Weight fluctuations and aging can lead to an altered distribution of subcutaneous fat and changes in skin elasticity.1 In the posterior and lateral upper torso, this process may result in overhanging subcutaneous fat and skin, popularly known as bra-line bulging. This is cosmetically undesirable and, in most patients, unresponsive to dieting and exercise. It is also difficult to treat by liposuction, heat, ultrasound, or cryolipolysis. Plastic surgery options such as the bra-line back lift1 are the most appropriate for patients with a severe degree of bra-line bulging. Furthermore, surgical procedures are invasive, time consuming, complicated because of significant underlying anatomic structures, and may result in complications and scar formation. There is a clear need for alternative bra-line lipolysis options.
Injection lipolysis using deoxycholic acid (DCA) is a minimally invasive technique recently approved by the Food and Drug Administration (FDA) to treat subcutaneous fat in the submental area, by injecting a cytolytic drug into the superficial adipose tissue.2,3 DCA used here (ATX-101, before FDA-approval; Kybella [United States], Belkyra [Canada]; Kythera Biopharmaceuticals, Inc., Westlake Village, CA, acquired by Allergan, Inc.) is a proprietary formulation of synthetically derived DCA used for injection lipolysis.4 When injected into tissues, DCA destroys cell membranes causing cytolysis, preferentially of fat cells, because of a higher affinity for adipose cell membranes than other tissue cell membranes.3 Presently, it is the first and only FDA-approved injectable treatment for improving the appearance of moderate-to-severe convexity or fullness associated with submental fat in adults.2
Given the efficacy and safety of DCA injection lipolysis in the submental area, its use for body contouring in other anatomical areas to treat small volume, localized fat deposits should be explored.5 This technique can be an excellent therapeutic approach for mild excess fat in the pectoralis/underarm/triceps/upper back (collectively called the “bra-line” in females) in carefully selected patients, usually with a body mass index <25.
A 46-year-old, healthy Caucasian female (Case A) presented for improving the appearance of bilateral bra-line bulging in the upper back. General examination was normal. Local examination revealed diffuse, nontender bilateral excess fat, homogenous to palpation, measuring approximately 4 cm bilaterally, located in the upper back just above the horizontal bra-line, medial to the posterior axillary line (Figure 1A).
Figure 1.
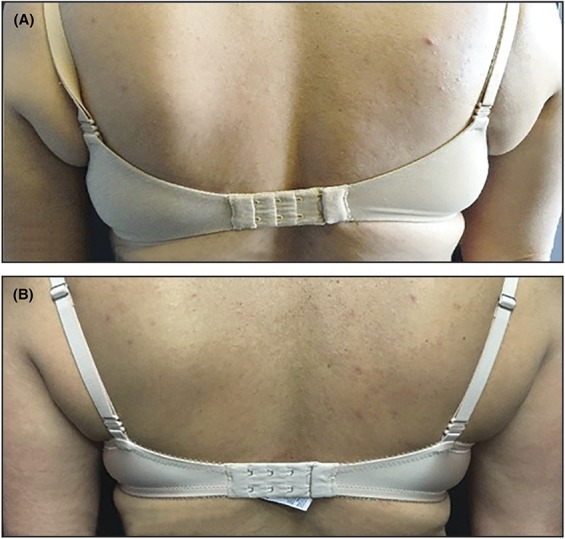
Case A before DCA injection (A) and 3 months after DCA injection (B). DCA, deoxycholic acid.
Another patient, a 47-year-old, healthy East Indian female (Case B) presented with bra-line bulging at the lateral side of both breasts (in the area of the axillary tail of Spence). General examination was normal. On local examination, diffuse, nontender bilateral bulging of adipose tissue with homogenous consistency, measuring 2 cm bilaterally was palpated medial to the anterior axillary line (Figure 2A).
Figure 2.
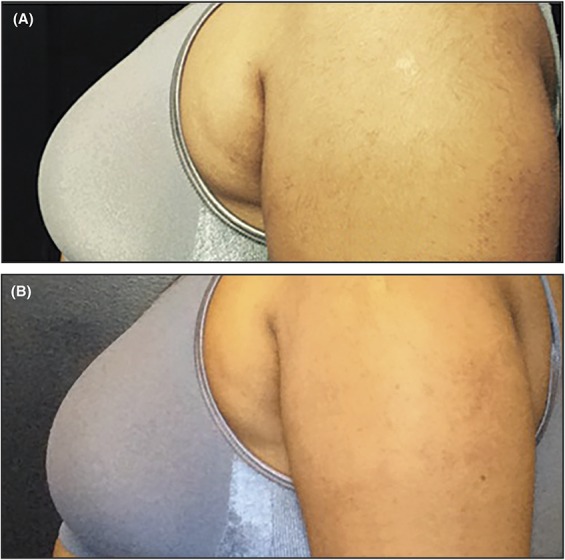
Case B before DCA injection (A) and 9 months after DCA injection (B). DCA, deoxycholic acid.
Both patients were unwilling to undergo surgical intervention. The option of DCA injection lipolysis was offered as a minimally invasive treatment after confirming that the patients did not have cutaneous disease in the treatment area, were free of any systemic diseases, had no known allergies, and were not pregnant or lactating. The procedure and potential side effects (injection site edema, hematoma, pain, numbness, erythema, and induration) were explained, and off-label consent was obtained. The number of injections and treatment sessions were determined according to each patient's fat distribution and treatment goals. The principles of the 1975 Declaration of Helsinki were followed.
Both patients received 1 injection treatment session, seated upright for proper visualization of anatomic contours. Patient A received 2-mL DCA injections on each side (total 4 mL). Patient B received 1-mL DCA injections on each side (total 2 mL). DCA was injected with a 32-gauge needle held perpendicular to the skin. Injections of 0.15 mL each were distributed with injections spaced 0.5 to 1.0 cm apart, covering the treatment area. Care was taken to inject DCA only into the subcutaneous fat and not intradermally or into underlying muscles or soft tissues. For Case B, the injection site was in the direction of the pectoralis major tendon. DCA was injected with utmost caution to avoid lymph nodes and important neurovascular structures in close proximity. Ice was applied 5 minutes before and after treatment at the injection sites to minimize pain. After injection, both patients experienced moderate tenderness and a subcutaneous itching sensation in the treated areas, which subsided within 10 minutes. They were observed until the pain subsided. They experienced mild swelling in treated areas for 5 to 7 days. Both cases A and B reported a gradual decrease in fat bulging after treatment beginning 1 month and continuing until 3 and 9 months, respectively (Figures 1B and 2B). During follow-up, there was no re-accumulation of fat in treated areas, although neither patient experienced significant weight fluctuation. Both patients were highly satisfied with the initial treatment results. One more treatment session is planned for Case A, whereas Case B required no further treatment.
Conclusions
DCA injection, a minimally invasive procedure, was effectively used for the reduction of localized fat above the bra-line and was well tolerated. This report highlights my earliest experience with injectable treatment of bra-line fat accumulation in 2 patients and is the first US report of DCA lipolysis in this anatomic region. This area is relatively difficult to treat with other modalities but seems to be responsive to DCA injection. Safety can be ensured by administering DCA only in the subcutaneous fat. Thorough knowledge of the anatomy of underlying structures and skin thickness is essential. Efficacy can be maximized by careful patient selection. Lipolysis with DCA injection administered by trained physicians is a promising approach for treating bra-line fat. Here we demonstrate excellent efficacy with low dose DCA treatment in thin individuals. It is likely that most patients will need significantly more DCA per injection session. Large-scale clinical trials are needed to prove efficacy and safety of this technique.
Footnotes
Medical writing support was provided Vidula Bhole, MD, MHSc, of Cactus Communications, and funded by Allergan, Inc. Allergan, Inc. also paid for this article to be Open Access.
The author has indicated no significant interest with commercial supporters.
References
- 1.Hunstad JP, Khan PD. The bra-line back lift: a simple approach to correcting severe back rolls. Clin Plast Surg 2014;41:715–26. [DOI] [PubMed] [Google Scholar]
- 2.FDA approves treatment for fat below the chin. Available from: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm444978.htm. Accessed November 23, 2016.
- 3.Thuangtong R, Bentow JJ, Knopp K, Mahmood NA, et al. Tissue-selective effects of injected deoxycholate. Dermatol Surg 2010;36:899–908. [DOI] [PubMed] [Google Scholar]
- 4.Prescribing information. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2015/206333Orig1s000lbl.pdf. Accessed November 23, 2016.
- 5.Sykes JM, Allak A, Klink B. Future applications of deoxycholic acid in body contouring. J Drugs Dermatol 2017;16:43–6. [PubMed] [Google Scholar]


