Abstract
Aims
To conduct a systematic review and meta‐analysis of studies in order to estimate the effect of US medical marijuana laws (MMLs) on past‐month marijuana use prevalence among adolescents.
Methods
A total of 2999 papers from 17 literature sources were screened systematically. Eleven studies, developed from four ongoing large national surveys, were meta‐analyzed. Estimates of MML effects on any past‐month marijuana use prevalence from included studies were obtained from comparisons of pre–post MML changes in MML states to changes in non‐MML states over comparable time‐periods. These estimates were standardized and entered into a meta‐analysis model with fixed‐effects for each study. Heterogeneity among the study estimates by national data survey was tested with an omnibus F‐test. Estimates of effects on additional marijuana outcomes, of MML provisions (e.g. dispensaries) and among demographic subgroups were abstracted and summarized. Key methodological and modeling characteristics were also described. Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines were followed.
Results
None of the 11 studies found significant estimates of pre–post MML changes compared with contemporaneous changes in non‐MML states for marijuana use prevalence among adolescents. The meta‐analysis yielded a non‐significant pooled estimate (standardized mean difference) of −0.003 (95% confidence interval = −0.012, +0.007). Four studies compared MML with non‐MML states on pre‐MML differences and all found higher rates of past‐month marijuana use in MML states pre‐MML passage. Additional tests of specific MML provisions, of MML effects on additional marijuana outcomes and among subgroups generally yielded non‐significant results, although limited heterogeneity may warrant further study.
Conclusions
Synthesis of the current evidence does not support the hypothesis that US medical marijuana laws (MMLs) until 2014 have led to increases in adolescent marijuana use prevalence. Limited heterogeneity exists among estimates of effects of MMLs on other patterns of marijuana use, of effects within particular population subgroups and of effects of specific MML provisions.
Keywords: Adolescent, epidemiology, marijuana, meta‐analysis, policy, systematic review
Introduction
Marijuana is one of the most commonly used psychoactive substances in the world 1. Although some individuals may use marijuana without serious consequences 2, 3, use is associated with impaired functioning 2, 3, 4, 5, 6, vehicular accidents 7, 8, 9, 10, psychiatric symptoms 11, 12, 13 and addiction 14, 15, 16. Marijuana use often begins in adolescence 17, 18, 19, when heavy use is associated particularly with poor outcomes 16, 17, 20, 21, 22, including altered brain development 23, 24 and decreased educational attainment 25, 26, 27.
More than 30 years of evidence from annual surveys of students show the importance of social context to adolescent marijuana use 28. State substance use laws constitute one modifiable component of social context that could influence adolescent substance use through substance availability, social norms and risk perceptions. For example, state minimum legal drinking age laws demonstrate how state‐level policies can affect various outcomes, including crime and suicidal behaviour 29, 30, 31, adolescent and adult drinking 32, 33 and both alcohol and drug use disorders 34.
As of November 2016, state‐level referendum and legislation resulted in 28 US states with policies that legalized marijuana use for medical purposes. Marijuana components may benefit some individuals with selected medical conditions 35. However, since the first medical marijuana law (MML) was enacted in California in 1996, public debate has focused on the potential for MMLs to increase recreational use of marijuana in adolescents 36, 37, 38, 39, 40. Others have speculated that secular trends in marijuana use are not affected by MMLs or that its medicalization could reduce its recreational appeal to adolescents 41, 42, 43.
Empirical evidence can inform this debate. Although existing evidence is observational due to the uncontrolled and self‐selecting process of state marijuana policy implementation, we can learn about the association between MML passage and changes in marijuana use by comparing trends in marijuana use in MML states to contemporaneous trends in non‐MML states. Given how rapidly US state marijuana laws are changing, a comprehensive review of the empirical literature is needed to provide a foundation for further research in this high‐priority area 44. Therefore, we searched, reviewed and synthesized systematically the results of studies evaluating the effects of MML passage on adolescent marijuana use. Primarily, we meta‐analyze estimates of the association between MML passage and changes in past‐month marijuana use among adolescents. Secondly, motivated by scholars who urge consideration of specific MML provisions (e.g. marijuana dispensaries) 45, 46, we review results examining these provisions. Thirdly, we summarize effects of MMLs on additional outcomes (e.g. frequent marijuana use) and effects among particular subgroups (e.g. female adolescents). Fourthly, we summarize key strengths and limitations of this literature, and provide the basis of a strategic plan for future research.
Methods
This review follows the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) statement guidelines 47.
Literature search
Using a systematic search, we queried 15 on‐line literature databases (Box 1). We additionally searched the first 300 references in Google Scholar (sorted by relevance), and ensured that pre‐selected empirical law journals were indexed in the literature databases. The search algorithm (Box 2) was applied to the indexed text of titles and abstracts. The search was conducted in January and was repeated in December 2016.
Box1. Literature sources.
Electronic Literature Databases
PubMed, PsychInfo, EBSCOhost (which included: Academic Search Complete, E‐Journals, EconLit, Education Research Complete, Education Full Text, ERIC, National Criminal Justice Reference Service Abstracts, Social Sciences Full Text, Social Work Abstracts, and SocINDEX with Full Text), Social Sciences Research Network, RAND Documents, and ProQuest Dissertations & Theses Global.
Google Scholar
First 300 references (sorted by relevance).
Empirical law journals
Journal of Empirical Legal Studies (SocINDEX), Journal of Law & Economics (Social Sciences Full Text), Law & Society Review (Social Sciences Full Text), Law & Social Inquiry (SocINDEX), Journal of Legal Studies (E‐Journals).
Box 2. Search algorithm.
(medic*)
AND
(marijuana OR cannabis)
AND
(legal* OR law* OR polic* OR legis*)
AND
(youth* OR young* OR underage* OR adolesc* OR teen* OR child* OR school* OR kid* OR juvenile*)
Note: Asterisks (*) indicate ‘wildcard’ operators, whereby all search terms that begin with the text string before the asterisk were included in the algorithm (e.g. medic* corresponds to ‘medical’, ‘medicinal’, ‘medicalized’, etc.)
Identifying information for returned papers was entered into a database. Duplicate entries were removed. Primary exclusion criteria (Box 3) were applied to titles, abstracts and the full texts. Remaining papers were included in the final review and the screening process was repeated for the references of these papers. Secondary exclusion criteria (Box 4) determined the meta‐analytical sample. A Master's‐level research assistant (A.L.) conducted the initial screening of all titles, supervised by the first (A.S.) and senior (D.H.) authors. This research assistant (A.L.) and the senior author (D.H.) screened all abstracts independently. Only abstracts excluded by both reviewers were removed from the review. The first (A.S.) and senior author (D.H.) screened full texts independently. Agreement between two authors was required for exclusion of full texts. Disagreements were resolved by short discussion between these reviewers.
Box 3. Primary study exclusion criteria—systematic review.
1. Anything other than an empirical research report
2. Not concerned with the effects of medical marijuana laws on marijuana use
3. Focused on a population outside of the United States
4. No results on individuals under the age of 20
5. Only results for children under the age of 12
6. Not published in English
7. Did not minimally present results of statistical tests of data spanning multiple time‐points from both states that did and did not pass medical marijuana laws.
Box 4. Secondary study exclusion criteria—meta‐analysis.
1. Not published in a peer‐reviewed journal
2. Analyses included only a single state
3. Did not estimate effects of MMLs overall (e.g. specific MML characteristics only or no overall pre‐ versus post‐test)
4. Did not appropriately apply difference‐in‐difference methodology.
Data abstraction
A data abstraction tool [developed by the first (A.S.), second (M.W.) and senior authors (D.H.)] captured systematically the key results and specifications of included studies. Two pre‐doctoral fellows (D.F., E.G.) and the first author (A.S.) each applied the tool to one‐third of the papers. Authors of studies were contacted if results or specifications of interest were not reported.
The primary study outcome abstracted for meta‐analysis was the pre–post MML‐passage effect on past‐month marijuana use among adolescents as measured by either a prevalence difference or odds ratio (OR), where the reference is contemporaneous change in non‐MML states. Although not meta‐analyzed, pre‐law differences in prevalence of past‐month marijuana use between states that did and did not pass MMLs were also abstracted, when available, as were three types of specific estimated effects: (1) additional marijuana outcomes (e.g. frequent use); (2) specific MML provisions (e.g. dispensaries) and specific states’ laws (e.g. Montana's MML); and (3) subgroup analyses (e.g. among female adolescents).
Meta‐analysis
Primary outcomes from each study were standardized for meta‐analysis. Prevalence differences were converted to Cohen's h 48 and ORs to Cohen's d 49. An overall estimate and 95% confidence interval (CI) was obtained from a meta‐analysis model with fixed‐effects for each study using the metafor package in R 50. Heterogeneity in the study estimates by data source was tested with an omnibus F‐test. A sensitivity analysis additionally included estimates from non‐peer‐reviewed papers.
Results
Results of the search
We retrieved 1668 papers from electronic literature databases and 1331 from references of reviewed papers (n = 2999) (Fig. 1). After removing 1055 duplicates, 1944 unique papers were included at the initial screening stage. The texts of 45 papers were screened in full. Twenty‐one papers passed primary exclusion criteria.
Figure 1.
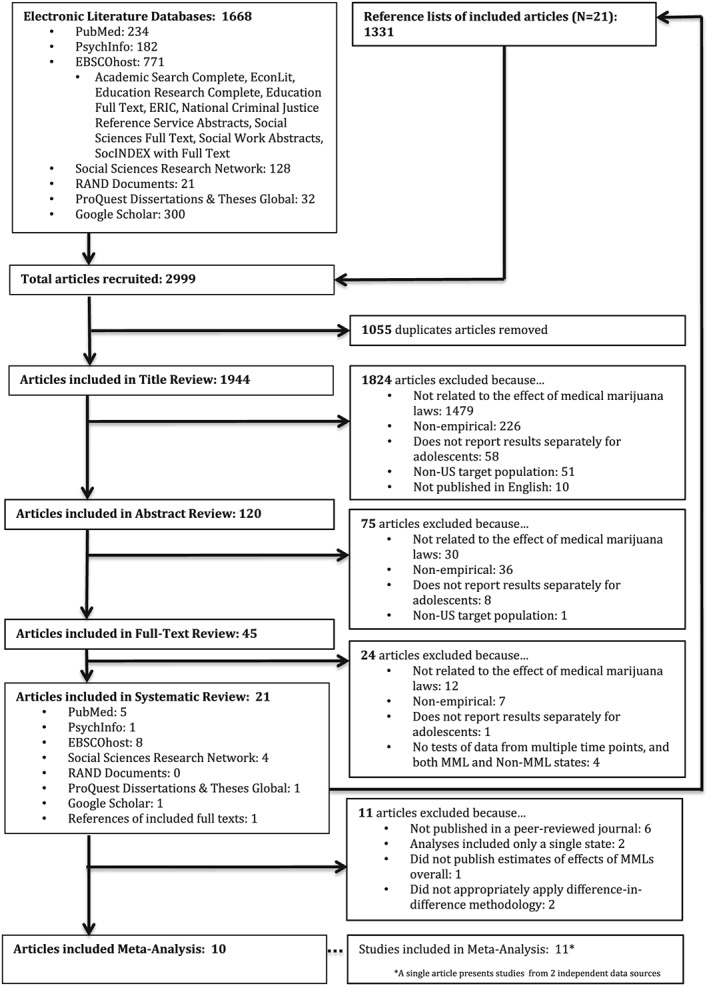
Systematic search flow‐chart
Eleven studies presented in 10 papers passed review for inclusion in the meta‐analysis (Table 1) (one paper included two studies from independent data sources). Characteristics of studies excluded for secondary reasons are shown in Supporting information, Tables S1 and S2.
Table 1.
Primary analyses results and basic analyses characteristics included in the meta‐analysis.
| Studies | Main sample size | Ages | Pre–post MML change in past‐month marijuana use within MML states | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Study no. | Paper [reference number] | Data source | No. of participants | No. of MML states included with pre–post data | MML states included with pre–post data | Years | Range | OR or PD (95% CI) | Standardized effect sizea (95% CI) |
| 1 | Hasin et al., 2015 63 | MTF | 1 098 270 | 21 | AZ, CA, CO, CT, DE, IL, ME, MD, MA, MI, MN, MT, NV, NH, NJ, NM, NY, OR, RI, VT, WA | 1991–2014 | 13–18b | OR = 0.92 (0.82, 1.04) | −0.046 (−0.109, +0.018) |
| 2 | Keyes et al., 2016 64 | 973 089 | 21 | AZ, CA, CO, CT, DE, IL, ME, MD, MA, MI, MN, MT, NV, NH, NJ, NM, NY, OR, RI, VT, WA | 1992–2014 | 13–18b | OR = 0.95 (0.86, 1.04) | −0.028 (−0.083, +0.027) | |
| 3 | Anderson et al., 2015 53 | NLSY | 40 986c | 6 | CO, ME, MD, NV, OR, WA | 1997–2003 | 12–19 | PD = −0.4 (−4.71, +3.91) | −0.011 (−0.127, +0.104) |
| 4 | Pacula et al., 2015 46 | 46 375c | 7 | CO, ME, MD, MT, NV, OR, WA, VT | 1997–2005 | 12–20 | PD = +0.5 (−1.46, +2.46) | +0.014 (−0.039, +0.067) | |
| 5 | Wen et al., 2015 69 | NSDUH | ~269 500 | 9 + DC | AZ, CT, DE, D.C., MI, MT, NM, NJ, RI, VT | 2004–2012 | 12–20 | PD = −0.43 (−1.37, +0.51) | −0.015 (−0.046, +0.017) |
| 6 | Martins et al., 2016 65 | ~175 000d | 10 | AZ, CT, DE, IL, MA, MI, NH, NJ, NM, RI | 2004–2013 | 12–17 | OR = 1.03 (0.97, 1.09) | +0.016 (−0.017, +0.049) | |
| 7 | Wall et al., 2016 60 | 250e | 8 | AZ, DE, MI, MT, NJ, NM, RI, VT | 2002–2011 | 12–18 | PD = +0.43 (−0.12, +0.98) | +0.014(−0.004, +0.032) | |
| 8 | Harper et al., 2012 94 | 357e | 6 + DC | D.C., MI, MT, NM, MI, RI, VT | 2002–2009 | 12–17 | PD = −0.53 (−1.02, +0.03) | −0.018 (−0.037, +0.001) | |
| 9 | Anderson et al., 2015 53 | YRBS | 846 928 | 16 + DC | AK, AZ, CA, CO, DE, D.C., HI, ME, MI, MT, NV, NJ, NM, OR, RI, VT, WA | 1993–2011 | ~16f | PD = ‐0.7 (−2.86, +1.46) | −0.018 (−0.071, +0.036) |
| 10 | Choo et al., 2014 52 | NAg | 5 | ME, MT, NV, RI, VT | 1991–2011 | ~16f | PD = +0.7 (‐0.7, +2.0) | 0.017 (−0.014, +0.049) | |
| 11 | Johnson et al., 2017 73 | 715 014 | 12 | AK, AZ, CO, DE, ME, MI, MT, NV, NJ, NM, RI, VT | 1991–2011 | ~16f | OR = 0.93 (0.86, 0.99) | −0.040 (−0.083, +0.003) | |
CI = confidence interval; OR = odds ratio; PD = prevalence difference, in percentage points; MTF = Monitoring the Future Study; NLSY = National Longitudinal Survey of Youth; NSDUH = National Survey on Drug Use and Health; YRBS = Youth Risk Behavior Survey.
ORs are standardized to Cohen's d. Prevalence differences are standardized using the arcsine transformation to yield Cohen's h as described in Cohen (2008) 48. Baseline prevalences necessary for computations of Cohen's h are taken to be 1%, 10 and 20% for NLSY, NSDUH and YRBS, respectively, based on approximate unadjusted overall prevalences of past‐month marijuana use reported in the manuscripts included in this review. Differences in these prevalences reflect differences in the age distributions between data sets.
Some respondents are older than 18 or younger than 13 in the MTF sample, but ages were censored for these groups in analytical files.
Person‐years.
Sample n not provided in manuscript. Approximate n is provided based on approximate sample sizes of included states [17 500*(all 50 states)*10 years = 175 000].
Analyses performed on state‐wide aggregated data.
Age range of overall sample not reported. Mean age estimated based on reported mean age of sample in MML (16.0) and non‐MML states (16.2) within the national YRBS sample.
Unweighted sample size not reported in manuscript.
Independent reviewers agreed on the classification of 87.5% of the abstracts (kappa = 0.71, 95% CI = 0.58–0.85) and 97.8% of the full texts (kappa = 0.96, 95% CI = 0.87–1.00).
Three authors of included studies were contacted for additional information (see Acknowledgements) 51, 52, 53.
Characteristics of studies included in meta‐analysis (Table 1)
Data from the 11 studies came from four large national surveys: Monitoring the Future (MTF, n = 2) 54; National Longitudinal Survey of Youth (NLSY, n = 2) 55; National Survey on Drug Use and Health (NSDUH, n = 4) 56; and the Youth Risk Behavior Survey (YRBS, n = 3) 57. Except for the NLSY, these surveys employed a repeated cross‐sectional design with an average of at least several hundred adolescents sampled in each US state. The NLSY recruited participants in a single year (1997) and followed participants annually. Each measured participants annually, with the exception of the biennial YRBS.
Studies from the same national survey differed in years analyzed and thus the set of states with data before and after MML passage also differed (Fig. 2). Studies based on MTF data encompassed the widest range of years (1991 or 1992–2014) and thus overlapped with the passage of the largest number of MMLs (21). The MTF and the YRBS also uniquely include data prior to the first MML in 1996. In contrast, data from four of 11 studies exclude years prior to 2002 and thus exclude data collected prior to the earliest‐passing MMLs (e.g. California, Oregon, Washington and Colorado). An additional two YRBS studies did not include these Pacific Coast states. Although 28 states had MMLs as of November 2016, only a median of nine MML states (range = 5–21) contributed to overall estimates of MML effects among meta‐analyzed studies. Furthermore, only the NSDUH and the state‐specific YRBS (as opposed to the national YRBS 53) were designed to provide state‐representative data.
Figure 2.
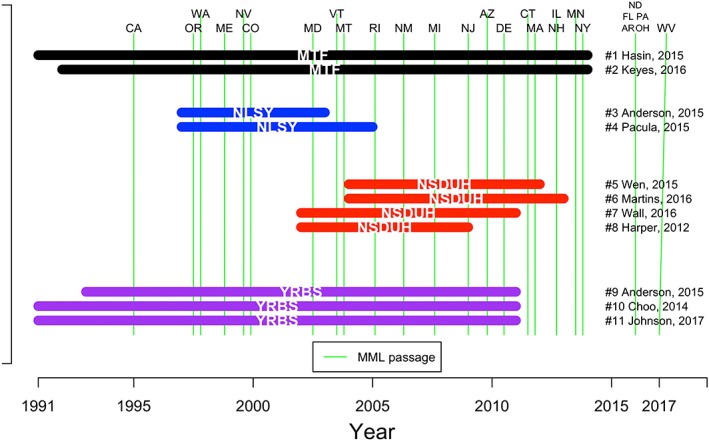
Years of coverage, and overlap with passage of state medical marijuana laws (MMLs), of studies included in meta‐analysis. MTF = Monitoring the Future Study; NLSY = National Longitudinal Survey of Youth; NSDUH = National Survey on Drug Use and Health; YRBS = Youth Risk Behavior Survey. [Colour figure can be viewed at http://wileyonlinelibrary.com]
Statistical modeling procedures employed in the meta‐analyzed studies (Supporting information, Table S3)
All 11 studies estimated the effect of MML passage using a difference‐in‐difference (DID) approach where differences in marijuana use from pre‐ to post‐MML passage were compared to contemporaneous differences in non‐MML states 58, 59. The analytical strategies used within each study were statistically appropriate and expected to yield valid findings from the respective data. Nevertheless, there were some differences in the model specifications and assessment of assumptions (Supporting information, Table S3).
To test the effects of a policy at the state level, adjustments for background differences between states that pass MML and those that do not must be made. For this, statistical models utilize one of two approaches: (1) they include state fixed‐effects (where state is treated as a categorical predictor with a dummy variable for each state); or (2) they include a dichotomous variable indicating whether a state ever passed a law within the study period. Both approaches serve to offset the influence of time‐invariant pre‐law differences between MML and non‐MML states 60. The categorical state predictor method is more rigorous, in that each MML state uses its own pre‐law period as a control, but should only be employed when adequate sample sizes are available across time within every state. When these conditions are not met, a dichotomous grouped MML state predictor can be used. This latter method should additionally model states as random‐effects so that sparsely sampled states can borrow information from similar states that are sampled adequately 61. Seven of the 11 studies (75%) treated each state as a categorical predictor, and the remaining used a dichotomous indicator of whether or not a state ever passed a law.
As MMLs were passed at different points in time, statistical models must also adjust for secular trends in marijuana use. Eight (73%) used a categorical indicator for year, and three used a smooth continuous function of years via a cubic spline.
The unit of analysis in two of the 11 studies (both from NSDUH) was an aggregated state summary variable. The remaining studies analyzed individual‐level data. For the purpose of testing overall state policy effects the use of aggregated data is adequate, while individual‐level data allow for further control of effects accounting for individual characteristics (e.g. demographics) that may also contribute to use. Nine (82%) analyses controlled for individual‐level variables and seven (64%) controlled for state‐level variables.
Crucial for reproducibility 62, three of 11 studies (27%) provided statistical modeling code 63, 64, 65.
Finally, consistent time trends between states with and without the policy, prior to policy enactment (i.e. ‘parallel paths’), can be checked or modeled to help support the validity of the DID approach 66. Only four (36%) studies assessed the ‘parallel‐paths’ assumption. Due to limitations of the data used in these analyses, assessment was performed in a variety of ways, including visual inspection of pre‐policy trends, tests of policy ‘lead’ indicator variables and inclusion of state specific linear trends 67. None found that pre‐policy trend differences were a significant factor.
Meta‐analysis
Pre–post MML change in past‐month marijuana use prevalence among adolescents in MML states (Table 1, Fig. 3)
Figure 3.
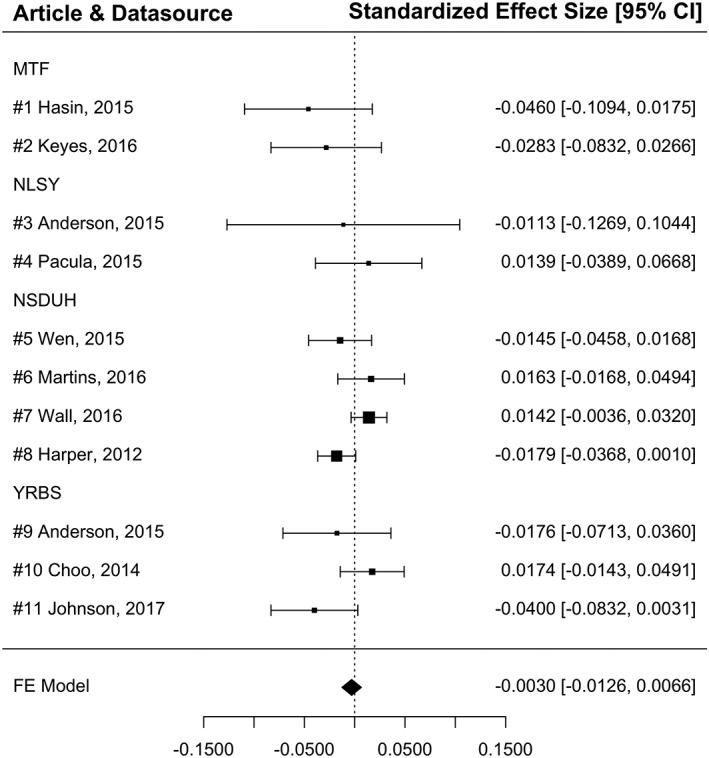
Fixed‐effects meta‐analysis: pre–post medical marijuana law (MML) change in past‐month marijuana prevalence within MML states. MTF = Monitoring the Future Study; NLSY = National Longitudinal Survey of Youth; NSDUH=National Survey on Drug Use and Health; YRBS = Youth Risk Behavior Survey; FE = fixed‐effects. FE model: , where corresponds to the final fixed‐effects estimate, θi corresponds to the i th study's standardized estimate and wi corresponds to the inverse of the variance of the i th study's standardized estimate
Of the 11 studies included in the meta‐analysis, none found significant (P < 0.05) changes in past‐month marijuana use following MML passage within MML states (compared to comparable changes in non‐MML states). A fixed‐effect meta‐analysis of these results yielded a standardized mean difference of −0.003 (95% CI = −0.013, +0.007). In a separate model, data source (i.e. MTF, NLSY, NSDUH, YRBS) was not found to impact study effect size significantly (P = 0.46). A sensitivity analysis that additionally included estimates from the five unpublished studies yielded nearly identical results (standardized mean difference [95% CI = −0.004 (−0.012, +0.005)]).
Pre‐law difference in past‐month marijuana prevalence between MML and non‐MML states (Table 2)
Table 2.
Estimates of pre‐law differences between medical marijuana law (MML) and non‐MML states from studies included in the meta‐analysis.
| Study | Data source | Pre‐law difference in past‐month marijuana use between MML and non‐MML states | |
|---|---|---|---|
| Study no. | Paper [reference number] | OR or PD (95% CI) | |
| 1 | Hasin et al., 2015 63 | MTF | OR = 1.27 (1.07, 1.57) |
| 2 | Keyes et al., 2016 64 | OR = 1 .21 (1.06, 1.39) | |
| 6 | Martins et al., 2016 65 | NSDUH | OR = 1.61 (1.41, 1.84) |
| 7 | Wall et al., 2016 60 | PD = +1.65 (0.86, 2.41) | |
CI = confidence interval; OR = odds ratio; PD = prevalence difference in percentage points; MTF = Monitoring the Future Study; NSDUH = National Survey on Drug Use and Health.
Estimates of pre‐law differences in past‐month marijuana use between MML and non‐MML states indicate the extent of important pre‐existing differences between MML and non‐MML states. These estimates were reported by four of the 11 studies included in the meta‐analysis and all found a significantly higher pre‐law prevalence of past‐month marijuana use among adolescents in MML states compared to non‐MML states.
Specific effects and robustness checks
The following sections summarize tests of additional marijuana outcomes, of individual state MMLs, of particular MML provisions and of tests among population subgroups. Often a single report assessed a specific effect multiple times under modified conditions (e.g. tested both the presence of active dispensaries and the presence of for‐profit dispensaries). Simple counts of significant and non‐significant results should therefore be interpreted with caution.
Additional marijuana outcomes (Table 3)
Table 3.
Additional marijuana outcomes from all 21 papers included in the systematic review.
| Study no. | Paper [reference number] | Data source | Pre–post MML change within MML states | |
|---|---|---|---|---|
| (95% CI) | ||||
| Initiation (i.e. past‐year use among ‘at‐risk sample‘) | ||||
| 15 | Wen et al., 2015 69 | NSDUH | PD = +0.32 (+0.01, +0.63) | |
| Frequency | ||||
| 20+ days (past month) | ||||
| 4 | Pacula et al., 2015 46 | NLSY | PD = +0.9 (–0.47, +2.27) | |
| 5 | Wen et al., 2015 69 | NSDUH | PD = −0.25 (−0.58, +0.08) | |
| 11 | Johnson et al., 2017 73 | YRBS | OR = 1 (0.89, 1.13) | |
| 17 | Pacula et al., 2013 70 | NLSY | PD = +0.3 (−1.07, +1.67) | |
| 10+ days (past month) | ||||
| 3 | Anderson et al., 2015 53 | NLSY | PD = 0.8 (–1.94, +3.54) | |
| 3 | Anderson et al., 2015 53 | YRBS | PD = −0.4 (−1.58, +0.78) | |
| Days/occasions used (past month) | ||||
| 1 | Hasin et al., 2015 63 | MTF | OR = 0.93 (0.82, 1.06) | |
| 4 | Pacula et al., 2015 46 | NLSY | Δ‐days = +0.46 (+0.05, +0.88) | |
| Days used (past month) among users | ||||
| 5 | Wen et al., 2015 69 | NSDUH | %Δ‐days = –0.28 (−1.16, +0.60) | |
| 18 | Choi 2014 68 | NSDUH | Δ‐days = +1.82 (+1.18, +2.46) | |
| Past year use | ||||
| 1 | Hasin et al., 2015 63 | MTF | OR = 0.93 (0.80, 1.06) | |
| 18 | Choi, 2014 68 | NSDUH | PD = +0.43 (−1.51, +2.37) | |
| Past 30‐day use at school | ||||
| 3 | Anderson et al., 2015 53 | YRBS | PD = –0.5 (−1.68, +0.68) | |
| Past‐year DSM‐IV marijuana use disorder | ||||
| 5 | Wen et al., 2015 69 | NSDUH | PD = –0.07 (−0.76, +0.62) | |
| 18 | Choi 2014 68 | NSDUH | PD = +0.49 (−1.31, +2.30) | |
| Treatment admissions | ||||
| 3 | Anderson et al., 2015 53 | TEDS | %Δ‐MJ admissions = −6.7 (−29.2, 15.8) | |
| 4 | Pacula et al., 2015 46 | TEDS | %Δ‐MJ admissions = –12.9 (−23.3, −2.5) | |
| 17 | Pacula et al., 2013 70 | TEDS | %Δ‐MJ admissions = –15 (−27.2, −2.8) | |
MML = medical marijuana law (MML); MTF = Monitoring the Future Study; NLSY = National Longitudinal Survey of Youth; NSDUH = National Survey on Drug Use and Health; TEDS = Treatment Episode Data Set; YRBS = Youth Risk Behavior Survey.
Additional marijuana outcomes (e.g. heavy marijuana use) may be affected by MML, but hidden in tests of ‘any marijuana use’ if, for example, changes occur only among existing users. Nineteen tests of additional marijuana outcomes were conducted, of which five were significant. One test each indicated a significant pre–post increase in number of days used in the past month [change (Δ) in no. of days, 95% CI = +0.46 (0.05, +0.88)] 46 and in the number of days used in the past month among users [Δ in no. of days, 95% CI = +1.82 (1.18, +2.46)] 68. A single test found a significant pre–post increase in marijuana use initiation [prevalence difference = +0.32 (+0.01, +0.63)] 69. Two tests found a significant pre–post decrease in treatment admissions for marijuana use [%Δ‐MJ admissions = –12.9 (−23.3, −2.5) 46 and −15 (–27.2, −2.8) 70].
Individual state laws (Table 4)
Table 4.
Specific effects and robustness checks results from across all 21 papers included in the systematic review.
| Paper [reference number] | Pre–post MML change within MML states | |
|---|---|---|
| Overall finding | ||
| + (increase, P < 0.05) or – (decrease, P < 0.05) or NS (P > 0.05) | ||
| MML provisions and individual state laws | ||
| Individual states | ||
| Montana | 95; 95; 95; 95; 95; 95; 52 | NS, NS, NS, NS, NS, NS, − |
| Rhode Island | 95; 95; 95; 52 | NS, NS, NS, NS |
| Michigan | 95 | NS |
| Colorado | 88 | NS |
| Maine | 52 | NS |
| Nevada | 52 | – |
| Vermont | 52 | NS |
| Law variations | ||
| Requirement for patient registries | 70; 70; 69; 46; 73 | NS, NS, NS, +, +a |
| Registration rates | 51 | +b |
| Allowance for dispensaries | 70; 70; 46; 73; 73; 73; 73; 63; 69 | NS, NS, NS, NS, NSc, NSd, NSe, NS, + |
| Number of patients allowed per care‐giver | 73; 73 | NS, NSf |
| Allowance for home cultivation | 70; 73; 69; 95; 73; 46; 70 | NS, NS, NS, NSg, NSh, −, − |
| Number usable ounces allowed | 73; 73 | NSi, + |
| Generic ‘chronic pain’ as eligible condition | 69 | NS |
| MML provision index score | 73 | – |
| Senate/ballot‐passed | 96; 96 | NSj, NSk |
| Subgroups | ||
| Grade | ||
| 8th | 63; 64 | –, − |
| 9th and higher | 52; 63; 64; 52; 52; 63; 64; 52 | NSl, NSm, NSm, NSm, NSn, NSo, NSo, NSo |
| Age group | 53; 53 | NSp, NSq |
| Perceived risk | 64; 87) | –r, NSs |
| Gender | 53; 53 | NSt, NSu |
A test of the same specific effect from the same study is listed more than once if tests are formulated differently (e.g. different years data used or comparison group). MML = medical marijuana law; NS = not significant.
‘voluntary registration’ [Maine];
per‐capita registration rate;
‘active’ dispensaries;
‘for‐profit’ dispensaries;
dispensary index score;
≥ 5 patients allowed per care‐giver;
limit (yes/no) for no. of plants allowed for home cultivation;
≥ 10 plants allowed for home cultivation;
usable amount is limited to 2.5 ounces (yes/no);
ballot‐passed;
senate‐passed;
9th grade;
10th grade;
11th grade;
12th grade;
<17 years old;
≥17 years old;
perceives great or moderate risk of harm in occasional marijuana use;
perceives no or slight risk of harm in occasional marijuana use;
males;
females.
Examining the effect of individual state MMLs is important if MML effects differ for each particular law. This aim is approached by comparing trends in one MML state to a set of control states, a single control state or even a synthetic control, when the use of a traditional control group is questionable 71, 72. Three studies reported 16 tests of pre–post change in past‐month marijuana use for seven state laws (Montana, Rhode Island, Michigan, Colorado, Maine, Nevada and Vermont). Two tests found significant pre–post decreases in marijuana use (Montana, Nevada). These tests are distinguished by an extended span of data years (1991–2011) compared to 10 non‐significant tests from a single study spanning only a fraction of that period (2003–2009).
MML provisions (Table 4)
The specific provisions of MML are important targets of study because they indicate heterogeneity within this class of state policy and are potentially actionable in terms of further policy adaptations. For example, permitting dispensaries may indicate how widely medical marijuana is available (via increased supply and resulting diversion of marijuana to the youth recreational market) or visible (e.g. through dispensary advertising) in a state. A total of nine types of MML provisions and characteristics were tested.
Five tests examined whether or not a state required medical marijuana patients to be registered. Two indicated a significant pre–post increase in past‐month marijuana use among states that required patients to be registered.
Nine tests examined allowances for dispensaries. Only one indicated a significant pre–post increase in past‐month marijuana use in states that permitted dispensaries.
Seven tests examined allowance for home cultivation of medical marijuana. One indicated a significant pre–post decrease in past‐month marijuana use in states that allowed home cultivation.
Two tests each examined: number of patients allowed per care‐giver; number of ounces allowed per user; and whether the MML was passed by state legislature or ballot initiative. A single test each examined: generic ‘chronic pain’ as an eligible condition; and an ‘index score’ for MML provisions. Of all these tests, one test for number of ounces allowed and the single test for the MML provision ‘index’ (described in the original manuscript 73) indicated a significant pre–post decrease in past‐month marijuana use.
One study 51 found a positive relationship between adolescent marijuana use prevalence and the proportion of adults in that state who were registered as authorized medical marijuana users. Among the MML characteristics examined previously, this variable is unique in its potential to indicate year‐to‐year changes in the extent to which the state population is engaging with the medical marijuana market. This type of characteristic is important to study, as medical marijuana markets can ebb and flow in response to various economic and political forces while the letter of the MML in that state remains constant.
Subgroup analyses
Subgroup analyses may identify effects that are particular to vulnerable populations. Effects in different subgroups may even be countervailing, and thus hidden when testing overall populations. Ten tests were conducted among school‐grade‐specific subgroups, two among age‐specific subgroups, two among subgroups defined by perceived risk of marijuana use and two among gender‐specific subgroups. Two tests among 8th‐grade students and the test among adolescents who perceived great or moderate risk in occasional marijuana use indicated pre–post decreases in past‐month marijuana use.
Discussion
This systematic review screened 2999 unique papers retrieved from 17 sources, yielding 21 unique studies. Ultimately, 11 studies passed secondary exclusion criteria designed to ensure optimal study quality. Studies employed a wide variety of state‐ and individual‐level adjustments, specifications of state‐specific effects and secular trends and data that varied substantially in the number of analyzed years and states. However, all estimates of pre–post changes in past‐month marijuana use within MML states from these studies were non‐significant. Fixed‐effects meta‐analysis of these estimates yielded a non‐significant pooled association centered around the null, which was robust to the inclusion of estimates from non‐peer‐reviewed manuscripts and a test of the impact of data source on these estimates.
A single analysis excluded from the meta‐analysis estimated a significant positive estimate of pre–post changes in past‐month marijuana use 74. Close examination of the modeling specifications of included studies revealed that the outlier study reporting the positive effect was unique in its exclusion of a crucial adjustment for pre‐existing differences between states that did and did not pass MMLs during the study period. In a replication and commentary on this study 60, inclusion of this adjustment was shown to reduce the estimate of the pre–post change in past‐month marijuana use to non‐significance. Furthermore, all four studies that estimated pre‐law differences between MML and non‐MML states found a significantly higher prevalence of past‐month marijuana use in MML states compared to non‐MML states before MMLs were passed, illustrating the importance of incorporating these differences into studies of MML effects.
The great preponderance of tests of specific MML effects were non‐significant. Significant positive effects on additional marijuana use outcomes were observed for marijuana initiation 69 and days used in the past‐month 46 overall and among users 68. Significant negative effects were also observed for tests of marijuana treatment admissions within the Treatment Episode Data Set (TEDS) 46, 70. Whether heterogeneity in results occurred spuriously or due to real differences in MML effects between populations is unclear. Pacula 46 speculated that differences in the age distribution of the NLSY (a fixed cohort that ages as laws are passed) versus the TEDS (whose age distribution remains constant over time) may explain some differences. This explanation is consistent with observations of significant negative pre–post changes in past‐month marijuana use observed among 8th‐graders in the MTF 63, 64, in contrast to significant positive effects of MMLs on the prevalence of use among adults 69, 75.
Limitations of reviewed studies are noted. First, all studies used data from four large‐scale surveys (MTF, NSDUH, NLSY, YRBS). The non‐independence of studies somewhat limited the value of replication, although variation in study methods (e.g. years, states included) partially offset this concern. Ideally, multiple studies with little overlap in study designs and sampling frames would have examined the research question, each presenting results from a range of models reflecting both user prevalence and patterns of use among users. However, given that nationally representative data sets are limited while reproducibility is paramount 76, showing that different research teams demonstrated almost the same findings across overlapping data sources is an important gain in knowledge. Each of these data sources also has weaknesses 70. The MTF and NLSY are not designed to directly provide state‐representative estimates. The NSDUH is designed for this purpose, but NSDUH data prior to 2002 cannot be included 77, and thus inference is limited to states passing MML after 2002. The YRBS is only conducted biennially and state participation is inconsistent over time, with important MML states (California, Oregon, Washington, Colorado) excluded entirely.
Secondly, all studies employed a DID modeling strategy to identify MML effects. Although the DID approach can adjust statistically for both unmeasured time‐invariant and measured time‐varying confounding variables, inferences from DID tests rely upon correct model assumptions, as is always the case. The consistency of pre‐policy trends in the outcome variables between the treated and control states is an assumption not always tested in this literature. A second assumption is that MMLs affect only adolescents in states that pass them. If the alternative operated (i.e. spill‐over effects or contamination bias 78, 79, 80), this would weaken the ability to draw policy‐relevant conclusions from DID tests. Adolescents in non‐MML states may be affected by the national conversation around MML passage in states other than their own (through popular culture and/or social media), or inter‐state diversion of medical marijuana may affect price and/or availability of marijuana in non‐MML states. As of this writing, more than half of US states now have MMLs, and attitudes towards marijuana have become more positive in adults and in adolescents nation‐wide 81, 82; the directionality between changes in state and national attitudes and passage of state MMLs is unknown.
Thirdly, the provisions included in MMLs vary substantially across states and over time, as do local, state and federal regulatory practices 45, 46. Current evidence does not present strong or consistent support for the effects of particular MML provisions on adolescent marijuana use, but this may be due to unmeasured dynamics of these policies and the federal enforcement surrounding them, which were considered by only a single study 51. More is needed to understand how federal policy modifies the effect of state MMLs. Until then, the variations in the provisions of MMLs present challenges to policymakers who seek to make predictions about the effects of a potential MML for their own unique populations 83.
Fourthly, multiple studies have observed associations between MML passage and increases in marijuana use among adults 69, 75, 84, 85. These findings suggest that different mechanisms operate among different age groups; for example, perhaps via greater interest in MML or direct knowledge of the MML among adults than among teens. Further study of adults is warranted, as well as clarification of these differential mechanisms.
In summary, current evidence does not support the hypothesis that MML passage is associated with increased marijuana use prevalence among adolescents in states that have passed such laws up until 2014. Based on this evidence, we recommend several steps to advance the understanding of current and future marijuana policy effects. First, continued exploration of the effects of these state policies on different measures of use among adolescents is warranted. While evidence is clear regarding MML effects on annual and past‐month prevalence, evidence regarding effects on daily/near‐daily use, marijuana abuse/dependence and intensity of use have not been explored as thoroughly, and warrant additional consideration in light of decreasing national trends in marijuana risk perceptions among adolescents 54, 86. Secondly, continued monitoring of adolescent marijuana use in MML states is critical in light of differential development of commercialized markets. Recent studies have shown a rapid diffusion of medical marijuana stores and increased commercialization in selective states following the 2009 Ogden memo, which de‐prioritized federal enforcement against individuals compliant with state MMLs 51, 75, 87, 88, 89. Studies evaluating the impact of this rapid commercialization on youth marijuana use have shown a more consistently positive effect 51, 90, 91. Such findings are particularly relevant in light of recent recreational marijuana laws, all of which so far allow commercial distribution systems 92. Thirdly, further studies should be conducted in adults, for which the limited literature suggests a positive effect of MMLs on marijuana use 65, 69, 75. Fourthly, investigators should experiment with process‐based models of information and product diffusion that can estimate MML effects even in the presence of spill‐over effects into non‐MML states 93. Finally, increased coordination among researchers across multiple disciplines is needed to maximize efficiency in studying these urgent research questions in the context of rapidly changing marijuana policy.
Declaration of interests
None.
Supporting information
Table S1 Basic characteristics of studies—excluded from meta‐analysis, published in peer‐reviewed journals.
Table S2 Results and basic characteristics of studies excluded from the meta‐analysis because they were not published in peer‐reviewed journals.
Table S3 Primary model specifications of meta‐analyzed studies.
Acknowledgements
Support is acknowledged from National Institute on Drug Abuse grants R01DA034244 (D.S.H., R.L.P.), R01DA040924 (Principle Investigator M.C.), K01DA030449 (Principle Investigator M.C.), T32DA031099 (D.S.F., E.G.; Principle Investigator D.S.H.), National Institute on Alcohol Abuse and Alcoholism grant K01AA021511 (Principle Investigator K.M.K.), and by the New York State Psychiatric Institute (D.S.H., M.M.W.). We are grateful for consultations with Drs Esther Choo, Rosanna Smart and Mark Anderson, who were generously responsive in providing additional information concerning studies included in this review.
Sarvet, A. L. , Wall, M. M. , Fink, D. S. , Greene, E. , Le, A. , Boustead, A. E. , Pacula, R. L. , Keyes, K. M. , Cerdá, M. , Galea, S. , and Hasin, D. S. (2018) Medical marijuana laws and adolescent marijuana use in the United States: a systematic review and meta‐analysis. Addiction, 113: 1003–1016. doi: 10.1111/add.14136.
References
- 1. World Health Organization . Management of substance abuse, Cannabis 2017. Available at: http://www.who.int/substance_abuse/facts/cannabis/en (accessed 22 September 2017) (Archived at http://www.webcitation.org/6td9qF58M).
- 2. Blanco C., Hasin D. S., Wall M. M., Florez‐Salamanca L., Hoertel N., Wang S. et al Cannabis use and risk of psychiatric disorders: prospective evidence from a US national longitudinal study. JAMA Psychiatry 2016; 73: 388–395. [DOI] [PubMed] [Google Scholar]
- 3. Fergusson D. M., Boden J. M., Horwood L. J. Psychosocial sequelae of cannabis use and implications for policy: findings from the Christchurch Health and Development Study. Soc Psychiatry Psychiatr Epidemiol 2015; 50: 1317–1326. [DOI] [PubMed] [Google Scholar]
- 4. Lev‐Ran S., Imtiaz S., Taylor B. J., Shield K. D., Rehm J., Le Foll B. Gender differences in health‐related quality of life among cannabis users: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend 2012; 123: 190–200. [DOI] [PubMed] [Google Scholar]
- 5. Compton W. M., Gfroerer J., Conway K. P., Finger M. S. Unemployment and substance outcomes in the United States 2002–2010. Drug Alcohol Depend 2014; 142: 350–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kalousova L., Burgard S. A. Unemployment, measured and perceived decline of economic resources: contrasting three measures of recessionary hardships and their implications for adopting negative health behaviors. Soc Sci Med 2014; 106: 28–34. [DOI] [PubMed] [Google Scholar]
- 7. Lenne M. G., Dietze P. M., Triggs T. J., Walmsley S., Murphy B., Redman J. R. The effects of cannabis and alcohol on simulated arterial driving: Influences of driving experience and task demand. Accid Anal Prev 2010; 42: 859–866. [DOI] [PubMed] [Google Scholar]
- 8. Hartman R. L., Huestis M. A. Cannabis effects on driving skills. Clin Chem 2013; 59: 478–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brady J. E., Li G. Trends in alcohol and other drugs detected in fatally injured drivers in the United States, 1999–2010. Am J Epidemiol 2014; 179: 692–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ramaekers J. G., Berghaus G., van Laar M., Drummer O. H. Dose related risk of motor vehicle crashes after cannabis use. Drug Alcohol Depend 2004; 73: 109–119. [DOI] [PubMed] [Google Scholar]
- 11. Agrawal A., Nelson E. C., Bucholz K. K., Tillman R., Grucza R. A., Statham D. J. et al Major depressive disorder, suicidal thoughts and behaviours, and cannabis involvement in discordant twins: a retrospective cohort study. Lancet Psychiatry 2017; 4: 706–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gage S. H., Hickman M., Zammit S. Association between cannabis and psychosis: epidemiologic evidence. Biol Psychiatry 2016; 79: 549–556. [DOI] [PubMed] [Google Scholar]
- 13. Kraan T., Velthorst E., Koenders L., Zwaart K., Ising H. K., van den Berg D. et al Cannabis use and transition to psychosis in individuals at ultra‐high risk: review and meta‐analysis. Psychol Med 2016; 46: 673–681. [DOI] [PubMed] [Google Scholar]
- 14. Hasin D. S. US Epidemiology of Cannabis Use and Associated Problems. Neuropsychopharmacology 2017; 1: 195–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hasin D. S., Kerridge B. T., Saha T. D., Huang B., Pickering R., Smith S. M. et al Prevalence and correlates of DSM‐5 cannabis use disorder, 2012–2013: findings from the National Epidemiologic Survey on Alcohol and Related Conditions‐III. Am J Psychiatry 2016; 173: 588–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Volkow N. D., Baler R. D., Compton W. M., Weiss S. R. Adverse health effects of marijuana use. N Engl J Med 2014; 370: 2219–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chen C. Y., Storr C. L., Anthony J. C. Early‐onset drug use and risk for drug dependence problems. Addict Behav 2009; 34: 319–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kandel D. B., Yamaguchi K., Chen K. Stages of progression in drug involvement from adolescence to adulthood: further evidence for the gateway theory. J Stud Alcohol 1992; 53: 447–457. [DOI] [PubMed] [Google Scholar]
- 19. King K. M., Chassin L. A prospective study of the effects of age of initiation of alcohol and drug use on young adult substance dependence. J Stud Alcohol Drugs 2007; 68: 256–265. [DOI] [PubMed] [Google Scholar]
- 20. Fergusson D. M., Boden J. M. Cannabis use and later life outcomes. Addiction 2008; 103: 969–976; discussion 77–8. [DOI] [PubMed] [Google Scholar]
- 21. Hall W., Degenhardt L. Adverse health effects of non‐medical cannabis use. Lancet 2009; 374: 1383–1391. [DOI] [PubMed] [Google Scholar]
- 22. Cerda M., Moffitt T. E., Meier M. H., Harrington H., Houts R., Ramrakha S. et al Persistent cannabis dependence and alcohol dependence represent risks for midlife economic and social problems: a longitudinal cohort study. Clin Psychol Sci 2016; 4: 1028–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zalesky A., Solowij N., Yucel M., Lubman D. I., Takagi M., Harding I. H. et al Effect of long‐term cannabis use on axonal fibre connectivity. Brain J Neurol 2012; 135: 2245–2255. [DOI] [PubMed] [Google Scholar]
- 24. Meier M. H., Caspi A., Ambler A., Harrington H., Houts R., Keefe R. S. et al Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci USA 2012; 109: E2657–E2664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lynskey M., Hall W. The effects of adolescent cannabis use on educational attainment: a review. Addiction 2000; 95: 1621–1630. [DOI] [PubMed] [Google Scholar]
- 26. Maggs J. L., Staff J., Kloska D. D., Patrick M. E., O'Malley P. M., Schulenberg J. Predicting young adult degree attainment by late adolescent marijuana use. J Adolesc Health 2015; 57: 205–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chatterji P. Illicit drug use and educational attainment. Health Econ 2006; 15: 489–511. [DOI] [PubMed] [Google Scholar]
- 28. Keyes K. M., Schulenberg J. E., O'Malley P. M., Johnston L. D., Bachman J. G., Li G. et al The social norms of birth cohorts and adolescent marijuana use in the United States, 1976–2007. Addiction 2011; 106: 1790–1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cook P. Paying the Tab: The Costs and Benefits of Alcohol Control. Princeton, NJ: Princeton University Press; 2007. [Google Scholar]
- 30. Wagenaar A. C., Toomey T. L. Effects of minimum drinking age laws: review and analyses of the literature from 1960 to 2000. J Stud Alcohol Suppl 2002. 206–225. [DOI] [PubMed] [Google Scholar]
- 31. Birckmayer J., Hemenway D. Minimum‐age drinking laws and youth suicide, 1970–1990. Am J Public Health 1999; 89: 1365–1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Carpenter C., Kloska D., O'Malley P., Johnston L. D. Alcohol control policies and youth alcohol consumption: evidence from 28 years of monitoring the future. BE J Econom Anal Policy 2007; 7: 25. [Google Scholar]
- 33. O'Malley P. M., Wagenaar A. C. Effects of minimum drinking age laws on alcohol use, related behaviors and traffic crash involvement among American youth: 1976–1987. J Stud Alcohol 1991; 52: 478–491. [DOI] [PubMed] [Google Scholar]
- 34. Norberg K. E., Bierut L. J., Grucza R. A. Long‐term effects of minimum drinking age laws on past‐year alcohol and drug use disorders. Alcohol Clin Exp Res 2009; 33: 2180–2190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Whiting P. F., Wolff R. F., Deshpande S., Di Nisio M., Duffy S., Hernandez A. V. et al Cannabinoids for medical use: a systematic review and meta‐analysis. JAMA 2015; 313: 2456–2473. [DOI] [PubMed] [Google Scholar]
- 36. Medical marijuna referenda movement in America: hearing before the Subcommittee on Crime of the Committee on the Judiciary House of Representatives. Washington, DC: House of Representatives; 1997. [Google Scholar]
- 37. Pacula R. L., Kilmer B., Grossman M., Chaloupka F. J. Risks and prices: the role of user sanctions in marijuana markets. BE J Econom Anal Policy 2010; 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Thurstone C., Lieberman S. A., Schmiege S. J. Medical marijuana diversion and associated problems in adolescent substance treatment. Drug Alcohol Depend 2011; 118: 489–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. O'Connor A. Marijuana use growing among teenagers 2011. Available at: https://well.blogs.nytimes.com/2011/12/14/marijuana-growing-in-popularity-among-teenagers (accessed 22 September 2017) (Archived at http://www.webcitation.org/6tdA12566).
- 40. Khatapoush S., Hallfors D. ‘Sending the wrong message’: did medical marijuana legalization in California change attitudes about and use of marijuana? J Drug Issues 2004; 34: 751–770. [Google Scholar]
- 41. O'Keef K., Earleywine M., Mirken B. Marijuana use by young people: the impact of state medical marijuana laws. 2008. Available at: http://csdp.org/research/2005TeenUseReport.pdf (accessed 22 September 2017) (Archived at http://www.webcitation.org/6tdAAVUVY).
- 42. MacCoun R. J. Drugs and the law: a psychological analysis of drug prohibition. Psychol Bull 1993; 113: 497–512. [DOI] [PubMed] [Google Scholar]
- 43. Wakefield M., Terry‐McElrath Y., Emery S., Saffer H., Chaloupka F. J., Szczypka G. et al Effect of televised, tobacco company‐funded smoking prevention advertising on youth smoking‐related beliefs, intentions, and behavior. Am J Public Health 2006; 96: 2154–2160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. National Institute on Drug Abuse . 2016–2020 NIDA Strategic Plan: Advancing Addiction Science. Bethesda, MD: National Institutes of Health, US Department of Health and Human Services; 2015. [Google Scholar]
- 45. Pacula R. L., Hunt P., Boustead A. Words can be deceiving: a review of variation among legally effective medical marijuana laws in the United States. J Drug Policy Anal 2014; 7: 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Pacula R. L., Powell D., Heaton P., Sevigny E. L. Assessing the effects of medical marijuana laws on marijuana use: the devil is in the details. J Policy Anal Manage 2015; 34: 7–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Liberati A., Altman D. G., Tetzlaff J., Mulrow C., Gotzsche P. C., Ioannidis J. P. et al The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: explanation and elaboration. PLOS Med 2009; 6: e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc.; 2008. [Google Scholar]
- 49. Borenstein M., Hedges L., Higgins J. P. T., Rothstein H. R. Introduction to Meta‐analysis. Hoboken, JJ: Wiley & Sons; 2009. [Google Scholar]
- 50. Viechtbauer W. Conducting meta‐analyses in {R} with the {metafor} package. J Stat Softw 2010; 36: 1–48. [Google Scholar]
- 51. Smart R. The kids aren't alright but older adults are just fine: effects of medical marijuana market growth on substance use and abuse. Los Angeles, CA: University of California; 2015. [Google Scholar]
- 52. Choo E. K., Benz M., Zaller N., Warren O., Rising K. L., McConnell K. J. The impact of state medical marijuana legislation on adolescent marijuana use. J Adolesc Health 2014; 55: 160–166. [DOI] [PubMed] [Google Scholar]
- 53. Anderson D. M., Hansen B., Rees D. I. Medical marijuana laws and teen marijuana use. Am Law Econ Rev 2015; 17; 4950528. [Google Scholar]
- 54. Johnston L. D., O'Malley P. M., Miech R. A., Bachman J. G., Schulenberg J. E. Monitoring the Future National Survey Results on Drug use, 1975–2016: Overview, Key Findings on Adolescent Drug use. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2017. [Google Scholar]
- 55. Moore W., Pedlow S., Krishnamurty P. National Longitudinal Survey of Youth 1997 (NLSY97) Technical Sampling Report. Chicago, IL: Kirk Wolter National Opinion Research Center; 2000. [Google Scholar]
- 56. Substance Abuse and Mental Health Services Administration . National Survey on Drug Use and Health: Summary of Methdological Studies, 1971–2014. Rockville, MD: Maryland Center for Behavioral Health Statistics and Quality; 2014. [PubMed] [Google Scholar]
- 57. Brener N. D., Kann L., Shanklin S., Kinchen S., Eaton D. K., Hawkins J. et al Methodology of the Youth Risk Behavior Surveillance System—2013. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2013. [Google Scholar]
- 58. Imbens G. W., Wooldridge J. M. Recent developments in the econometrics of program evaluation. J Econ Lit 2009; 47: 5–86. [Google Scholar]
- 59. Angrist J. D., Pischke J. S. Mostly Harmless Econometrics: An Empiricist's Companion. Princeton, NJ: Princeton University Press; 2009. [Google Scholar]
- 60. Wall M. M., Mauro C., Hasin D. S., Keyes K. M., Cerda M., Martins S. S. et al Prevalence of marijuana use does not differentially increase among youth after states pass medical marijuana laws: commentary on and reanalysis of US National Survey on Drug Use in Households data 2002–2011. Int J Drug Policy 2016; 29: 9–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Clarke P., Crawford C., Steele F., Vignoles A. Revisiting fixed‐ and random‐effects models: some considerations for policy‐relevant education research. J Educ Econ 2015; 23: 259–277. [Google Scholar]
- 62. Baker M. Why scientists must share their research code Nature 2016. Available at: http://www.nature.com/news/why-scientists-must-share-their-research-code-1.20504 (accessed 22 September 2017) (Archived at http://www.webcitation.org/6tdAEaK90).
- 63. Hasin D. S., Wall M., Keyes K. M., Cerda M., Schulenberg J., O'Malley P. M. et al Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: results from annual, repeated cross‐sectional surveys. Lancet Psychiatry 2015; 2: 601–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Keyes K. M., Wall M., Cerda M., Schulenberg J., O'Malley P. M., Galea S. et al How does state marijuana policy affect US youth? Medical marijuana laws, marijuana use and perceived harmfulness: 1991–2014. Addiction 2016; 111: 2187–2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Martins S. S., Mauro C. M., Santaella‐Tenorio J., Kim J. H., Cerda M., Keyes K. M. et al State‐level medical marijuana laws, marijuana use and perceived availability of marijuana among the general U.S. population. Drug Alcohol Depend 2016; 169: 26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Hunt P. E., Miles J. The impact of legalizing and regulating weed: issues with study design and emerging findings in the USA In: Nielsen S., Bruno R., Schenk S., editors. Non‐medical and Illicit Use of Psychoactive Drugs. Current Topics in Behavioral Neurosciences, Vol. 34 New York, NY: Springer; 2015, pp. 173–198. [DOI] [PubMed] [Google Scholar]
- 67. Wolfers J. Did unilateral divorce laws raise divorce rates? A reconciliation and new results. Am Econ Rev 2006; 96: 1802–1820. [Google Scholar]
- 68. Choi A. The impact of medical marijuana laws on marijuana use and other risky health behaviors. Health & Healthcare in America: From Economics to Policy. Washington, DC: Ashecon; 2014. [Google Scholar]
- 69. Wen H., Hockenberry J. M., Cummings J. R. The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. J Health Econ 2015; 42: 64–80. [DOI] [PubMed] [Google Scholar]
- 70. Pacula R., Powell D., Heaton P., Sevigny E. L. Assessing the effects of medical marijuana laws on marijuana and alcohol use: the devil is in the details. Report no.: Working Paper 19302. Cambridge, MA: National Bureau of Economic Research; 2013.
- 71. Abadie A., Diamond A., Hainmueller J. Synthetic control methods for comparative case studies: estimating the effect of California's tobacco control program. J Am Stat Assoc 2010; 105: 493–505. [Google Scholar]
- 72. Abadie A., Diamond A., Hainmueller J. Comparative politics and the synthetic control method. Am J Polit Sci 2015; 59: 495–510. [Google Scholar]
- 73. Johnson J., Hodgkin D., Harris S. K. The design of medical marijuana laws and adolescent use and heavy use of marijuana: analysis of 45 states from 1991 to 2011. Drug Alcohol Depend 2017; 170: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Stolzenberg L., D'Alessio S. J., Dariano D. The effect of medical cannabis laws on juvenile cannabis use. Int J Drug Policy 2016; 27: 82–88. [DOI] [PubMed] [Google Scholar]
- 75. Hasin D., Sarvet A. L., Cerda M., Keyes K. M., Stohl M. S., Galea S. et al U.S. adult illicit cannabis use, cannabis use disorder, and medical marijuana laws: 1991–1992 to 2012–2013. JAMA Psychiatry 2017; 74: 579–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Munafò M., Nosek B. A., Bishop D. V. M., Button K. S., Chambers C. D., du Sert N. P. et al A manifesto for reproducible science. Nature Human Behavior 2017. Available at: https://www.nature.com/articles/s41562-016-0021 (accessed 22 September 2017) (Archive at http://www.webcitation.org/6wDy57JGu). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Substance Abuse and Mental Health Services Administration Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- 78. Schwartz S., Gatto N. M., Campbell U. B. Extending the sufficient component cause model to describe the Stable Unit Treatment Value Assumption (SUTVA). Epidemiol Perspect Innov 2012; 9: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. VanderWeele T. J. Concerning the consistency assumption in causal inference. Epidemiology 2009; 20: 880–883. [DOI] [PubMed] [Google Scholar]
- 80. Torgerson D. J. Contamination in trials: is cluster randomisation the answer? BMJ 2001; 322: 355–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Compton W. M., Han B., Jones C. M., Blanco C., Hughes A. Marijuana use and use disorders in adults in the USA, 2002–14: analysis of annual cross‐sectional surveys. Lancet Psychiatry 2016; 3: 954–964. [DOI] [PubMed] [Google Scholar]
- 82. Pacek L. R., Mauro P. M., Martins S. S. Perceived risk of regular cannabis use in the United States from 2002 to 2012: differences by sex, age, and race/ethnicity. Drug Alcohol Depend 2015; 149: 232–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Hernan M. A., VanderWeele T. J. Compound treatments and transportability of causal inference. Epidemiology 2011; 22: 368–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Chu Y. L. Do medical marijuana laws increase hard drug use? The Journal of Law and Economics 2015; 58: 481–517. [Google Scholar]
- 85. Chu Y. W. The effects of medical marijuana laws on illegal marijuana use. J Health Econ 2014; 38: 43–61. [DOI] [PubMed] [Google Scholar]
- 86. Azofeifa A., Mattson M. E., Schauer G., McAfee T., Grant A., Lyerla R. National estimates of marijuana use and related indicators—national survey on drug use and health, United States, 2002–2014. Contract no.: 11. Morb Mort Wkly Rep Surveill Summ 2016; 65: 1–28. [DOI] [PubMed] [Google Scholar]
- 87. Ghosh T. S., Van Dyke M., Maffey A., Whitley E., Erpelding D., Wolk L. Medical marijuana's public health lessons—implications for retail marijuana in Colorado. N Engl J Med 2015; 372: 991–993. [DOI] [PubMed] [Google Scholar]
- 88. Schuermeyer J., Salomonsen‐Sautel S., Price R. K., Balan S., Thurstone C., Min S. J. et al Temporal trends in marijuana attitudes, availability and use in Colorado compared to non‐medical marijuana states: 2003–11. Drug Alcohol Depend 2014; 140: 145–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Cambron C., Guttmannova K., Fleming C. B. State and national contexts in evaluating cannabis laws: a case study of Washington State. J Drug Issues 2016; 47: 74–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. D'Amico E. J., Miles J. N., Tucker J. S. Gateway to curiosity: medical marijuana ads and intention and use during middle school. Psychol Addict Behav 2015; 29: 613–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Salomonsen‐Sautel S., Min S. J., Sakai J. T., Thurstone C., Hopfer C. Trends in fatal motor vehicle crashes before and after marijuana commercialization in Colorado. Drug Alcohol Depend 2014; 140: 137–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Kilmer B., Pacula R. L. Understanding and learning from the diversification of cannabis supply laws. Addiction 2017; 112: 1128–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Chen X. J. Information diffusion in the evaluation of medical marijuana laws’ impact on risk perception and use. Am J Public Health 2016; 106: e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Harper S., Strumpf E. C., Kaufman J. S. Do medical marijuana laws increase marijuana use? Replication study and extension. Ann Epidemiol 2012; 22: 207–212. [DOI] [PubMed] [Google Scholar]
- 95. Lynne‐Landsman S. D., Livingston M. D., Wagenaar A. C. Effects of state medical marijuana laws on adolescent marijuana use. Am J Public Health 2013; 103: 1500–1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. de Silva N., Torgler B. Smoke signals and mixed messages: medical marijuana and drug policy signalling effects. Contract no.: Working Paper no. 2011–18. Basel, Switzerland: Center for Research in Economics, Management and the Arts; 2011.
- 97. Wall M. M., Poh E., Cerda M., Keyes K. M., Galea S., Hasin D. S. Adolescent marijuana use from 2002 to 2008: higher in states with medical marijuana laws, cause still unclear. Ann Epidemiol 2011; 21: 714–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Wen H., Hockenberry J. M., Cummings J. R. The effect of medical marijuana laws on marijuana, alcohol, and hard drug use. Contract no.: Working Paper 20085. Cambridge, MA: National Bureau of Economic Research; 2014.
- 99. Johnson J. K. Do state liberalized marijuana policies affect adolescent marijuana and alcohol use? A State‐Level Analysis. Waltham, MA: Heller School of Social Policy and Management, Brandeis University; 2015. [Google Scholar]
- 100. Anderson D. M., Hansen B., Rees D. I. Medical marijuana laws and teen marijuana use. Contract no.: Discussion Paper no. 6592. Bonn, Germany: Institute for the Study of Labor; 2012.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Basic characteristics of studies—excluded from meta‐analysis, published in peer‐reviewed journals.
Table S2 Results and basic characteristics of studies excluded from the meta‐analysis because they were not published in peer‐reviewed journals.
Table S3 Primary model specifications of meta‐analyzed studies.


