Abstract
Background.
Low back pain (LBP) is a significant health problem and common reason to visit the GP. Evidence suggests GPs experience difficulty applying evidence-based guidelines.
Objective.
Explore GPs’ underlying beliefs about acute LBP and how these influence their clinical management of patients.
Methods.
Eleven GPs from one geographical region within New Zealand were recruited by purposive sampling. Audio recordings of semi-structured qualitative interviews were transcribed verbatim. Data were analysed with an Interpretive Description framework.
Results.
Four key themes emerged related to the causes of acute LBP, GP confidence, communicating diagnostic uncertainty and encouraging movement and activity. Acute LBP was seen as a direct representation of tissue injury, consequently the assessment and management of patients’ attitudes and beliefs was not a priority. Participants’ confidence was decreased due to a perceived inability to diagnose or influence the tissue injury. Despite this, diagnoses were provided to patients to provide reassurance and meet expectations. Guideline recommendations regarding activity conflicted with a perceived need to protect damaged tissue, resulting in reported provision of mixed messages about the need to be both active and careful.
Conclusions.
GPs’ initial focus upon tissue injury during acute care, and providing a diagnostic label, may influence patients’ subsequent alignment with a biomedical perspective and contribute to consultation conflict and patients’ perception of blame when discussion of psychosocial influences is introduced. Demonstrating the relevance of the biopsychosocial model to acute LBP may improve GPs’ alignment with guidelines, improve their confidence to manage these patients and ultimately improve outcomes.
Keywords: Attitudes, general practice, guideline adherence, health knowledge, low back pain, practice, qualitative research.
Introduction
Low back pain (LBP) is a common reason to visit the GP (1–3). Costs associated with LBP represent a major financial burden in developed countries (1,4–6). Psychosocial factors, including beliefs about injury, movement and recovery, are important in the development of back pain and disability (7–10).
Numerous clinical guidelines, based upon a biopsychosocial model, have been developed to improve patient outcomes and decrease costs (see Table 1 for a summary of New Zealand guidelines) (11–15). Care which is consistent with these guidelines produces better patient outcomes at lower cost (16–18). Evidence suggests that the current practice of GPs is inconsistent with these guidelines (2,19). Patient expectation and the desire to avoid conflict in the patient–doctor relationship seem to have an important (negative) influence on guideline adherence (20–28).
Table 1.
Summary of clinical guidance provided to New Zealand GPs (11,15)
| Core messages |
| • Acute LBP is common and episodes are nearly always short-lived |
| • Serious causes of LBP are rare |
| • Reassurance is very helpful |
| • Investigations are not helpful for acute LBP unless there are signs of serious disease (Red Flags). There are risks associated with investigation |
| • There is strong evidence for the benefits of activity. Advice to stay or become physically active and resume normal activities, including work, as soon as possible is helpful |
| • Adequate analgesia may help patients to stay active |
| • Prolonged bed rest and use of opiates or diazepam can be harmful |
| • Patients’ attitudes and beliefs should be considered as much as anatomical and pathological factors. Fear of pain has a major influence on impairment and chronicity |
| Recommended assessment |
| • History and site of the pain and any previous episodes |
| • Activities associated with pain and limitations |
| • Risk factors for serious disease (Red Flags) |
| • Any factors which may be barriers to recovery and early resumption of normal activities, including work (this includes the assessment of psychosocial risk factors (Yellow Flags)—these relate to attitudes and beliefs, behaviours, compensation issues, emotions, family and work) |
| • The level of activity required to resume usual activities |
| • Examination of the degree of functional limitation and any relevant neurological signs |
| Recommended management |
| • Advise patients to stay active and continue normal activities. This should include reassurance that movement and activity will not cause harm |
| • Provide an explanation and reassurance, an exact diagnosis is often not possible and can be unhelpful |
| • Control pain if necessary to enable activity |
| • Promote staying at, or quickly returning to, work |
| • Provide ongoing support |
There is strong evidence that health professionals’ beliefs are associated with their patients’ beliefs about back pain, as well as their own guideline adherence (29). Clinicians influence their patients’ understanding of the problem and their recovery expectations; many messages received from clinicians reinforce patient perceptions that their back is vulnerable and needs protection (30).
GPs’ conceptual framework, and how they communicate this to patients, needs to be better understood to optimize management of acute LBP. While previous qualitative studies have highlighted the importance of patient expectations and maintaining doctor–patient relationships (24,25,27), most qualitative research has focussed on chronic back pain (25,31–33). Many people who consult their GP for a new episode of back pain do not return for further consultation, despite continuing to experience pain and disability (34). Regardless of the reason for this, it indicates that GPs may only interact once with most patients experiencing an episode of back pain and information received during this consultation may need to inform long-term self-management (30). It is therefore important to understand GP management during consultations for acute back pain. This study explores GPs’ underlying beliefs about acute LBP and how these influence their management.
Methods
Design
This qualitative investigation used the framework of Interpretive Description (ID) (35). This methodology was selected because it is orientated towards a clinical context and aims to develop findings which will assist health professionals in their clinical practice (35–37). ID identifies themes and patterns among participant perspectives, while also accounting for individual variation (35–37). ID values previous theoretical and clinical knowledge as a starting point for the research which can be challenged and refined as the research progresses (36,37). The researchers acknowledged the risk this foreknowledge could bias the research. Consequently, the primary investigator and interviewer (BD) acknowledged his own assumptions and preconceptions (consistent with background information presented above) prior to data collection and circulated these among the entire research team. This step helped to make any influence over the design and development of the research explicit (36).
Participant recruitment
Potential participants were contacted by approaching the managers of 17 general practices within one region of New Zealand. All GPs within these practices (99) were eligible for inclusion and there were no exclusion criteria. These practices were selected to maximize the range of participant characteristics in terms of GP gender and length of experience, as well as practice location (urban, suburban) and the culture/socio-economic status of their patient populations (35). Respondents were screened to obtain diversity related to these characteristics. After initial recruitment individual GPs were purposively invited to join the study because either their or their practice population’s characteristics were different to those of respondents already interviewed.
Data collection
Following written informed consent, face-to-face semi-structured interviews were audio-recorded. An interview guide with open-ended questions allowed flexibility to discuss items as they arose (Table 2). Afterward, participants completed a demographic information sheet, and the Tampa Scale of Kinesiophobia, as modified by Houben et al. (38) to assess the fear of movement and (re)injury clinicians have for their patients.
Table 2.
Semi-structured interview guide
| • Their personal approach to managing LBP in general practice |
| • Any personal experience they have had of LBP and its influence on their practice |
| • Their views about the importance of LBP among their patient population |
| • Managing LBP |
| ○ Challenges/enjoyable aspects |
| ○ Tips learned from experience |
| ○ Influential experiences |
| ○ The most important thing they do for someone presenting with acute LBP |
| ○ The important things for patients to know about LBP and how well they communicate these |
| ○ Anything they avoid saying to patients with back pain |
| • First consultation for acute LBP |
| ○ What they hope to achieve/prioritize |
| ○ Screening for pathology |
| ○ Explanations they provide to patients |
| ▪ Pain and healing processes |
| • Perceptions of the biopsychosocial model vs. the acute care model for patients with acute LBP |
| ○ Ability to influence their patients’ attitudes and beliefs? |
| ○ When management shifts from acute to chronic care |
| • Their thoughts about common patient attitudes and beliefs (fear avoidance/catastrophization) |
| • Their views on statements from the New Zealand Acute LBP Guide |
| • Recommendations for the development of a resource to assist GPs to manage LBP |
| • Other thoughts or ideas |
Data collection and analysis occurred concurrently, informing each other iteratively. Recruitment was suspended when no new themes or variants on established themes occurred with two subsequent interviews. The research team debated and agreed theme saturation.
Data analysis
Interview recordings were transcribed verbatim. Participants did not review transcripts or validate findings (37). Constant comparative analysis compared pieces of data to develop themes (39). In groups of three, transcripts were read and then re-read to identify initial broad themes within each while taking care not to prematurely focus or close the analysis (35,37). After the first three transcripts were analysed, a thematic framework was created based upon similarities within these broad themes. Individual comments from participants were subsequently coded by theme within NVivo 9.2 software (QSR International Pty Ltd). Transcripts continued to be analysed within groups of three. When each group was analysed, emergent themes were either integrated into the existing framework, or the framework was reorganized to accommodate the new perspective. Individual comments were then coded by theme within NVivo. When new themes emerged, previous transcripts were recoded with reference to the new theme. As analysis progressed broad themes were refined and data classified into more focussed subthemes. Primary coding was performed by one researcher (BD). The third transcript was independently analysed by an external researcher (MP), previously uninvolved in the study. This analysis was then compared to that of the primary researcher. Themes were then cross-referenced to the original data to verify these represented participants’ accounts (40). This process resulted in minor reorganization of the thematic framework but no significant conflicts arose, verifying existing themes. Following analysis of the sixth interview, a detailed theme summary was discussed by the research team, resulting in further reorganization of the thematic framework and suggestions of new avenues to explore with subsequent interviews.
The research team
The initial research team comprised of academics and clinicians with backgrounds in physiotherapy (BD, GDB, SD), general practice AD and psychology (FM, SD). AD, GDB and SD had previous qualitative LBP research experience. The variety of backgrounds and perspectives within this team helped to ensure that the research was not biased by any single viewpoint. Following external verification of themes, MP (a physiotherapist with qualitative LBP research experience), reviewed subsequent theme summaries to ensure ongoing consistency and joined the research team.
Results
Interviews were conducted with eleven GPs between April 2011 and January 2012. Seven GPs were interviewed following the initial approach to practice managers. Four eligible respondents were not interviewed because their characteristics were similar to previous participants. A further seven GPs at six practices were then invited to participate to add diversity and four of these GPs were interviewed. Interview duration was between 43 and 78 minutes. Participant characteristics are shown in Table 3.
Table 3.
Characteristics of GP participants
| Participant code, sex | Age, years | Ethnicity | Practice location and population | Years’ practicing | LBP history | TSKa |
|---|---|---|---|---|---|---|
| GP01, male | blank | NZ European | Central city Low socio-economic |
28 | Yes | 35 |
| GP02, female | 44 | NZ European | Central city Student |
13 | No | 27 |
| GP03, male | 67 | NZ European | Central city Student |
12 | Yes | 28 |
| GP04, male | 55 | NZ European | Suburb Low socio-economic |
10 | No | 26 |
| GP05, male | 49 | British | Suburb Low socio-economic |
12 | No | 28 |
| GP06, female | 30 | NZ European | Suburb Low socio-economic |
2 | Yes | 22 |
| GP07, male | 57 | NZ European | Suburb High socio-economic |
26 | Yes | 37 |
| GP08, female | 38 | NZ European | Central city High socio-economic |
12 | Yes | 29 |
| GP09, male | 38 | NZ European | Suburb Low socio-economic |
10 | No | 30 |
| GP10, female | 34 | NZ European | Suburb Mixed socio-economic |
1.5 | No | 34 |
| GP11, female | 46 | Maori | Suburb Mixed socio-economic |
20 | Yes | 25 |
| Mean (SD) | 45.8 (10.9) | 13.3 (8.1) | 29.2 (4.3) |
TSK, Tampa Scale of Kinesiophobia.
aScored on a range from 17 to 68 with higher scores indicating greater levels of fear avoidance beliefs.
LBP was seen as being a very common problem in general practice which could have a large impact upon patients’ lives. Overall, participants did not see acute LBP to be a challenging condition to manage, as they expected most patients to get better regardless of health care received. Participants thought it was difficult to predict who would develop chronic pain, which was perceived as being considerably more challenging to manage. Generally LBP was not seen as being an enjoyable part of the job and chronic LBP was ‘very hard work’. One participant referred to the failure of his training programme to prepare him for managing back pain.
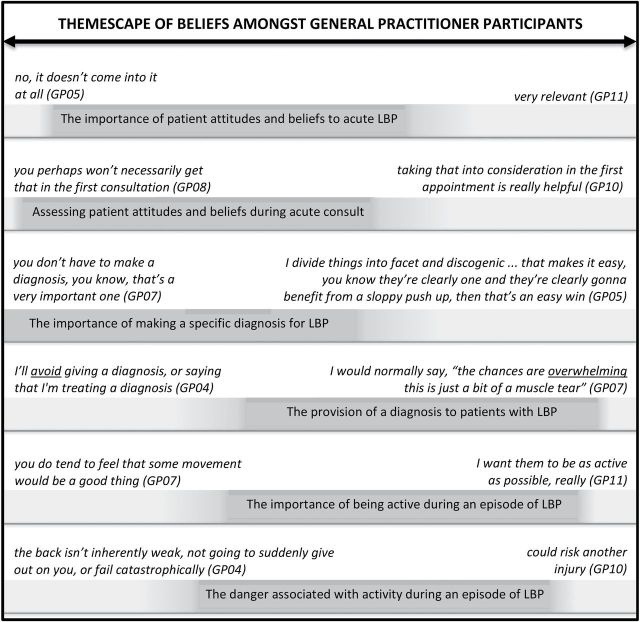
Participants were aware of clinical guidelines and much of their practice appeared to be consistent with these, however, their own back pain and clinical experiences seemed to have a strong influence on beliefs (see online supplementary Data, Box 1). Consequently, interviews demonstrated marked inter-participant variation. Four key themes emerged related to management difficulties or inconsistencies. These themes were selected for presentation in this paper as they may have value for informing practice. For each theme there was a continuum of views with no one participant being consistently extreme. Figure 1 demonstrates where the views of the majority lay relative to the range of perspectives expressed. This representation of themes and the diversity of views related to them will be described as a ‘Themescape’.
Figure 1.
Themescape which we have developed to demonstrate the range of participant beliefs related to individual themes. It illustrates where the views of the majority (darker shading with text) were positioned relative to the range of perspectives expressed in the interviews (quotes above theme bars); there was a continuum of views with no one participant being consistently extreme (the shading attempts to illustrate the continuity of views). It is important to note that this figure is a visual representation of the variety of viewpoints elicited. It does not attempt to provide a quantitative analysis of views; hence all bars (and shaded areas representing themes) are the same length.
Participant quotations which exemplify key themes are presented within the text. Additional quotes illustrating important themes are shown in online supplementary Data. Text within quotation marks is from mimicked explanations directly to an imagined patient. Participant emphasis is shown with underlining.
The causes of, and influences upon, acute LBP
Acute back pain was seen as normally being directly related to acute injury of a musculoskeletal structure in the back (see online supplementary Data, Box 2). Ruling out alternative pathological explanations for the person’s pain was the key consultation priority for all participants. Identifying a causal relationship between an injurious movement and an episode of pain assisted this process:
I guess I just have a lot of anxiety- like as soon as they give me a clear history of a definite injury, and there’s no red flags, I feel so much happier about the whole situation (GP06)
Seeking a biomechanical explanation reinforced the GPs’ concept that acute tissue injury was the important element of the presentation. Most participants did not think they were able to diagnose the injured tissue, but this was not seen as being problematic:
it’s not usually possible to have the confidence to give a diagnosis really for some of the underlying sort of cause ... it doesn’t matter too much what the details are of which particular little bit of the soft tissue’s involved because the treatment is the same regardless (GP04)
The influence of psychosocial factors
Psychosocial factors were seen as having the potential to influence patients’ pain experience, behaviour and prognosis. These influences were seen as being much more relevant to chronic pain, which was strongly differentiated from ‘true’ acute pain (see online supplementary Data, Box 3):
The reasons in behind why they have chronic pain, are complex and interleaved and, complicated (GP01)
There were a range of views regarding when patient attitudes and beliefs become important, reflecting general uncertainty about how and why they influence pain and outcomes:
I’m not so sure as it’s um relevant to the true acute back pain ... where it’s relevant is the transition from acute back pain, self-limiting ... the transition between that and chronic pain (GP04)
As a consequence most participants did not prioritize the assessment or discussion of beliefs during the first consultation (see online supplementary Data, Box 4). Even for those who considered beliefs to be important during the acute phase, raising them during the initial consultation was perceived as being dangerous. It could adversely affect the doctor–patient relationship and cause unnecessary conflict. It could also prolong the consultation:
if they’ve come in with their back pain ... then you’ll address the back pain, I mean you haven’t got time to go through all that other stuff (GP02)
There was often an element of blame or suspicion when non-physical factors were identified as influencing acute pain. There was a perception that this pain was less ‘real’. These patients were seen as being difficult to treat because such influences are often beyond the GPs’ control.
the problem isn’t so much that they have pain but they can’t cope with the pain that they have (GP05)
All participants discussed some form of reassurance as being part of their first consultation, despite many considering beliefs to be unimportant at this time. When directly questioned about this apparent contradiction a participant replied:
just like reassuring someone with chest pain that they are not having a heart attack. Always good practice to reassure (GP07)
Some participants considered reassuring patients their problem was not serious and did not require investigation to be a management challenge. Only one participant prioritized identifying and addressing patient attitudes and beliefs during the first consultation. She found this to be a very rewarding aspect of her practice and rejected concerns raised by other participants related to the time it took, or patient resistance:
sometimes there needs to be time spent on allaying their concerns ... a chance to have any specific worries that they’ve got addressed at that point, so that they’re not continuing to worry about them, and having that affect their recovery ... people are increasingly more aware to their attitudes, to the influence over their recovery from illnesses. So I think people are generally receptive to talking about things like that ... you can definitely incorporate it in there (GP10)
GP confidence
The participants’ reliance on the biomedical model decreased confidence in their ability to explain and manage acute back pain. Tissue injury is associated with a natural history of healing, and they felt they did not possess sufficient understanding of anatomy and biomechanics to explain or influence this process. Participants felt they could not influence outcomes and consequently referred (and deferred) to other health professionals.
you send people where they’re going to get the best bang for their buck, and that’s where- you know, to my mind, I always say to people ‘well the physio knows more about the muscles, and the joints, and how things should be working and moving than I do’ (GP11)
Some of the more experienced participants did reflect that they were better placed to manage patients within the context of biopsychosocial factors than other health professionals because they knew the person, their family, their background and their context.
Communicating diagnostic uncertainty
Although participants were personally comfortable with a lack of diagnostic precision, they perceived that patients expect a definite diagnosis and find it reassuring. This appeared to be a key challenge which participants approached in one of two ways (see online supplementary Data, Box 5). The first was to diagnose a muscle strain:
give them a very clear answer that this is a muscle strain of the back (GP06)
This was seen as being accessible to a broad range of patients. It also acknowledged their pain had an objective source, provided a positive outlook and was thought to give patients confidence to be active. The other approach was to explain that one of a range of things may have been injured, but it is unimportant to determine which because the diagnosis does not influence management:
the disc that might have been protruded slightly ... or it might be a facet joint that got a little bit kinked, or they might have strained a ligament (GP03)
An exception to the uncertain diagnosis approach was invariably made when a patient’s pain was referred to the leg. Nearly all participants assumed referred pain was due to a pinched nerve and reported describing this to patients:
‘a disc bulges out the side cause you’ve injured your back, it’s pushing on a nerve’ (GP09)
Movement and activity—‘active rest’
All participants expressed a degree of positivity towards movement and activity during an episode of pain and most reported encouraging activity (see online supplementary Data, Box 6). Changing the beliefs of patients who considered rest to be the best treatment could be challenging. Views about activity were informed by guideline recommendations, but there was uncertainty as to how or why exercise might be helpful:
I don’t- I don’t know, but it does seem to- yes, um, so whether we’re, um, you know, some movement I’m sure’s good for sprains. And it tends to build up all the other surrounding muscles, so it helps with the posture. I don’t know. There- you know, certain bio- biomechanical reasons (GP07)
Models for the effect of activity on back pain primarily related to the prevention of stiffness, strengthening of muscles and promotion of healing. Only a few participants also mentioned pain modulatory and psychological benefits. The predominance of a biomechanical rationale was reflected in explanations which participants reported providing to patients; most described negative consequences of not being active rather than positive benefits.
‘you don’t want to seize up’ (GP08)
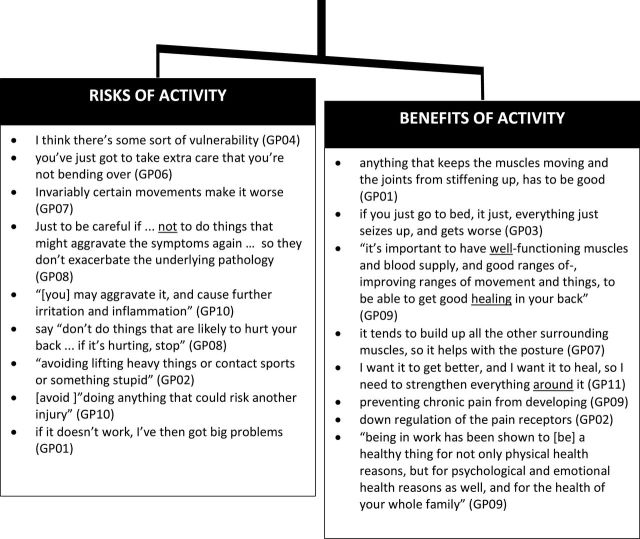
Participants saw acute pain as communicating the presence of tissue injury which should be protected to prevent deterioration, and this conflicted with their guideline-informed understanding that activity is beneficial. These two considerations were weighed up when providing activity advice (Fig. 2). Consequently, many participants reported cautioning patients against doing things which could aggravate their injury. This included encouraging avoidance behaviours to protect the back. Advice was either guided by pain, or activities thought to be dangerous:
Figure 2.
GP participant perceptions of the balance between the risks and benefits of activity. When considering activity during an episode of acute LBP and providing advice to their patients, participants weighed the benefits against these risks. Text within quotation marks is from where participants mimicked an explanation directly to an imagined patient.
avoiding lifting heavy things or contact sports or something stupid (GP02)
Much of the advice which participants reported conveying to patients contained mixed messages and reinforced the need to be active and protective at the same time. One participant referred to this as ‘active rest’.
‘keep active, so try and go about your normal, day to day business as best you can without doing things that specifically aggravate it and cause you a lot of pain, and doing anything that could risk another injury’ (GP10)
Participants reported wanting to ensure the patient did not perceive that they had gotten worse as a result of following GP advice, as this could jeopardize their ongoing relationship. Overly protective advice seemed to function as a safety net in order to prevent increased pain (considered to represent increased tissue damage).
if it doesn’t work, I’ve then got big problems, so if I confidently say to them ‘look if you go and do this you’re going to get better’ and they do it and don’t get better, the next consultation is really hard (sigh) because it raises, all of the things that I’ve said then become suspect, ‘what do you mean you gotta keep moving, I did what you said and I’m worse’, you know, so, it’s that sort of stuff (GP01)
Discussion
Summary
Participants approached acute LBP from a biomedical perspective. Finding a specific injurious event reassured them that pathology was not present. Acute pain was seen as a direct representation of tissue injury, normally uninfluenced by other factors; consequently the assessment and management of psychosocial influences was not a priority. Participants thought a specific structural diagnosis was neither achievable nor important for directing management, but often provided a diagnosis to meet patient expectations and provide reassurance. Guideline recommendations regarding activity conflicted with a perceived need to protect damaged tissue, resulting in the reported provision of mixed messages about the need to be active and careful. In general, participants’ views were consistent but each had thoughts relevant to some themes which deviated from those generally held. This resulted in a range of perspectives related to each theme.
Strengths and limitations
The qualitative methodology allowed an in-depth exploration of not just the participants’ management approaches, but also the framework which underlies these judgements. We cannot say if the participants’ self-reported management accurately reflects their usual practice as we did not audit or observe treatment interactions. The interviews and primary analysis were conducted by the same researcher (BD); the risk of bias was identified and steps taken to minimize its influence.
Care needs to be taken when generalizing qualitative research findings beyond the participants involved. We have described participants’ characteristics so that judgements can be made about applicability to other settings (41). The participants had a wide range of practice experience and cared for populations from varied socio-economic strata, however, they were predominantly New Zealand Europeans practicing in urban or suburban practices. This is reflective of the New Zealand general practice population (42) and provides depth of insight in this context, but may limit generalizability. New Zealand has an insurance system whereby people receive subsidized care and earnings compensation if their pain is the result of an injurious event. This may have made participants more likely to associate acute pain with injury than GPs who operate under different funding regimes.
Comparison with other studies
Consistent with previous studies, the participants valued the maintenance of the doctor–patient relationship and avoiding conflict (20,24,25). In contrast to these studies, however, the main reason for failing to adhere to guideline recommendations to assess psychosocial factors and reassure that movement and activity will not cause harm, was inconsistency with their underlying belief framework. Studies of chronic LBP have found that conflict between GPs’ biopsychosocial and patients’ biomedical concepts creates relationship difficulties (32,33). Participants in the current study approached chronic LBP from a biopsychosocial perspective, but not acute LBP. This may help explain why GPs do not integrate assessment and management of psychosocial factors into acute LBP care (20,24).
The participants’ reported explanations that pain referred to the leg is due to disc compression of a nerve is consistent with people who have consulted a UK GP for LBP being more likely to think that LBP is caused by a slipped disc or a trapped nerve (43).
Although participants did not see acute LBP as being a challenging condition, many participants did not feel empowered to explain and actively manage acute LBP because they felt they were not able to influence the natural history, and that they had less knowledge and understanding of the anatomy and biomechanics than other health disciplines. Breen et al. (24) similarly reported a lack of GP confidence related to LBP management.
Implications for clinical practice and future research
The acute phase of back pain is arguably the time when guideline adherence has the most potential to improve outcomes and reduce costs. Efforts to improve the presentation and dissemination of guidelines will not change practice behaviour if they conflict with GP values (44–46). Many of the underlying frameworks upon which GPs make management decisions seem contradictory, or not based upon recent evidence. This indicates that not only do GPs need to be better informed about the benefits of following guidelines, but also how and why guidelines improve outcomes.
LBP is very prevalent (47) and a number of participants had experienced episodes themselves. These participants invariably reported that these episodes had influenced how they viewed and managed back pain. Clinical experience also appeared to be an important influence. Reliance upon personal and clinical experience may have contributed to the wide inter-participant variation found.
A guide to screening for psychosocial warning signs (yellow flags) was developed in New Zealand over 15 years ago (48), but the participants did not prioritize these factors because their underlying belief framework indicated acute pain is not normally influenced by other factors. Highlighting the influence attitudes and beliefs have on all pain experiences (49) may help to demonstrate the applicability of the biopsychosocial model to acute pain, increase the priority given to these factors and reduce associated blame (25,33).
Participants provided diagnostic labels despite an inability to accurately diagnose, and against guideline recommendations (11,14). They felt simple musculoskeletal diagnoses were helpful to reassure (themselves as much as their patients) that pathology was not present. Pathoanatomical diagnoses negatively influence symptom appraisal and prognostic expectations, contribute to avoidance behaviours and are associated with poorer outcomes (30,50,51). Increased confidence in their ability to screen for pathology may decrease GPs’ reliance upon finding an injury to provide an alternate explanation. Reducing the emphasis on the tissue injury may also increase the GP’s confidence in their ability to manage LBP without referral, given most factors demonstrated to influence outcome are psychosocial, an area of practice at which GPs excel.
Patients desire a clear diagnosis not only to legitimize their experience (31,52,53), but also because they think it necessary to inform management (30,54). Providing a surrogate diagnosis, like a ‘muscle strain’, may misinform management. Injured tissue requires protection while it heals and increased pain is assumed to indicate further injury, whereas guidelines recommend remaining as active as possible despite pain (12). A better understanding of how activity improves outcomes may help GPs to promote activity in a way they feel is safe, without providing mixed messages, encouraging avoidance behaviours, or reinforcing a biomedical model.
The GPs’ initial focus upon biomedical aspects during acute care, and providing a diagnostic label, may lay the foundations for their patients’ subsequent alignment with this model and contribute to relationship difficulties and patients’ perception of blame when discussion of psychosocial influences is introduced (32,50,54). GPs wish to provide the best possible care to their patients within a time-limited consultation. They will not prioritize factors they consider inconsequential, nor provide advice which conflicts with their beliefs (44–46). Demonstrating the relevance of the biopsychosocial model to acute LBP may improve GPs alignment with guidelines, improve their confidence to manage these patients and ultimately improve outcomes.
Supplementary material
Supplementary material is available at Family Practice online.
Declaration
Funding: This research was supported by the Department of Primary Health Care and General Practice, University of Otago, Wellington. Dr SD’s time is funded by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for the South West Peninsula.
Ethical approval: New Zealand Central Regional Ethics Committee (CEN/11/EXP/014).
Conflict of interest: There are no conflicts of interest.
Supplementary Material
Acknowledgements
We thank the participants for sharing their views. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health in England.
References
- 1. Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain 2000; 84: 95–103. [DOI] [PubMed] [Google Scholar]
- 2. Williams CM, Maher CG, Hancock MJ, et al. Low back pain and best practice care: a survey of general practice physicians. Arch Intern Med 2010; 170: 271–7. [DOI] [PubMed] [Google Scholar]
- 3. Davis P, Suaalii-Sauni T, Lay-Yee R, Pearson J. Pacific Patterns in Primary Health Care: A comparison of Pacific and all patient visits to doctors: The National Primary Medical Care Survey (NatMedCa): 2001/02. Wellington: Ministry of Health, 2005, Report number: 7. [Google Scholar]
- 4. Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J 2008; 8: 8–20. [DOI] [PubMed] [Google Scholar]
- 5. van Tulder MW, Koes BW, Bouter LM. A cost-of-illness study of back pain in The Netherlands. Pain 1995; 62: 233–40. [DOI] [PubMed] [Google Scholar]
- 6. Wieser S, Horisberger B, Schmidhauser S et al. Cost of low back pain in Switzerland in 2005. Eur J Health Econ 2010; 12: 455–87. [DOI] [PMC free article] [PubMed]
- 7. Linton SJ. A review of psychological risk factors in back and neck pain. Spine (Phila Pa 1976) 2000; 25: 1148–56. [DOI] [PubMed] [Google Scholar]
- 8. Delitto A, George SZ, Van Dillen LR, et al. ; Orthopaedic Section of the American Physical Therapy Association. Low back pain. J Orthop Sports Phys Ther 2012; 42: A1–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ramond A, Bouton C, Richard I, et al. Psychosocial risk factors for chronic low back pain in primary care–a systematic review. Fam Pract 2011; 28: 12–21. [DOI] [PubMed] [Google Scholar]
- 10. Iles RA, Davidson M, Taylor NF, O’Halloran P. Systematic review of the ability of recovery expectations to predict outcomes in non-chronic non-specific low back pain. J Occup Rehabil 2009; 19: 25–40. [DOI] [PubMed] [Google Scholar]
- 11. New Zealand Guidelines Group. New Zealand Acute Low Back Pain Guide. Wellington, NZ: Accident Compensation Corporation, 2004. http://www.acc.co.nz/PRD_EXT_CSMP/groups/external_communications/documents/guide/prd_ctrb112930.pdf [Google Scholar]
- 12. Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J 2010; 19: 2075–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Savigny P, Watson P, Underwood M; Guideline Development Group. Early management of persistent non-specific low back pain: summary of NICE guidance. BMJ 2009; 338: b1805. [DOI] [PubMed] [Google Scholar]
- 14. Chou R, Qaseem A, Snow V, et al. ; Clinical Efficacy Assessment Subcommittee of the American College of Physicians; American College of Physicians; American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 2007; 147: 478–91. [DOI] [PubMed] [Google Scholar]
- 15. Hoffman MC, MacVicar J. Acute Low Back Pain. Dunedin, NZ: Best Practice Advocacy Centre New Zealand, 2009. http://www.bpac.org.nz/BPJ/2009/June/docs/bpj21_lowerbackpain_pages_6-12.pdf [Google Scholar]
- 16. McGuirk B, Bogduk N. Evidence-based care for low back pain in workers eligible for compensation. Occup Med (Lond) 2007; 57: 36–42. [DOI] [PubMed] [Google Scholar]
- 17. McGuirk B, King W, Govind J, Lowry J, Bogduk N. Safety, efficacy, and cost effectiveness of evidence-based guidelines for the management of acute low back pain in primary care. Spine (Phila Pa 1976) 2001; 26: 2615–22. [DOI] [PubMed] [Google Scholar]
- 18. Rutten GM, Degen S, Hendriks EJ, Braspenning JC, Harting J, Oostendorp RA. Adherence to clinical practice guidelines for low back pain in physical therapy: do patients benefit? Phys Ther 2010; 90: 1111–22. [DOI] [PubMed] [Google Scholar]
- 19. Jackson JL, Browning R. Impact of national low back pain guidelines on clinical practice. South Med J 2005; 98: 139–43. [DOI] [PubMed] [Google Scholar]
- 20. Crawford C, Ryan K, Shipton E. Exploring general practitioner identification and management of psychosocial Yellow Flags in acute low back pain. N Z Med J 2007; 120: U2536. [PubMed] [Google Scholar]
- 21. Shye D, Freeborn DK, Romeo J, Eraker S. Understanding physicians’ imaging test use in low back pain care: the role of focus groups. Int J Qual Health Care 1998; 10: 83–91. [DOI] [PubMed] [Google Scholar]
- 22. Espeland A, Baerheim A, Albrektsen G, Korsbrekke K, Larsen JL. Patients’ views on importance and usefulness of plain radiography for low back pain. Spine (Phila Pa 1976) 2001; 26: 1356–63. [DOI] [PubMed] [Google Scholar]
- 23. Saunders KW, Von Korff M, Pruitt SD, Moore JE. Prediction of physician visits and prescription medicine use for back pain. Pain 1999; 83: 369–77. [DOI] [PubMed] [Google Scholar]
- 24. Breen A, Austin H, Campion-Smith C, Carr E, Mann E. “You feel so hopeless”: a qualitative study of GP management of acute back pain. Eur J Pain 2007; 11: 21–9. [DOI] [PubMed] [Google Scholar]
- 25. Corbett M, Foster N, Ong BN. GP attitudes and self-reported behaviour in primary care consultations for low back pain. Fam Pract 2009; 26: 359–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wrapson W, Mewse AJ. Does the doctor or the patient control sick leave certification? A qualitative study interpreting patients’ interview dialogue. Fam Pract 2011; 28: 202–9. [DOI] [PubMed] [Google Scholar]
- 27. Schers H, Braspenning J, Drijver R, Wensing M, Grol R. Low back pain in general practice: reported management and reasons for not adhering to the guidelines in The Netherlands. Br J Gen Pract 2000; 50: 640–4. [PMC free article] [PubMed] [Google Scholar]
- 28. Schers H, Wensing M, Huijsmans Z, van Tulder M, Grol R. Implementation barriers for general practice guidelines on low back pain a qualitative study. Spine (Phila Pa 1976) 2001; 26: E348–53. [DOI] [PubMed] [Google Scholar]
- 29. Darlow B, Fullen BM, Dean S, Hurley DA, Baxter GD, Dowell A. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: a systematic review. Eur J Pain 2012; 16: 3–17. [DOI] [PubMed] [Google Scholar]
- 30. Darlow B, Dowell A, Baxter GD, Mathieson F, Perry M, Dean S. The enduring impact of what clinicians say to people with low back pain. Ann Fam Med 2013; 11: 527–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. McIntosh A, Shaw CF. Barriers to patient information provision in primary care: patients’ and general practitioners’ experiences and expectations of information for low back pain. Health Expect 2003; 6: 19–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Allegretti A, Borkan J, Reis S, Griffiths F. Paired interviews of shared experiences around chronic low back pain: classic mismatch between patients and their doctors. Fam Pract 2010; 27: 676–83. [DOI] [PubMed] [Google Scholar]
- 33. Chew-Graham C, May C. Chronic low back pain in general practice: the challenge of the consultation. Fam Pract 1999; 16: 46–9. [DOI] [PubMed] [Google Scholar]
- 34. Croft PR, Macfarlane GJ, Papageorgiou AC, Thomas E, Silman AJ. Outcome of low back pain in general practice: a prospective study. BMJ 1998; 316: 1356–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Thorne S, Kirkham SR, MacDonald-Emes J. Interpretive description: a noncategorical qualitative alternative for developing nursing knowledge. Res Nurs Health 1997; 20: 169–77. [DOI] [PubMed] [Google Scholar]
- 36. Hunt MR. Strengths and challenges in the use of interpretive description: reflections arising from a study of the moral experience of health professionals in humanitarian work. Qual Health Res 2009; 19: 1284–92. [DOI] [PubMed] [Google Scholar]
- 37. Thorne S, Kirkham SR, O’Flynn-Magee K. The analytic challenge of Interpretative Description. Int J Qual Methods. 2004; 3 (1): Article 1. [Google Scholar]
- 38. Houben RM, Vlaeyen JW, Peters M, Ostelo RW, Wolters PM, Stomp-van den Berg SG. Health care providers’ attitudes and beliefs towards common low back pain: factor structure and psychometric properties of the HC-PAIRS. Clin J Pain 2004; 20: 37–44. [DOI] [PubMed] [Google Scholar]
- 39. Thorne S. Data analysis in qualitative research. Evidence Based Nursing. 2000; 3 (3): 68–70. [Google Scholar]
- 40. Morse JM, Barrett M, Mayan MJ, Olsen K, Spiers J. Verification strategies for establishing reliability and validity in qualitative research. Int J Qual Methods 2002; 1 (2): 13–22. [Google Scholar]
- 41. Lincoln YS, Guba EG. Naturalistic Inquiry. Beverly Hills, CA: Sage Publications, 1985, p. 416. [Google Scholar]
- 42. Pande MM. General practice in urban and rural New Zealand: results of the 2007 RNZCGP membership survey. J Prim Health Care 2009; 1: 108–13. [PubMed] [Google Scholar]
- 43. Klaber Moffett JA, Newbronner E, Waddell G, Croucher K, Spear S. Public perceptions about low back pain and its management: a gap between expectations and reality? Health Expect 2000; 3: 161–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Grol R, Dalhuijsen J, Thomas S, Veld C, Rutten G, Mokkink H. Attributes of clinical guidelines that influence use of guidelines in general practice: observational study. BMJ 1998; 317: 858–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Marriott S, Palmer C, Lelliott P. Disseminating healthcare information: getting the message across. Qual Health Care 2000; 9: 58–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Michie S, Johnston M. Changing clinical behaviour by making guidelines specific. BMJ 2004; 328: 343–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hoy D, Bain C, Williams G, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum 2012; 64: 2028–37. [DOI] [PubMed] [Google Scholar]
- 48. Kendall NA, Linton SJ, Main CJ. Guide to Assessing Psychosocial Yellow Flags in Acute Low Back Pain: Risk Factors for Long-Term Disability and Work Loss. Wellington, NZ: Accident Compensation Corporation and the New Zealand Guidelines Group, 1997. [Google Scholar]
- 49. Tracey I, Mantyh PW. The cerebral signature for pain perception and its modulation. Neuron 2007; 55: 377–91. [DOI] [PubMed] [Google Scholar]
- 50. Slade SC, Molloy E, Keating JL. The dilemma of diagnostic uncertainty when treating people with chronic low back pain: a qualitative study. Clin Rehabil 2012; 26: 558–69. [DOI] [PubMed] [Google Scholar]
- 51. Abenhaim L, Rossignol M, Gobeille D, Bonvalot Y, Fines P, Scott S. The prognostic consequences in the making of the initial medical diagnosis of work-related back injuries. Spine (Phila Pa 1976) 1995; 20: 791–5. [DOI] [PubMed] [Google Scholar]
- 52. Verbeek J, Sengers MJ, Riemens L, Haafkens J. Patient expectations of treatment for back pain: a systematic review of qualitative and quantitative studies. Spine (Phila Pa 1976) 2004; 29: 2309–18. [DOI] [PubMed] [Google Scholar]
- 53. Lillrank A. Back pain and the resolution of diagnostic uncertainty in illness narratives. Soc Sci Med 2003; 57: 1045–54. [DOI] [PubMed] [Google Scholar]
- 54. Dima A, Lewith GT, Little P, Moss-Morris R, Foster NE, Bishop FL. Identifying patients’ beliefs about treatments for chronic low back pain in primary care: a focus group study. Br J Gen Pract 2013; 63: e490–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.