Abstract
Empirically supported psychological therapies have been developed for many mental health conditions. However, in most countries only a small proportion of the public benefit from these advances. The English Improving Access to Psychological Therapies (IAPT) program aims to bridge the gap between research and practice by training over 10,500 new psychological therapists in empirically supported treatments and deploying them in new services for the treatment of depression and anxiety disorders. Currently IAPT treats over 560,000 patients per year, obtains clinical outcome data on 98.5% of these individuals and places this information in the public domain. Around 50% of patients treated in IAPT services recover and two-thirds show worthwhile benefits. The clinical and economic arguments on which IAPT is based are presented, along with details of the service model, how the program was implemented, and recent findings about service organization. Limitations and future directions are outlined.
Keywords: psychological therapies, dissemination, depression, anxiety disorders, outcome monitoring
1. Improved Prospects for People with Mental Health Problems
In recent decades considerable progress has been made in developing effective psychological therapies for a wide range of mental health problems (Lambert 2013, Nathan & Gorman 2015, Roth & Fonagy 2005). Various professional bodies (Australian Psychological Society, Division 12 of American Psychological Association Division 12), multi-disciplinary research networks (Cochrane Collaboration) and government organizations (NICE: the UK National Institute for Health and Care Excellence) have synthesized the research evidence and issued clinical guidelines recommending particular psychological treatments as evidence-based interventions for different mental health problems. Although the guidelines differ in some details (Moriana et al. 2017) there is a general consensus that empirically supported psychological treatments can have a major impact on mental health problems. For many conditions, psychological therapies can be considered as first line interventions, at least on a par with medication in the short-term and sometimes superior in the long-term (Hollon et al. 2006). Furthermore, a recent meta-analysis of patient preference surveys (McHugh et al. 2013) found that members of the public show a three-fold preference for psychological therapy, compared to medication. In view of these findings, one would expect empirically supported psychological therapies to be widely available in health care systems across the world. Unfortunately, that is not the case.
2. The Gap Between Science and Practice
In the United States (Marcus & Olfson 2010) and the United Kingdom (McManus et al. 2016) psychological therapies are used less often than medication and there is no Western country that reports patients are getting their preference with psychological therapies being more widely used than medication. Furthermore, when psychological therapies are available, they are often not those that are considered to be empirically supported (McHugh & Barlow 2012). For example, in the UK in 2007 it was estimated that 10% of adults with depression or anxiety disorders had some form of psychological therapy (McManus et al. 2009) but that less than 5% were receiving an empirically supported psychological therapy (Layard & Clark 2014 a, b).
Recently, the UK government has launched a programme that aims to overcome this problem and make empirically supported psychological treatments much more widely available within the National Health Service (NHS)
3. The English Improving Access to Psychological Therapies (IAPT) Program
3.1. Overview of the Program
The IAPT program aims to substantially increase access to psychological therapies for depression and anxiety disorders in England by training over 10,500 new therapists by 2021 and deploying them in new services for these conditions. The training follows national curricula and has initially particularly focused on cognitive-behaviour therapy (CBT), as this is where the manpower shortage was considered greatest. As the programme matures, training in other NICE recommended treatments for depression is also being made available. The clinical and other outcomes of patients who access the services are carefully monitored and reported on publically accessible websites (see below). From small beginnings in 2008 the programme has gradually grown to a point where it is now (in 2017) seeing over 960,000 people a year. Some people only receive an assessment and advice, or may be signposted elsewhere if their problems are considered more appropriate for a different type of service. However, around 60% (over 560,000 people) receive a course of treatment. The program uses a unique session-by-session monitoring system to record clinical outcomes and manages to capture pre-treatment and post-treatment depression and anxiety scores on 98.5% of patients who are seen at least twice before discharge. The most recently available data, which covers January to March 2017, shows that 51% of patients are judged to have recovered by the end of treatment, with approximately two out of three (66.3%) showing reliable improvement.
The current rate of access to IAPT services (960,000 patients per year) represents approximately 16% of the community prevalence of depression and anxiety disorders. The National Health Service Five Year Forward View for Mental Health (NHS England 2016a) commits the NHS to further expand access to 25% of prevalence (approx. 1.5 million people) by 2021.
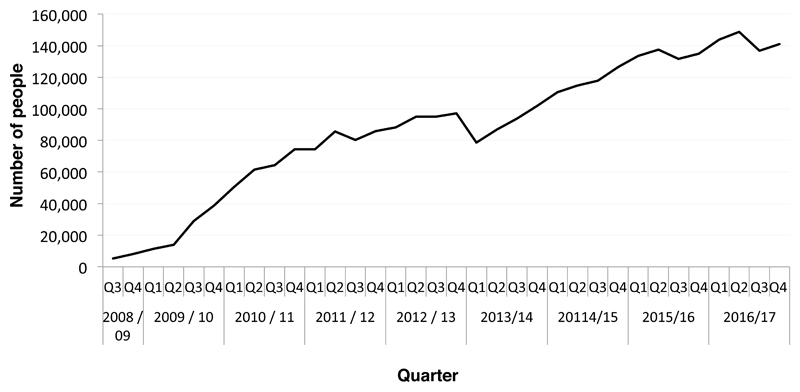
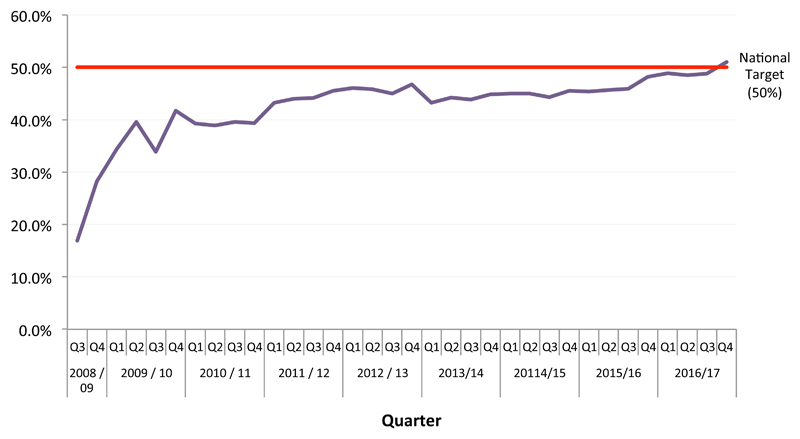
Figure 1 shows how the numbers of people who receive a course of treatment in IAPT services has increased since the start of the program, with the X axis representing each quarter year. Alan Johnson, who was the Minister for Health at the start of the IAPT initiative, stated that the program would aim to achieve recovery in 50% of treated patients. This target was based on the consensus view of a panel of clinical experts who considered what should be possible if the psychological therapies deployed in IAPT perform about as well as they have done in randomized controlled trials in more tightly controlled settings. Although some IAPT services achieved this ambitious target early in the program, Figure 2 shows that it has taken 8 years for the overall recovery rate to reach this level. Progress has been gradual. Services have learned from ongoing research into the determinants of service level variation in outcomes, have experimented with different delivery systems, and have benefited from a maturing workforce at both the clinician and leadership level. Further details of these developments will be provided later in the article.
Figure 1.
National number of people having a course of treatment (two or more sessions) in IAPT during each 3-month period (quarter) from the start of the program
Figure 2.
IAPT National recovery rate each 3 months (quarter) for people finishing a course of treatment (two or more sessions).
3.2. Which Therapies Are Available in IAPT Services?
IAPT services aim to deliver the psychological therapies that are recommended by the National Institute for Health and Care Excellence (NICE). The UK government established NICE as an independent organization that is charged with reviewing the evidence for treatments throughout medicine. Unlike some other bodies that issue clinical guidelines, NICE is not aligned to any professional group but instead draws on the expertise of all relevant professionals and also includes representation from patients. When NICE considers that there is sufficient evidence to show that certain treatments work, it issues a Clinical Guideline with recommendations about how the targeted condition should be treated within the NHS.
Starting in 2004, NICE systematically reviewed the evidence for the effectiveness of a variety of interventions for depression and anxiety disorders. These reviews led to the publication of a series of clinical guidelines (NICE 2004a, b; 2005a, b; 2006; 2009a, b; 2011; 2013) that strongly support the use of psychological therapies. Various specialized forms of CBT have the broadest indication as they are recommended for depression and all the anxiety disorders. Five other therapies (interpersonal psychotherapy, couples therapy, counselling, brief psychodynamic therapy, and mindfulness based cognitive therapy) are also recommended (with varying indications) for depression, but not for anxiety disorders. In the light of evidence that some individuals respond well to “low-intensity” interventions (such as guided self-help and computerized CBT) NICE also advocates a stepped-care approach to the delivery of psychological therapies in mild to moderate depression and some anxiety disorders. In moderate to severe depression and in some other anxiety disorders (such as post-traumatic stress disorder) low-intensity interventions are not recommended and instead it is suggested that patients should start by being offered “high-intensity” face-to-face psychological therapy. Table 1 summarizes the key the NICE recommendations that guide the delivery of treatment in IAPT services.
Table 1.
Summary of NICE’s Recommendations for the Psychological Treatment of Depression and Anxiety Disorders
| Place in Stepped Care Service | Disorder & NICE Clinical Guideline Numbers | Recommended Intervention |
|---|---|---|
|
Step 3: High intensity component of IAPT service (Primarily weekly, face-to-face, one-to-one sessions with a suitably trained therapist. In some disorders, such as depression, CBT can also be delivered effectively to small groups of patients. Couples therapy naturally involves the therapist, the depressed client and his/her partner). |
Depression: moderate to severe Depression: mild to moderate (CG90, CG91, CG123) |
CBT or IPT1, each with medication CBT or IPT1 Behavioural Activation (BA) 1,2 Couples Therapy3 Counselling for Depression1 Brief psychodynamic therapy1 |
| Depression Relapse Prevention (CG123) |
CBT4 Mindfulness based CT4 |
|
| Panic disorder (CG 113, CG123) |
CBT | |
| Generalised Anxiety Disorder (CG113,CG123) |
CBT | |
| Social Anxiety Disorder (CG159) |
CBT | |
| PTSD (CG26,CG123) |
CBT, EMDR | |
| Obsessive-Compulsive Disorder (CG31, CG123) |
CBT | |
| Body Dysmorphic Disorder (CG31) |
CBT | |
|
Step 2: Low intensity service (Less intensive clinician input than the high intensity service. Patients are typically encouraged to work through some form of self-help programme with frequent, brief guidance and encouragement from a Psychological Well-being Practitioner (PWP) who acts as a coach). |
Depression (CG90,CG91,CG123) |
Individual Guided Self-Help based on CBT, Computerized CBT, Behavioural Activation, Structured Group Physical Activity Program |
| Panic disorder (CG113, CG123) |
Guided Self-Help based on CBT, Psychoeducational Groups, Computerized CBT | |
| Generalized Anxiety Disorder (CG113, CG123) |
Guided Self-Help based on CBT, Psycho-educational Groups, Computerized CBT | |
| PTSD (CG26,CG123) |
No recommendation5 | |
| Social Anxiety Disorder (CG159) |
No first line recommendation6 | |
| Obsessive-Compulsive Disorder (CG31, CG123) |
Guided Self-Help based on CBT | |
|
Step 1: Primary Care (outside of IAPT service) |
Recognition of problem Moderate to Severe Depression with a chronic physical health problem |
Assessment/Referral/Active Monitoring Collaborative care (consider if depression has not responded to initial course of high intensity intervention and/or medication) |
Notes
CBT = cognitive behaviour therapy. IPT = interpersonal therapy. EMDR = eye movement desensitization reprocessing therapy (considered by many to be a form of CBT). Behavioural Activation is a variant of CBT. Active Monitoring includes careful monitoring of symptoms, psychoeducation about the disorder and sleep hygiene advice.
The procedures used in CBT vary with clinical condition. NICE recommends disorder specific forms of CBT, not a generic CBT intervention.
NICE’s (2009a,b) guidance on the treatment of depression come in two parts: recommendations for the treatment of “depression” and recommendations for the treatment of “depression in people with a chronic physical health problem”. The two guidelines are very similar. However, it should be noted that the “depression with a physical health problem” guideline does not recommend IPT, behavioural activation, counselling or brief psychodynamic therapy as high intensity interventions.
Although the NICE Guidance for Depression (NICE 2009a) recommends Behavioural Activation for the treatment of mild to moderate depression, it notes that the evidence base is not as strong as for CBT or IPT. A revision of the guideline is underway that will take into account more recent published studies.
If the relationship is considered to be contributing to the maintenance of the depression, and both parties wish to work together in therapy. IAPT recognises two forms of couples therapy and supports training courses in each. One closely follows the behavioural couples therapy model. The other is a broader approach with a systemic focus.
CBT during treatment in the acute episode and/or the addition of mindfulness-based cognitive therapy when the episode is largely resolved. Mindfulness is not recommended as a primary treatment for an acute depressive episode
NICE does not recommend any low intensity interventions for PTSD and recommends that you do NOT offer psychological debriefing.
NICE recommends individual CBT based on the Clark &Wells or Heimberg models. Low intensity intervention (guided self-help) is not routinely recommended but can be offered to individuals who are initially unwilling to accept face-to-face CBT. There is a third line recommendation for psychodynamic treatment specifically developed for social anxiety disorder if individual CBT and guided self-help have been declined.
Each year NHS Digital issues an Annual Report on the IAPT program which shows the activity levels and outcomes for services in every local health area (otherwise known as a clinical commissioning group - CCG). The report (NHS Digital 2015) that covers the 2014/15 financial year (April 2014 to March 2015) includes statistics on the proportion of patients who had each of the different types of therapy somewhere in their overall treatment plan and also makes it possible to see how many services offer a range of NICE recommended high intensity therapies for depression. The majority of courses of treatment were CBT related as 48% of all treatments were low intensity interventions based on CBT principles and 20% were high intensity CBT. Counselling accounted for a further 10% of treatments. IPT accounted for only 1% of treatments and 0.5% were couples therapy or brief psychodynamic therapy. A further 4% were identified as other high intensity therapies (including mindfulness) and 17% were unidentified with respect to treatment intensity or type. As IAPT develops it will aim to expand capacity for the four NICE recommended depression therapies that are in short supply (IPT, Couples Therapy, Brief psychodynamic therapy, Mindfulness based cognitive therapy) as it is considered important to provide patients with a choice of treatments when NICE recommends several alternatives for the same clinical condition. Inspection of CCG level data (NHS Digital 2015) indicates that almost all areas offer an element of choice, with 96% of CCGs having at least some capacity in 2 NICE recommended high intensity therapies for depression, 75% having capacity in at least 3 such therapies, and 48% offering at least 4 high intensity therapies. The most common offer was CBT and counselling, with both being available in 85% of CCGs.
3.3. Historical Background
NICE provided the first step in the story of the development of IAPT by issuing clinical guidelines that strongly recommended psychological therapies. However, NICE does not have an implementation budget. IAPT therefore needed advocates. Economists and clinical researchers combined resources to argue that increasing access to psychological therapies would largely pay for itself by reducing other depression and anxiety-related public costs (welfare benefits and medical costs) and increasing revenues (taxes from return to work, increased productivity etc.). This argument was first outlined in a paper (Layard 2005) for Tony Blair’s Policy Unit entitled “Mental Health: Britain’s Biggest Social Problem”. The policy unit responded by organizing a Downing Street Seminar in which Richard Layard (a distinguished economist from the London School of Economics and a Member of the House of Lords) and myself laid out the arguments. Many of those present expressed surprise that psychological therapy had now become so scientifically validated. The impact was considerable. A few months later the Labour Party’s general election manifesto included a commitment to “improve our services for people with mental health problems at primary and secondary levels, including behavioural as well as drug therapies” (Labour Party, 2005, page 65).
The arguments that were initially presented in private at the policy unit seminar were subsequently elaborated and published in academic articles (e.g. Layard et al. 2007) and more populist pamphlets such as the Depression Report (Layard et al. 2006) and We need to Talk (Mental Health Foundation et al., 2006), a report that was sponsored by numerous mental health and other charities. The pamphlets were widely distributed to the public and to policy makers. For example, the Depression Report was included in every copy of a national newspaper (the Observer) on Sunday 18th June 2006.
The arguments for IAPT are outlined in full in Layard & Clark (2014a, b). They can be briefly summarized as follows. Depression and anxiety problems are extremely common affecting around 15% of the adult population at any one time. As well as causing much personal distress, such mental health problems are the most important cause of disability in the working age population. This means that failure to tackle depression and anxiety disorders has a strong negative effect on a nation’s income, making it more difficult for society to pay for treatment of many of the physical illnesses (such as cardiovascular disease and cancer) that have a greater impact later in working life and in retirement. Furthermore, expanding access to psychological therapies would have no net cost. This is because the estimated cost of a course of NICE recommended treatment within a stepped care model would be around £6501, while the savings to the health service would exceed that amount, as would the savings to the Treasury (in increased tax revenues and reduced benefit payments for people returning to work).
3.4. Doncaster and Newham Pilots
One of the first decisions of the group of experts convened by the Department of Health was to develop some pilot projects that would examine whether routine clinical services could achieve clinical outcomes in line with those suggested by the research literature. In 2006 the NHS in England comprised 154 local health areas (termed primary care trusts at the time). Two of those local areas (Doncaster and Newham) were chosen as pilot sites (termed “Demonstration sites” by the Department of Health). Full details of the clinical services that were developed in the two demonstrations sites and the outcomes they obtained in their first year can be found in Clark et al. (2009) and Richards & Suckling (2009).
Briefly, each demonstration site received substantial funds to recruit and deploy an expanded workforce of CBT focused psychological therapists. Doncaster had been pioneering the use of low intensity therapies (especially guided self-help) and chose to particularly expand the work force that delivered these treatments, although some additional capacity to deliver high intensity interventions (face-to-face CBT) was also developed. Many of the guided self-help sessions were delivered over the telephone. As low intensity interventions and stepped care are not recommended by NICE for PTSD, the Doncaster site excluded this anxiety disorder but encouraged referrals for other anxiety disorders, as well as depression. Newham initially placed greater emphasis on high intensity CBT, although it also operated a stepped care model when appropriate, using a newly recruited workforce of low intensity therapists (subsequently called Psychological Well-being Practitioners or PWPs). The low intensity therapies included computerized CBT (cCBT), guided self-help and psychoeducation groups.
To determine whether the demonstration sites were able to achieve the outcomes one might expect from the randomized controlled trials that underpin NICE’s recommendations, both demonstration sites agreed to adopt a session by session outcome monitoring system that had already demonstrated its worth in achieving high levels of pre-post treatment data completeness in community samples (Gillespie et al. 2002). At every clinical contact patients were asked to complete simple measures of depression (PHQ-9: Kroenke et al. 2001) and anxious affect (GAD-7: Spitzer et al. 2006).
Since the creation of the National Health Service (NHS) in 1948, most patients who received specialist psychological therapy had to be referred by their general practitioner (GP), partly to help constrain NHS costs. However, there was some concern that requiring patients to be referred by a GP might be an impediment to access for some members of the community. For this reason, the demonstration sites were allowed to also accept self-referrals as an experiment to see whether this facilitated access for people would not otherwise be seen.
The main findings from the first year of operation of the two demonstration sites (Clark, et al. 2009) were as follows:
3.4.1. Clinical Problems
The two sites saw somewhat different populations. Although Doncaster did not use formal diagnoses, GP referral letters mentioned depression as the main problem in 95% of cases. In the remaining 5% anxiety was mentioned as the main problem, mainly GAD (3.9%). Newham established ICD-10 diagnoses. Main problems were: depression (46% of patients), anxiety disorders (43%) and other problems (11%).
3.4.2. Numbers seen
Taken together, the two sites saw an impressively large number of people (over 3,500) in the first year, with the use of low intensities therapies and stepped care being the key ingredients for managing large numbers. For this reason, as the year progressed the Newham site increased the size of its PWP workforce.
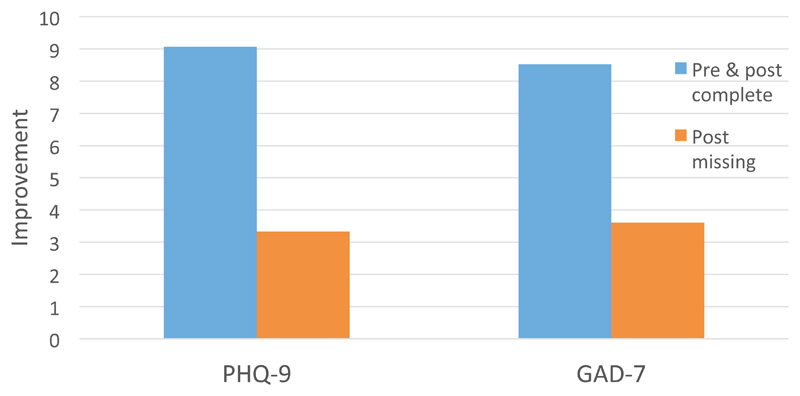
3.4.3. Data completeness
The session by session outcome monitoring system ensured that almost all (over 99% on Doncaster and 88% on Newham) patients who received at least two sessions had pre and post treatment PHQ-9 and GAD-7 scores. For patients who discontinued therapy earlier than expected, the scores from the last available session were used as post-treatment scores. As well as the new session-by-session outcome monitoring scheme, the sites also obtained outcome data on the CORE-OM (Barkham et al. 2001) using a more conventional pre and post-treatment only data collection protocol. As is usual in community samples, this protocol produced a much lower data completeness rate (6% in Doncaster, 54% in Newham), mainly due to missing post-treatment scores. Figure 3 shows the mean improvements in depression (assessed by the PHQ-9) and anxiety (assessed by the GAD-7) in patients treated in Newham who did, and did not, provide post-treatment data on the conventional (CORE-OM based) outcome monitoring protocol. Patients who failed to provide post data on conventional system showed less than half of the improvement of those who provided post-treatment data. This finding led the IAPT national team to conclude that services that have substantial missing data rates are likely to overestimate their effectiveness. For this reason, session-by-session outcome monitoring was adopted in the subsequent national roll-out of IAPT (see below).
Figure 3.
Improvement in PHQ-9 and GAD-7 scores between initial assessment (pre) and last available session (post) in people who either completed both the pre and post-treatment CORE-OM or who failed to complete the CORE-OM at post. Data from the Newham Demonstration site. Figure derived from Clark et al. (2009)
3.4.4. Self-referral versus GP referral
Newham, which has a mixed ethnic community, made extensive use of self-referral. Comparisons of self-referred and GP referred patients indicated that the self-referrers had similarly high PHQ-9 & GAD-7 scores as the GPs referrals but tended (non-significantly) to have had their problem longer. Importantly, self-referrals more accurately tracked the ethic mix of the community (minorities were under-represented among GP referrals) and had higher rates of PTSD and social phobia, both conditions that traditionally tend to be under-recognized. These findings led the government to include self-referral in the subsequent national roll-out
3.4.5. Outcomes
The high level of data completeness on the PHQ-9 and GAD-7 made it possible to accurately assess any clinical improvements that patients achieved while being treated in the demonstration sites. All patients who received at least two sessions (including assessment) were included in the analysis, irrespective of whether they were coded as completers or drop-outs by their therapist. As a group, patients treated in both sites showed large improvements (pre-post treatment uncontrolled effect sizes of 0.98 – 1.26). Individuals were considered clinically recovered if they scored above the clinical cut-off on the PHQ and/or the GAD at pre-treatment and below the clinical cut-off on both at post-treatment. Using this criterion, 55% (Newham) and 56% (Doncaster) of patients recovered. Self-referrers and patients from ethnic minorities were no less likely to recover than (respectively) GP referrals and Caucasians.
The economic argument for IAPT (Layard et al. 2007) was partly based on the assumption that clinical improvement would be sustained and that treatment would improve peoples’ employment status as well as symptoms. To assess whether clinical improvements were sustained, patients in both sites were asked to re-complete the outcome measures 9 months (on average) after discharge. Unfortunately, data completeness at follow-up (36% in Newham and 51% in Doncaster) was much lower than at post-treatment (88% and 99% respectively). However, among those people who did provide data, the gains that were achieved in therapy were largely maintained. To assess employment changes, pre-treatment and post-treatment employment status was compared. It had been assumed that IAPT services would achieve an overall improvement in employment status in 4% of the total treated cohort (Layard et al 2007). The observed rate was 5%.
Although the outcomes observed in the demonstration sites were broadly in line with expectation, it is important to realise that the sites were not set up as randomized controlled trials and it is likely that some of the observed improvement would have happened anyway (e.g. natural recovery). Various studies suggest that natural recovery rates over a period of time that is similar to the duration of IAPT treatment are high among recent onset (< 6 months) cases of depression and anxiety disorders but are substantially lower among more chronic cases. Building on this observation, Clark et al. (2009) separately computed the recovery rates among recent onset and chronic cases. Most cases (83% in Newham, 66% in Doncaster) had been depressed or anxious for over 6 months and it seemed safe to conclude that treatment had provided added benefit to this group as the recovery rates (52% at each site) comfortably exceeded the 5-20% one might expect from natural recovery or minimal intervention. However, among the minority of cases with a recent onset, it was not possible to exclude the possibility that much of the improvement may have been due to natural recovery (see Clark et al. 2009, pp 919).
3.5. National Implementation Plan
The success of the Doncaster and Newham pilot projects and continuing public discussion of the combined clinical and economic arguments for IAPT led to the development of a plan for a national roll out of the program. The broad outline of the plan was announced on World Mental Health Day 2007 (10th October) by Alan Johnson, who was the Labour Government’s Secretary of State for Health at the time. Alan Johnson announced that:
“We will build a ground breaking psychological therapy service in England. Backed by new investment rising to £170 million by 2010-11, the service will be capable of treating 900,000 additional patients suffering from depression and anxiety over the next three years. Around half are likely to be completely cured, with many fewer people with mental health problems having to depend on sick pay and benefits”
Over the next 12 months a panel of experts worked on further details of the plan and the first IAPT services opened their doors to patients in September 2008. Implementation was phased. In the first year some 35 services opened, covering about a quarter of the country, and about 1,000 trainees began their training. The areas that launched the initial services were selected in open competition based on their ability to provide the trainees with patients who had the conditions they had been trained to treat – plus a core of experienced staff who could treat more complex cases and act as supervisors for the trainees. The areas also needed to commit to systematically collecting outcome data and entering it into one of two bespoke IT systems. There were two further annual waves of selection and the whole country had an IAPT service after three years.
In 2010 there was a change of government. The new government (a Conservative and Liberal Democrat Coalition) committed to further expanding the capacity of IAPT services in a key document entitled “No Health without Mental Health” (DH, 2011). In 2015 the government changed again (to a Conservative administration) and the new government again committed to expanding the IAPT program by supporting the proposals in a key document entitled “Five Year Forward View for Mental Health” (NHS England 2016).
The 2008 National Implementation Plan laid out the key features of an IAPT service, which are briefly summarized below. Some of the more critical features are then outlined in further detail.
3.6. Key features of IAPT service model
Patients should receive a professional, person-centered assessment that identifies the key problems that require treatment (problem descriptors), clarifies patients’ goals, assesses risk, and agrees a course of treatment.
NICE-recommended psychological therapies (see Table 1) are provided.
The therapists who are employed in the service should be fully trained in how to deliver the relevant treatment(s) or be clinical trainees who are attending an IAPT recognized training course.
Patient outcomes should be measured on a session-by-session basis, with at least 90% completeness of data.
Treatment should follow a stepped care model, when appropriate (see Table 1).
Patients should be offered a choice of therapies when NICE indicates that several therapies are effective for a particular condition. Whenever possible patients should also be offered choice in terms of when and where they are seen.
The Service operates a “hub and spoke” model. There is a central office where the clinical director and administrator work and where there are rooms for supervision, training, keeping patients’ records, and the telephone support for guided self-help. But most of the face-to-face therapy is given much nearer to where the patients live, often in family doctor practices or other community locations.
The service accepts self-referral as well as referrals from family doctors and other health professionals.
All therapists should receive weekly, outcome informed supervision which ensures that all cases are discussed at regular intervals and decisions about whether to step-up to high intensity therapy are made in a timely fashion if a patent is not responding to low intensity treatment.
3.7. Therapist training
Therapist training is at the heart of the IAPT model. A lack of suitably trained therapists was considered the main obstacle to the implementation of NICE guidelines so the IAPT program has paid considerable attention to how to train therapists in order to equip them to competently deliver the relevant treatments.
In order to guide the training of the new workforce, the Department of Health commissioned and distributed separate national curricula for the training of high intensity CBT therapists and Psychological Well-Being Practitioners (PWPs). The high intensity CBT curriculum is closely aligned to the particular CBT programmes that had been shown to be effective in the RCTs that contributed to NICE’s recommendations. A wide range of general CBT assessment and intervention strategies are included in the curriculum. In addition, trainees are required to be taught at least two evidence based treatments for depression (cognitive behaviour therapy and behavioural activation) and at least one specific, evidence based treatment for each anxiety disorder. In panic disorder examples include Barlow & colleagues’ CBT programme and Clark & colleagues’ cognitive therapy program. In PTSD, examples include Foa’s imaginal reliving, Ehlers & Clark’s cognitive therapy or Resick’s Cognitive Processing Therapy. Roth and Pilling (2008) developed a competency framework that specified the clinical skills that are required to deliver empirically supported CBT treatments for depression and anxiety disorders. The high intensity curriculum aims to ensure that these skills are taught on IAPT training courses. In addition to specifying the skills that trainees should acquire, the curriculum also specifies how these skills should be assessed (through a mixture of ratings of actual therapy sessions using the revised version of the Cognitive Therapy Rating Scale (CTS-R: Blackburn et al. 2001) and written assignments in the form of case reports and essays). Trainees only graduate from a course if they have been able to demonstrate the skills in practice.
A separate curriculum was issued for training the psychological well-being practitioners (PWPs) who deliver the low intensity therapies. The four sections of the curriculum cover: 1) engagement and assessment, 2) evidence based low intensity treatments, 3) values, policy, culture and diversity, 4) working within an employment, social and healthcare context. As low intensity working was relatively new, there were few published therapist manuals. To redress this shortfall, a substantial set of teaching aids developed by David Richards (one of the pioneers of low intensity work) and his colleagues were produced to supplement the curriculum. As with the high intensity curriculum, assessment procedures are also specified, with particular emphasis being placed on structured role-plays covering a wide range of different skills.
Both the high intensity CBT and the PWP training programmes are conceived as joint university and in-service trainings. Over a period of approximately one-year high intensity trainees attend a university based course for lectures, workshops and case supervision two days a week, while PWPs attend university for one day per week. For the rest of their time, both sets of trainees work in an IAPT service where they receive further regular supervision. The services are also encouraged to provide the trainees with the opportunity of directly observing therapy sessions conducted by experienced staff that work in the service. Successful applicants to the high intensity CBT courses are required to already worked for several years in mental health services and generally belong to a core mental health profession (clinical psychologist, social worker, mental health nurse). Recruits to the PWP training courses generally do not have a core mental health profession and many are recent graduates from university psychology courses who have some subsequent experience working in mental health in a junior capacity.
The initial emphasis of IAPT training was on CBT. However, as the programme has developed bespoke curricula for training clinicians in other NICE recommended therapies for depression (interpersonal therapy, couples therapy, counselling, brief psychodynamic therapy) and the prevention of relapse in recurrent depression (mindfulness based cognitive therapy) have been created. Readers who are interested in viewing these curricula will find them on the Health Education England (HEE) website (https://hee.nhs.uk). Roth and Pilling have also extended their competency framework to cover these therapies. The extended framework can be accessed online at the University College London (UCL) Competence Framework website ( http://www.ucl.ac.uk/pals/research/cehp/research-groups/core/competence-frameworks ).
3.8. Outcome measurement
Prior to IAPT the NHS was not good at recording the outcomes of mental health treatment. A survey of psychological therapy services (Clark et al. 2008, Stiles et al. 2007,) found that only 38% of patients had an assessment of their symptoms at the beginning and end of treatment. Generally, therapists only aimed to give patients a symptom questionnaire to complete at the beginning and end of treatment. As patients do not always finish therapy when expected and therapists were not in the habit of regularly giving outcome measures, this meant that post-treatment outcomes were often not available. The Doncaster and Newham pilot projects (see Figure 3) showed that this can lead services to over-estimate their effectiveness. This is because patients who fail to complete post-treatment measures tend to have done less well. To get round this problem, IAPT adopted a session-by-session outcome monitoring system that was successfully piloted in a community psychological therapy service developed that for the many people who were victims of a large car bomb (Gillespie et al. 2002). The monitoring system was further tested and refined in the Doncaster and Newham IAPT pilots (Clark et al 2009, Richards & Suckling 2009). Patients are asked to complete brief measures of depression, anxiety and mental health related disability every session. In this way, post-treatment outcome data is available even if a patient finishes therapy earlier than expected. Therapists are encouraged to review the measures at the start of each treatment session and to use them in treatment planning. Services have specialized IT systems that display the measures in graphical form and also make them available to supervisors and service managers. Adoption of the session-by-session outcome monitoring system has enabled IAPT services to obtain outcome data on 98.5% of all patients who have a course of treatment (NHS Digital 2016).
It is good practice to ask patients to complete outcome measures before the start of a clinical session. This ensures that valuable clinical time is not wasted with completing measures. Questionnaires are often completed while a person is waiting for their appointment or earlier on the day of the appointment. On some occasions, the IAPT worker may want the person to complete measures within sessions, to introduce them to the measures and engage them in the process of objective measurement of symptoms. At the start of the IAPT program, patients whose therapy sessions were delivered over the telephone were often asked to verbally report their symptoms in the session, with their PWP entering their answers into the IT system. The increasing availability of online portals for completing questionnaires means that many patients are now able to enter their data via the internet before a telephone call with their therapist. This practice is strongly recommended.
Table 2 shows the outcome measures that are used on a session by session basis. The PHQ-9 (Kroenke et al. 2001) is used to measure symptoms of depression. The GAD-7 (Spitzer et al. 2006) is the default measure of anxiety. GAD-7 was originally developed as a measure of the severity of generalized anxiety disorder but it also gives elevated scores in other anxiety disorders and is sensitive to improvement in those disorders. However, it mainly focuses on anxious affect and worry. It does not have items that assess some of the key features of other anxiety disorders (such as fear and avoidance of social or agoraphobic situations; obsessions or compulsions; or intrusive memories). For this reason, clinicians are also encouraged to use more specific measures for other anxiety disorders (DH 2011).
Table 2.
IAPT’s Main Outcome measures
| Main Mental Health Problem (primary problem descriptor) | Depression Measure | Recommended Anxiety Measure | Back-up to “Recommended Anxiety Measure” for calculating recovery if recommended measure is missing | Measure of Disability |
|---|---|---|---|---|
| Depression | PHQ-9 | GAD-7 | WSAS | |
| Generalized anxiety disorder | PHQ-9 | GAD-7 | WSAS | |
| Mixed anxiety/depression | PHQ-9 | GAD-7 | WSAS | |
| No problem descriptor | PHQ-9 | GAD-7 | WSAS | |
| Social anxiety disorder | PHQ-9 | SPIN | GAD-7 | WSAS |
| PTSD | PHQ-9 | IES-R | GAD-7 | WSAS |
| Agoraphobia | PHQ-9 | MI | GAD-7 | WSAS |
| OCD | PHQ-9 | OCI | GAD-7 | WSAS |
| Panic disorder | PHQ-9 | PDSS | GAD-7 | WSAS |
| Health anxiety (hypochondriasis) | PHQ-9 | HAI | GAD-7 | WSAS |
Note: Recovery, reliable improvement and reliable deterioration rate calculations are based the pair of measures highlighted in bold. When the measure in bold in the third column is missing, the recovery calculation is based on the combination of PHQ-9 and GAD-7, if this is different. PHQ-9 = patient health questionnaire depression scale (Kroenke et al. 2001). GAD-7 = the generalised anxiety disorder scale (Spitzer et al. 2006). SPIN = social phobia inventory (Connor et al. 2000). IES-R = impact of events scale revised (Creamer et al2003). MI = mobility inventory (Chambless et al. 1985). OCI = obsessive-compulsive inventory (Foa et al. 1998). PDSS = panic disorder severity scale (Shear et al. 2001). HAI = health anxiety inventory (Salkovskis et al. 2002). WSAS = work and social adjustment scale (Mundt et al. 2002).
In addition to the session by session measures in Table 2, patients are also asked on an occasional basis to complete questionnaires that assess the extent to which they are satisfied with their IAPT assessment and treatment.
3.9. Outcome metrics
A large number of metrics can be derived from the IAPT dataset. The three that IAPT services are required to report are the percentages of patients who have recovered, have reliably improved, and have reliably deteriorated. In most research studies computation of these metrics would be based on change in the symptom questionnaire most closely related to the disorder being treated. So, the depression measure in a trial of depression treatments and the anxiety measure in a trial of anxiety treatments. However, this is assessing recovery from a syndrome but the IAPT service is treating a person. It was therefore decided that a stricter criterion was required in which scores on both depression and anxiety measures would be considered irrespective of the clinical problem (depression, PTSD, OCD, GAD, etc.) that is being treated.
Patients are considered recovered if their scores on depression and/or anxiety are above the clinical cut-off on either measure at the start of treatment and their scores on both are below the clinical cut-off at the end of treatment. IAPT operates a policy of only claiming demonstrated recovery. This means that the small (less than 2%) number of patients who have missing post-treatment data are coded as not recovered. Patients are considered reliably improved if their scores on depression and/or anxiety have reduced by a reliable amount and neither measure has shown a reliable increase. Conversely, patients are reliably deteriorated if their scores on depression and/or anxiety have increased by a reliable amount and neither measure has shown a reliable decrease. In recent reports (NHS Digital 2016) these metrics are supplemented by reporting pre-treatment and post-treatment means and standard deviations plus pre-post treatment effect sizes on each symptom measure.
3.10. Public transparency about clinical outcomes
Once a month patient data from each IAPT service flows in pseudo-anonymized data form to NHS Digital (www.digital.nhs.uk ), which is a government agency that manages national statistics. NHS Digital issues regular reports on the numbers of people accessing IAPT services and their outcome, along with a range of process variables (average number of sessions, types of therapy, etc.). The richest dataset appears in the annual reports. Most data provided by NHS Digital is also available in Public Health England’s Common Mental Health Disorders Profiling Tool (https://fingertips.phe.org.uk/profile-group/mental-health/profile/common-mental-disorders), along with other contextual information about CCGs (for example, social deprivation score). By accessing the websites, patients can see what their local service offers and the outcomes it achieves. Commissioners of services and clinicians working within the services can benchmark their service against others, celebrate successes, and consider developing collaborative networks in which local services come together to discuss common problems and learn from each other’s solutions. As we will see later, this unprecedented level of public transparency is helping services understand and reduce regional variation in clinical outcomes.
3.11. What has IAPT Achieved (Summer 2017)?
IAPT is a work in progress. However, at the time of writing services have been established in all 209 of the local health regions (CCGs) in England. Over 7,000 new therapists have been trained (NHS England 2015), with approximately 60% being high intensity therapists and 40% being PWPs. The services also have a small number of employment advisors who liaise with therapists to help unemployed patients return to work as their clinical condition improves.
NHS Digital reports (available at www.digital.nhs.uk ) show that IAPT services see over 960,000 people a year, which represents around 16% of the community prevalence of depression and anxiety disorders (McManus et al. 2016). Gender representation among people treated in the services (65% female) closely matches the relative prevalence of common mental health problems in the community (62% female. See McManus et al. 2016). Some people are only seen once to be assessed, given advice and, if necessary, signposted to other services2. However, over 560,000 people (approximately 60%) go on to have a course of treatment involving two or more therapy sessions. The average waiting time between assessment and the start of treatment is 29 days and the mean number of therapy sessions is 6.4 (NHS Digital 2016, Tables 2a and 3a respectively). Thirty-six percent of people only receive low intensity interventions, 28% only receive high intensity interventions, and 34% receive both (NHS Digital 2016, Table 4g). This means that during the course of their treatment in IAPT’s stepped care services 70% of patients receive at least one low intensity intervention and 62% receive at least one high intensity intervention.
Everyone who has two or more treatment sessions before discharge is included in the cohort of individuals who are assessed for clinical outcomes. 98.5% of these individuals have pre-treatment and post-treatment scores on both the depression and anxiety measures3. The overall recovery rate for the cohort (based on data from January to March 2017) is 51% and 66.3% people show reliable improvement. The reliable deterioration rate is approximately 6% (NHS Digital 2016, Table 4g), which is less than one might expect for individuals on a wait list. Pre-post treatment effect sizes are large (NHS Digital 2016, Table 6c). For depression cases the pre-post effect size on the PHQ-9 is 1.4. For anxiety and stress related cases the pre-post effect size on the GAD-7 is 1.5.
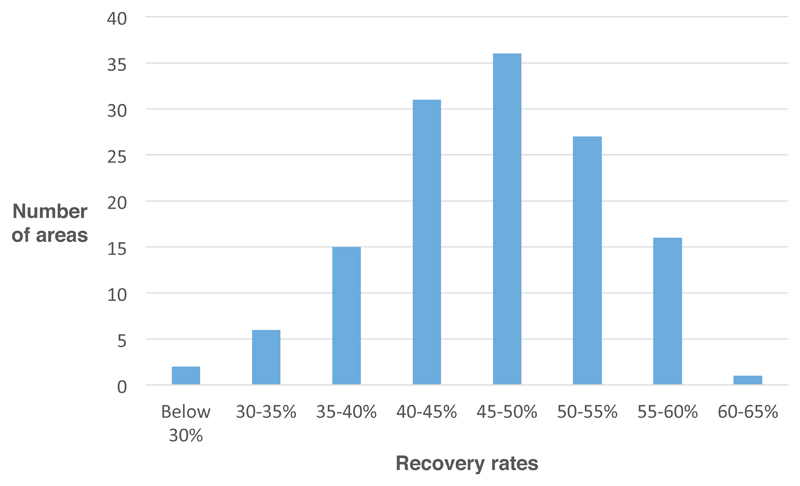
3.12. Variability in Outcomes
The overall outcomes achieved by IAPT services are encouraging. It does seem possible to disseminate empirically supported treatments at scale while maintaining average clinical outcomes that are broadly in line expectation from randomized controlled. However, inspection of CCG-level data (NHS Digital 2016) indicates that IAPT services show considerable variation in the outcomes that they achieve. Figure 4 shows the spread of recovery rates across IAPT services during the year from April 2015 to March 2016. The lowest recorded recovery rate for the year was 21% and the highest was 63%. For reliable improvement the lowest rate was 35% and the highest was 80%. For reliable deterioration the lowest rate was 3% while the highest was 10%.
Figure 4.
IAPT Recovery rates during 2015/16 vary greatly between areas (CCGs).
Clearly, it is important that we understand the determinants of such variability. If some of the determinants are features of a service that are changeable, it should be possible to use the information to help lower performing services to move to towards the level of the highest performers. In the next two sections we look at what is currently known about the predictors of outcome variability. Thankfully, many are variables that are potentially changeable and there is evidence that lower performing services are moving steadily upwards in their recovery rates. For example, 53 IAPT services had recovery rates below 45% in March 2016 but by March 2017 the number had dropped to 24. This period coincided with some intensive work that the NHS England Improvement Team conducted with low performing services and with a series of Regional “Enhancing Recovery” workshops that aimed to disseminate knowledge about the determinants of outcome variability.
3.13. Importance of NICE Compliance
IAPT services are expected to provide patients with NICE recommended treatment and that is generally what they do. However, a minority of patients receive treatments that are not in line with NICE guidance. This creates a natural experiment. Does it matter if your therapist deviates from NICE guidance? Gyani et al. (2013) used a patient-level data download from the 32 services that were established in the first year of the IAPT program to answer this question. Among high intensity therapies the main contrast that was available at the time was that between CBT and counselling. NICE recommends both for the treatment of depression (see Table 1). Consistent with this recommendation, there was no difference in the recovery rates associated with CBT and counselling among patients with a diagnosis of depression4. In contrast to the recommendations for depression, NICE does not recommend counselling for the treatment of generalized anxiety disorder (GAD). Consistent with this position, CBT was associated with a higher recovery rate than counselling among patients with a diagnosis of GAD. A further natural experiment emerged in the data on low intensity interventions. For the treatment of depression, NICE recommends guided self-help but not pure (non-guided) self-help. However, a significant minority of patients received pure self-help. Consistent with NICE guidance, guided self-help was associated with a higher recovery rate than pure self-help among patients with a diagnosis of depression.
Gyani et al’s (2013) findings replicate in a more recent IAPT dataset (NHS Digital 2016, Table 7d). For generalized anxiety disorder, CBT (57%) and Guided Self-Help (61%) had significantly higher recovery rates than counselling (50%) during 2015/16. For depression, guided self-help (49%) was associated with a significantly higher recovery rate than pure (non-guided) self-help (37%).
Taken together these findings would appear to support the value of aligning clinical interventions with NICE guidance.
4. Understanding Variability in Service Outcomes
4.1. Analyses of national data
One of the great strengths of the IAPT program is that it collects outcome data on almost everyone who has a course of treatment. Analyses of this data can give us clues to the determinants of outcome variability. The most obvious thing to consider is whether services differ in the extent to which they see more or less severe cases. Surprisingly it seems that services are very similar, at least in terms of the average severity of symptoms that patients report at the start of treatment (NHS Digital 2016, Table 6c). The PHQ -9 is a scale that ranges from 0 to 27. The average PHQ score for depressed patients treated in the IAPT services is 17.30 with a very small standard deviation (0.74). The GAD-7 is a scale that ranges from 0 to 21. The average GAD score for patients with anxiety disorders treated in the IAPT services is 14.8 and the standard deviation is once again extremely small (0.50).
If average symptom severity is not a predictor of between service outcome variability, what is? Gyani et al. (2011) identified two factors that discriminated between services with high and low recovery rates during the first year of the IAPT program. Firstly, there was evidence for a dose response effect. Services that gave a higher average number of treatment sessions obtained better outcomes. Secondly, higher step-up rates from low intensity to high intensity therapy among those who had failed to respond adequately to the former were associated with higher overall recovery rates. This seems to suggest that it is important that services provide patients with the opportunity to progress throughout the stepped care system, if necessary.
Clark et al. (2017) recently used CCG-level data downloaded from public websites (NHS Digital and the Common Mental Health Disorders Profiles Tool) to identify organizational features of a service that predict outcome variability. A regression model that included five organizational variables was built using data for the 2014/15 financial year. The researchers then waited until the 2015/16 data was released and tested whether the model also predicted within service change in outcomes between the two years. They argued that consistency of results between these two types of analysis would strengthen the argument that the organizational features have a causal role as any potentially spurious third variables were unlikely to be the same in the two analyses. The five organizational variables, which are described below, were generally consistent across the analyses.
4.1.1. Waiting times
Services that have a shorter waiting time between initial assessment and the start of treatment achieve better outcomes. This may be because patients lose enthusiasm for engaging in therapy if they have to wait too long after making the decision to come forward for treatment. Inspection of the regression lines suggests waits should ideally not be longer than 4-6 weeks.
4.1.2. Problem descriptor completeness
The NICE recommended approach to treatment varies with clinical condition as specified by ICD-10 codes (WHO 1992). For some clinical conditions (such as depression) several schools of therapy are recommended. For others (such as the anxiety disorders) only one school (CBT) is recommended but the procedures used can be radically different depending on the particular condition. For example, video feedback is strongly recommended as part of CBT for social anxiety disorder but plays no role in the treatment of PTSD which places a much stronger emphasis on memory work. For this reason, assessors in IAPT services are encouraged to work with patients to accurately describe the problems that they would like their treatment to focus on and to give these the appropriate ICD-10 code(s). In some services problem descriptors are identified for almost all patients, but in others the problem descriptor rate is low, perhaps because staff are less convinced about the value of the psychiatric classification. Whatever the reason, services with higher rates of problem descriptor identification achieve better outcomes.
4.1.3. Dose of therapy
The dose of therapy effect identified in Gyani et al’s (2013) analysis of the first year of the IAPT program replicated when re-examined seven years later. Services that gave a higher average number of treatment sessions achieved better outcomes. The optimal mean number of session appears to be 9-10, but many patients recover with less sessions and some need substantially more.
4.1.4. Missed appointments
Services vary considerably in the percentage of clinical appointments that patients miss without notifying the service in advance. Services with higher rates of missed appointments have poorer overall outcomes.
4.1.5. Is the service predominantly focused on providing therapy?
IAPT services vary in the proportion of referrals that receive a course of therapy, as opposed to just an assessment session, advice and signposting. Services in which a particularly high proportion of people go on to have a course of therapy have better overall outcomes. The finding is reminiscent of the positive relationship in surgery between post-operative outcome and the volume of operations conducted by hospitals and individual surgeons (Hu et al. 2003).
In addition to these five organizational variables, the social deprivation effect previously identified by Dalgadillo et al. (2015) was replicated. Services in more socially deprived areas had poorer outcomes. However, the effect of social deprivation was reduced when it was entered into a multiple regression together with the organizational variables. This suggests that if someone lives in a socially deprived area, it is particularly important that they have a high quality IAPT service.
4.2. Importance of clinical leadership
In 2015 NHS England invited twelve of the highest performing IAPT services to an event which aimed to identify aspects of the services that might have helped them achieve their excellent outcomes. Soft data from this event suggested that the quality of clinical leadership in a service may have been critically important. In all of the services the clinical leaders had a strong focus on patients achieving recovery and reliable improvement. They helped create an innovation environment in which the staff were interested in the service’s outcome data primarily because it gave them clues about how to further improve their clinical work. The leaders supported staff in this enterprise by enabling them to attend multiple continued professional development events. Staff also received personal feedback on the outcomes that they achieved with their patients, benchmarked against the service’s average. For such benchmarking to be effective, it is essential that it occurs in a supportive environment. In general, the IAPT program has benefitted from having clear targets for recovery. However, targets are a two edged sword. Under poor leadership they can appear burdensome and oppressive. Under good leadership they can create an innovation climate.
4.3. Plan, Do, Study, Act methodology
Some IAPT services have used the Plan, Do, Study, Act methodology (Langley et al. 2009) to improve the outcomes they achieve. For a short period of time (say one month) the service reviews the notes and other available information on all patients who had not achieved full recovery by the end of treatment. Careful study of the information is used to generate hypotheses about changes to service provision that might have helped the patients to gain further benefit. These changes are then implemented (Act) and their effect observed. Pimm (2016) reported that this methodology enabled the large service that he leads move from an average recovery percentage in the mid 40s to one in the mid 60s. Several other services have recently implemented the same methodology with beneficial results.
5. Limitations and Criticisms of the IAPT Program
5.1. Limitations
IAPT is an ongoing project. There are several aspects of the services that need to be addressed as the initiative develops. First, the program needs to expand as it is still only meeting approximately 16% of the prevalence of depression and anxiety in the community (see below for expansion plans). Second, access to the services for older people needs to be improved. People over the age of 65 who have received treatment in the services achieve particularly good results with 60% recovering (NHS Digital 2016). However, this group of individuals is under-represented. Third, services are inconsistent in the use of outcome questionnaires that are specifically tailored to assess key aspects of the different anxiety disorders (see Table 2). Items on these questionnaires are particularly helpful for guiding treatment but a recent report (NHS Digital 2016, Table 6b) revealed that only about 1 in 5 patients with the relevant anxiety disorder are given the optimum symptom measure. Finally, IAPT services rarely follow up patients to see if they remain as well as patients do in the randomised controlled trials that generated the NICE guidelines. Clark et al. (2009) followed up patients who were treated in the Doncaster and Newham pilot nine months after the end of therapy and found that treatment gains were generally maintained. However, commissioners have been unwilling to fund systematic follow up in routine IAPT services. This is unfortunate as planned follow up is likely to increase clinician’s motivation to conduct relapse prevention interventions before the end of treatment and would also be a good way of identifying individuals who could benefit from a small number of booster sessions.
5.2. Criticisms
IAPT, like everything human, has its critics. Some of the complaints are justified, since what happens on the ground never corresponds exactly to what its originators intended. For example, there have been health commissioners who have limited the number of sessions of treatment a person can receive to an arbitrary low number (6 or less). This is inappropriate and leads to lower recovery rates, as we have seen above. Some criticisms are misleading. For example, some people say that IAPT only provides CBT, but in fact it provides a range of NICE-recommended therapies. In the most recent workforce census (NHS England 2015) 27% of the high intensity therapists employed in IAPT described themselves as either counsellors or therapists from non-CBT therapies. However, these therapists are unevenly distributed and it is undoubtedly the case that some services need to expand their capacity for such therapies in order to provide patients with a full range of choice. There has also been concern that investment in the IAPT program might be counterbalanced by disinvestment in other aspects of the mental health system. While local commissioners do reconfigure services from time to time, the evidence indicates that the IAPT program has more than doubled the NHS investment in psychological therapies (see Layard & Clark 2014a, b). Finally, some critics (Griffiths & Steen 2013) argue that IAPT exaggerates its recovery rates as a substantial number of people who are referred to the services do not go on to have a course of treatment and are therefore not included in the recovery computation. This argument is misplaced. The vast majority of referrals that do not go on to have a course of treatment are either individuals who are never seen in the service or people whose assessment indicates that their problems are not appropriate for treatment in IAPT (NHS Digital 2016, Table 4a).
6. Future Development of the Program
The UK Government’s recently published document on “Implementing the Five Year Forward View for Mental Health” (NHS England 2016b) includes a commitment to expand the IAPT program so that it caters for 1.5 million people (around a quarter of the community prevalence of depression and anxiety disorders) by 2021. In order to achieve this expansion up to 4,500 additional psychological therapists (NHS England 2016b, page 17) should be trained. Services will also be encouraged to make greater use of digitally assisted therapy in order to promote efficiency and increase convenience for patients.
Around two thirds of the expansion will focus on people with long term physical health problems (such as diabetes, chronic obstructive pulmonary disease, cardiovascular disease) in the context depression or anxiety disorders. Such individuals are currently under-represented in IAPT services. Research (see Layard & Clark 2014a, b for review) shows that: a) the costs of physical healthcare are increased by up to 50% in people with long term physical health conditions (LTCs) who are also depressed or anxious, and b) much of this excess cost can be recouped by providing appropriate mental health treatment. To ensure that the treatment progresses in the most helpful manner, new “IAPT-LTC” services will be created that deliver physical and mental health care in the same location with physicians and therapists closely coordinating their work. The new IAPT-LTC services will also provide treatment for people who are distressed by medically unexplained symptoms.
One of the most active areas of psychotherapy research in recent years has been internet based therapy. Numerous randomised controlled trials have shown that internet based CBT can be effective in depression and anxiety disorders, especially if patients are supported to work through the internet program by a clinician. Some internet assisted treatments achieve clinical outcomes that are broadly in line with face to face therapy (Andersson et al. 2014) but with a substantial saving in therapist time. As one of the main mechanisms of support is asynchronous messaging, the programs have the additional advantage that patients can work on their therapy at times that are most convenient for them (often evenings and weekends) while therapists can continue to operate in normal clinical hours. IAPT will look to increase the use of internet assisted treatment programs that have a strong evidence base and are able to save therapist time and/or improve patient convenience without impairing clinical outcomes.
7. Conclusion
The English IAPT program has greatly increased the availability of empirically supported psychological therapies for depression and anxiety disorders. A session by session monitoring system ensures that outcomes are recorded for almost everyone. Overall outcomes are broadly in line with expectation from clinical trials. Study of the determinants of regional variation in outcomes is starting to reveal information about the optimal way to organize services. Every country is different. However, it is hoped that some of the lessons that have been learned from IAPT will help other countries in their own quests to realise the mass public benefits that can be achieved by increasing the availability of psychological therapies.
Summary Points.
Effective psychological therapies have been developed for depression and all the anxiety disorders. NICE recommends these treatments as first line interventions.
However, in most countries very few patients receive empirically supported psychological therapies, mainly because there are insufficient appropriately trained therapists.
Layard and Clark argued that making evidence-based psychological therapies more widely available would save money as well as reduce suffering
The UK government funded two pilot projects (Doncaster and Newham) that successfully demonstrated that community psychological services can achieve clinical outcomes in line with those reported in clinical trials.
Starting in 2008 the Government developed a plan to Improve Access Psychological Therapies (IAPT) throughout England by training a large cohort of therapists in empirically supported treatments and deploying them in new community services for depression and anxiety disorders.
Training courses based in national curricula that specify key clinical interventions and the competences required to deliver them were developed. IAPT services use a novel session-by-session outcome monitoring system that obtains pre-treatment and post-treatment measures of anxiety and depression on 98% of all treated patients. Therapists receive regular supervision.
From small beginnings IAPT has grown to the point where it now treats over 560,000 people each year. Overall outcomes are generally in line with expectations from the research literature. Around 50% of patients recover and two-thirds show reliable improvement.
IAPT services vary in their clinical outcomes. Analyses of the predictors of such variability are being used to identify treatment delivery and service organization features that can enhance outcomes. This information is being used to further improve the performance of IAPT services.
Future Issues.
IAPT is a work in progress. Although it has greatly improved public access to empirically supported psychological therapies in England there is still some way to go. Currently around 960,000 are seen in IAPT services each year. This represents around 16% of the community prevalence of depression and anxiety disorders. The UK government is committed to expand the program so at least 1.5million people are seen each year by 2021.
The expansion will particularly focus on people with depression and anxiety in the context of long-term physical health conditions (such diabetes & cardiovascular disease) as these people are unrepresented in IAPT services and failure to treat their mental health problems makes their physical health care more complicated and expensive.
To maximize the benefit of delivering psychological therapies for mental health problems to people who also have long-term health conditions (LTCs), new IAPT services are being developed that ensure physical and mental health care is co-ordinated and co-located. Psychological therapy protocols are also being adapted to take into account the features of particular LTC and to also promote self-management of aspects of the LTC.
Expanding IAPT is a financial challenge as health service budgets are tight. The recent development of digitally assisted psychological therapy may be one effective way of increasing the number of people who can be treated with a finite resource. In digitally assisted therapy patients can acquire much of the learning that would occur in face-to-face therapy by working through study modules online with therapists focusing on encouragement of self-study and on enhancing learning. The best digitally assisted therapies can greatly reduce therapist time per patient without loss of effectiveness when compared to traditional face-to-face therapy. For this reason, IAPT is exploring the use of such therapies. Key challenges will include identifying the most effective digitally assisted therapy programs, training IAPT therapists to make effective use of the programs, and identifying the individuals for who the programs are, and are not, likely to be helpful.
Acknowledgements
Richard Layard and David M Clark are two of the original architects of the IAPT program. DMC has also served as a Clinical and Informatics Advisor to the UK Government Bodies (Department of Health and NHS England) that developed the program. However, the views expressed in this article are personal and not necessarily the same those of any government agency.
IAPT is the work of many. First of all are the key people who helped develop and launch the Program. They include psychologists and therapists Jeremy Clarke, Sheena Liness, Stephen Pilling, David Richards, Tony Roth, and Graham Turpin, psychiatrists Louis Appleby and Ben Wright, general practitioners Alan Cohen and John Haigh, economist Martin Knapp, administrators James Seward, Kathryn Tyson, Karen Turner, Kevin Mullins, Felicity Dorman, and Jeremy Heywood, and ministers of health Alan Johnson, Andy Burnham, Andrew Lansley, Jeremy Hunt, Paul Burstow, and Norman Lamb. None of their efforts would have had an impact without the hard work and innovation of the many thousands of clinicians, data analysts and administrators who work in IAPT services every day in order to improve the prospects for people with common mental health problems. Their efforts are in turn strongly supported by NHS England’s excellent National IAPT team.
DMC acknowledges the support of the Wellcome Trust and the NIHR Oxford Health Biomedical Research Centre.
Footnotes
The actual cost appears to be around £680 per person if one divides the total investment in IAPT in 2015/16 by the total number of courses of treatment or equivalent clinical activity.
The Annual IAPT Report covering April 2015 to March 2016 (NHS Digital 2016) includes detailed information on what happened to the whole cohort of IAPT referrals. Inspection of the discharge codes for referrals suggests that of the 663,087 patients who were considered suitable for IAPT after assessment 81% (537,131) went on to have a course of treatment. The remaining 19% either declined treatment or did not engage.
The ability of IAPT to collect and report outcome data on everyone who is treated is likely to be one of the reasons why the program has been embraced and expanded by three successive government administrations that cover the left, centre and right of political thinking. No other mental health program in England provides politicians with such clear information to show that it is working as planned.
Pybis et al. (2017) have recently replicated this finding using a more recent patient-level download of IAPT data.
Manuscript accepted by Annual Review of Clinical Psychology. Published version will appear on the Annual Review’s website (http://www.annualreviews.org/).
Literature Cited
- Andersson G, Cuijpers P, Carlbring P, Riper H, Hedman E. Guided Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta-analysis. World Psychiatry. 2014;13:288–95. doi: 10.1002/wps.20151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkham M, Margison F, Leach C, Lucock M, Mellor-Clark J, et al. Service profiling and outcomes benchmarking using the CORE-OM: Toward practice-based evidence in the psychological therapies. J Consult Clin Psychol. 2001;69:184–96. doi: 10.1037//0022-006x.69.2.184. [DOI] [PubMed] [Google Scholar]
- Blackburn IM, James IA, Milne DL, Baker C, Standart S, et al. The Revised Cognitive Therapy Scale (Cts-R): Psychometric Properties. Behav Cogn Psychother. 2001;29:431–46. [Google Scholar]
- Chambless DL, Caputo GC, Jasin SE, Gracely EJ, Williams C. The mobility inventory for agoraphobia. Behav Res Ther. 1985;23:35–44. doi: 10.1016/0005-7967(85)90140-8. [DOI] [PubMed] [Google Scholar]
- Clark DM, Canvin L, Green J, Layard R, Pilling S, Janecka M. Transparency about the outcomes of mental health services (IAPT approach): an analysis of public data. Lancet. 2017 doi: 10.1016/S0140-6736(17)32133-5. online pub December 7th. [publically available data is used to understand differences in outcome between IAPT services] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark DM, Fairburn CG, Wessely S. Psychological treatment outcomes in routine NHS services: a commentary on Stiles et al. 2007. Psychol Med. 2008;38:629–34. doi: 10.1017/S0033291707001869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark DM, Layard R, Smithies R, Richards DA, Suckling R, Wright B. Improving access to psychological therapy: Initial evaluation of two UK demonstration sites. Behav Res Ther. 2009;47:910–20. doi: 10.1016/j.brat.2009.07.010. [shows that when services have missing outcome data they over-estimate how well they perform] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor KM, Davidson JRT, Churchill LE, Sherwood A, Foa E, Weisler RH. Psychometric properties of the social phobia inventory (SPIN). New self-rating scale. Br J Psychiatry. 2000;176:379–86. doi: 10.1192/bjp.176.4.379. [DOI] [PubMed] [Google Scholar]
- Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale - Revised. Behav Res Ther. 2003;41:1489–96. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- Delgadillo J, Asaria M, Ali S, Gilbody S. On poverty, politics and psychology: the socioeconomic gradient of mental healthcare utilisation and outcomes. Br J Psychiatry. 2015;209:429–30. doi: 10.1192/bjp.bp.115.171017. [DOI] [PubMed] [Google Scholar]
- DH. The IAPT data handbook. NHS Rep. v2.0.1. Department of Health; London, UK: 2011a. [detailed specification of the all the variables in the IAPT dataset] [Google Scholar]
- DH. No health without mental health: a cross-government mental health outcomes strategy for people of all ages. Mental Health Service Reform Rep. Department of Health; London, UK: 2011b. [Google Scholar]
- Foa EB, Kozak MJ, Salkovskis PM, Coles ME, Amir N. The validation of a new obsessive-compulsive disorder scale: The Obsessive-Compulsive Inventory. Psychol Assessment. 1998;10:206–14. [Google Scholar]
- Gillespie K, Duffy M, Hackmann A, Clark DM. Community based cognitive therapy in the treatment of post-traumatic stress disorder following the Omagh bomb. Behav Res Ther. 2002;40:345–57. doi: 10.1016/s0005-7967(02)00004-9. [early demonstration psychological therapies can do as well in routine settings as in research trials] [DOI] [PubMed] [Google Scholar]
- Griffiths S, Steen S. Improving Access to Psychological Therapies (IAPT) programme: setting key performance indicators in a more robust context: a new perspective. Journal of Psychological Therapies in Primary Care. 2013;2:133–41. [Google Scholar]
- Gyani A, Shafran R, Layard R, Clark DM. Enhancing Recovery Rates: Lessons from Year One of IAPT. Behav Res Ther. 2013;51:597–606. doi: 10.1016/j.brat.2013.06.004. [identifies predictors of variation in recovery rates within IAPT services] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollon SD, Stewart MO, Strunk D. Enduring effects for cognitive behavior therapy in the treatment of depression and anxiety. Annu Rev Clin Psychol. 2006;57:285–315. doi: 10.1146/annurev.psych.57.102904.190044. [DOI] [PubMed] [Google Scholar]
- Hu JC, Gold KF, Pashos CL, Mehta SS, Litwin MS. Role of surgeon volume in radical prostatectomy outcomes. J Clin Oncol. 2003;21:401–5. doi: 10.1200/JCO.2003.05.169. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labour Party. Britain forward not back: manifesto 2005. 2005 ( http://www.politicsresources.net/area/uk/ge05/man/lab/manifesto.pdf)
- Lambert MJ. Bergin and Garfield's Handbook of Psychotherapy and Behavior Change. New York: John Wiley and Sons, Inc; 2013. [Google Scholar]
- Langley GJ, Moen RD, Nolan KM, Nolan TW, Norman CL, Provost LP. The improvement guide: A practival approach to enhancing organizational performance. San Francisco: Jossey-Bass; 2009. [Google Scholar]
- Layard R. Mental health: Britain's biggest social problem?; Presented at No.10 Strategy Unit Seminar on Mental Health; London. 2005. [Google Scholar]
- Layard R, Bell S, Clark DM, Knapp M, Meacher M, et al. The depression report: a new deal for depression and anxiety disorders. LSE Rep. London School of Economics and Political Science; London, UK: 2006. [Google Scholar]
- Layard R, Clark D, Knapp M, Mayraz G. Cost-benefit analysis of psychological therapy. Natl Inst Econ Rev. 2007;202:90–98. [Google Scholar]
- Layard R, Clark DM. Thrive: The Power of Psychological Therapy. London: Penguin Books; 2014a. [outlines the clinical and economic arguments for the IAPT program] [Google Scholar]
- Layard R, Clark DM. Thrive : how better mental health care transforms lives and saves money. Princeton, New Jersey: Princeton University Press; 2014b. [US version of Thrive: The power of psychological therapy. Outline clinical & economic arguments for IAPT] [Google Scholar]
- Marcus SC, Olfson M. National trends in the treatment for depression from 1998 to 2007. Arch Gen Psychiatry. 2010;67:1265–73. doi: 10.1001/archgenpsychiatry.2010.151. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Barlow DH. Dissemination and Implementation of Evidence-Based Psychological Interventions. Oxford: Oxford University Press; 2012. [Google Scholar]
- McHugh RK, Whitton SW, Peckham AD, Welge JA, Otto MW. Patient preference for psychological vs pharmacologic treatment of psychiatric disorders: a meta-analytic review. J Clin Psychiatry. 2013;74:595–602. doi: 10.4088/JCP.12r07757. [meta-analysis demonsrating that patients prefer psychologcal therapies to medication in a 3:1 ratio] [DOI] [PMC free article] [PubMed] [Google Scholar]
- McManus S, Bebbington P, Jenkins R, Brugha T. Mental Health and Wellbeing in England. NHS Digital; Leeds, UK: 2016. Adult Psychiatric Morbitity Survey. 2014. [Google Scholar]
- McManus S, Meltzer T, Brugha P, Bebbington P, Jenkins R. Adult Psychiatric Morbidity in England. Results of a Household Survey. 2007. NHS Health and Social Care Information Centre; Leeds, UK: 2009. [Google Scholar]
- Mental Health Foundation, Mind, Rethink, Salisbury Centre, and Young Minds. We Need to Talk: the case for psychological therapy in the NHS. London: 2006. ( https://www.centreformentalhealth.org.uk/we-need-to-talk ) [Google Scholar]
- Moriana JA, Galvez-Lara M, Corpas J. Psychological treatments for mental disorders in adults: A review of the evidence of leading international organizations. Clin Psychol Rev. 2017;54:29–43. doi: 10.1016/j.cpr.2017.03.008. [DOI] [PubMed] [Google Scholar]
- Mundt JC, Marks IM, Shear MK, Greist JH. The work and social adjustment scale: a simple measure of impairment in functioning. Br J Psychiatry. 2002;180:461–64. doi: 10.1192/bjp.180.5.461. [DOI] [PubMed] [Google Scholar]
- Nathan PE, Gorman JM. A Guide to Treatments That Work. Oxford: Oxford Univeristy Press; 2015. [Google Scholar]
- NHSDigital. Psychological therapies: annual report on the use of IAPT services in England. NHS England Annual Rep. 2014/15. Health and Social Care Information Centre; Leeds, UK: 2015. [Google Scholar]
- NHSDigital. Psychological therapies: annual report on the use of IAPT services in England. NHS England Rep. 2015-16; Health and Social Care Information Centre; Leeds, UK. 2016. [Google Scholar]
- NHSEngland. 2015 Adult IAPT workforce census report. NHS England and Health Education England Rep; London, UK: 2015. [Google Scholar]
- NHSEngland. The five year forward view for mental health. NHS England Mental Health Taskforce Rep; London, UK: 2016a. [Google Scholar]
- NHSEngland. Implementing the five year forward view for mental health. NHS England Rep; London, UK: 2016b. [Describes NHS' future plans for expanding the IAPT program] [Google Scholar]
- NICE. Clinical Guideline 22. National Institute for Clinical Excellence; London,UK: 2004a. Anxiety: management of anxiety (panic disorder, with and without agoraphobia, and generalised anxiety disorder) in adults in primary, secondary and community care. [PubMed] [Google Scholar]
- NICE. Clinical Guideline 23. National Institute of Clinical Excellence; London, UK: 2004b. Depression: management of depression in primary and secondary care. [Google Scholar]
- NICE. Clinical Guideline 31. National Institute of Clinical Excellence; London, UK: 2005a. Obsessive-compulsive disorder: core interventions in the treatment of obsessive-compulsive disorder and body dysmorphic disorder. [PubMed] [Google Scholar]
- NICE. Clinical Guideline 26. National Institute for Clinical Excellence; London, UK: 2005b. Post-traumatic stress disorder (PTSD): The management of PTSD in adults and children in primary and secondary care. [Google Scholar]
- NICE. Technology Appraisal 97. National Institute for Clinical Excellence; London, UK: 2006. Computerized cognitive behaviour therapy for depression and anxiety. [Google Scholar]
- NICE. Clinical Guideline 91. National Institute for Clinical Excellence; London, UK: 2009a. Depression in adults with chronic physical health problem: treatment and management. [Google Scholar]
- NICE. Clinical Guideline 90. National Institute for Clinical Excellence; London, UK: 2009b. Depression: treatment and management of depression in adults. [Google Scholar]
- NICE. Clinical Guideline 123. National Institute for Clinical Excellence; London, UK: 2011. Common mental health disorders: identification and pathways to care. [Summary of many of the clinical guidelines that underpin the IAPT program] [Google Scholar]
- NICE. Clinical Guideline 159. National Institute for Health and Care Excellence; London, UK: 2013. Social anxiety disorder: Recognition, assessment and treatment. [PubMed] [Google Scholar]
- Pimm J. Plan, Do, Study, Act: a methodology for enhancing recovery in your service; Enhancing Recovery in IAPT Services Regional Conf; Birmingham, UK: 2016. [Google Scholar]
- Pybis J, Saxon D, Hill A, Barkham M. The comparative effectiveness and efficiency of cognitive behaviour therapy and generic counselling in the treatment of depression: evidence from the 2nd UK National Audit of psychological therapies. BMC Psychiatry. 2017;17:215. doi: 10.1186/s12888-017-1370-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards DA, Suckling R. Improving access to psychological therapies: phase IV prospective cohort study. Br J Clin Psychol. 2009;48:377–96. doi: 10.1348/014466509X405178. [DOI] [PubMed] [Google Scholar]
- Roth A, Fonagy P. What Works for Whom? A Critical Review of Psychotherapy Research. New York: Guilford Press; 2005. [Google Scholar]
- Roth AD, Pilling S. Using an evidence-based methodology to identify the competencies required to deliver effective cognitive and behavioural therapy for depression and anxiety disorders. Behav Cogn Psychother. 2008;36:129–47. [Google Scholar]
- Salkovskis PM, Rimes KA, Warwick HM, Clark DM. The Health Anxiety Inventory: development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychol Med. 2002;32:843–53. doi: 10.1017/s0033291702005822. [DOI] [PubMed] [Google Scholar]
- Shear MK, Rucci P, Williams J, Frank E, Grochocinski V, et al. Reliability and validity of the Panic Disorder Severity Scale: replication and extension. J Psychiatr Res. 2001;35:293–6. doi: 10.1016/s0022-3956(01)00028-0. [DOI] [PubMed] [Google Scholar]
- Spitzer Rl, Kroenke K, Williams JW, Löwe B. A brief measure for assessing generalized anxiety disorder: The gad-7. Arch Intern Med. 2006;166:1092–97. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stiles WB, Barkham M, Mellor-Clark J, Connell J. Effectiveness of cognitive-behavioural, person centered, and psychodynamic therapies in UK primary care routine practice: replication in a larger sample. Psychol Med. 2007 doi: 10.1017/S0033291707001511. [DOI] [PubMed] [Google Scholar]
- WHO. The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. Geneva: World Health Organisation; 1992. [Google Scholar]