Abstract
Objective
To appreciate the impact of the opioid epidemic in workers, we described opioid prescription patterns in a U.S. industrial cohort over a ten-year period and assessed predictors of chronic prescription.
Methods
A multiyear (2003–2013) cross-sectional analysis of employer-sponsored health care claims for enrolled workers (N: 21,357- 44,769) was performed.
Results
The proportion of workers prescribed opioids nearly doubled in the ten-year period. The strongest predictor of chronic opioid prescribing was year, with an increase in prescriptions each year from 2003 to 2013 (OR= 2.90, 95% CI: 2.41–3.48). Additional predictors included older age, white race, hourly wage, low back pain, and osteoarthritis.
Conclusions
Opioid prescribing for industrial workers substantially increased from 2003 to 2013. Occupational health professionals should be aware of the potential for chronic opioid use among workers to assess job safety and appropriate treatment of work-related injuries.
Introduction
In the last fifteen years, there has been an epidemic of opioid prescribing, opioid abuse, overdose, and overdose deaths in the United States (1, 2). The opioid epidemic is a major health problem affecting all people, but poses unique concerns for working individuals.
Industrial workers are susceptible to acute occupational and repetitive strain injuries (3). The aging workforce has increasingly been prescribed opioids for chronic pain conditions such as arthritis since 1999(1). Most estimates of opioid prescriptions in workers come from Worker’s Compensation claims, and estimates of opioid prescribing within 15 days of a work-related injury range from 6–53%, (4) depending on the geographic region and severity of the injury. Early opioid prescription for acute work-related low back pain is associated with increased worker disability, higher medical costs, prolonged claim duration, and lower work retention (5–8). Few studies have assessed the predictors of opioid prescribing among industrial workers(9).
Data to support the prescription of opioids for chronic pain reduction or functional improvement are lacking, (10–12) and chronic opioid use increases the risk of opioid abuse, overdose, fracture, and adverse cardiac outcomes(11, 13, 14). A recent large claims-based cohort study determined that 0.5% of injured workers prescribed opioids are diagnosed with opioid use disorder within 12 months of injury (15).
Workers diagnosed with opioid use disorder pose a much greater economic burden on the healthcare system, and workers on short term disability with diagnosed opioid abuse have significantly greater lost wages and time away from work than those without a diagnosis of opioid use disorder (15). The excess employer and societal costs related to opioid abuse are substantial. A 2011 cost analysis determined total yearly employer costs for opioid abuse to be greater than $25 billion in 2007 U.S. dollars irrespective of healthcare costs, which also totaled $25 billion. Lost work time, wages, and premature death made up the bulk of the employer-related costs (16). A more recent cost analysis determined employer-related excess health care costs and lost wage costs per employee with diagnosed opioid abuse to be close to $12,000 US dollars annually (17).
Assessing the burden and consequences of opioid prescribing in workers poses a unique challenge due to the siloed nature of Occupational Health and the Worker’s Compensation System. Workers may obtain prescriptions outside of the Workers’ Compensation system for pain that may or may not be related to a workplace injury (18). There is potential risk of opioid misuse if workers are filling prescriptions using multiple payment sources, such as private insurance and Workers’ Compensation (19). Another challenge is that clinicians outside of Occupational Health may have limited training in assessing workplace hazards. The American College of Occupational and Environmental Medicine recommends against the prescription of opioids for acute or chronic pain in safety-sensitive jobs (20). However, not all prescribers may be familiar with a patient’s occupational history, including work tasks, exposures, and safety risks.
In summary, industrial workers prescribed opioids may be at increased risk for injury, opioid misuse, and opioid use disorder. The objectives of this study are 1). to describe prescription patterns of opioids in an industrial cohort from employer-sponsored health insurance, which would represent prescriptions not covered by Worker’s Compensation, and 2). to describe predictors of chronic opioid use in an industrial cohort.
Methods
In this multiyear cross-sectional study, we analyzed employer-sponsored health claims from 76, 432 industrial workers from the years 2003 through 2013. To be eligible for study inclusion, workers needed to have three consecutive months of enrollment in the employer-sponsored health plan during any given year. In each year, over 80% of workers elected health benefits. The number of employees analyzed each year ranged from 22,714 to 44,704. The population of workers decreased over the course of the study period largely due to recession-related plant closures.
We obtained claims data on an industrial cohort from a specialty metals corporation with multiple manufacturing facilities geographically dispersed throughout the United States. Data analysis occurred between October of 2016 and June of 2017. We assessed opioid prescription frequency during each year from January to December, and did not attempt to track individuals through time. Any of the following medications were classified as opioids: oxycodone, hydrocodone, codeine, morphine, fentanyl, hydromorphone, tramadol, meperidine, methadone, buprenorphine, Demerol, and propoxyphene. Antitussive syrups and liquids, migraine relief medications, and antiemetic and antidiarrheal medications containing opioid medications were not classified as opioids for the purposes of this study. Long-term opioid therapy is defined as daily or near daily use of opioids over the course of 90 days or more (21). Prescription pharmacy claims provide number of days supplied, however, this is a frequent underestimate of the intended days’ supply in the case of opioid therapy, as pharmacists calculate this number using the maximum amount of medications a patient could take in 24 hours (22). Therefore, we defined chronic, or long-term, opioid prescription as the prescription of three or more consecutive opioids with a period of no more than 30 days between prescriptions, as has been done studies that utilize pharmacy claims data (23, 24).
We assessed the proportion of workers receiving one or more opioid prescriptions each year as well as the proportion of workers being prescribed opioids chronically each year during the study period. We also assessed the proportion of workers who were diagnosed with opioid use disorder (ICD-9 304.00, 304.01, 304.02, 304.03, 965.00, 965.09). To assess factors associated with chronic opioid use among those receiving opioid prescriptions, we analyzed employee-sponsored health claims data during each year of the study period. We assessed the relationship between chronic opioid prescriptions and opioid use disorder and age, sex, race, wage type, geographic region, and co-morbid conditions including psychiatric conditions, low back pain, other back and neck pain, neuropathic pain, and osteoarthritis. Co-morbid conditions were identified using International Classification of Diseases, Volume 2, Clinical Modification (ICD-9-CM) codes (see Table, Supplemental Digital Content 1, for the code listing).
Statistics/ data analysis
Statistical analyses were performed using SAS Version 9.4 (SAS Institute, Cary, NC). Descriptive statistics were calculated for the start and end year of the study (2003 and 2013, respectively) for the total eligible population and for the cohort of workers receiving at least one opioid prescription. Among those receiving one or more opioid prescriptions in a calendar year, unadjusted analyses were used to examine potential associations between demographic factors (age, sex, race/ethnicity, employee type, geographic region), co-morbid medical conditions, calendar year, and chronic opioid use. We then developed multivariate marginal (population-average) generalized linear models using generalized estimating equations (GEE) to determine predictors of chronic opioid use (Yes/No) among the cohort receiving any opioid prescriptions. All p-values were two sided and α < 0.05 was considered statistically significant.
Results
Table 1 displays characteristics for the total population of workers enrolled in health benefits as well as the sub-population of workers receiving one or more opioid prescription in 2003 compared to 2013. There were 44, 704 workers enrolled in the health plan in 2003 compared to 22, 714 in 2013. The proportion of employees electing benefits each year did not change much throughout the study period, ranging from 80.1–87.3%, with the low in 2004 and the high in 2008. The decrease in population was largely due to recession-related plant closures. The population of workers dropped in all regions over the ten-year period, and especially in the Mid-West and South (Table 1). Over three quarters of workers were white, 21% were female, and 67% received an hourly wage. The proportion of workers diagnosed with depression, anxiety, low back pain, other back and neck pain, osteoarthritis, and diabetes increased over the ten-year period.
Table 1.
Characteristics of Total Population and Workers Prescribed One or More Opioid, 2003 and 2013
| Year | 2003 | 2013 | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Population | Prescribed Opioids, n=4,698 |
Total, n= 44, 704 |
Prescribed Opioids, n= 4,239 |
Total, n= 22,714 |
||||
|
| ||||||||
| Characteristics | n | % | n | % | n | % | n | % |
| Age-mean, sd | 43.9 | 10.3 | 43.6 | 10.3 | 48.5 | 10.5 | 47.3 | 11.1 |
| Gender | ||||||||
| Female | 1118 | 23.8 | 9530 | 21.3 | 1090 | 25.7 | 4815 | 21.2 |
| Male | 3580 | 76.2 | 35174 | 78.7 | 3149 | 74.3 | 17899 | 78.8 |
| Race/Ethnicity | ||||||||
| White | 3807 | 81.0 | 35318 | 79.0 | 3319 | 78.3 | 17501 | 77.0 |
| Black | 576 | 12.3 | 5448 | 12.2 | 463 | 10.9 | 2188 | 9.6 |
| Hispanic | 247 | 5.3 | 2920 | 6.5 | 343 | 8.1 | 2012 | 8.9 |
| Other | 68 | 1.5 | 1018 | 2.3 | 114 | 2.7 | 1013 | 4.5 |
| Census Region | ||||||||
| Northeast | 476 | 10.1 | 6444 | 14.4 | 693 | 16.4 | 5061 | 22.3 |
| Midwest | 1327 | 28.3 | 14202 | 31.8 | 1644 | 38.8 | 8369 | 36.8 |
| South | 2509 | 53.4 | 20557 | 46.0 | 1447 | 34.1 | 6652 | 29.3 |
| West | 386 | 8.2 | 3501 | 7.8 | 455 | 10.7 | 2632 | 11.6 |
| Employee Type | ||||||||
| Hourly | 3415 | 72.7 | 30099 | 67.3 | 3184 | 75.1 | 15297 | 67.3 |
| Salary | 1283 | 27.3 | 14605 | 32.7 | 1055 | 24.9 | 7417 | 32.7 |
| Diagnosed Condition | ||||||||
| ADHD | 14 | 0.3 | 65 | 0.2 | 41 | 1.0 | 147 | 0.6 |
| Anxiety/Depression/Bipolar Disorder | 280 | 6.0 | 1710 | 3.8 | 441 | 10.4 | 1426 | 6.3 |
| Low Back Pain | 1205 | 25.7 | 5103 | 11.4 | 1215 | 28.7 | 3185 | 14.0 |
| Other Back and Neck Pain | 1095 | 23.3 | 5073 | 11.4 | 1100 | 26.0 | 3128 | 13.8 |
| Neuropathic Pain | 489 | 10.4 | 1770 | 4.0 | 310 | 7.3 | 702 | 3.1 |
| Chronic Pain/ Fibromyalgia | 123 | 2.6 | 553 | 1.2 | 200 | 4.7 | 386 | 1.7 |
| Headache | 366 | 7.8 | 1631 | 3.7 | 306 | 7.2 | 789 | 3.5 |
| Nonopioid Use Disorder | 135 | 2.9 | 608 | 1.4 | 110 | 2.6 | 309 | 1.4 |
| Osteoarthritis | 583 | 12.4 | 2101 | 4.7 | 781 | 18.4 | 1526 | 6.7 |
| Diabetes Mellitus | 359 | 7.6 | 2597 | 5.8 | 509 | 12.0 | 2001 | 8.8 |
There was a substantial increase in opioid prescriptions with 10.5% of workers receiving one or more prescriptions in 2003 compared to 18.7% in 2013. Compared to their percentage contribution to the total population, women, hourly workers and workers in the South comprised a greater percentage of those receiving opioids. Workers receiving one or more opioid prescription in each year were also more likely to have comorbid medical conditions (Table 1). Figure 1 illustrates the rise in prescribed opioids, chronic opioid use, and diagnoses of opioid use disorder over the ten-year study period. The increase in opioid prescriptions was statistically significant (p<.0001). There was also a statistically significant increase in chronic opioid prescriptions among workers 0.69% (n=310) in 2003 compared to 2.9% (n=681) in 2013 (p<0.0001). The proportion of workers diagnosed with opioid use disorder increased more than ten-fold from 2003 (n=11, 0.02%) to 2013 (n=67, 0.28%), p<0.0001 (Figure 1). In addition, the proportion of workers prescribed opioids chronically among those prescribed any opioids in a given year nearly tripled in the ten-year period (6.6% in 2003 compared to 16.0% in 2013) (Figure 2).
Figure 1.
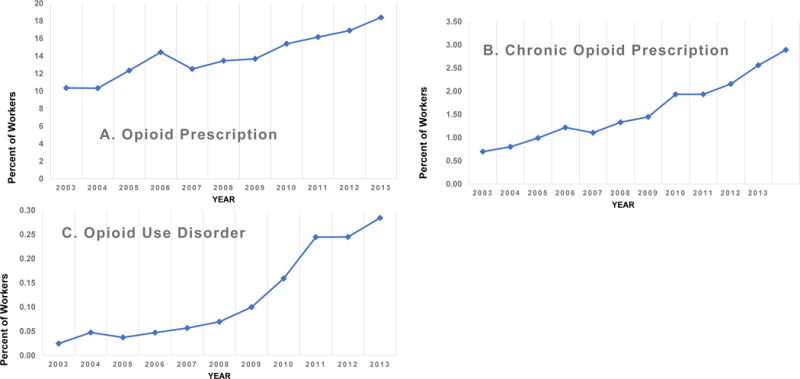
A. Percent of workers enrolled in employer-sponsored health plan prescribed any opioid each year from 2003–2013. B. Percent of workers enrolled in the employer-sponsored health plan prescribed three or more opioids consecutively during each year from 2003–2013. C. Percent of workers enrolled in the employer-sponsored health plan who were diagnosed with opioid use disorder from 2003–2013.
Figure 2.
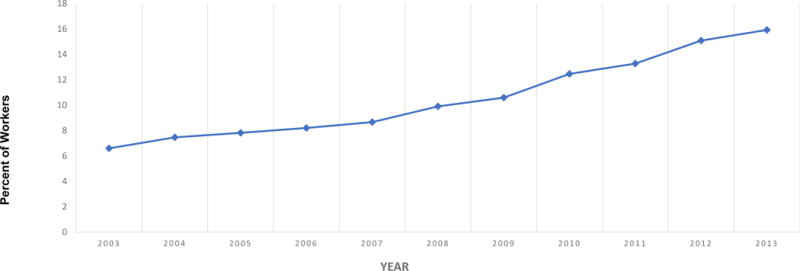
Percent of workers prescribed opioids chronically each year among those prescribed one or more opioid in the same year.
Before adjusting for potential confounding factors among those ever-prescribed opioids, older age workers, whites, hourly workers, and workers in facilities outside of the Northeast had higher odds of being prescribed opioids chronically (Table 2). Workers with a diagnosis of depression/anxiety, low back pain, other back and neck pain, neuropathic pain, headache, osteoarthritis, and diabetes all had higher odds of being prescribed opioids chronically (Table 2). Year was also strongly associated with chronic opioid prescription, with workers having more than a 3-fold odds of being prescribed opioids chronically in 2013 compared to 2003 (OR=3.23, 95% CI: 2.63–3.96).
Table 2.
Predictors of Chronic Opioid Prescription Among Workers Prescribed Opioids, 2003–2013
| Covariate | Unadjusted Model* | Adjusted Model* | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| OR | 95% CI | OR | 95% CI | |||
| Age | ||||||
| 26 – 35 (vs <26) | 1.52 | 1.01 | 2.28 | 1.44 | 1.02 | 2.04 |
| 36 – 45 (vs <26) | 1.89 | 1.29 | 2.78 | 1.67 | 1.19 | 2.34 |
| 46 – 55 (vs <26) | 2.40 | 1.65 | 3.50 | 1.82 | 1.30 | 2.53 |
| >55 (vs <26) | 2.65 | 1.81 | 3.87 | 1.67 | 1.19 | 2.35 |
| Male (vs female) | 1.03 | 0.94 | 1.13 | 1.11 | 1.00 | 1.22 |
| Race/Ethnicity | ||||||
| Black (vs White) | 0.66 | 0.57 | 0.76 | 0.64 | 0.55 | 0.75 |
| Hispanic (vs White) | 0.57 | 0.47 | 0.69 | 0.60 | 0.49 | 0.74 |
| Other race (vs White) | 0.54 | 0.38 | 0.76 | 0.55 | 0.38 | 0.81 |
| Salary (vs hourly) | 0.74 | 0.66 | 0.82 | 0.74 | 0.67 | 0.82 |
| Census Region | ||||||
| Midwest (vs Northeast) | 1.77 | 1.53 | 2.05 | 1.63 | 1.40 | 1.89 |
| South (vs Northeast) | 1.43 | 1.24 | 1.65 | 1.65 | 1.42 | 1.92 |
| West (vs Northeast) | 1.67 | 1.38 | 2.02 | 1.83 | 1.51 | 2.22 |
| Comorbid Conditions | ||||||
| ADHD | 1.10 | 0.52 | 2.33 | 1.09 | 0.67 | 1.78 |
| Depression, Anxiety, Bipolar Disorder | 1.32 | 1.10 | 1.58 | 1.30 | 1.13 | 1.50 |
| Low Back Pain | 1.78 | 1.60 | 1.97 | 1.55 | 1.41 | 1.70 |
| Other Back and Neck Pain | 1.79 | 1.60 | 1.99 | 1.46 | 1.33 | 1.62 |
| Neuropathic Pain | 1.53 | 1.31 | 1.80 | 1.43 | 1.26 | 1.63 |
| Chronic Pain and Fibromyalgia | 1.47 | 1.12 | 1.92 | 1.28 | 1.06 | 1.56 |
| Headache | 1.30 | 1.09 | 1.55 | 1.26 | 1.09 | 1.46 |
| Nonopioid Use Disorder | 1.28 | 0.96 | 1.70 | 1.27 | 1.02 | 1.59 |
| Osteoarthritis | 1.90 | 1.68 | 2.15 | 1.67 | 1.50 | 1.86 |
| Diabetes Mellitus | 1.31 | 1.11 | 1.54 | 1.11 | 0.96 | 1.28 |
| Year | ||||||
| 2004 (vs 2003) | 1.04 | 0.77 | 1.39 | 0.99 | 0.78 | 1.27 |
| 2005 (vs 2003) | 1.23 | 0.96 | 1.56 | 1.16 | 0.95 | 1.43 |
| 2006 (vs 2003) | 1.38 | 1.10 | 1.73 | 1.28 | 1.05 | 1.56 |
| 2007 (vs 2003) | 1.25 | 0.98 | 1.59 | 1.19 | 0.97 | 1.47 |
| 2008 (vs 2003) | 1.63 | 1.29 | 2.05 | 1.58 | 1.29 | 1.92 |
| 2009 (vs 2003) | 1.57 | 1.23 | 2.01 | 1.43 | 1.16 | 1.78 |
| 2010 (vs 2003) | 1.90 | 1.50 | 2.41 | 1.71 | 1.39 | 2.10 |
| 2011 (vs 2003) | 2.06 | 1.65 | 2.58 | 1.87 | 1.53 | 2.28 |
| 2012 (vs 2003) | 2.57 | 2.07 | 3.19 | 2.34 | 1.93 | 2.83 |
| 2013 (vs 2003) | 3.23 | 2.63 | 3.96 | 2.90 | 2.41 | 3.48 |
Analyzed using multivariate marginal (population-average) generalized linear models using generalized estimating equations (GEE)
After adjusting for age, sex, race, wage type, geographic region, and comorbid conditions, significant predictors of chronic opioid prescriptions included age, male sex, white race, hourly wage, geographic region outside the Northeast, comorbid pain and psychiatric conditions, and year. The odds of receiving opioids chronically increased with age. Compared to those less than 26 years old, all other age groups had elevated odds of chronic opioid prescription, with those between the ages of 46–55 (OR= 1.82, 95% CI:1.30–2.53) showing the highest odds. Male compared to female workers prescribed opioids were 11% more likely to receive them chronically (OR=1.11, 95% CI: 1.00–1.22). Minorities had statistically significantly lower odds of receiving opioids chronically, with a 26–45% lower likelihood. Salaried workers similarly had lower odds of being prescribed opioids chronically compared to hourly wage earners (OR= 0.74, (95% CI: 0.67–0.82). Workers outside of the Northeast region had higher odds of being prescribed opioids chronically. Workers with comorbid psychiatric and pain conditions remained at higher odds of receiving opioids chronically after controlling for other factors. The conditions with the strongest relationship included osteoarthritis (OR= 1.67, 95% CI: 1.50–1.86), low back pain (OR= 1.55, 95% CI: 1.41–1.70), other back and neck pain (OR= 1.46, 95% CI: 1.33–1.62), and neuropathic pain (OR=1.43, 95% CI: 1.26–1.63). Diabetes Mellitus and ADHD were not associated with chronic opioid prescriptions in the adjusted model. Those diagnosed with non-opioid substance use disorder had 27% higher odds of receiving a chronic opioid prescription (OR= 1.27 CI: 1.02–1.59). Year remained the strongest predictor of chronic opioid prescription in the adjusted model. Workers had higher odds of being prescribed opioids chronically in later years compared to 2003, with the likelihood of chronic prescriptions increasing steadily each year until 2013 (OR= 2.90, 95%CI: 2.41–3.48) (Table 2).
Discussion
Ours is the first study of which we are aware to describe the prevalence of opioid prescriptions among a working cohort in the span of opioid epidemic. The prevalence of non-Worker’s Compensation opioid prescriptions increased each year from 2003 to 2013 in this privately insured national industrial cohort. The diagnosis of opioid use disorder increased 10-fold over the ten-year period. Older age, white, and hourly workers were more likely to receive chronic opioid prescriptions. While female workers were more likely to receive opioids, men were more likely to receive opioids chronically. Workers outside of the Northeast were also more likely to receive opioid prescriptions chronically. Comorbid behavioral health conditions and multiple pain conditions including low back pain and osteoarthritis were associated with chronic opioid prescription. When controlling for demographic factors and comorbid conditions, year remained the strongest predictor of chronic opioid prescriptions, with a steady increase in the odds of chronic opioid prescription over the ten-year period. Opioid prescribing leveled off nationally in 2010 and began to taper in 2012 (1), however, in this study, we found a steady increase in opioid prescriptions and chronic prescribing through 2013.
There were recession-related plant closures over the study period, which would result in job loss. Each year, we described an employed and privately insured cohort. Unemployed and uninsured individuals are more likely to misuse opioids and more likely to be diagnosed with opioid use disorder(13). This working cohort, however, may have experienced recession-related financial stress. Psychologic distress has been associated with longer duration of opioid prescription for low back pain, a common diagnosis among industrial workers (25).
A recent national survey demonstrated that 38% of American adults, and 35% of those who were employed full-time received an opioid prescription in 2015, (13) which is a much greater proportion than we found in our population. We described the majority (80–87%) of the working population who elected employer-sponsored private insurance, and do not know the insurance status of the remaining 13–20% of the workforce. Results from the national survey demonstrated that individuals receiving Medicaid benefits had a higher prevalence of opioid prescriptions, while those who were uninsured had a lower proportion of opioid prescriptions. It is unlikely that our results would change differentially if we were able to describe the full working population. The cross-sectional study found similar predictors of opioid use as found in our study such as older age, non-Hispanic white race, and lack of college education. Males were also more likely to meet criteria for misuse (13). The difference in opioid prescription prevalence is likely partially explained by an underestimate of opioid use in our study.
Our study is limited in that we have relied on employer-sponsored health claims data to estimate opioid use. We did not have record of Workers’ Compensation claims or an estimate of recreational drug use. According to a recent survey, 16.1% of workers aged 18–25 and 6.5% of workers aged 26 and older participate in non-medical use of prescription pain relievers (26). In addition, we analyzed each year in cross-sections, and therefore, may have misclassified some chronic prescriptions as non-chronic. Our study, therefore, likely underestimates the prevalence of chronic opioid use among workers. Strengths of our study include the large size of the cohort and the geographic span of the population, which increases the generalizability of our findings. We also provide a view of non-Workers’ Compensation prescription claims for a working population, which is an aspect often overlooked. We demonstrated that workers, while generally healthier than the total population, (27) are also susceptible to the epidemic of opioid prescribing. Potential risks of chronic opioid prescribing that is unique to workers includes lost work time and disability (5, 7, 8, 15). Our study is limited that we were not able to estimate dose or strength of prescription, which would give a better perception of complication risk.
Opioid prescribing for industrial workers by private clinicians increased substantially from 2003 to 2013. Occupational medicine clinicians should not only consider risk factors for misuse when prescribing opioids, but should also consider occupational hazards. Opioids should not be prescribed in workers operating vehicles or heavy machinery or in those whose jobs are highly cognitive (20). Workers may obtain prescription opioids from multiple sources including private clinicians, and therefore occupational health providers should reference prescription monitoring programs.
Supplementary Material
Acknowledgments
Funding Sources/Conflict of interest statement
Mellisa Pensa was supported by a National Institute of Occupational Health and Safety (NIOSH) training grant (1T01 OH008607-08). during the period the research was conducted. She is currently an instructor in the Yale School of Medicine and Associate Director of the Yale Occupational and Environmental Medicine Program. She has no potential conflicts of interest.
Deron Galusha and Linda Cantley were supported by grants from the National Institute on Aging (Disease, Disability and Death in an Aging Workforce, NIH/NIA, 2R01 AG026291 11A and from the National Institute of Occupational Health and Safety (Occupational Exposure to PM2.5 and Cardiovascular Disease (CVD), NIOSH, 5R01 009939 06). They have no potential conflicts of interest. The study sponsor had no role in the study design, collection, analysis, and interpretation of data, writing the report, or the decision to submit the report for publication.
Footnotes
Financial Disclosures:
Mellisa Pensa, Deron Galusha, and Linda Cantley haves no financial disclosures.
References
- 1.Guy GP, Zhang K, Bohm MK, Losby J, Lewis B, Young R, Murphy LB, Dowell D. Vital Signs: Changes in Opioid Prescribing in the United States, 2006–2015. MMWR Morbidity and mortality weekly report. 2017;66:697–704. doi: 10.15585/mmwr.mm6626a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rudd RA, S P, David F, Scholl L. Increases in Drug and Opioid-Involved Overdose Deaths — United States, 2010–2015. MMWR Morbidity and mortality weekly report. 2016;65:1445–1452. doi: 10.15585/mmwr.mm655051e1. [DOI] [PubMed] [Google Scholar]
- 3.U.S. Department of Labor: Bureau of Labor Statitics. Employer-reported workplace injuries and illnesses, 2015. Washington, D.C.: Bureau of Labor Statistics; 2016. [Google Scholar]
- 4.Webster BS, Cifuentes M, Verma S, Pransky G. Geographic variation in opioid prescribing for acute, work-related, low back pain and associated factors: a multilevel analysis. Am J Ind Med. 2009;52:162–171. doi: 10.1002/ajim.20655. [DOI] [PubMed] [Google Scholar]
- 5.Busse JW, Ebrahim S, Heels-Ansdell D, Wang L, Couban R, Walter SD. Association of worker characteristics and early reimbursement for physical therapy, chiropractic and opioid prescriptions with workers’ compensation claim duration, for cases of acute low back pain: an observational cohort study. BMJ Open. 2015;5:e007836. doi: 10.1136/bmjopen-2015-007836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Franklin GM, Stover BD, Turner JA, Fulton-Kehoe D, Wickizer TM. Early opioid prescription and subsequent disability among workers with back injuries: the Disability Risk Identification Study Cohort. Spine (Phila Pa 1976) 2008;33:199–204. doi: 10.1097/BRS.0b013e318160455c. [DOI] [PubMed] [Google Scholar]
- 7.Tao XG, Lavin RA, Yuspeh L, Weaver VM, Bernacki EJ. The association of the use of opioid and psychotropic medications with workers’ compensation claim costs and lost work time. J Occup Environ Med. 2015;57:196–201. doi: 10.1097/JOM.0000000000000333. [DOI] [PubMed] [Google Scholar]
- 8.Volinn E, Fargo JD, Fine PG. Opioid therapy for nonspecific low back pain and the outcome of chronic work loss. Pain. 2009;142:194–201. doi: 10.1016/j.pain.2008.12.017. [DOI] [PubMed] [Google Scholar]
- 9.Stover BD, Turner JA, Franklin G, et al. Factors associated with early opioid prescription among workers with low back injuries. The journal of pain : official journal of the American Pain Society. 2006;7:718–725. doi: 10.1016/j.jpain.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 10.Chaparro LE, Furlan AD, Deshpande A, Mailis-Gagnon A, Atlas S, Turk DC. Opioids compared to placebo or other treatments for chronic low-back pain. Cochrane Database of Systematic Reviews. 2013 doi: 10.1002/14651858.CD004959.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chou R, Deyo R, Devine B, Hansen R, Sullivan S, Jarvik JG, Blazina I, Dana T, Bougatsos C, Turner J. In: The Effectiveness and Risks of Long-Term Opioid Treatment of Chronic Pain. Quality AfHRa, editor. Rockville, MD: Agency for Healthcare Research and Quality; 2014. [DOI] [PubMed] [Google Scholar]
- 12.Noble M, Treadwell JR, Tregear SJ, et al. Long-term opioid management for chronic noncancer pain. Cochrane Database of Systematic Reviews. 2010 doi: 10.1002/14651858.CD006605.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM. Prescription opioid use, misuse, and use disorders in u.s. adults: 2015 national survey on drug use and health. Annals of Internal Medicine. 2017 doi: 10.7326/M17-0865. [DOI] [PubMed] [Google Scholar]
- 14.Vowles KE, McEntee ML, Julnes PS, Frohe T, Ney JP, van der Goes DN. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain. 2015;156:569–576. doi: 10.1097/01.j.pain.0000460357.01998.f1. [DOI] [PubMed] [Google Scholar]
- 15.Johnston SS, Alexander AH, Masters ET, et al. Costs and Work Loss Burden of Diagnosed Opioid Abuse Among Employees on Workers Compensation or Short-term Disability. J Occup Environ Med. 2016;58:1087–1097. doi: 10.1097/JOM.0000000000000865. [DOI] [PubMed] [Google Scholar]
- 16.Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL. Societal Costs of Prescription Opioid Abuse, Dependence, and Misuse in the United States. Pain Medicine. 2011;12:657–667. doi: 10.1111/j.1526-4637.2011.01075.x. [DOI] [PubMed] [Google Scholar]
- 17.Rice JB, Kirson NY, Shei A, et al. Estimating the costs of opioid abuse and dependence from an employer perspective: a retrospective analysis using administrative claims data. Appl Health Econ Health Policy. 2014;12:435–446. doi: 10.1007/s40258-014-0102-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shafer LA, Raymond C, Ekuma O, Kraut A. The impact of opioid prescription dose and duration during a Workers Compensation claim, on post-claim continued opioid use: A retrospective population-based study. American journal of industrial medicine. 2015;58:650–657. doi: 10.1002/ajim.22453. [DOI] [PubMed] [Google Scholar]
- 19.Becker WC, Fenton BT, Brandt CA, et al. Multiple Sources of Prescription Payment and Risky Opioid Therapy Among Veterans. Med Care. 2017;55(Suppl 7 Suppl 1):S33–S36. doi: 10.1097/MLR.0000000000000722. [DOI] [PubMed] [Google Scholar]
- 20.Hegmann KT, Weiss MS, Bowden K, et al. ACOEM practice guidelines: opioids and safety-sensitive work. Journal of occupational and environmental medicine. 2014;56:e46–53. doi: 10.1097/JOM.0000000000000237. [DOI] [PubMed] [Google Scholar]
- 21.Von Korff M, Saunders K, Thomas Ray G, et al. De facto long-term opioid therapy for noncancer pain. The Clinical journal of pain. 2008;24:521–527. doi: 10.1097/AJP.0b013e318169d03b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mosher HJ, Richardson KK, Lund BC. The 1-Year Treatment Course of New Opioid Recipients in Veterans Health Administration. Pain Medicine. 2016;17:1282–1291. doi: 10.1093/pm/pnw058. [DOI] [PubMed] [Google Scholar]
- 23.Edelman EJ, Gordon K, Becker WC, et al. Receipt of opioid analgesics by HIV-infected and uninfected patients. Journal of general internal medicine. 2013;28:82–90. doi: 10.1007/s11606-012-2189-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weisberg DF, Gordon KS, Barry DT, et al. Long-term Prescription of Opioids and/or Benzodiazepines and Mortality Among HIV-Infected and Uninfected Patients. Journal of acquired immune deficiency syndromes (1999) 2015;69:223–233. doi: 10.1097/QAI.0000000000000591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deyo RA, Smith DH, Johnson ES, et al. Opioids for back pain patients: primary care prescribing patterns and use of services. Journal of the American Board of Family Medicine : JABFM. 2011;24:717–727. doi: 10.3122/jabfm.2011.06.100232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Substance Abuse and Mental Health Services Administration. Results from the 2014 National Survey on Drug Use and Health: Detailed tables. 2015 [PubMed] [Google Scholar]
- 27.Commentary for the Then and Now Forum: The Healthy Worker Effect. Journal of occupational and environmental medicine. 2017;59:335–346. doi: 10.1097/JOM.0000000000000979. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


