Synopsis
Tele-ICUs are a relatively recent innovation to deal with several issues such as ICU personnel shortage and improving care. In tele-ICUs, clinical teams monitor ICU patients remotely and support clinicians in multiple ICUs. The tele-ICU and ICU clinicians function as virtual teams. Little is known how these virtual teams function and what challenges they encounter. We examined the challenges from the perspective of nurses in a tele-ICU. We used a case study design and conducted interviews with 10 tele-ICU nurses. The nurses encounter several challenges in interacting with the multiple ICUs that they monitor remotely and have developed a range of strategies to cope with these challenges.
Keywords: Virtual teams, dynamic relationships, intensive care units, tele-medicine
INTRODUCTION
Intensive care units (ICUs) are highly complex organizations where lives are hanging by a thread. Approximately 400,000 to 500,000 people die each year in American ICUs 1,2. The highly complex environment and large responsibilities put a burden on ICU staff. There is a shortage of ICU personnel 3–7, and in the past decades, the number of critical care beds has increased while the number of hospitals offering critical care services has decreased. Tele-ICUs may be a solution for the shortage of ICU personnel. In a tele-ICU, patients are monitored remotely by physicians and nurses trained in critical care. A tele-ICU nurse can monitor up to as many as 50 ICU patients in different ICUs and hospitals. Tele-ICU nurses use the most recent technology that provides access to patient information as well as video and audio links to patient rooms. Tele-ICU physicians and nurses collaborate with physicians and nurses in the ICUs in what can be considered virtual teams. We know little about the collaboration between staff in the tele-ICU and ICUs in this type of virtual team. Tele-ICUs are virtual teams that pose unique challenges because of their dynamic fluid membership: tele-ICU nurses and physicians have to deal with many ICUs simultaneously 8. In this paper, we describe the work system barriers experienced by tele-ICU nurses and identify strategies tele-ICU nurses use in dealing with these barriers. We also explore the negative or positive consequences of strategies.
BACKGROUND
Tele-ICUs are units where intensivists and nurses provide 24/7 care, support and advice from a distance to remote ICUs. Various forms of health information technology (IT) are used to support the sharing of information between the tele-ICU and the ICUs. Technologies allow tele-ICU intensivists and nurses to monitor patients, to observe patients and medical devices in the patient room though a camera, and to communicate with ICU nurses and providers. Several studies provide a detailed description of the evolution of the tele-ICU, the tele-ICU organization, and tele-ICU nurses’ activities 3,7,9–13. Tele-ICUs are a relatively new phenomenon; but the “oldest” tele-ICU has already been in existence for more than 15 years 3. Nearly 10% of patients in American ICUs are currently monitored by tele-ICUs 9.
The tele-ICU team can be comprised of multiple clinicians: board-certified intensivists, critical care nurses, clerical personnel and, in some instances, a pharmacist. Personnel in the ICU (including residents on duty in the ICU) receive instructions or guidance from the tele-ICU staff and may have the opportunity to learn new skills and knowledge 14. Tele-monitoring is crucial to the tele-ICU model. Personnel in the tele-ICU receive patient data in real time and, therefore, can detect trends in patient status; they can then alert personnel in the ICU 15.
Tele-ICU physicians and nurses work at workstations that are commonly composed of multiple monitors, a two-way camera, microphone, and a high-speed dial phone. Clinical data captured about the ICU patient are directly streamed to the tele-ICU. Tele-ICU clinicians are dependent on information communicated over the phone or entered into the computer from the bedside to inform them on the current state of the patient. They monitor numerous clinical indicators, such as blood pressure, heart rate, ventilator settings, and oxygen saturation. Other data such as patient care plans, labatory results, and X-rays are electronically sent or faxed to the tele-ICU. Most tele-ICU software uses “smart alarms” to alert the clinicians to possible significant changes in patient status.
Tele-ICU Literature
Most studies on the tele-ICU have focused on clinical and financial outcomes 16–22. Several studies have reported that implementation of an ICU telemedicine program can improve clinical care outcomes (e.g., reduced length of stay, reduced mortality, reduced complications) and reduce healthcare costs 16,19–24. However, other studies have failed to confirm some of these positive outcomes 25–28.
The study by Anders and colleagues 15 focuses on the functions of the tele-ICU. The researchers performed 40 hours of observation of eight tele-ICU nurses and one tele-ICU physician in one tele-ICU. Results showed that the tele-ICU fulfills three functions: (1) anomaly response: tele-ICU nurses processed information related to alerts and alarms and contacted other staff in the tele-ICU or the ICU if they perceived the need for follow-up or action; (2) access to specialized expertise: experienced tele-ICU nurses were observed to mentor junior ICU nurses; ICU nurses had access to expertise and experience of the tele-ICU nurses thereby augmenting their knowledge base; and (3) sense-making: tele-ICU nurses can make sense of what is happening with patients because they have access to many sources of data and have the resources (time, expertise) to synthesize the data. Research on tele-ICUs is limited; in particular nursing issues related to tele-ICU have been overlooked 29. Few studies have explored how tele-ICU nurses deal with multiple interactions across varied ICUs and hospitals 30,31. We need to know more about the work system barriers experienced by tele-ICU nurses, as well as the strategies they use to deal with these barriers and their consequences.
METHODS
Study design
We used a case study design to investigate work system barriers experienced by tele-ICU nurses and strategies they use to deal with multiple ICUs 32,33. A case study can be defined as a research strategy and an empirical inquiry that investigates a phenomenon within its real-life context, using multiple data collection instruments. We used various methods (observations, interviews, surveys and field notes) to collect data in the tele-ICU. In this paper we focus on the analysis of interview data.
Setting/sample
The participating tele-ICU has been in existence since 2003 and monitors 260 beds in 15 ICUs of 6 different hospitals. The tele-ICU employs totally 42 nurses and 20 physicians in different shifts. On average, a tele-ICU nurse monitors 45 beds. We interviewed 10 tele-ICU nurses who volunteered to participate in the study.
Data collection instrument
We used a semi-structured interview guide (see http://cqpi.wisc.edu/wp-uploads/2016/07/Tele-ICU_Nurse_Interview_Guide.pdf for the interview guide). The interviews addressed the following topics: a typical day in the tele-ICU; tools and software used; interaction with multiple ICUs; how to deal with crisis situations; communication between tele-ICU and ICU; relationship with ICUs; trust in relationships with ICUs; and quality of care. In this paper we examine work system barriers experienced by tele-ICU nurses in dealing with multiple ICUs. The questions asked included: “What are the challenges of interacting with multiple ICUs”? We used additional prompts such as: “Why is it easy? – Could you give us specific examples?’; Why is it difficult? – Could you give us specific examples”? The interviews lasted about one hour. Interviews were audio-recorded, transcribed and made anonymous to protect confidentiality of the interviewees. The study was approved by the Institutional Review Board of the University of Wisconsin – Madison.
Data analysis
Interview data were analyzed using the qualitative data analysis NVivo© software. The transcripts of the interviews were imported in NVivo© and were coded to answer the research question. We took several steps to analyze the data. First, we identified barriers and strategies used by tele-ICU nurses to deal with the barriers. This initial coding was performed on two interview transcripts. Over several team meetings, we discussed the coding, and began to create nodes (major categories of interview text based on their content similarities and unique relationships) for the three major topics related to our research objective: work system barriers, strategies to deal with the barriers, and consequences of the strategies. The researchers then coded the text in NVivo© and identified barriers, strategies and consequences, while keeping track of the nodes, their definitions and examples. Finally, we created three matrices to link (1) barriers and strategies, (2) strategies and consequences, and (3) barriers and consequences. We also computed frequencies for each barrier, strategy and consequence. When a nurse mentioned a specific topic several times during the interview, the topic was counted as one. The minimum number of times a topic is mentioned is 1 (one nurse); and the maximum is 10 (10 nurses mentioned it).
RESULTS
Barriers
The 10 tele-ICU nurses mentioned a total of 166 barriers in dealing with multiple ICUs. The barriers were categorized in 6 main categories: barriers with regard to the particular characteristics of the different ICUs; barriers with regard to patient care; barriers with regard to the relationship between the ICUs and the tele-ICU; barriers with regard to the technology; barriers associated with the organization of the tele-ICU; and barriers in the tasks of tele-ICU nurses. Results are summarized in Table 1.
Table 1.
Barriers reported by tele-ICU nurses
| Barriers | Examples | # of nurses |
|---|---|---|
| Barriers related to characteristics of the ICUs | ||
| Variety of ICUs | Different ICUs have different characteristics and differences in the way work is organized. | 7 |
| Variety in ICU care processes | Different ICUs have different patient care processes and protocols. | 6 |
| Variety of ICU staff | Different ICU clinicians have different personalities, behaviors and characteristics. | 8 |
| Limited ICU nurse experience | ICU RNs have limited experience in the ICU. | 5 |
| Barriers with regard to patient, patient information and patient care issues | ||
| Lack of and poor access to patient-related information | The tele-ICU RN has limited access to patient-related information or cannot find patient-related information. | 3 |
| Lack of care for patient from ICUs | ICU may be too busy with one patient and may not be able to provide care to the other patient. | 2 |
| Lack of knowledge of patient | The tele-ICU RN has limited knowledge or not the most up-to-date patient information about a patient. | 7 |
| Lack of or poor documentation | Documentation on patient care is lacking or poor. | 6 |
| Barriers in the relationship between tele-ICU and ICU | ||
| ICU’s lack of familiarity with tele-ICU staff and purpose | ICU staff has lack of familiarity with tele-ICU staff and the purpose of the tele-ICU. | 10 |
| Lack of acceptance of tele-ICU | The ICU clinicians do not accept the tele-ICU, do not want to work with the tele-ICU, and do not see value of the tele-ICU. | 9 |
| Lack of or poor communication with ICU | The communication between the tele-ICU RN and ICU staff is limited or poor. | 6 |
| Lack of familiarity with ICU staff | The tele-ICU RN is not familiar with the ICU staff. | 9 |
| Lack of or variety of trust between tele-ICU and ICU | There is a variety in trust from tele-ICU to ICUs and vice versa. | 8 |
| Tele-ICU RN has lack of awareness regarding of what’s happening in ICUs | Tele-ICU RN does not know what’s going on in the ICU. For example, how busy the ICU is, the workload of the ICU RNs, etc. | 5 |
| Variety in acceptance and use of tele-ICU | There are differences in level of acceptance and use of the tele-ICU by the ICUs. Some ICUs need the tele-ICU more than others. | 9 |
| Conflict with ICU | The tele-ICU RN has a different opinion about patient care than ICU staff. | 6 |
| Barriers with regard to the technology (equipment, devices, or health information technology) | ||
| Lack of familiarity with and knowledge of ICU equipment or devices | The tele-ICU RN does not know or is not familiar with ICU equipment and devices (e.g. ventilator, infusion pump, and monitors). | 6 |
| Problem with tele-ICU equipment or software | ICUs do not use tele-ICU software to document because ICUs have lack of familiarity with tele-ICU software such as VISICU software. | 5 |
| General IT problems | Tele-ICU RN has problem with IT, either with tele-ICU equipment/software or other IT problem(s). | 2 |
| Barriers with regard to the organization and characteristics of the tele-ICU | ||
| Variation in ICU assignment | The tele-ICU RN gets assigned to different ICUs for each shift. | 2 |
| Variation of tele-ICU staff, work styles and personalities | The clinicians in the tele-ICU have a variety of personalities and the tele-ICU RN has to learn to work with different personalities. | 2 |
| Barriers with regard to the job or task design of tele-ICU nurses | ||
| Cognitive or memory load | The tele-ICU RN has to remember different things, including ways of login into EHR, passwords, way to access information, etc. | 9 |
| High workload | The tele-ICU RN experiences high workload, for example because of the number of admissions, demands from multiple ICU staff, insufficient staff coverage, etc. | 10 |
| Interruption(s) | The tele-ICU RN is interrupted when performing his/her tasks | 9 |
| Staying vigilant | It is hard for tele-ICU RN to stay alert and awake, and maintain attention after prolonged periods in his/her shift. | 3 |
| Uncertainty | The tele-ICU RN experiences uncertainty with regard to what will happen next. | 3 |
Strategies
Tele-ICU nurses mentioned 98 instances of strategies in dealing with the barriers; those were categorized in 14 major strategies. Table 2 shows data for strategies.
Table 2.
Strategies used by tele-ICU nurses in dealing with barriers
| # | Strategies | Description | # of nurses |
|---|---|---|---|
| 1 | Adapt to ICU | The tele-ICU nurse has to adapt the way they deal with ICU staff, so they can be more receptive to the tele-ICU. | 7 |
| 2 | Anticipate or prevent problems | Tele-ICU nurse anticipate problem and take action to prevent problems. | 8 |
| 3 | Ask for (additional) information | The tele-nurse asks for (additional or specific) information from ICU staff to assess changes in patient conditions, ICU protocols, ICU equipment, when tele-ICU nurse cannot find information on the flow sheet. | 7 |
| 4 | Ask for support | The tele-ICU nurse asks for help and support from their colleagues in the tele-ICU in order to handle multiple ICUs. | 9 |
| 5 | Check information | The tele-ICU nurse checks to make sure that the patient information that s/he has is correct | 4 |
| 6 | Facilitate communication | The tele-ICU nurse performs actions that may improve relationships and communications with ICUs. | 10 |
| 7 | Figure out | The tele-ICU nurse tries to figure out how to work with different ICUs, different EHRs and different ICU nurses (i.e. how to communicate with them). | 6 |
| 8 | Obtain and search for (additional) information | The tele-ICU nurse obtains and searches for (additional) patient related information without interacting with ICU staff. | 8 |
| 9 | Organize information and tasks | The tele-ICU nurse better organizes the available patient information in order to help him/her deal with multiple patients. For example, tele-ICU nurse uses paper notes to keep track of patient, uses a mental checklist to remember what to come back to after getting interrupted. | 10 |
| 10 | Prioritize | The tele-ICU nurse makes active decisions on what problem to tackle first. For example, when there are a lot of admissions, tele-ICU nurse needs to prioritize which patient to handle first. | 4 |
| 11 | Provide support | The tele-ICU nurse provides informational or emotional support to ICU nurses or tele-ICU nurses to help them taking care of patients. | 10 |
| 12 | Share information | The tele-ICU nurse shares information (such as standardized protocol) with ICUs. | 4 |
| 13 | Take little or no action | The tele-ICU nurse does not interact with ICU nurses because of lack of ICU acceptance. | 4 |
| 14 | Workaround problem | The tele-ICU nurse works around the problem. For example, the tele-ICU nurse uses password cheat sheets to help him/her remember the passwords, the tele-ICU nurse tricks the system to log in | 9 |
Consequences
Although we did not explicitly ask about possible consequences of dealing with barriers in interacting with multiple ICUs, nurses reported a total of 25 instances of consequence that were categorized into 12 major categories (see Table 3).
Table 3.
Consequences of dealing with barriers experienced by tele-ICU nurses
| # | Consequences | Description | # of nurses |
|---|---|---|---|
| 1 | Additional workload | The tele-ICU RN experiences additional workload. | 1 |
| 2 | Delay in patient care | Care provided to an ICU patient is delayed (e.g., delay in assistance, delay in switching between patients). | 1 |
| 3 | Error | Tele-ICU RN makes error when she deals with multiple ICUs. For example, tele-ICU RN entered information into the wrong patient chart or missed alerts. | 1 |
| 4 | Improved patient care | The care provided to the ICU patient is improved. | 1 |
| 5 | Improved relationship between tele-ICU and ICU | The relationship between the tele-ICU and ICU is improved (e.g., more information provided, experience of RN aids credibility) | 5 |
| 6 | Increased knowledge about patient by tele-ICU | The tele-ICU RN has additional knowledge about the patient, e.g., because of increased communication with the ICU | 1 |
| 7 | No impact on patient care | There is no impact on care provided to the ICU patient | 1 |
| 8 | Poor communication | Communication between the ICU and tele-ICU RN is negatively affected | 1 |
| 9 | Feeling bad | Tele-ICU RN feels bad about her work in the tele-ICU or bad because of lack of acceptance by ICU RN | 3 |
| 10 | Frustrating | Frustration is experienced by the tele-ICU RN. | 4 |
| 11 | Stressful | Stress is experienced by the tele-ICU RN | 3 |
| 12 | Time consuming | The tele-ICU spends more time performing tasks (e.g., finding information, navigating systems, logging in). | 1 |
Relationships between barriers, strategies, and consequences in interacting with multiple ICUs
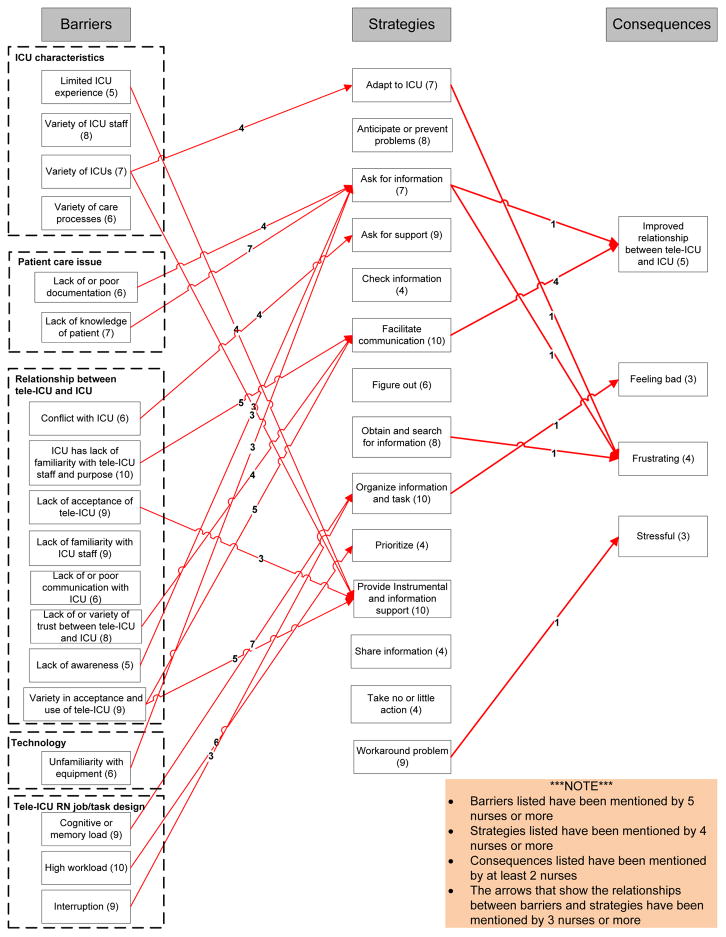
The relationships between barriers, strategies and consequences are displayed in Figure 1. Only the main data are shown in Figure 1 in order to facilitate reading and comprehension of the graph. Barriers were included if they were mentioned by at least 5 tele-ICU nurses; strategies if they were mentioned by at least 4 nurses; and consequences if they were mentioned by at least 2 nurses. Relationships between barriers and strategies were included if they were mentioned by at least 3 nurses.
Figure 1.
Relationships between barriers, strategies and consequences in dealing with multiple ICUs.
DISCUSSION
Results of our analyses on barriers experienced by tele-ICU nurses in dealing with multiple ICUs show a range of barriers, strategies and consequences. Most comments about barriers concern the relationship of the tele-ICU with the ICUs (see Table 1). A lot of ambiguity and sometimes conflict can occur because the ICUs are not familiar with the tele-ICU and its staff or do not understand the purpose of tele-ICU (mentioned by 10 nurses). We also found limited trust between the tele-ICU and the ICUs (N=8); limited acceptance and use of the tele-ICU by the ICUs (N=9); and –on the tele-ICU side-also lack of familiarity with staff in the different ICUs. All of this can result in poor communication (N=6) and even conflict (N=6).
A second major category of barriers is created by the large diversity in the different ICUs monitored by tele-ICU nurses. The tele-ICU monitors a total of 15 ICUs in 6 different hospitals. This variety in ICUs (mentioned 7 times) implies that tele-ICU nurses deal with a large variety of ICU staff (N=8), variety in the experience of ICU nurses (N=5), and a variety of ICU protocols and care processes (N=6). The tele-ICU nurses, although all trained as ICU nurses themselves, often have limited experience in some types of ICUs (e.g., cardiac ICU in an urban hospital). Tele-ICU nurses have to deal with different kinds of hospitals (teaching, academic etc.) and different ICUs (open and closed ICUs, cardiac, medical, surgical, neurological, special, etc.) within these hospitals. Apart from differences in ICU type, ICUs may have different care processes, protocols, health IT applications and medical devices. All of these differences can, on one hand, be an interesting challenge and provide opportunities for tele-ICU nurses to learn new things; but on the other hand, these differences can be confusing 34.
A third major barrier in the interaction with multiple ICUs is the way the job of a tele-ICU nurse is designed. Tele-ICU nurses mention high mental workload (N=10), have occasional problems with the long 12-hour shifts that require them to stay vigilant for a long time (N=3), and are often interrupted in their activities (N=9). Tele-ICU nurses can monitor up to 50 ICU patients, and are often interrupted with requests from (nurses in) the ICUs that they monitor, and from colleagues (both physicians and nurses) in the tele-ICU. Part of the high workload is the large volume of patients being admitted and discharged. That makes it sometimes difficult to keep track of what is happening with patients and contribute to high cognitive workload (N=9).
Tele-ICU nurses developed a wide range of strategies to deal with the different barriers (see Table 2). We linked the strategies to barriers (see Figure 1). Tele-ICU nurses “react” to barriers using different strategies, e.g., by facilitating communication, providing support, organizing information, and asking for or finding additional information.
Evidently, if tele-ICU nurses can facilitate communication with the ICUs, this strategy can help in reducing or mitigating problems with the relationship with the ICUs 8,35. If the ICU staff realizes that the tele-ICU is there to help and assist them, instead of being “Big Brother” and controlling what they do, that may improve the relationship 7. However, it is interesting to note that tele-ICU nurses still have to rely on these strategies, even after being in existence for 6 years. The large variety in ICU characteristics, ranging from differences in perspectives on patient care to a variety in care processes and protocols to a variety of staff and equipment, and the subsequent high cognitive workload prompt tele-ICU nurses to organize and prioritize the information that they need. With regard to the strategy of organizing and prioritizing information (N=10), most tele-ICU nurses use paper notes (with color codes) to keep track of what they were doing when they were interrupted. Many of them use these paper notes for the handoffs. In dealing with simultaneous dynamic relationships with multiple ICUs, tele-ICU nurses use a large range of strategies to deal with multiple challenges.
Strategies are often helpful with more than one type of barriers. As shown in Figure 1, the strategy of asking for information is used by tele-ICU nurses to deal with barriers related to patient care issues as well as unfamiliarity with equipment. Tele-ICU nurses deal with barriers related to the ICUs’ lack of familiarity and knowledge of the tele-ICU and ICUs’ lack of acceptance of the tele-ICU by engaging in communication with the ICUs.
Finally, tele-ICU nurses mentioned a number of consequences of dealing with barriers (see Table 3). When strategies for certain problems are successful, this can result in improved relationships between the tele-ICU and ICUs and improved quality of care and patient safety 14. However, when tele-ICU nurses cannot successfully cope with barriers, this can lead to frustration, stress, and other negative feelings 7,8.
Study Limitations
This study took place in one tele-ICU and, therefore, the generalizability of the results is limited. During the semi-structured interviews, we asked nurses about barriers they experienced in dealing with muliple ICUs. Probes and follow-up questions were used to ask nurses about how they dealt with strategies; but we did not explicitely and consistently ask them about potential consequences or outcomes. Therefore, data on consequences should be considered as exploratory. Further research is needed to deepen our understanding of the impact of barriers and strategies used by tele-ICU nurses to manage a large number of diverse ICUs.
Key Points.
There is a shortage of intensive care personnel, both intensivists and critical nurses.
This shortage can partly be remediated by implementation of tele-ICUs.
The literature shows that tele-ICUs can have several benefits (improved clinical outcomes), but that the virtual collaboration between personnel in the ICUs that are monitored and the tele-ICU can be difficult.
Tele-ICU nurses have to deal with many different hospitals, ICUs, ICU staff, health information technology, medical devices and protocols which makes their life difficult. This lack of familiarity can cause all kind of barriers and tele-ICU nurses have to develop strategies to deal with these barriers.
Implications for nursing practice?
Several of the recommendations below pertain to the concept of “familiarity breeds trust”. Results of this study have shown that unfamiliarity with and the variety in ICUs, ICU staff, ICU processes and procedures, and ICU technology are related to many of the barriers in the work of a tele-ICU nurse.
When implementing the tele-ICU:
Include ICU clinicians in an early stage in the design and implementation of the tele-ICU
Build support for tele-ICU coverage before roll-out
Designate an ICU champion
If possible, have personnel of the tele-ICU and the ICUs that are to be monitored meet each other. Face-to-face contact reduces many of the barriers that we have found in this study
Install 2-way (instead of one-way) cameras
After having implemented the tele-ICU
If possible, continue to organize meetings in which tele-ICU personnel and ICU personnel can meet. Face-to-face contact reduces many of the barriers that we have found in this study
If possible, make a visit to the tele-ICU as part of the educational program for physicians and nurses. Often a visit to the tele-ICU results in a better understanding of what the tele-ICU exactly does (and what it does not do).
Evidently, tele-ICU personnel would be benefit greatly from standardization in the ICUs that they monitor. However, in many (but not all!) cases tele-ICUs monitor ICUs in separate health systems that use different technology (e.g. EHRs, smart pumps, etc.) and processes, which makes a standardized approach very difficult. However, within healthcare organizations that have several hospitals and ICUs, processes and technolgy can be standardized with often very positive outcomes 36. And tele-ICU implementation itself often has some standardization of care as a result 35.
Some of the procedures with regard to communication with the ICUs that are monitored can be standardized. This creates clearer expectations about responsibilities of the personnel in the ICU and in the tele-ICU.
Another form of standardization can be achieved by designing policies and procedures for the use of the in-room cameras, speakers, and microphones 37. The use of this technology often results in a feeling of “Big Brother is watching me” in ICU rooms.
Hiring tele-ICU nurses who have worked or a still working part-time in the ICUs that are monitored does improve the relationship between nurses in the tele-ICU and ICU and increases trust and satisfaction 8.
Since 2011 tele-ICU nursing is recognized as a professional specialty and nurses working in the tele-ICU can get a CCRN-E certification 38. Being a tele-ICU nurse indeed requires specific skills and knowledge to be able to provide care at a distance. Recognizing the difficulties that virtual teamwork can generate, such as having to cope with a large variety of ICU characteristics and the lack of amiliarity with the ICU context, but trying to establish relationships and trust with the nurses in the ICUs requires effort from tele-ICU nurses. They should be made aware of these (potential) problems and trained in how to cope with the problems of virtual teams.
Acknowledgments
This study was made possible with support from the National Science Foundation (NSF Grant #: OCI-0838513, PI: Carayon, and NSF grant # CMMI 1536987, PI: Li) and the cooperation from the manager and the nurses who work in the tele-ICU.
Footnotes
disclosure statement
The authors have no conflict of interest.
Contributor Information
Peter L.T. Hoonakker, Senior Scientist, Center for Quality and Productivity Improvement, University of Wisconsin-Madison, Madison, WI 53706, USA.
Pascale Carayon, Professor in the Department of Industrial and Systems Engineering and Director of the Center for Quality and Productivity Improvement, University of Wisconsin-Madison, Madison, WI 53706, USA.
References
- 1.Angus DC, Linde-Zwirble WT, Sirio CA, et al. The effect of managed care on ICU length of stay: implications for medicare. JAMA. 1996;276(13):1075–1082. [PubMed] [Google Scholar]
- 2.Mukhopadhyay A, Tai BC, See KC, et al. Risk factors for hospital and long-term mortality of critically ill elderly patients admitted to an intensive care unit. BioMed research international. 2014;2014:960575. doi: 10.1155/2014/960575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Breslow MJ. Remote ICU care programs: current status. J Crit Care. 2007;22(1):66–76. doi: 10.1016/j.jcrc.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 4.Juraschek SP, Zhang X, Ranganathan V, Lin VW. United States Registered Nurse Workforce Report Card and Shortage Forecast. Am J Med Qual. 2012;27(3):241–249. doi: 10.1177/1062860611416634. [DOI] [PubMed] [Google Scholar]
- 5.Bureau of Labor Statistics (BLS) Table 6: The 30 occupations with the largest projected employment growth, 2014–24. [Accessed February 2017, 2016];Economic News Release. 2016 http://www.bls.gov/news.release/ecopro.t06.htm.
- 6.Allen L. The nursing shortage continues as faculty shortage grows. Nursing Economic$ 2008;26(1):35–40. [PubMed] [Google Scholar]
- 7.Mullen-Fortino M, DiMartino J, Entrikin L, Mulliner S, Hanson CW, Kahn JM. Bedside nurses’ perceptions of Intensive Care Unit telemedicine. American Journal of Critical Care. 2012;21(1):24–32. doi: 10.4037/ajcc2012801. [DOI] [PubMed] [Google Scholar]
- 8.Hoonakker PLT, Pecanac KE, Brown RL, Carayon P. Virtual collaboration, satisfaction and trust between nurses in the tele-ICU and ICUs: Results of a multi-level analysis. Journal of Critical Care. 2017;37:224–229. doi: 10.1016/j.jcrc.2016.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lilly CM, Thomas EJ. Tele-ICU: Experience to date. Journal of Intensive Care Medicine. 2009;25(1):16–22. doi: 10.1177/0885066609349216. [DOI] [PubMed] [Google Scholar]
- 10.Stafford TB, Myers MA, Young A, Foster JG, Huber JT. Working in an eICU unit: life in the box. Crit Care Nurs Clin North Am. 2008;20(4):441–450. doi: 10.1016/j.ccell.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 11.Tang Z, Weavind L, Mazabob J, Thomas EJ, Chu-Weininger MYL, Johnson TR. Workflow in intensive care unit remote monitoring: A time-and-motion study. Critical Care Medicine. 2007;35(9):2057–2063. doi: 10.1097/01.ccm.0000281516.84767.96. [DOI] [PubMed] [Google Scholar]
- 12.Hoonakker PLT, Khunlertkit A, Mcguire K, Wiegmann DA, Carayon P, Wood KE. A day in life of a tele-Intensive Care Unit nurse. In: Albolino S, Bagnara S, Bellandi T, Llaneza J, Rosal G, Tartaglia R, editors. Healthcare Systems Ergonomics and Patient Safety 2011. Leiden, The Netherlands: CRC Press; 2011. pp. 43–46. [Google Scholar]
- 13.Nielsen M, Saracino J. Telemedicine in the intensive care unit. Critical Care Nursing Clinics. 2012;24(3):491–500. doi: 10.1016/j.ccell.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Khunlertkit A, Carayon P. Contributions of tele–intensive care unit (Tele-ICU) technology to quality of care and patient safety. Journal of Critical Care. 2013;28(3):315.e311–315.e312. doi: 10.1016/j.jcrc.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 15.Anders S, Patterson ES, Woods DD, Ebright P. Projecting trajectories for a new technology based on cognitive task analysis and archetypal patterns: The electronic ICU. 8th Annual Naturalist Decision Making Conference; 2007; Asilomar, CA. [Google Scholar]
- 16.Zawada ETJ, Herr P, Larson D, Fromm R, Kapaska D, Erickson D. Impact of an intensive care unit telemedicine program on a rural health care system. Postgrad Med. 2009;121(3):160–170. doi: 10.3810/pgm.2009.05.2016. [DOI] [PubMed] [Google Scholar]
- 17.Ries M. Tele-ICU: A new paradigm in critical care. International Anesthesiology Clinics. 2009;47(1):153–170. doi: 10.1097/AIA.0b013e3181950078. [DOI] [PubMed] [Google Scholar]
- 18.Thomas EJ, Chu-Weininger MYL, Lucke J, Wueste L, Weavind L, Mazabob J. The impact of a tele-ICU provider attitudes about teamwork and safety climate. Crit Care Med. 2007;35:A145. doi: 10.1136/qshc.2007.024992. [DOI] [PubMed] [Google Scholar]
- 19.Breslow MJ, Rosenfeld BA, Doerfler M, et al. Effect of a multiple-site intensive care unit telemedicine program on clinical and economic outcomes: An alternative paradigm for intensivist staffing. Critical Care Medicine. 2004;32(1):31–38. doi: 10.1097/01.CCM.0000104204.61296.41. [DOI] [PubMed] [Google Scholar]
- 20.Willmitch B, Golembeski S, Kim SS, Nelson LD, Gidel L. Clinical outcomes after telemedicine intensive care unit implementation. Crit Care Med. 2012;40(2):450–454. doi: 10.1097/CCM.0b013e318232d694. [DOI] [PubMed] [Google Scholar]
- 21.Chen J, Sun D, Yang W, et al. Clinical and economic outcomes of telemedicine programs in the intensive care unit: A systematic review and meta-analysis. Journal of Intensive Care Medicine. 2017 doi: 10.1177/0885066617726942. ePub ahead of print. [DOI] [PubMed] [Google Scholar]
- 22.Rosenfeld BA, Dorman T, Breslow MJ, et al. Intensive care unit telemedicine: alternate paradigm for providing continuous intensivist care. Crit Care Med. 2000;28(12):3925–3931. doi: 10.1097/00003246-200012000-00034. [DOI] [PubMed] [Google Scholar]
- 23.Coustasse A, Deslich S, Bailey D, Hairston A, Paul D. A business case for tele-intensive care units. The Permanente Journal. 2014;18(4):76–84. doi: 10.7812/TPP/14-004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilcox ME, Adhikari NK. The effect of telemedicine in critically ill patients: systematic review and meta-analysis. Critical care (London, England) 2012;16(4):R127. doi: 10.1186/cc11429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Young LB, Chan PS, Lu X, Nallamothu BK, Sasson C, Cram PM. Impact of telemedicine intensive care unit coverage on patient outcomes: A systematic review and meta-analysis. Arch Intern Med. 2011;171(6):498–506. doi: 10.1001/archinternmed.2011.61. [DOI] [PubMed] [Google Scholar]
- 26.Kumar S, Merchant S, Reynolds R. Tele-ICU: Efficacy and cost-effectiveness of remotely managing critical care. Perspectives in Health Information Management. 2013 Spring;2013:1–13. [PMC free article] [PubMed] [Google Scholar]
- 27.Thomas EJ, Lucke J, Wueste L, Weavind L, Patel B. Association of telemedicine for remote monitoring of intensive care patients with mortality, complications, and length of stay. JAMA. 2009;302(24):2671–2678. doi: 10.1001/jama.2009.1902. [DOI] [PubMed] [Google Scholar]
- 28.Morrison JL, Cai Q, Davis N, et al. Clinical and economic outcomes of the electronic intensive care unit: Results from two community hospitals. Crit Care Med. 2010;38(1):2–8. doi: 10.1097/CCM.0b013e3181b78fa8. [DOI] [PubMed] [Google Scholar]
- 29.Cummings J, Krsek C, Vermoch K, Matuszewski K. Intensive care unit telemedicine: Review and consensus recommendations. Am J Med Qual. 2007;22(4):239–250. doi: 10.1177/1062860607302777. [DOI] [PubMed] [Google Scholar]
- 30.Zuiderent T, Winthereik BR, Berg M. Talking about distributed communication and medicine: On bringing together remote and local actors. Human-Computer Interaction. 2003;18(1–2):171–180. [Google Scholar]
- 31.Young LB, Chan PS, Cram P. Staff acceptance of tele-icu coverage: A systematic review. CHEST Journal. 2011;139(2):279–288. doi: 10.1378/chest.10-1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hoonakker PLT, Carayon P, Khunlertkit A, Mcguire K, Wiegmann DA. Case study research: An example from the tele-ICU. In: Goebel M, Christie CJ, Zschernack S, Todd AI, Mattison M, editors. Organizational Design And Management (ODAM) X. Grahamstown, South Africa: IEA Press; 2011. pp. 121–127. [Google Scholar]
- 33.Yin RK. Case study research: Design and methods. Newbury Park, CA: Sage; 1984. [Google Scholar]
- 34.Hoonakker PLT, Carayon P, McGuire K, et al. Motivation and job satisfaction of tele-ICU nurses. Journal of Critical Care. 2013;28(3):315e313–315.e321. doi: 10.1016/j.jcrc.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 35.Goedken CC, Moeckli J, Cram PM, Reisinger HS. Introduction of tele-ICU in rural hospitals: Changing organisational culture to harness benefits. Intensive & critical care nursing. 2017;40:51–56. doi: 10.1016/j.iccn.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 36.Irwin RS, Flaherty HM, French CT, Cody S, Chandler MW, Lilly CM. Interdisciplinary collaboration: The slogan that must be achieved for models of delivering critical care to be successful. Chest. 2012;142(6):1611–1619. doi: 10.1378/chest.12-1844. [DOI] [PubMed] [Google Scholar]
- 37.Shahpori R, Hebert M, Kushniruk A, Zuege D. Telemedicine in the intensive care unit environment—A survey of the attitudes and perspectives of critical care clinicians. Journal of Critical Care. 2011;26(3):328.e329–328.e315. doi: 10.1016/j.jcrc.2010.07.013. [DOI] [PubMed] [Google Scholar]
- 38.Goran SF. A new view: Tele-intensive care unit competencies. Critical Care Nurse. 2011;31(5):17–29. doi: 10.4037/ccn2011552. [DOI] [PubMed] [Google Scholar]