Abstract
Background.
Older populations often suffer from multimorbidity and guidelines for each condition are often associated with recommended drug therapy management. Yet, how different and specific multimorbidity is associated with number and type of multi-drug therapies in general populations is unknown.
Aim.
The aim of this systematic review was to synthesize the current evidence on patterns of multi-drug prescribing in family practice.
Methods.
A systematic review on six common chronic conditions: diabetes mellitus, cardiovascular disease, cerebrovascular disease, chronic obstructive pulmonary disease (COPD), osteoarthritis and depression was conducted, with a focus on studies which looked at any potential combination of two or more multimorbidity. Studies were identified from searches of MEDLINE, EMBASE, PsychINFO, the Allied and Complementary Medicine Database (AMED) and the Health Management Information Consortium (HMIC) databases from 1960 to 2013.
Results.
A total of eleven articles were selected based on study criteria. Our review identified very few specific studies which had explicitly investigated the association between multimorbidity and multi-drug therapy. Relevant chronic conditions literature showed nine observational studies and two reviews of comorbid depression drug treatment. Most (seven) of the articles had focused on the chronic condition and comorbid depression and whether antidepressant management had been optimal or not, while four studies focused on other multimorbidities mainly heart failure, COPD and diabetes.
Conclusions.
Very few studies have investigated associations between specific multimorbidity and multi-drug therapy, and most currently focus on chronic disease comorbid depression outcomes. Further research needs to identify this area as key priority for older populations who are prescribed high levels of multiple drug therapy.
Keywords: Chronic disease, COPD, depression, drug therapy, multimorbidity, osteoarthritis.
Introduction
In recent decades the prevalence of chronic medical conditions has increased as a result of increased proportion of elderly people (1), which in consequence is associated with high impact on health care. Using a national primary care database in Scotland, a recent work by Barnett et al. (2) found that 23% of patients had ‘multimorbidity’ and 8% had physical and mental health multimorbidity. Salisbury et al. (3) in England showed that patients with multimorbidity (based on Quality and Outcomes Framework) had 9.4 primary care consultations per year compared with 3.8 among those without multimorbidity. Managing of the rising prevalence of multimorbidity is a challenge and there are increasing needs for health care systems to address the needs of such patients (4).
Patients with multimorbidity are more likely to have multi-drug therapy (5). Previous research has shown that multiple drug treatments are common in the older population (6,7). In England, the average number of medicines prescribed for each person per year has increased by 53.8% from 11.9 (in 2001) to 18.3 (in 2011) (8) and one in six patients over the age of 65 receives 10 drugs or more (9). Treatments for multiple conditions may interfere with each other, leaving those patients particularly vulnerable to adverse events (4). Strict adherence to the individual guidelines for each of the chronic condition does not always equate to optimal care, and on the contrary, may be associated with adverse effects in form of multiple side effects of medication, drug interactions, poor drug compliance and often an impracticable self-care regimen (10). Clinicians may also find it difficult to manage individuals with multiple chronic conditions. One such complexity may arise when a drug that improves one chronic disease is found to worsen another. In these scenarios, clinicians often have to set priorities in managing patients with multimorbidity (11).
Guidelines for the care of chronic conditions are disease-specific (4) and yet most do not take into account of patients who also have multimorbidity (12). Examples of this focus are the development of several National Service Frameworks in the UK for chronic disease management, for instance, diabetes. Such guidelines rarely modify or discuss the applicability of their recommendations for patients with multiple chronic conditions. Furthermore, they often fail to acknowledge the potential problems of multiple drug therapy among this group of patients (8).
Multi-drug therapy in this concept, we would propose that is defined as the specific use of two or more drugs for two or more chronic conditions in an individual. This term is distinct to the broader term ‘polypharmacy’, which has been variably applied to this concept and has been defined as ‘the administration of more medicines than are clinically indicated, representing unnecessary drug use’ (13–15). Often many of polypharmacy studies are limited to older people (9), and do not take into account other younger age groups that could also have the problem of multi-drug therapy and for different conditions. Based on this key gap in the literature, we undertook a systematic review to identify current studies investigating multi-drug therapy in patients with specific chronic condition multimorbidity.
We selected six common chronic conditions in general populations, which are associated with specific drug treatments as part of routine guidelines. The first group of three concordant diseases were cardiovascular diseases, cerebrovascular disease and diabetes mellitus. The other three discordant conditions were chosen empirically were chronic obstructive pulmonary disease (COPD), osteoarthritis (OA) and depression. The management and related drug treatments for each of these common chronic conditions are defined by specific guidelines, such as those developed by the National Institute for Clinical Excellence (NICE) in the UK (16,17). The concordant diseases share common pathological or causal links and have common drug interventions, while, the discordant conditions are major causes of morbidity, physical disability and psychological distress in general population. All six chronic condition examples are common reasons for consulting in general practice and as a result are likely to be the common multimorbid examples encountered in general practice. Therefore, using these six examples with implicit use of drug management as a key intervention in guidelines, we undertook a systematic review to identify studies on the patterns of multi-drug therapy in those specific multimorbidity examples.
Methods
Search strategy and data sources
The electronic search of five databases included MEDLINE, EMBASE, PsychINFO, the Allied and Complementary Medicine Database (AMED) and the Health Management Information Consortium (HMIC). The National Health Service (UK) database was used for all except the MEDLINE search which was conducted using the OVID database interface. Searches were limited to articles in English published between 1960 and October 2013. Studies on at least two of the selected chronic conditions that had investigated drug management in adults aged 18 years and over in primary or secondary care settings were included. Since there were no standard terms to identify ‘multiple drug therapy’, different search strategies were employed and tested, which led to the final single search strategy shown in the online supplementary material.
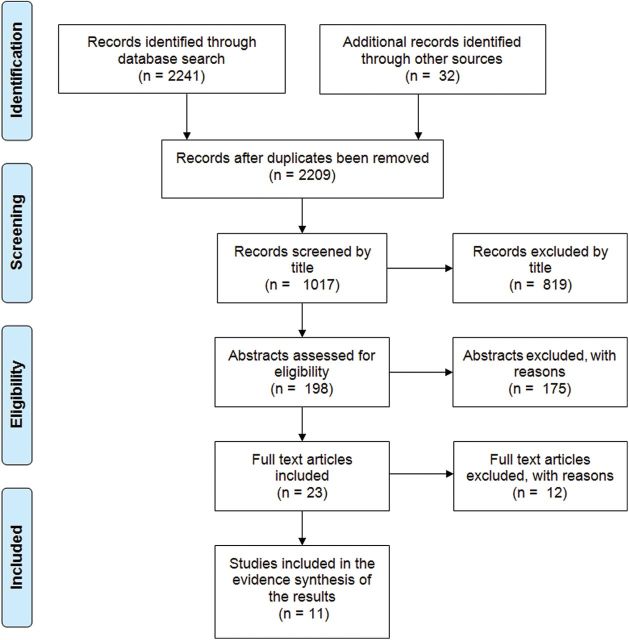
The search strategy was further expanded by examining the names of authors whose papers we had already retrieved; for each author we searched through all their publications to see if they had published other relevant papers for inclusion. Unpublished manuscripts and book chapters were not included in the search. Additional searches included Bibliography and reference list checking of key articles, hand searching of key journals, and online key web-sites (e.g. Department of Health (UK) and NICE) and experts were contacted. The flowchart for studies identified using PRISMA guidelines is reported in Fig. 1.
Figure 1.
Flowchart of article selection process.
Article selection and data extraction
The study inclusion were: (i) quantitative studies which had focused on drug therapy in patients with at least one of cardiovascular disease, cerebrovascular disease, diabetes mellitus, COPD, OA or depression, (ii) studies of adults aged 18 years and over, (iii) studies conducted in primary care or community settings and (iv) articles in English with full text available. Exclusion of studies was based on (i) age <18 years, (ii) studies outside of the clear pre-defined conditions (specifically on dementia, asthma, arthralgia and psychosis) and (iii) studies reported in non-English language. The full study reports were examined when citation titles or abstracts did not contain sufficient detail. When there were multiple reports, the study with the most recent and complete data was selected. If there were any discrepancies in selected papers between the two reviewers (LD and EOR), a third reviewer (UTK) independently reviewed the papers and through discussion, obtained a consensus.
Two reviewers independently extracted data for each study in terms of study design, study participants and their characteristics, type of intervention, type and method of outcome measurements and results. Included articles underwent a methodological quality and risk of bias assessment using the Critical Appraisal Skill Program (CASP) checklists for observational studies (18). However, only a few articles were identified and found to be very heterogeneous, and while the CASP list ensured structured data extraction, it did not provide cross-comparison in terms of quality, and so a narrative synthesis was undertaken (19).
Results
From a total of 1017 articles identified from the initial search of all databases, 198 abstracts were screened and after consensus review 23 papers were assessed, of which 11 studies met the inclusion criteria. A summary of the steps for screening the articles and the selection process is described in Fig. 1.
Characteristics of included studies
The 11 studies were published between 2003 and 2010. Of the 11 studies, nine were observational and there were two reviews of literature. Most of the articles (seven) focused on comorbid depression and chronic diseases and the risks and challenges of managing this group of patients. One study had examined specific ‘polypharmacy’ among elderly patients with multimorbidity (20). Another study focused on beta-blocker prescribing in patients with comorbid COPD and heart failure (21), one study had examined the drug management of post-acute myocardial infarction (AMI) in patients with other chronic medical conditions (22) and one study examined the association between comorbidity and trends in the prevalent and initial use of certain antihypertensives (23). The two systematic reviews (24,25) identified in our review; one was an extensive 12-year search of current evidence on the epidemiology of chronic diseases coexisting with depression while the other review highlighted the evidence about the under recognition, under diagnosis and under treatment of depression in patients with coexisting chronic diseases. Summary of study design, settings, sample, methods of measuring outcome and main findings is presented in Table 1.
Table 1.
Description and analysis of studies included in the review
| Author | Setting/context | Participants | Outcomes | Results |
|---|---|---|---|---|
| Bogner et al. (26), USA | Cross-sectional study in primary care. Data was collected using self-report from questionnaires and in-home interviews | 355 patients aged 65–92 (mean age 75.3 years) with varying degrees of depressive symptoms | Self-reported cardiovascular disease defined as heart failure, MI, stroke, angioplasty Physicians assessment of depression at the index visit and its management |
Patients reporting heart failure were more likely to be identified as depressed compared to those that did not report heart failure (OR = 2.34, 95% CI: 1.13–4.85) Older adults reporting heart failure were less likely to receive treatment for depression compared to those who did not report heart failure |
| Sales et al. (22), USA | Exploratory analysis of 1240 post-AMI patients from 139 physician practices. The authors used a pre-existing framework of care for patients with pre-existing comorbidities that suggests the effects of these conditions is related to treatment guidelines and symptoms experienced by patients | 1240 ambulatory post- AMI adult patients. Mean age 74 years and mean comorbidity was 2 | Effect of concordant (similar pathology as AMI and no conflict of drug treatment) comorbid conditions on guideline-defined AMI care Effects of symptomatic (conditions with different pathology or conflicts of drug treatment) comorbid conditions on guideline- defined AMI care |
Positive association between concordant and symptomatic conditions and guideline compliance (0.32 and 0.14, respectively; P < 0.001 for each) Highly concordant comorbid conditions was associated with a higher adherence to guideline- defined AMI care Highly symptomatic comorbid conditions was associated with a lower adherence to guideline- defined AMI care |
| Katon et al. (27), USA | Survey—consultation linkage of automated records from a Health Maintenance Organization with a focus on detection and care of patients with diabetes mellitus and comorbid depression. Study based in primary care | Questionnaires were sent to 9063 patients, 7841 eligible and 4385 had adequate data and consented to medical records review. Mean age of 59 years | Quality of depression care in a population-based sample of patients with diabetes and major depression. Proportion of the depressed patients identified as depressed 12 months prior to survey from medical records Proportion of depressed diabetic patients on adequate treatment for depression, i.e. adequate dose of antide pressants, at least four sessions of psychotherapy. |
Less than half (43%) of patients with diabetes received adequate care for their depression. Adequate care as defined by therapy with an antidepressant for >90 days at an adequate dose or at least four psychotherapy sessions in a 12-month period |
| Koenig (28), USA | Questionnaire survey of 422 physicians caring for older depressed patients in primary or secondary care | Physicians caring for 1000 depressed patient with congestive heart failure or chronic pulmonary disease during hospitalization or after discharge. Patients were aged 50 years or over | Physician attitudes regarding the management of depression in older medical patients Physicians reasons for not initiating antidepressant therapy or referring depressed patients to specialists |
48% of physicians initiated depression treatment, 14% referred for counselling and 11% referred to a psychiatrist. Most common reason for not initiating treatment was patients’ resistance to treatment due to stigma linked to depression. Others included— ‘pressing medical issues’, ‘unsure of diagnosis’ or ‘poorly prepared to treat’ |
| Corsonello et al. (20), Italy | Analysis of pre-existing hospital/ community-based data from a large observational study group in Italy | 2465 patients enrolled in the Gruppo Italiano di Farmacovigilanza nell’Anziano study group—all age study group but 1626 (65.9%) of the patients were older than 65 years | Proportion and characteristics of patients having >6 drugs at discharge. Multiple drug therapy was defined as >6 drugs at discharge from the hospital |
57.4% of patients had increased numbers of drugs at discharge and this was strongly correlated with multimorbidity—diabetes mellitus, congestive cardiac failure, COPD, depressive symptoms and renal insufficiency (OR = 4.32, 95% CI: 1.4–2.32); multiple drug therapy prior to admission (OR = 4.32, 95% CI: 3.13–5.96). |
| Gill et al. (29), USA | Secondary data analysis of electronic health record data was conducted in the Centricity Health Care User Research Network (CHURN) | 209 family medicine and general internal medicine providers in 40 primary care CHURN offices in 17 US states 1513 adults with a new episode of depression that had been diagnosed during the period October 2006 through July 2007 |
Prescription of antidepressant medication and doses of antidepressant medication were compared for patients with and without six comorbid conditions: diabetes, coronary heart disease, congestive heart failure, cerebrovascular disease, COPD and cancer | After controlling for age and sex, patients with multiple chronic conditions were less likely to be prescribed antidepressant medication (adjusted OR = 0.58; 95% CI: 0.35–0.96), but there was no significant difference by individual comorbidities. Patients with cerebrovascular disease were less likely to be prescribed a full dose of medication. There was no difference for any comorbidities in the prescription of minimally effective doses |
| Hawkins et al. (21), Scotland | Cross-sectional analysis of data from 61 primary care clinics in the Scottish continuous morbidity recording scheme. Data was collected from review of medical and prescription records. The authors examined and reported disease prevalence of coexisting COPD and heart failure as well as beta-blocker usage in these patients | Analysis of a total of 377439 patients’ records within the Scottish continuous morbidity recording scheme | Beta-blocker prescribing in patients with comorbid COPD and heart failure | Low OR = 0.3 (0.28–0.32), P = 0.001, beta-blocker prescribing in patients with COPD and heart failure. More patients with HF were prescribed beta-blockers if they did not have COPD (41%) compared to having COPD (18%) |
| Clarke and Currie (24), Australia | Systematic review of literature including guidelines from 1995 to 2007 with particular focus on the epidemiology and management of depression in patients with specific chronic diseases | 159 reviews were identified. The review examined the pharmacological and non-pharmacological therapy effective for treating depression and anxiety, coexisting with certain chronic diseases—stroke, asthma, heart disease, diabetes mellitus, cancer, arthritis and osteoporosis | Strong evidence for association of physical illness and depression suggests modelling guides that integrate care for patients with comorbid depression and chronic diseases | Drugs and non-pharmacological treatment are effective for treating depression in certain chronic diseases from current evidence |
| Egede and Simpson (25), Italy | A review of literature on the epidemiology treatment and costs of depression in type 2 diabetic patients | Systematic review of literature | Review of current evidence on the epidemiology and treatment of depression where it coexists with diabetes mellitus | Prevalence of multimorbidity of depression and diabetes was 10–30% from the review. Recognition and treatment of depression in primary care is less than optimal as only 50% of diabetic and depressed patients are treated in primary care. Selective serotonin reuptake inhibitors is preferred treatment in this group of patients |
| Gill et al. (30), USA | Cross-sectional study using secondary data from a national health record network of outpatient electronic medical record users | 5000 physicians in primary care. Participants included adult patients with an active diagnosis of depression. Four comorbidities were defined: diabetes, coronary heart failure, stroke and cancer | To compare antidepressant use in patients with and without multimorbidity | After controlling for age and gender, antidepressant treatment was significantly more likely for patients with diabetes (OR = 1.07, 95% CI: 1.03–1.11) but significantly less likely for patients with Coronary Heart Disease (OR = 0.94, 95% CI 0.90–0.99) |
| Greving et al. (23), The Netherlands | Cross-sectional study over 5-year period. Data was obtained from the integrated primary care information database (IPCI) which contains medical records of >100 GP in the Netherlands | All adults aged >18 years who had at least 6 months registration with their GP. All patients with either IPCI- coded diagnosis of hypertension or hypertension in the patient diary | To examine the association between comorbidity and trends in the prevalent and initial use of ACE-I and ARBs | The overall prevalence of ACE-I increased from 33% to 41% in hypertensive patients with diabetes, HF, proteinurea and/ or renal insufficiency. ACE-I were significantly more likely to be prescribed than classic hypertensives to patients with diabetes, HF and/or hypercholesterolaemia. Trends in prevalent use of ARB did not differ between patients with or without comorbidity |
CI, confidence interval; OR, odds ratio.
Chronic conditions and depression multimorbidity
Seven of the identified articles have focused on the drug therapy for depression coexisting with chronic diseases, such as cardiovascular disease and diabetes mellitus. Most of these studies (five) (25–29) have reported suboptimal treatment and very low recognition of depression in patients with chronic diseases and the high risk of drug side effects in this category of patients was also emphasized. For instance, Gill et al. (29) have found that patients with cerebrovascular disease were less likely to be prescribed a full dose of antidepressants after adjustment for age and gender. The authors concluded that patients presented to a primary care practice with new episodes of depression were treated less aggressively if they have multiple medical comorbidities. However, another study by Gill et al. (30) found that antidepressant treatment was significantly more likely for patients with diabetes but not significantly less likely for those with coronary heart disease.
A study by Koenig (28) examined physician’s attitudes towards identification and treatment of depression in a group of medical patients admitted to hospital. The study reported a low rate of diagnosis and treatment of depression in this group of patients. Physicians’ concern about treatment interaction was among the common reasons reported by physician for not treating these patients (58.8%).
Two systematic reviews (24,25) on comorbid depression were identified in our review. Clarke and Currie (24) reviewed pre-existing literature and clinical practice guidelines on the management of depression in patients with chronic conditions. A total of 159 studies were examined from 1995 to 2007. Their review highlighted the paucity of studies on the management of depression and chronic diseases, stressed the strong evidence for the association of physical illness and depression and recommended modelling guidelines to integrate care for patients with comorbid depression and chronic diseases.
Egede and Simpson (25) reviewed the literature on the epidemiology and treatment of depression in adults with type 2 diabetes. The review found that the recognition and treatment of comorbid depression was low in primary care (50%) and recommended that efforts should be aimed at optimizing the diagnosis and treatment of depression in diabetics.
Multimorbidity without depression
Only four primary studies had investigated multimorbidity with multi-drug therapy unrelated to depression. Corsonello et al. (20) used large data from community and university hospitals in Italy. They found that selected chronic diseases (diabetes, heart failure, COPD, renal insufficiency and depression) were a strong correlate of multiple drug treatments in elderly patients at discharge from the acute care hospital. They found that 57% of patients had the number of drugs increased at discharge with respect to the month prior to admission. They also observed that more drugs were taken among patients having >4 conditions.
An analysis of cross-sectional data from 61 primary care centres was conducted by Hawkins et al. (21) with the aim of investigating the treatment of HF in patients with COPD. While beta-blocker is now recommended for heart failure patients, the study reported that the use of beta-blockers in patients with COPD was suboptimal (<20%). Only 18% of patients with HF and COPD were prescribed beta-blockers compared to 41% of those without COPD and this has not improved over the 5-year study period despite the overall improvement in the trend of prescribing beta-blockers. Patients with COPD were more frequently (33%) prescribed calcium channel blockers compared to those without COPD (27%).
Greving et al. (23) examined the association between comorbidity and trends in the prevalent and initial use of angiotensin-converting enzyme inhibitors (ACE-I) and angiotensin II receptors blockers (ARBs) among adults with diagnosis of hypertension. The authors found that the overall prevalence of ACE-I increased from 33% to 41% in hypertensive patients with diabetes, HF, proteinurea and/or renal insufficiency. ACE-I were significantly more likely to be prescribed than classic antihypertensives to patients with diabetes, HF and/or hypercholesterolaemia. However, trends in the prevalent use of ARB did not differ between hypertensive patients with or without comorbidity.
Sales et al. (22) tested provider adherence to guidelines in the presence of comorbidity in post-AMI patients. The study used a standard framework to investigate how care compared post-AMI for the coexisting morbidities based on whether or not these coexisting illnesses were symptomatic or asymptomatic and concordant or not. They found that concordance of comorbidities and symptomatic scores increased the likelihood that patients received treatments recommended by guidelines for ischemic heart disease; even after controlling for confounding factors such as age, sex and race. The authors concluded that the presence of multimorbidity in an individual patient may alter the optimal approach of treatment to each of these conditions for the same patient and recommended the use of a framework that prioritizes treatments without being centred on a single condition.
Discussion
Multimorbidity is common in older adults, but using the six selected and common chronic conditions, very few studies have investigated the relationship between multimorbidity and prescribed multiple drug therapy. Our review highlights that the key evidence available is on chronic conditions and depression, which is associated with suboptimal drug treatment in multiple drug therapy. However there is a significant evidence gap in the current evidence on the patterns of multimorbidity and related multi-drug therapy. Such evidence is going to be crucial in the future for health care professionals to effectively manage these patients who currently form a large proportion of the patient population, and in ageing populations the scale of this as a problem issue will become even more significant.
Main findings
Our systematic review indicated that there are very few studies on prescribed drug therapy for individuals with multimorbidity, but most of the current evidence for the link between multimorbidity and multi-drug therapy is where the multimorbidity is defined by one chronic condition and the other by depression (25). The outcome from these studies was variable but the majority highlighted suboptimal drug treatment of depression in patients with multimorbid with at least one other chronic disease. These findings show that GPs might moderate their antidepressant prescribing in chronic conditions, which suggests potential adaptation of guidelines to suit the situation in each individual. There were few other multimorbid examples, which looked at suboptimal prescribing (heart failure and COPD), levels of multimorbid prescribing (cardiovascular and renal status) and adherence to guidelines given multimorbid status (in AMI patients). As far as one is able to draw implications from these isolated studies, they show conflicts can occur in multimorbidity resulting in suboptimal treatment (beta-blocker use in heart failure for those with COPD) (31), but guidelines can overcome potential conflicts as a result of multimorbid status (ACE-I use in renal dysfunction) (32).
What this review adds
While it is increasingly known that the multiple drug prescribing is common, this has not fully translated into the evidence on the relationship between multimorbidity and multi-drug therapy and how this relates to patient and clinical outcomes.
An ageing population with a high proportion of patients living with multiple chronic conditions has become the norm in general practice. Guidelines exist for the optimal management of individual chronic diseases and in the UK, financial incentives often exist for GPs that follow these guidelines and ensure optimal treatment of individual chronic diseases. The challenge, however, is managing patients with multimorbidity. Current evidence shows that the management of these patients does not always equate to the optimal treatment of each of their chronic diseases (9). On the contrary, this approach may be harmful to the patients because of problems arising from multiple drug interactions and often the impracticality of having to abide by multiple treatment regimes. The literature suggests that the risk of adverse drug reactions increases with the increase of number of medications used by the same patient due to undesirable combination of drugs (7,33).
As multiple drug prescribing increases with the increase in number of chronic conditions (34), this puts patients with multimorbidity at a higher risk. Calderón-Larrañaga et al. (35) found that multimorbidity is associated with adverse drug reactions due to prescription of multiple drugs by different specialties. The authors argued that with the clinical complexity of multimorbidity, patients need interventions by different specialists which require coordination of care. This all adds to the potential burden of care for such patients when multiple drug therapy is prescribed for each individual condition (34) and could lead to potential interactions between prescribed medications and consequent adverse drug events (35). Yet, there is no clear guidance as to the best approach towards the optimal treatment of patients with multimorbidity which presents a challenge to health care systems. Clinicians accordingly have limited guidance or evidence on how to integrate care decisions for patients with multiple chronic conditions (36).
Therefore, health care professionals need to consider this potential burden and support patients in prioritizing management strategies (34). There is a strong demand to implement efficient and cost-effective models of integrated care based on the principles of management of multiple chronic conditions (24).
The emphasis of the majority of the studies identified in this review has been chronic diseases comorbid with depression. Although depression is common in patients with chronic diseases, there are still a large proportion of patients with multimorbidity without depression. This could be because the multiple diseases have similar aetio-pathogenesis, e.g. cardiovascular diseases, cerebrovascular diseases and diabetes mellitus or because the diseases just coexist in one patient, e.g. diabetes mellitus and OA. All patients with multimorbidity, irrespective of and underlying causal link or not, will require systems and management pathways that will ensure that their multiple diseases are treated optimally in a way that is safe, cost effective and practical.
Limitations of this review
Our systematic search review examined five major databases and used a broadest possible strategy to ensure that and studies investigating two or more specified chronic conditions and related drug treatments were identified. The individual articles were systematically examined using a standardized appraisal tool with three independent appraisers.
Despite this rigorous approach it is possible that publication bias and outcome reporting bias may be inherent limitations to our results. The key challenge for this systematic literature review was the potential over-lap between the concept of multiple drug therapy and the current use of specific term of ‘polypharmacy’ which has been assumed to cover the former concept. However, here polypharmacy studies tend to focus often on the older persons or specific drug numbers or even incorporating definitions of safety. The distinction in this systematic review was to focus on broader issue of guideline-driven multiple drugs prescribing in younger to mid-life populations with chronic conditions. In terms of the approach we took for framing the search, the individual chronic conditions were initially cross-referenced with the large literature on drug treatments. However, when the focus of the specific link between drug treatments to the multimorbidity (combination of two or more of the specified conditions) was introduced, a significant gap in the literature was identified. This gap includes both the use of consistent terminology as well as specific studies which investigate the disease interaction (multimorbidity), drug interaction (multi-drugs) and clinical outcomes over a long-term follow-up. In the light of the nature of the research topic, a narrative synthesis was conducted to discuss the results as the studies were heterogeneous to allow for a formal quality appraisal. This approach could imply the loss of additional information that would be available about the quantitative power of the individual studies and statistical significance of any observed effect, which could not be estimated.
Conclusions
Our review has showed that there are very few studies investigating the drug management of patients with multimorbidity. It emphasizes the gap in evidence which addresses the management of chronic disease comorbidities and prescribed drug therapies.
There is an imperative that future research addresses the issue of multi-drug prescribing and develops methods on pharmaco-epidemiology in multimorbidity. Health care professionals will need to further develop ways in which to assess and best manage patients with multiple morbidities in order to deliver clinically appropriate, safe and cost-effective health care to an ever increasing population of patients with multiple chronic conditions.
Future research into the management of patients with multimorbidity which focuses on current drug treatment and seeks to propose clinically effective and practical ways to manage this group of patients is essential in order to ensure appropriate delivery of patient care and to avoid duplication and wastage which could arise from treating individual chronic disease separately. This issue has become a clinical priority.
Supplementary material
Supplementary material is available at Family Practice online.
Declaration
Funding: National Institute for Health Research (NIHR) In-Practice Fellowship (NIHR:IAT 09/1-PF/019) for EOR.
Ethical approval: none.
Conflict of interest: All authors of this research paper have no competing interests.
Supplementary Material
Acknowledgements
This report presents independent research commissioned by the NIHR. The views expressed are those of the authors and not necessarily those of the National Health Service, the NIHR or the Department of Health. They have directly participated in the planning and execution of this study and have read and approved the final version submitted.
References
- 1. van den Akker M, Buntinx F, Metsemakers JF, Roos S, Knottnerus JA. Multimorbidity in general practice: prevalence, incidence, and determinants of co-occurring chronic and recurrent diseases. J Clin Epidemiol 1998; 51: 367–75. [DOI] [PubMed] [Google Scholar]
- 2. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study The Lancet 2012; 6736(12): 60240–2. [DOI] [PubMed] [Google Scholar]
- 3. Salisbury C, Johnson L, Purdy S, Valderas JM, Montgomery AA. Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract 2011; 61: e12–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bayliss EA, Edwards AE, Steiner JF, Main DS. Processes of care desired by elderly patients with multimorbidities. Fam Pract 2008; 25: 287–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wehling M. Multimorbidity and polypharmacy: how to reduce the harmful drug load and yet add needed drugs in the elderly? Proposal of a new drug classification: fit for the aged. J Am Geriatr Soc 2009; 57: 560–1. [DOI] [PubMed] [Google Scholar]
- 6. Junius-Walker U, Theile G, Hummers-Pradier E. Prevalence and predictors of polypharmacy among older primary care patients in Germany. Fam Pract 2007; 24: 14–9. [DOI] [PubMed] [Google Scholar]
- 7. Veehof LJ, Stewart RE, Meyboom-de Jong B, Haaijer-Ruskamp FM. Adverse drug reactions and polypharmacy in the elderly in general practice. Eur J Clin Pharmacol 1999; 55: 533–6. [DOI] [PubMed] [Google Scholar]
- 8. Duerden M, Avery T, Payne R. Polypharmacy and medicines optimisation: making it safe and sound. The King’s Fund 2013. www.kingsfund.org.uk/publications (accessed December 2013). [Google Scholar]
- 9. Wise J. Polypharmacy: a necessary evil. BMJ 2013; 347: f7033. [DOI] [PubMed] [Google Scholar]
- 10. Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA 2005; 294: 716–24. [DOI] [PubMed] [Google Scholar]
- 11. Loza E, Jover JA, Rodriguez L, Carmona L; EPISER Study Group. Multimorbidity: prevalence, effect on quality of life and daily functioning, and variation of this effect when one condition is a rheumatic disease. Semin Arthritis Rheum 2009; 38: 312–9. [DOI] [PubMed] [Google Scholar]
- 12. Guthrie B, Payne K, Alderson P, McMurdo ME, Mercer SW. Adapting clinical guidelines to take account of multimorbidity. BMJ 2012; 345: e6341. doi:10.1136/bmj.e6341 [DOI] [PubMed] [Google Scholar]
- 13. Patterson SM, Hughes C, Kerse N, Cardwell CR. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Systemat Rev 2009; (4). [DOI] [PubMed] [Google Scholar]
- 14. Gnjidic D, Hilmer SN, Blyth FM, et al. Polypharmacy cutoff and outcomes: five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J Clin Epidemiol 2012; 65: 989–95. [DOI] [PubMed] [Google Scholar]
- 15. Bushardt RL, Massey EB, Simpson TW, Ariail JC, Simpson KN. Polypharmacy: misleading, but manageable. Clin Interv Aging 2008; 3: 383–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. National Institute for Health and Clinical Excellence (NICE). Type 2 diabetes: the management of type 2 diabetes (Update) 2010. http://guidance.nice.org.uk/CG66/Guidance/pdf/English (accessed 6 February 2012). [Google Scholar]
- 17. National Institute for Health and Clinical Excellence (NICE). Management of chronic obstructive pulmonary disease in adults in primary and secondary care (partial update, June 2010) NICE Clinical Guideline101. http://www.nice.org.uk/nicemedia/live/13029/49397/49397.pdf (accessed December 2013). [Google Scholar]
- 18. Critical Appraisal Skills Programme (CASP) 2013. http://www.phru.nhs.uk/Pages/PHD/CASP.htm (accessed 15 September 2013). [Google Scholar]
- 19. Jones M, Rait G, Falconer J, Feder G. Systematic review: prognosis of angina in primary care. Fam Pract 2006; 23: 520–8. [DOI] [PubMed] [Google Scholar]
- 20. Corsonello A, Pedone C, Corica F, Incalzi RA. Polypharmacy in elderly patients at discharge from the acute care hospital. Ther Clin Risk Manag 2007; 3: 197–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hawkins NM, Jhund PS, Simpson CR, et al. Primary care burden and treatment of patients with heart failure and chronic obstructive pulmonary disease in Scotland. Eur J Heart Fail 2010; 12: 17–24. [DOI] [PubMed] [Google Scholar]
- 22. Sales AE, Tipton EF, Levine DA, et al. Are co-morbidities associated with guideline adherence? The MI-Plus study of Medicare patients. J Gen Intern Med 2009; 24: 1205–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Greving JP, Denig P, van der Veen WJ, et al. Does comorbidity explain trends in prescribing of newer antihypertensive agents? J Hypertens 2004; 22: 2209–15. [DOI] [PubMed] [Google Scholar]
- 24. Clarke DM, Currie KC. Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence. Med J Aust 2009; 190 (suppl 7): S54–60. [DOI] [PubMed] [Google Scholar]
- 25. Egede LE, Simpson K. Epidemiology, treatment and costs of depression in adults with type 2 diabetes. Expert Rev Pharmacoecon Outcomes Res 2003; 3: 251–62. [DOI] [PubMed] [Google Scholar]
- 26. Bogner HR, Ford DE, Gallo JJ. The role of cardiovascular disease in the identification and management of depression by primary care physicians. Am J Geriatr Psychiatry 2006; 14: 71–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Katon WJ, Simon G, Russo J, et al. Quality of depression care in a population-based sample of patients with diabetes and major depression. Med Care 2004; 42: 1222–9. [DOI] [PubMed] [Google Scholar]
- 28. Koenig HG. Physician attitudes toward treatment of depression in older medical inpatients. Aging Ment Health 2007; 11: 197–204. [DOI] [PubMed] [Google Scholar]
- 29. Gill JM, Klinkman MS, Chen YX. Antidepressant medication use for primary care patients with and without medical comorbidities: a national electronic health record (EHR) network study. J Am Board Fam Med 2010; 23: 499–508. [DOI] [PubMed] [Google Scholar]
- 30. Gill JM, Chen YX, Lieberman MI. Management of depression in ambulatory care for patients with medical co-morbidities: a study from a national Electronic Health Record (EHR) network. Int J Psychiatry Med 2008; 38: 203–15. [DOI] [PubMed] [Google Scholar]
- 31. Swennen MH, Rutten FH, Kalkman CJ, van der Graaf Y, Sachs AP, van der Heijden GJ. Do general practitioners follow treatment recommendations from guidelines in their decisions on heart failure management? A cross-sectional study. BMJ Open 2013; 3: e002982. doi:10.1136/bmjopen-2013–002982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rushton CA, Strömberg A, Jaarsma T, Kadam UT. Multidrug and optimal heart failure therapy prescribing in older general practice populations: a clinical data linkage study. BMJ Open 2 January 2014; 4(1):e003698. doi:10.1136/bmjopen-2013–003698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kadam UT. Potential health impacts of multiple drug prescribing for older people: a case-control study. Br J Gen Pract 2011; 61(583):128–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Teljeur C, Smith SM, Paul G, Kelly A, O’Dowd T. Multimorbidity in a cohort of patients with type 2 diabetes. Eur J Gen Pract 2013; 19: 17–22. [DOI] [PubMed] [Google Scholar]
- 35. Calderón-Larrañaga A, Poblador-Plou B, González-Rubio F, Gimeno-Feliu LA, Abad-Díez JM, Prados-Torres A. Multimorbidity, polypharmacy, referrals, and adverse drug events: are we doing things well? Br J Gen Pract 2012; 62: e821–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Boyd C, Fortin M. Future of Multimorbidity research: how should understanding of multimorbidity inform health system design? Public Health Reviews 2010; 32: 451–74. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.