a systematic review. Am J Epidemiol 2010;172(5):501–16. [DOI] [PubMed] [Google Scholar]
- 27. Barton G, Goodall M, Bower P, et al. Increasing heart-health lifestyles in deprived communities: economic evaluation of lay health trainers. J Eval Clin Pract 2011;18(4):835–40, 1–6. [DOI] [PubMed] [Google Scholar]
- 28. Nawathe A, Glied S, Weintraub W, et al. The effect of a cardiovascular educational intervention on healthcare utilization and costs. Am J Manag Care 2010;16(5):339–46. [PMC free article] [PubMed] [Google Scholar]
- 29. Capewell S, Graham H. Will cardiovascular disease prevention widen health inequalities? PLoS Med 2010;7(8):e1000320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kumar J, Chambers R, Mawby Y, et al. Delivering more with less? Making the NHS Health Check work in financially hard times: real time learning from Stoke-on-Trent. Qual Prim Care 2011;19(3):193–9. [PubMed] [Google Scholar]
- 31. Marmot M. Fair Society, Healthy Lives: Strategic Review of Health Inequalities in England Post-2010. London: The Marmot Review, 2010. [Google Scholar]
- 32. White M, Adams J, Heywood P. How and why do interventions that increase health overall widen inequalities within populations? In: Babones S. (ed.). Social Inequality and Public Health. Bristol: The Policy Press, 2009,65–81. [Google Scholar]
- 33. Robson C. Real World Research: A Resource for Users of Social Research Methods in Applied Settings, 3rd edn Oxford: Blackwell, 2011. [Google Scholar]
- 34. Patton M. Qualitative Evaluation and Research Methods, 2ndedn Newbury Park, CA: Sage, 1990. [Google Scholar]


