Abstract
Introduction:
In line with Article 14 guidelines for the WHO Framework Convention on Tobacco Control, we aimed to assess the progress in training individuals to deliver tobacco cessation treatment.
Methods:
Cross-sectional web-based survey in May–September 2013 among 122 experts in tobacco control and training from 84 countries (73% response rate among 115 countries surveyed). We measured training program prevalence, participants, and challenges faced.
Results:
Overall, 21% ( n = 18/84) of countries, mostly low and middle-income countries (LMICs; P = .002), reported no training program. Among 66 countries reporting at least one training program, most (84%) trained healthcare professionals but 54% also trained other individuals including community health workers, teachers, and religious leaders. Most programs (54%) cited funding challenges, although stability of funding varied by income level. Government funding was more commonly reported in higher income countries (high 56%, upper middle 50%, lower middle 27%, low 25%; P = .03) while programs in LMICs relied more on nongovernmental organizations (high 11%, upper middle 37%, lower middle 27%, low 38%; P = .02).
Conclusions:
One in five countries reported having no tobacco treatment training program representing little progress in terms of training individuals to deliver tobacco treatment in LMICs. Without more trained tobacco treatment providers, one of the tenets of Article 14 is not yet being met and health inequalities are likely to widen. More effort and resources are needed to ensure that healthcare worker educational programs include training to assess tobacco use and deliver brief advice and that training is available for individuals outside the healthcare system in areas with limited healthcare access.
Introduction
Tobacco use is a leading cause of preventable death globally, with nearly 6 million deaths from tobacco-related illness each year, more than HIV, tuberculosis and malaria combined. 1 The greatest burden of tobacco related illness has historically been in high-income countries but this is changing. Of the nearly 1 billion smokers worldwide, 80% now live in low and middle-income countries (LMICs). 1
In 2005, the Framework Convention on Tobacco Control (FCTC) became the world’s first international public health treaty. 2 The FCTC aims to reduce the health consequences of tobacco use by promoting policies that prevent initiation of tobacco use and help existing tobacco users to quit. Article 14 of the FCTC directs countries to implement effective programs to help tobacco users to quit using evidence-based counseling and medication. In 2010, the Conference of the Parties to the FCTC introduced guidelines for implementing Article 14. 3 The guidelines recommend that countries develop national training standards for delivering tobacco dependence treatment and specify that healthcare systems and healthcare workers “should play a central role in promoting tobacco cessation and offering support to tobacco users” 3 through tobacco use screening, brief advice and referral to specialized treatment services where appropriate.
One of the key resources needed to implement Article 14 is sufficient numbers of healthcare workers trained to assess tobacco use and deliver brief advice about tobacco cessation. Prior studies show a need to improve healthcare worker training. The 2005 Global Health Professions pilot survey found that only between 6% and 37% of healthcare students in 10 countries received training in tobacco treatment. 4 The Article 14 guidelines also recommend training individuals outside the healthcare system to give brief advice and refer tobacco users to specialized services such as telephone quitlines. Having specialized treatment services to which healthcare workers and others can refer tobacco users requires individuals trained in behavioral and pharmacologic support for tobacco cessation. There is little information about the status of tobacco treatment training programs for healthcare workers, for individuals outside of the healthcare system, and for tobacco treatment specialists.
In 2008, we surveyed tobacco treatment training programs in 48 countries stratified by region and income level. 5 We found that training programs had increased in number in the decade prior to the survey and were more common in high-income than low-income countries. All programs reported that funding was a major challenge. To update this work, in 2013 we administered a new survey of training programs to a larger sample of informants in tobacco control and treatment. Our objective was to assess the availability and content of tobacco training programs in countries across different regions and income levels. We describe training methods and content in a separate paper. For this article, we measured training program availability and challenges and assessed which groups of individuals are being trained to deliver treatment to meet the human resource needs of implementing tobacco treatment services around the world.
Methods
Sample
We used nonprobability sampling methods to identify experts involved in tobacco treatment training around the world. First, we identified a sample of national and regional experts in tobacco treatment and control. These are tobacco control and treatment experts from the six WHO regions 6 and four World Bank income levels. 7 Experts were identified from participants in the prior tobacco treatment training survey 5 and participants in other international tobacco control surveys conducted by the research team. 8 , 9 We obtained email addresses for 197 tobacco control experts in 122 countries. We contacted these individuals directly by email and asked if they had a training program in their home country. Individuals that answered yes to the first item were invited to complete our survey about their training program. We also asked experts who reported that training programs were available in their country to provide us with contact information for other individuals involved in training programs in their countries.
Survey Instrument
The survey instrument included content from our previous survey with modifications based on the previous survey responses. 5 We combined this with novel content created by the training experts from the UK National Centre for Smoking Cessation and Training. Response options for each item covered the most common categorical responses from the previous survey and also allowed for open-ended responses.
In addition to the first item which asks respondents if they have training program in their country, our instrument included 28-items about individual training programs ( Supplementary Appendix A ). The instrument asked participants what year their training program started and how many people were trained in the past year. It asked about funding sources including government, professional organizations, educational institutions, nongovernmental organizations, pharmaceutical companies, tobacco companies, and participant fees. It asked participants what categories of people were trained, including healthcare students or workers (physicians, nurses, psychologists, pharmacists, dentists, and respiratory therapists), tobacco treatment and addictions specialists, and community workers (social workers, community health workers, teachers, dieticians, community and religious leaders). It asked about challenges faced by programs (funding, finding trainers, finding students, or finding training materials). It also assessed training methods and content; these results will be reported in a separate paper. The survey was pretested by three Massachusetts General Hospital Tobacco Research and Treatment Center research assistants and 42 National Centre for Smoking Cessation and Training associated trainers.
The survey was professionally translated from English to Spanish and French. Two native-speakers reviewed the translated versions, and any discrepancies in meaning between the original English version and the translated versions were discussed and edited.
Data Collection
Subjects were contacted by email between May and September 2013 and invited to complete the web-based survey. The web-based survey was administered using Lifeguide ( http://lifeguide.ecs.soton.ac.uk/ ). This electronic survey program generates a database of responses that allowed for response rate tracking and preliminary analysis during the survey administration phase. Subjects were contacted every 2 weeks, up to five times, with reminder emails which included a link to the online survey. If subjects had not responded by the second contact, we also attached a word document version of the survey that could be completed and returned as an email attachment. No remuneration was provided to subjects. Consent to participate was implied by response to the survey.
Response Rate
We calculated the response rate by country and by individual contact. The country response rate was calculated as the number of countries who responded divided by the number of countries contacted. We excluded countries from the denominator if our only contact email was returned as not deliverable. Some tobacco control experts reported that they were not involved in training in their country and we excluded countries if our only contact email reported they were not involved in training. Individual response rate was calculated as the number of individuals who responded divided by the number of individuals contacted, including our original contacts plus any additional contacts provided by other respondents, excluding contacts with invalid emails or contacts who reported no involvement in training.
Data Analysis
We calculated how many countries reported training programs among those countries with one or more expert respondent. We conducted the remainder of the analysis at the individual program level. We calculated descriptive statistics of program capacity, years in operation, funding sources, participants, and challenges. We report percentages for categorical responses and either means and standard deviations or median values and interquartile ranges (IQRs) for continuous responses depending on normality of the distribution. We compared these characteristics across income levels (high, upper-middle [UM], lower-middle [LM], and low-income) using the Cochran–Armitage test for trends by four income levels, and the Kruskal–Wallis chi-square test for comparison of continuous variables across income levels. We also compared individual program characteristics by region and by a dichotomous income classification (LMIC vs. high-income) using Fisher’s exact tests. All analyses were performed using SAS version 9.3 (Cary, NC).
Results
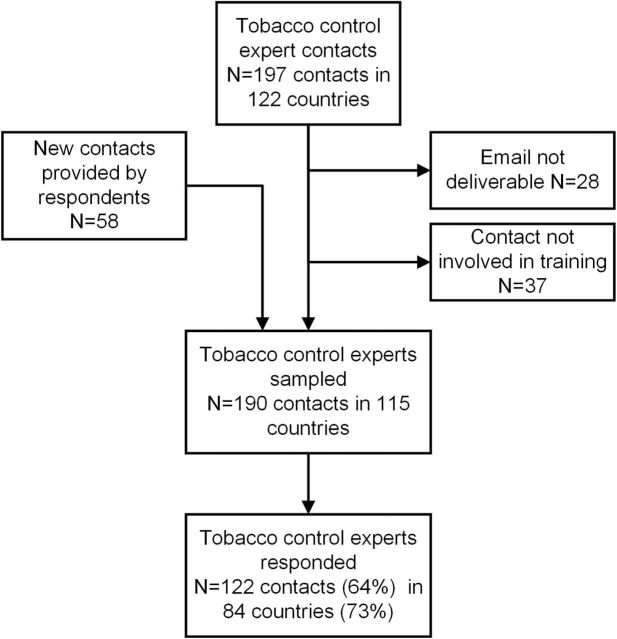
After excluding invalid emails and ineligible contacts (ie, those not involved in training programs) and adding new contacts provided by respondents ( Figure 1 ), our response rate denominators were 190 contacts in 115 countries. We received 122 responses from individual contacts (64%), and responses from 84 of 115 countries (73%). Neither the individual participant response rate nor country response rates differed significantly by income level or region. Of 122 individual respondents, 91% ( N = 111) responded in English, 6% ( N = 7) in French, and 3% ( N = 4) in Spanish. Respondents reporting on a training program were asked to list all of their roles in the training program. Forty-eight percent ( N = 50) listed multiple roles. Reported roles included trainers (52%, N = 54), program managers (42%, N = 44), researchers (32%, N = 33), administrators (20%, N = 21), and funders (5%, N = 5).
Figure 1.
Survey sample.
Country Training Program Frequency
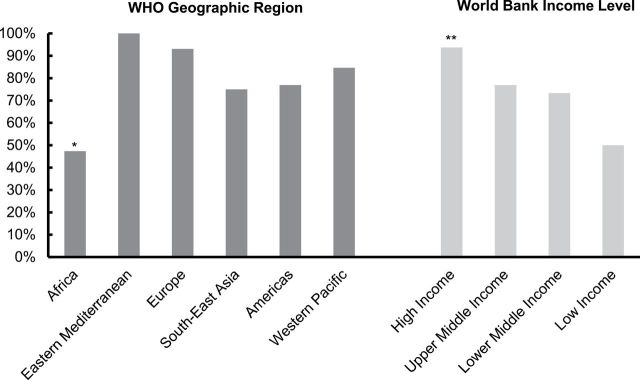
Overall, 104 experts from 66 countries (79% of 84 countries) reported on 104 individual training programs in their country ( Table 1 ) while respondents from the remaining 18 countries (18/84 countries, 21%) reported having no training program. By income level, the proportion of countries with at least one training program ranged from 94% among high-income countries to 50% among low-income countries (Cochran–Armitage trend test = 3.2, P = .002; Figure 2 ). The number of training programs also varied by region (Fisher’s exact test P = .003), with the fewest tobacco treatment training programs reported in the African region countries (44%).
Table 1.
Tobacco Control and Training Expert Sample
| Countries sent surveys | Countries responding | Program prevalence | Current programs | |
|---|---|---|---|---|
| N | N (% response) | N (% countries with ≥1 current program) | N | |
| All | 115 | 84 (73) | 66 (79) | 104 |
| World Bank income level | ||||
| High | 40 | 32 (80) | 30 (94) | 55 |
| UM | 33 | 25 (76) | 19 (76) | 30 |
| LM | 26 | 15 (58) | 11 (73) | 11 |
| Low | 16 | 12 (75) | 6 (50) | 8 |
| WHO geographic region | ||||
| Africa | 28 | 18 (64) | 8 (44) | 12 |
| Americas | 19 | 13 (68) | 10 (77) | 19 |
| Eastern Mediterranean | 13 | 7 (54) | 7 (100) | 9 |
| Europe | 36 | 29 (81) | 27 (93) | 45 |
| South-East Asia | 5 | 4 (80) | 3 (75) | 4 |
| Western Pacific | 14 | 13 (93) | 11 (85) | 15 |
UM = upper middle; LM = lower middle; WHO = World Health Organization.
Figure 2.
Percent of countries with training program by region and income level. *Fewer programs reported in Africa versus other regions (Fishers exact test P = .005); **Fewer programs reported in lower income countries (Cochran–Armitage trend = 3.2, P = .002).
Years of Operation and Volume
The 104 individual training programs described by respondents were reported to be in operation from less than 1 year to as long as 41 years, with a median of 8 years (IQR: 3–13 years). Programs reported they trained a median of 110 students per program (IQR: 30–250 students) in the last year. Programs’ years of operation and capacity did not differ by region or across country income levels. However, when dichotomized, programs in LMICs were less established than programs in high-income countries (high-income median 11 years [IQR: 4–13] vs. LMIC median 5 years [IQR: 3–11], Kruskal–Wallis χ 2 = 5.2, P = .02). The number of training programs appeared to be increasing, particularly with new training programs reported in LMICs ( Supplementary Appendix B ).
Program Funding
Government was the most commonly reported funding source (49%, N = 51), with most programs in high-income countries (56%, N = 31) reporting government funds while the minority of programs in lower-middle or low-income countries reported receiving government funds (UM 50% [ N = 15], LM 27% [ N = 3], low 25% [ N = 2], Cochran–Armitage trend test = 2.2, P = .03; Supplementary Appendix C ). Conversely, programs in LMIC were more likely to report funding from nongovernmental organizations (high-income 11% [ n = 6], UM 37% [ N = 11], LM 27% [ N = 3], low 38% [ N = 3], Cochran–Armitage trend test = −2.3, P = .02). One-quarter of all programs (25%, N = 26) reported being at least partially dependent on user fees for funding. Pharmaceutical companies funding was reported by 13 programs (13%). One lower middle-income country reported funds from a tobacco company. The only regional differences in funding were found in reported receipt of funding from educational institutions. No programs in Africa reported funding from educational institutions and only 13% ( N = 2) of Western Pacific programs reported educational funds, compared to 33% ( N = 3) in Eastern Mediterranean, 24% ( N = 11) in Europe, 25% ( N = 1) in Southeast Asia, and 53% ( N = 10) in the Americas (Fisher’s exact test P = .02).
Trainees
In total, programs reported training 22 324 individuals in 2012. Most programs (84%, N = 87) reported training healthcare workers or healthcare students (doctors, nurses, dentists, mid-level clinicians including clinical officers and physicians assistants, pharmacists, psychologists, respiratory therapists, or students of these professions; Table 2 ). Programs in high-income countries were more likely to report training healthcare workers than those in lower income countries (high-income 91% [ N = 50], UM 80% [ N = 24], LM 73% [ N = 8], low 63% [ N = 5], Cochran–Armitage trend test = 2.4, P = .01). Programs in Africa (50%, N = 6) and the Western Pacific (73%, N = 11) were the least likely to report training healthcare workers compared to other regions (89%–100% in other regions, Fisher’s exact test 0.02). Many programs reported training tobacco treatment specialists (33%, N = 34) and addictions specialists (23%, N = 24). A majority of programs (54%, N = 56) reported training individuals outside the healthcare system to deliver tobacco treatment services. Training religious and community leaders was more likely to be reported in Africa (33%, N = 4) and Southeast Asia (25%, N = 1) compared to other regions (0 to 11%, Fisher’s exact test P = .04). Other trainees specified by respondents included public health workers, public health students, midwives, fitness instructors, prison officers, and school-age students.
Table 2.
Types of Individuals Trained and Treatment Modalities by Income Level
| All | High | UM | LM | Low | P a | |
|---|---|---|---|---|---|---|
| N | 104 | 55 | 30 | 11 | 8 | |
| Does your program offer training to? | ||||||
| Tobacco or addictions specialists | ||||||
| Tobacco treatment specialists | 33% | 35% | 33% | 27% | 25% | .52 |
| Addiction specialists | 23% | 22% | 20% | 18% | 50% | .27 |
| Healthcare workers | ||||||
| Physicians | 50% | 51% | 57% | 55% | 13% | .21 |
| Clinical officers/physician assistants b | 28% | 29% | 23% | 45% | 13% | .78 |
| Nurses | 45% | 45% | 50% | 45% | 25% | .48 |
| Psychologists | 37% | 38% | 40% | 18% | 38% | .55 |
| Pharmacists | 32% | 35% | 37% | 18% | 13% | .17 |
| Dentists | 28% | 25% | 40% | 18% | 13% | .61 |
| Respiratory therapists | 17% | 22% | 17% | 9% | 0% | .09 |
| Healthcare students | ||||||
| Medical students | 34% | 40% | 27% | 36% | 13% | .14 |
| Medical residents c | 26% | 25% | 33% | 27% | 0% | .37 |
| Clinical officer/physician assistant students b | 11% | 13% | 3% | 18% | 13% | .99 |
| Nursing students | 18% | 16% | 20% | 27% | 13% | .76 |
| Psychology students | 11% | 7% | 10% | 18% | 25% | .09 |
| Pharmacy students | 12% | 11% | 10% | 27% | 0% | .94 |
| Community members | ||||||
| Social workers/social assistants | 19% | 20% | 17% | 18% | 25% | .92 |
| Community health workers | 17% | 16% | 17% | 18% | 25% | .61 |
| Dieticians | 11% | 16% | 7% | 0% | 0% | .04 |
| Teachers | 16% | 16% | 17% | 9% | 25% | .87 |
| Community or religious leaders | 10% | 9% | 3% | 18% | 25% | .19 |
| Other | 10% | 7% | 10% | 0% | 38% | .09 |
UM = upper middle; LM = lower middle. Categories were not mutually exclusive and respondents could select more than one option.
a Based on Cochrane–Armitage trend test.
b Mid-level clinicians.
c Postgraduate medical trainees.
Challenges
Most programs (54%) reported difficulty with funding ( Supplementary Appendix C ). Some low- and lower middle-income countries also reported difficulty finding trainers (high 9% [ N = 5], UM 17% [ N = 5], LM 36% [ N = 4], low 25% [ N = 2]; Cochran–Armitage trend test = −2.1, P = .03) and programs in low-income countries reported difficulty finding training materials (high 5% [ N = 3], UM 10% [ N = 3], LM 9% [ N = 1], low 38% [ N = 3]; Cochran–Armitage trend test = −2.4, P = .02). Other challenges reported by respondents were establishing a certification process, not having enough capacity to accommodate demand for training, and arranging time off from participants’ normal responsibilities to attend the program.
Discussion
This article reports the findings of an international survey of experts in tobacco control and treatment from 84 countries conducted in 2013. It updates and expands on our 2008 survey of 48 countries. 5 Both surveys aimed to identify the availability of programs to train individuals to deliver tobacco cessation treatment, a key component of the global strategy for tobacco cessation articulated in Article 14 of the FCTC. 5 In 2013, training programs were reported in 79% of countries, with 21% of countries reporting no programs at all. This represents little progress since our 2008 survey. The countries reporting no training programs were mostly LMICs, where 80% of smokers live. 1 This shortage of training programs represents a disparity in availability of training programs by income level and compromises the ability of many LMICs to deliver assistance to help smokers to quit and to meet their obligations to clause 14 of the FCTC. In contrast to programs in high-income countries, those in LMICs reported being newer, more likely to be funded by nongovernmental organizations rather than governments, more likely to report difficulty finding trainers and materials (but not trainees), and less likely to train healthcare workers, which are fewer in number in LMICs. International cooperation, as promoted in the FCTC as a whole and in the Article 14 implementation guidelines, 3 may offer a solution. High-income and middle-income countries should share methods of training the trainers to help those low-income countries challenged to increase their training capacity. Helping countries to obtain training materials may be an issue of insufficient investment of resources in training programs or a need for adaptation of training materials from other countries, or both.
Although the results of the two surveys cannot be directly compared, the overall findings were similar to the 2008 survey where respondents in 77% of countries reported that the country had a training program. At both times, fewer training programs were reported in low-income countries and in Africa; most programs reported training healthcare workers; and funding was the biggest challenge.
Training all healthcare workers to record tobacco use and offer brief advice is a basic, core component for the successful implementation of the Article 14 guidelines. 3 Offering training in tobacco treatment to healthcare workers has demonstrated effectiveness in increasing abstinence rates among patients. 10 , 11 Incorporating training in the delivery of brief advice for tobacco cessation into healthcare worker curricula, and addressing tobacco use among healthcare workers themselves, are crucial steps in developing a national infrastructure for cessation support. 3 Consistent with that strategy and similar to the 2008 survey, we found that most training programs reported training healthcare workers. However, even high-income countries may fall short in terms of adequacy of training for healthcare workers to deliver advice and counseling. 12 A majority of programs also reported offering training to individuals outside of the healthcare system. Training these individuals is a strategy that could help meet unmet demand for cessation services in areas of healthcare worker shortages. 13 , 14 Tobacco cessation has been clearly shown to reduce the burden and mortality of common conditions such as coronary artery disease, chronic obstructive pulmonary disease, and tuberculosis. 15 , 16 Linking provision of tobacco treatment services to the standard treatment algorithms for these conditions can create demand and support for tobacco treatment training programs.
A strength of this study is its relatively large sample of respondents from economically and regionally diverse countries. It also has several important limitations. First, this is not a probability sample as there are no comprehensive global lists of tobacco treatment training programs. We likely overestimate the prevalence of training programs because it may be harder to identify expert contacts in countries with less developed tobacco cessation infrastructure. Second, this is a cross-sectional study. Although we have data from the 2008 survey, the sample changed substantially, with only 22 individual programs responding to both surveys, and we are unable to do a longitudinal analysis to compare changes in the training program prevalence or quality over time. Third, data were self-reported and we were unable to verify the accuracy of the responses. Because we identified some of our respondents from surveys on other tobacco control topics, their depth of knowledge about training programs may be variable depending on the respondent’s role. In a separate paper we present data about training program content, but cannot attest to actual quality or impact of training programs surveyed. Finally, we made multiple statistical comparisons for the survey items across geographical regions and income levels and this large number of tests may produce type I errors.
In summary, full implementation of the FCTC Article 14 guidelines will require infrastructure that can support and sustain training as well as treatment delivery. Unfortunately our current survey results suggest that training for tobacco cessation treatment is largely unchanged since 2008. Training needs include working to ensure that assessment of tobacco use and delivery of brief advice is included in all healthcare worker educational programs, extending training beyond healthcare workers to meet the needs of areas with limited healthcare worker supply, and securing stable infrastructure and funding for these programs. Establishing sustainable funding for tobacco cessation, including training from government sources such as tobacco tax revenue should be a priority. Raising the priority of tobacco treatment and training will be necessary to achieve full implementation of Article 14 guidelines. We hope that the FCTC Cooperation Centre, newly established in Uruguay, will support countries in implementing Article 14 and in promoting cooperation between countries, a theme repeated many times in the FCTC itself and in the Article 14 guidelines.
Funding
This work was supported by the National Centre for Smoking Cessation and Training and Cancer Research UK, by the Health Resources and Services Administration (grant number T32HP12706-03-00), and by the National Institutes of Health, National Cancer Institute (grant number 5 R25 CA 0571120).
Declaration of Interests
None declared.
Supplementary Material
Acknowledgments
We acknowledge the contributions of our French and Spanish translation reviewers, Dr Carol Clair and Dr Joseph Joyner, and the translational services of Kwintessential. We are grateful for the contributions of our survey respondents. GRK contributed to survey design, led data collection, led data analysis, led the manuscript writing and is responsible for the overall content. NAR contributed to survey design, data collection, and data analysis. MR contributed to survey design, data collection, and data analysis. AM contributed to survey design and data analysis. RM contributed to survey design and data analysis. HP-A contributed to study design and data analysis. AB contributed to study design. AM contributed to survey design, data collection, and data analysis. All authors contributed to the writing and critical revision of the manuscript and approved the final article. Ethical approval: This research was deemed exempt from informed consent by the Partners Healthcare Institutional Review Board in Boston, Massachusetts, United States.
References
- 1. World Health Organization . WHO Report on the Global Tobacco Epidemic, 2011: Warning about the dangers of tobacco. Secondary WHO Report on the Global Tobacco Epidemic, 2011: Warning about the dangers of tobacco 2011 . 2011. http://whqlibdoc.who.int/publications/2011/9789240687813_eng.pdf . Accessed July 5, 2015 .
- 2. Asma S, Song Y, Cohen J, et al. CDC Grand Rounds: global tobacco control . MMWR Morb Mortal Wkly Rep . 2014. ; 63 ( 13 ): 277 – 280 . [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization . FCTC/COP4(8): Guidelines for Implementation of Article 14 of the WHO Framework Convention on Tobacco Control (Demand Reduction Measures Concerning Tobacco Dependence and Cessation). Secondary FCTC/COP4(8): Guidelines for Implementation of Article 14 of the WHO Framework Convention on Tobacco Control (Demand Reduction Measures Concerning Tobacco Dependence and Cessation) 2010 . 2010. www.who.int/fctc/protocol/guidelines/adopted/article_14/en/index.html . Accessed July 5, 2015 .
- 4. Centers for Disease Control and Prevention . Tobacco use and cessation counseling--global health professionals survey pilot study, 10 countries, 2005 . MMWR Morb Mortal Wkly Rep . 2005. ; 54 ( 20 ): 505 – 509 . [PubMed] [Google Scholar]
- 5. Rigotti NA, Bitton A, Richards AE, Reyen M, Wassum K, Raw M . An international survey of training programs for treating tobacco dependence . Addiction . 2009. ; 104 ( 2 ): 288 – 296 . doi: 10.1111/j.1360-0443.2008.02442.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization . About WHO: WHO regional offices . 2014. . http://who.int/countryfocus/country_offices/memberstatesbyregion/en/print.html . Accessed January 18, 2015 .
- 7. World Bank . About Data: How we Classify Countries . 2014. . http://data.worldbank.org.ezp-prod1.hul.harvard.edu/data-catalog/world-development-indicators?display=graph . Accessed January 18, 2015 .
- 8. Piné-Abata H, McNeill A, Murray R, Bitton A, Rigotti N, Raw M . A survey of tobacco dependence treatment services in 121 countries . Addiction . 2013. ; 108 ( 8 ): 1476 – 1484 . doi: 10.1111/add.12172 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pine-Abata H, McNeill A, Raw M, et al. A survey of tobacco dependence treatment guidelines in 121 countries . Addiction . 2013. ; 108 ( 8 ): 1470 – 1475 . doi: 10.1111/add.12158 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Olano-Espinosa E, Matilla-Pardo B, Minué C, Antón E, Gómez-Gascón T, Ayesta FJ . Effectiveness of a health professional training program for treatment of tobacco addiction . Nicotine Tob Res . 2013. ; 15 ( 10 ): 1682 – 1689 . doi: 10.1093/ntr/ntt040 . [DOI] [PubMed] [Google Scholar]
- 11. Carson KV, Verbiest ME, Crone MR, et al. Training health professionals in smoking cessation . Cochrane Database Syst Rev . 2012. ; 5 : CD000214 . doi: 10.1002/14651858.CD000214.pub2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Raupach T, Al-Harbi G, McNeill A, Bobak A, McEwen A . Smoking cessation education and training in U.K. medical schools: a national survey . Nicotine Tob Res . 2015. ; 17 ( 3 ): 372 – 375 . doi: 10.1093/ntr/ntu199 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Centers for Disease Control and Prevention . Influence of religious leaders on smoking cessation in a rural population--Thailand, 1991 . MMWR Morb Mortal Wkly Rep . 1993. ; 42 ( 19 ): 367 – 369 . [PubMed] [Google Scholar]
- 14. Bittencourt L, Scarinci IC . Is there a role for community health workers in tobacco cessation programs? Perceptions of administrators and health care professionals . Nicotine Tob Res . 2014. ; 16 ( 5 ): 626 – 631 . doi: 10.1093/ntr/ntt217 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Basu S, Glantz S, Bitton A, et al. The effect of tobacco control measures during a period of rising cardiovascular disease risk in India: a mathematical model of myocardial infarction and stroke . PLoS Med . 2013. ; 10 ( 7 ): e1001480 . doi: 10.1371/journal.pmed.1001480 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Basu S, Stuckler D, Bitton A, Glantz SA . Projected effects of tobacco smoking on worldwide tuberculosis control: mathematical modelling analysis . BMJ . 2011. ; 343 : d5506 . doi: 10.1136/bmj.d5506 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.