Abstract
Objective/Background
Approximately 400,000 adolescents give birth in the US annually. Although one-half experience depressive symptoms, less than 25% comply with referrals for depression evaluation and treatment. The current study tested the effectiveness of an internet based depression intervention on seeking depression treatment.
Methods
Based upon the Theory of Planned Behavior (TPB), the intervention included vignettes, questions and answers, and resources. Before the intervention, immediately after the intervention, and two-weeks later the adolescent mothers (n=151) answered questions related to TPB variables and depression treatment. Data were compared to adolescent mothers (n=138) in the control group. Data were collected in community organizations or home visits for the control group. Adolescent mothers in the intervention group answered questions and completed the intervention from a computer of their choice.
Results
The adolescents were primarily African American (89.2%); less than high school educated (51.7%); had given birth in last year (97.1%); with a mean age 18.2 years. The intervention led to significant changes in attitude, perceived control, intention to seek mental health treatment, and actually seeking depression treatment.
Conclusions/Discussion
Untreated postpartum depression dramatically impacts a mother’s relationships with her child, her functioning at work and school, health care seeking behaviors, mothering skills, and her development as well as the development of her child. An Internet based depression intervention is an inexpensive method to increase rates of depression treatment.
Keywords: adolescent, depression, internet, intervention
National experts (Gaynes et al., 2005; Williams, O’Connor, Eder, & Whitlock, 2009) agree that both adolescents and new mothers have inadequate rates of depression evaluation and treatment. When a young woman is both an adolescent and a new mother, she is particularly vulnerable to depression. High rates of depressive symptoms in adolescent mothers have been identified, with rates of symptoms averaging 50% (Logsdon, Birkimer, Simpson, & Looney, 2005; Logsdon, Ziegler, Hertweck, & Pinto-Foltz, 2008). However, the rates of adherence to referrals for depression evaluation and treatment in adolescent mothers have been unacceptably low, ranging from 0 to 25% (Logsdon et al., 2008; Logsdon, Usui, Pinto-Foltz, & Rakestraw, 2009; Logsdon, Hines-Martin, & Rakestraw, 2009). The prevailing practice of providing written educational materials on depression and treatment at hospital discharge or in clinic/private practice waiting rooms, as well as the less common procedure of screening for depression and referring positive screens for evaluation and treatment, are simply not resulting in sufficient rates of depression evaluation and treatment in adolescent mothers. National experts recommend that new and innovative strategies are needed to address this important national health issue of depression in adolescent mothers (Gaynes et al., 2005; McPeak, Sandrock, Spector, & Pattishall, 2015; Williams et al., 2009). Phipps and colleagues reported the results of one randomized clinical trial of an intervention provided to pregnant adolescents during pregnancy to prevent postpartum depression (Phipps, Raker, Ware, & Zlotnick, 2013). Other than a pilot study conducted by our research team, few investigators have developed specific interventions that focus on overcoming barriers to depression treatment in adolescent mothers after delivery (Logsdon, Foltz, Stein, Usui, & Josephson, 2010).
A plethora of classic, international research studies have demonstrated that mothering is adversely impacted in women with postpartum depression (Logsdon, Wisner, Pinto-Foltz, 2006), including impaired maternal infant interaction (Beck, 1995), diminished gratification in the maternal role (Killien, 1998), and lower feelings of self-efficacy (Frowman & Owen, 1990). Maternal depression has been shown to have negative association with adverse child outcomes including socio-emotional, cognitive, and behavioral development (Kingston, Tough, & Whitfield, 2012; Maughan, Cicchetti, Toth, & Rogosch, 2007). The outcomes are cumulative when depression goes untreated (Brennan, Andersen, Hammen, & Bor, 2000; National Institute of Child Health and Human Development, 1999). The effects go well beyond interfering with early maternal-infant bonding and interactions and have been shown to be associated with poor school readiness and self-regulation (Brennan, Andersen, Hammen, & Bor, 2000; Campbell, Matestic, von Stauffenberg, Mohan, & Kirchner, 2007). The effects of depression on early maternal-infant interactions are further complicated in adolescent mothers due to deficits in executive functioning associated with a prefrontal cortex that is still developing (Chico, Gonzalez, Ali, Steiner, & Fleming, 2014; McPeak et al., 2015). These data suggest that it is critical that all mothers, but especially adolescent mothers, receive early screening and treatment for depressive symptoms.
Numerous clinical trials have determined that depressive symptoms and overall functioning improve with depression treatments such as therapy, antidepressants, and psycho-educational interventions (Dennis & Stewart, 2004; Gjerdingen, 2003; O’Hara, Stuart, Gorman, & Wenzel, 2000). In a secondary data analysis, Logsdon and colleagues (Logsdon, Wisner, & Hanusa, 2009) investigated whether mothering behaviors also improved with antidepressant treatment in women with postpartum depression. A subset of women (n=27) from a randomized clinical trial (double-blind eight week trial of nortriptyline compared with sertraline) completed outcome measures of mothering. The two antidepressants were equally efficacious in improving maternal gratification and self-efficacy. Treatment of depression is critical to improve public health, particularly in vulnerable adolescent mothers and their offspring, but it is important to address barriers to treatment.
Internet-based interventions for depression have been successful in overcoming barriers to treatment including the social stigma of seeking depression treatment in adolescents (Wisdom, Clarke, & Green, 2006). For example, a website in Australia (Blue Pages) provided an education intervention consisting of evidence-based information on depression and treatment. The reduction in mean scores on the Center for Epidemiologic Studies of Depression screening scale was 3.0 (95% confidence interval 0.6 to 5.2) (Christensen, Griffiths, & Jorm, 2004). Similarly, a self-directed Internet intervention for depression delivered as part of a high school curriculum was successful in improving depression symptoms in adolescent girls compared to a control group (n=157), but rates of completion of the intervention were low. Feedback on the intervention indicated that the amount of material, the age-appropriateness of the themes and examples and time available for access to the intervention were problematic (O’Kearney, Kang, Christensen, & Griffiths, 2009).
Use of Internet and social media are almost ubiquitous in adolescents and young adults, and the rates of use continue to climb. More than half of adolescents access the Internet at least daily, including those of low income, and rates vary little by race/ethnicity (Lenhart, Purcell, Smith, & Zickuhr, 2010). In the health care system, use of Internet interventions to promote behavior change has the advantage of reaching and the impacting the health of many people (Bennett & Glasgow, 2009). The low implementation costs and high potential for sustainability are promising features in addressing pervasive health problems in the U.S. (Bennett et al., 2010; Bennett et al., 2012; McNeill, Viswanath, Bennett, Puleo, & Emmons, 2007), such as obesity and depression. It is well-established that a large percentage of low-income and ethnically diverse individuals have access to the Internet (Bleakley, Berzel, VanDevanter, & Messeri, 2004; Klnd, Huang, Farr, & Pomerantz, 2005), particularly by smart phones as reported by the Pew Research Center (Lenhart et al., 2010).
In general, adolescents are an underserved population with many unmet health needs (National Academy of Sciences, 2009), and this is particularly true for adolescent mothers. Prior to our study, use of an Internet-based depression intervention had not been tested with adolescent mothers or in adolescents who reside outside of urban areas, even though both groups may differ from other adolescents in important ways. Though rates of mental illness in non-urban populations are comparable to urban populations, few people in rural areas seek mental health treatment (Hauenstein et al., 2007; Murry, Heflinger, Suiter, & Brody, 2011). There is also a strong propensity for self-reliance and a preference for self-managing health problems in rural populations (Murry et al., 2011). Thus, there is a gap in scientific knowledge related to the effectiveness of Internet health interventions with adolescent mothers, particularly those residing in non-urban areas. This study addressed that scientific gap by testing a tailored intervention based upon the Theory of Planned Behavior (TPB; Ajzen, 1991). Prominent researchers have recommended the need for trials of innovative interventions to address depression in adolescent mothers (Yozwiak, 2010).
Theoretical Support
The TPB (Ajzen, 1991; Ajzen, 1998) has been used extensively to predict health behavior. TPB states that an individual’s behavior is principally determined by behavioral intention, and that intention is predicted by perceived behavioral control, subjective norms, and attitudes. An individual engages in a behavior that she evaluates positively (attitude), where she perceives social pressure or peer acceptance to do so (subjective norms), and when she believes that it is achievable (perceived behavioral control). Consistency of message, strong evidence, and tailoring of the message to diverse groups are recommended (Fishbein, Von Haeften, & Appleyard, 2001). TPB has been successfully used to frame research with samples of adolescents related to such issues as decisions regarding sexual behavior (Bishop, 2002; Gilllmore et al., 2004), intention to breastfeed (Swanson, Power, Kaur, Carter, & Shepherd, 2006), drug prevention practices (Stephenson, Quick, Atkinson, & Tschida, 2005), HIV/AIDS prevention (Kinsler, Sneed, Morisky, & Ang, 2004), susceptibility to smoking (Unger, Rohrbach, Howard-Pitney, Ritt-Olson, & Mouttapa, 2001), as well as beliefs and attitudes associated with the intention to accept a diagnosis of depression (Van Voorhees et al., 2006) and to use social networking (Baker & White, 2011). In developed countries, beliefs and attitudes toward treatment are thought to be the critical determinants of mental health seeking behavior, as opposed to access to care (Fortney, Rost, & Zhang, 1998; Kessler et al., 1997; Leaf et al., 1988), making the TPB an appropriate framework for this study.
Research Questions
RQ1: What is the association between exposure to the Internet-based depression intervention and study outcomes (attitude and subjective norms towards depression and depression treatment, perceived control, intention to seek depression evaluation and treatment), when controlling for baseline measures (pre-test)?
RQ1 (a): Are changes in outcomes dose related?
RQ2: What is the association between use of the Internet-based depression intervention and actual seeking of depression evaluation and treatment, when controlling for baseline depression symptoms and county?
RQ3: What is the association between intention to seek depression treatment and actual seeking of treatment, when controlling for baseline depression symptoms?
Preliminary Studies
Over the past 10 years our research team has completed and published several research studies with adolescent mothers that have provided a strong foundation for the current study. A summary of findings from preliminary studies follows.
Barriers to depression treatment in low-income adolescent mothers
This study explored barriers to depression treatment in low-income, unmarried, adolescent mothers in a southern, urban area of the United States. The authors utilized a phenomenological approach and focus group methodology. Participants (n = 9) were enrolled in a teen parent program, an option of the public school system. The metaphor of a merry-go-round emerged from the data and represented the ups and downs that the adolescent mothers experience as they struggle to adjust to the role of mother. The adolescent mothers did not realize their feelings could be labeled as depression, and they did not know how to seek assistance from professionals for these feelings. Thus, depression literacy was a profound barrier to depression treatment (Logsdon et al., 2009).
Intention to seek mental health treatment in adolescent mothers
The aims of this study were to determine the efficacy of the Theory of Reasoned Action in predicting intention to seek depression treatment in adolescent mothers (n=64). Results indicated that subjective norms, but not attitude, was a significant predictor of intention to seek depression treatment in adolescent mothers (F =4.82; p =.00; R2=.14). Thus, the peers, family culture and values of the teen mother influenced her intention to seek mental health treatment. Findings from this study, as well as support from the literature, established the need for a culturally sensitive educational intervention related to depression and depression treatment that includes messages that family and peers find mental health treatment to be acceptable (Logsdon et al, 2009).
Telephone based depression care management intervention for adolescent mothers
This Phase 1 clinical trial combined qualitative and quantitative methods to modify a collaborative care, telephone based, depression care management intervention for adolescent mothers, and to determine the acceptability, feasibility, and initial efficacy of the intervention in a sample of adolescent mothers (n=97) who were recruited from an adolescent parent program. Our findings indicated that 25% of adolescent mothers who participated in the intervention received depression treatment. Feasibility and acceptability of the intervention were limited by the use of an adult to deliver the message, attitude and subjective norms related to depression and depression treatment, and challenges related to when the adolescents were free to receive telephone calls. Many of the adolescents were employed, attended school full time, and cared for their infants. The study demonstrated that an approach to overcoming barriers to depression treatment different from telephone based depression care management is needed for low-income adolescent mothers (Logsdon et al., 2010). An intervention delivered through the internet and that resonates with adolescent mothers has the potential to overcome time barriers identified in this study. Such an approach has been successful in the past in changing subjective norms in adolescents (Norman & Skinner, 2007; Rotheram-Borus, O’Keefe, Kracker, & Foo, 2000).
Use of Social Media by (Urban and Rural) Adolescent Mothers
Using a cross-sectional design, a convenience sample of urban (n=200) as well as a small sample of rural adolescent mothers (n=15), completed surveys at 1–3 days postpartum on a mother-baby unit of a university hospital or in the community during home visits with nurses in order to determine their preferred health care resources and use of social media to obtain health information. All adolescent mothers were socioeconomically disadvantaged. No differences existed between urban and rural adolescent mothers (all p-values >0.05). Adolescent mothers received the most health information from the following: Parents (69%); doctors/nurses (69%); internet (64%); and parents of friends (42%). Preferences for sources of health information included family (58%), internet (61%), and health care professionals (92%). Twenty five percent of adolescents searched for health information on the Internet 1–2 days per week; 22% had received health information from Facebook. Adolescent mothers used media extensively for communication. Fifty percent of the sample accessed a computer several times per day. The Internet was most frequently accessed through computers at school (81%), the library (97%), and through cell phones (72%). Using images of parents and health care providers to relay the health information is recommended (Logsdon et al., 2014; Logsdon, Mittelberg, & Myers, 2015).
Pilot Study of Intervention for this Study
In a five step process, a product design team of interdisciplinary researchers collaborated with community partners to create and test a prototype website for an Internet-based depression intervention. The approach to constructing the website was based upon Instructional Design Theory. The iterative process involved the following steps: (1) Focus groups of adolescent mothers provided information on what messages and visual images would make an adolescent mother with depressive symptoms seek depression treatment (develop brand); (2) Development of prototype website; (3) Focus groups of adolescent mothers tested the images and message; (4) Revision of website based upon feedback; and (5) Testing of website with adolescent mothers. Feedback on the website indicated that it was easy to use (77%), which is in the highly acceptable range of product usability in the commercial/business world (Bangor, Kortum, & Miller, 2008). Attitudes related to depression and depression treatment improved after viewing the website (p=.023). Though study results were promising, the impact of the website on subsequent treatment for depression was not determined (Logsdon et al., 2013). In addition, this pilot study was limited to adolescent mothers (n=136) who lived in an urban area and used the website at school. Thus, generalizability of study findings should be tested in a more diverse group, and access to the website needs to be tested in contexts outside of schools.
In summary, preliminary work strengthened our commitment to investigate how to assist adolescent mothers with depressive symptoms to seek and receive depression evaluation and treatment to improve their health and functioning and lessen the impact of depression on their infant. The purpose of this study is to provide information on how an Internet-based depression intervention can achieve those goals.
Methods
Study Design
A pre-test post-test design was used.
Sample
Adolescent mothers from 20 urban, suburban and rural counties in Kentucky were included in the study, 10 intervention group counties and 10 comparison group counties. The counties were matched based upon comparable racial/socioeconomic composition of counties and the number of adolescent births.
A convenience sample was used. Eligibility criteria for the study include (1) adolescent mother, 13–21 years of age; (2) delivery of a living child within last 12 months; and (3) infant lives with adolescent. Screening questions for eligibility criteria were completed before potential participants in the intervention group were allowed to enroll in the Internet-based depression intervention. For the comparison group, staff from community agencies determined eligibility of potential participants and then invited them to participate in the study.
Retention
The intervention group was sent an email reminder to complete the 2-week post-test. The staff from the community agency administered the second set of study instruments to the comparison group in their homes. Based upon our previous longitudinal study (Logsdon et al., 2013), we estimated that 30% of the eligible/willing participants would be lost to follow-up. We increased the amount of the stipend ($25) for completion of the second posttest to serve as an incentive. Our Research and Advisory Board has previously helped our research team to determine the amount of study stipend that is appropriate but not coercive.
Power Analysis for Sample Size
Based on data from the CDC National Vital Statistics annual birth rate, we estimated that there would be 3464 adolescent mothers that met study criteria (n = 2001 in the intervention counties, n = 1463 in the comparison counties). The intervention counties have a significantly larger number of adolescent mothers because Metro Louisville/Jefferson County was included in the intervention group, and this is the largest city/county (in population) in the state of Kentucky.
We expected 200 adolescent mothers to enroll in the intervention and complete the first posttest. Based upon our previous longitudinal study (Logsdon & Gohmann, 2008), we estimated that 30% of the eligible/willing participants would be lost to follow-up. As a result, we anticipated that data from 140 participants would be available for analysis from the intervention group. We expected a comparable number of participants in the comparison group. Power calculations were based on the anticipated total sample size (n=280) that would be available for complete analysis
Procedures
Data were collected from November 2013–March 2016. The study was approved by the university human studies protection program and by human studies review groups for each community agency. For the comparison group, data were collected by subcontracts with community agencies that provided voluntary home visitation to pregnant women and new parents to promote safe environments for the optimal growth and development of children. Staff from the counties in the comparison group recruited adolescent mothers, explained the research study and preamble, distributed the instruments, and provided stipends to study participants.. This process was repeated two weeks later. Adolescent mothers completed instruments during home visits with staff from the community organization.
Study procedures were included in a manual that was provided to each community agency (comparison group) to ensure fidelity to study procedures. The manual outlined the processes of communication, training, problem solving, and evaluation. In addition, the research team provided a one-hour orientation session to each agency, and a member of the research team assessed fidelity of study procedures two times for each community agency. Fidelity ranged from 92–95%, and further orientation was provided to correct any deviations from study procedures.
Adolescent mothers in the intervention group were recruited from community agencies in the 10 intervention counties by the research staff. Upon arriving at the website for the study intervention, using a computer of her choice, the adolescent mother read the study preamble and proceeded to the pretest. After completing the pretest, she viewed the intervention. After viewing each section of the website, the adolescent mother was instructed to complete the first post-test. She was not allowed to take the post-test until all sections of the intervention were viewed. At the completion of the post-test, the adolescent mother was awarded an electronic gift certificate for purchases at a retail store, which was sent to her email address. This method has been used with adolescents in other studies to maintain anonymity (Koo & Skinner, 2005), and our other studies with adolescent mothers have established that gift certificates to retail stores are their preferred stipends. At the end of two weeks, she was instructed by email to return to the website and complete the second posttest. Again, at the completion of the posttest she was awarded an electronic gift certificate for purchases at a retail store, which was sent to her email address.
Participants in each group received a $15 stipend for completing time 1 instruments. They received a $25 stipend for completing time 2 instruments.
Intervention
The purpose of the Internet intervention was to persuade adolescent mothers with symptoms of depression to seek and receive depression evaluation and treatment. Internet-delivered interventions have been shown to effectively change behavior (Steele, Mummery, & Dwyer, 2009). The Internet-based depression intervention consisted of the following components: Video Vignettes, Community Resources, and Answers to Common Questions. The homepage embedded Video Vignettes of other adolescent mothers describing their experience with depression and how they successfully sought depression treatment. This component was designed to decrease stigma about depression and to increase normative beliefs about seeking treatment and increase attitudes about the efficacy of treatment, leading to changes in Attitudes and Subjective Norms. After reviewing the video vignettes, the user selected the other website components by clicking on a tab at the top of the website. The Resources component consisted of county and national resources for pregnant and parenting adolescent mothers to include referrals for counseling services and suicide and child abuse prevention hotlines. This component was designed to increase Perceived Behavioral Control by facilitating opportunities to seek depression treatment. The “Common Questions” listed ten questions that are commonly asked about postpartum depression and mental health treatment, including information about medication, counseling, and the range of feelings that teen mothers may experience in the postpartum period. This component is designed to increase positive attitudes about mental health treatment, decrease stigma towards depression, and increase self-efficacy to seek treatment resulting in changes in Attitudes, Subjective Norms, and Perceived Behavioral Control.
Discussion boards and “ask the expert” strategies were not included since a recent systematic review indicated that they were seldom used (Crutzen et al., 2011). Behavior change in Internet-based interventions is associated with longer and more consequential involvement with the website and by endorsement of website’s personal relevance (Crutzen et al., 2008; Strecher, Shiffman, & West, 2006). In developing the prototype website, we collaborated with our community partners to ensure that the site was engaging to adolescents in order to increase use (Danaher, Boles, Akers, Gordon, & Severson, 2006). Dose of intervention was calculated at the individual-level and was based upon patterns of engagement of website (unique visitors, use of specific sections of site, time spent). That is, we were able to calculate for each individual user analytics (e.g., number of visits to the website, time on website, sequential pattern on the website, time on website, clicks on websites, etc.).
Each of the counties in the study provide mental health services to low-income individuals through county health departments or subcontracted services. Reimbursement for mental health services is available through Medicaid, sliding scale fee structures, or private insurance.
Instruments
Adolescent mothers in both groups completed the same measures, which were based upon TBP. The intervention group completed a pre-test before starting the intervention. Outcome measures were completed immediately after the intervention and two weeks later. Adolescents in the comparison group completed the same measures twice, two weeks apart.
Questionnaires with established reliability and validity in adolescent mothers and based upon TPB were used to measure study variables of Attitude (Attitude Towards Seeking Psychological Help; 10 items; Respondents rated each statement in a Likert-type response format consisting of the alternatives agree, partly agree, partly disagree, and disagree. The range of scores is from 0 to 30 with a high score indicating a positive attitude toward seeking help; Fisher & Turner, 1995), Subjective Norms (Stigma Scale for Receiving Psychological Help; 5 items; Each question is rated from 0 (strongly disagree) to 3 (strongly agree) with higher scores indicating greater perception of stigma associated with receiving psychological treatment; Komiya, Good, & Sherrod, 2000), Perceived Behavior Control (Health Self Determination Index; 1 item; kids like to make plans for their health themselves; □ REALLY TRUE for ME □ SORT of TRUE for ME; Cox, Cowell, Marion, & Miller, 1990), and Intention to Seek Depression Treatment (Mental Health Intention Scale; 3 items; example of one item: how likely is it that you’ll actually get mental health treatment; revised from Gerend, Lee, & Shepherd, 2007). In our previous studies, reliabilities of each of these instruments had Cronbach’s alphas ranging from .74 to .89 indicating good internal consistency.
For those adolescent mothers with symptoms of depression, questions inquired if the adolescent has plans to make an appointment for depression treatment, has made an appointment for depression treatment, or has received depression treatment in the last two weeks and if not, what were the barriers to depression treatment.
The Patient Health Questionnaire (PHQ-2) was used to screen for symptoms of depression (Arroll, Khin, & Kerse, 2003). This instrument has a sensitivity of .85 in adolescents in a primary care setting (Borner, Braunstein, St Victor, & Pollack, 2010), and sensitivity of 100% among postpartum women at 4–6 months postpartum (Chae, Chae, Tyndall, Ramirez, & Winter, 2012). The PHQ-2 inquires about the frequency of depressed mood and anhedonia over the past 2 weeks, scoring each as 0 (“not at all”) to 3 (“nearly every day”). The PHQ-2 was validated by 6000 patients in 8 primary care clinics and 7 obstetrics–gynecology clinics.
Last, in the intervention group, we asked participants to provide feedback on the intervention itself.
Data Analysis
Potential confounding and effect modification was a serious concern of the research team. To adjust analyses for potential differences between the groups, while maximizing power, Propensity Scoring using a “greedy” algorithm was used to minimize potential bias (Guo & Fraser, 2010). This minimized differences between groups, similar to randomization in a RCT. We started data analysis with straight forward tests for differences between the two groups of adolescent mothers. This allowed us to test if randomization was successful and no significant differences between controls and intervention group existed. Analysis of Variance (ANOVA) techniques were used to test for differences between continuous variables, while Kruskal-Wallis, Fischer’s Exact Tests and Wilcoxon methods were used to test for differences among categorical variables; when and where appropriate.
Cronbach’s alphas we calculated for each instrument to test the internal consistency of the instruments in our population. Repeated measures ANOVA techniques were used to test if changes occurred over time both within groups and between groups using an adjusted approach.
Subsequently, we developed adjustment models to test for independent predictors of (1) attitude, (2) subjective norms, (3) perceived control, (4) intention of treatment, and (5) actual treatment. That is, to examine the outcomes (1) Attitudes, (2) Perceived Control, (3) Subjective Norms, and (4) Intention to Seek Treatment, separate mixed-effects general linear models were developed for each outcome (four separate models developed). The two groups (intervention vs. comparison), were analyzed as fixed effects and time (week since enrollment) was analyzed as a repeated measures effect. This allowed us to examine whether these outcomes significantly change over time. Traditional risk factors (e.g., age, ethnicity) were incorporated as covariates during secondary analyses. All main effects and all two-way interaction were investigated for significance from the mixed-effects models developed. All variables were entered into the model simultaneously in one step.
To answer the RQ1 -- what is the association between exposure to the Internet-based depression intervention and study outcomes – we estimated the dose (magnitude of exposure) of the Internet-based social marketing intervention for each individual in the counties that received the intervention (e.g., time on site, number of clicks, webpages viewed, etc.). Generalized linear models were developed in which each outcome was made a function of dose to test whether (1) Attitudes, (2) Perceived Control, (3) Subjective Norms, and (4) Intention to Seek Treatment were impacted by dose of the intervention.
To answer RQ2 – what is the association between use of the internet-based depression intervention and actual seeking of depression evaluation and treatment- a mixed-effects general linear model was developed in which (self-reported) treatment was the outcome. Initially, the two groups (intervention and comparison), were analyzed as fixed effects and time (week since enrollment) using repeated measures ANOVA. Baseline depression level and county of residence were incorporated into the model, allowing us to adjust for baseline depression level and county of residence.
Traditional risk factors (e.g., age, ethnicity) were incorporated as covariates during secondary analyses. All main effects and all two-way interaction were investigated for significance from the mixed-effects models developed. In addition, logistic regression techniques was used to test whether the odds an adolescent mothers seeks depression treatment was impacted by the intervention.
To answer RQ3 – what is the association between intention to seek depression treatment at baseline and actual seeking of treatment – initially we performs a descriptive analysis of the proportion of those we reported intent at baseline actually seeking treatment at follow-up. In addition, a logistic regression model was developed to test whether the odds an adolescent mother seeks depression evaluation and treatment can be predicted from their intention to seek treatment. Traditional risk factors (e.g., depression level, county of residence, age, and ethnicity) were incorporated as covariates during secondary analyses. All main effects and all two-way interaction were investigated for significance.
Results
Demographics
Loss of follow-up was low for both groups (n=3, 2.1% for the controls; n=5, 3.1% for the intervention group). There were no significant differences in demographics between the control group and intervention group, at baseline. See Table 1. The women were primarily African American (n=124, 89.2% and n=133, 86.4%, respectively), had less than a high school education (n=72, 51.7% and n=84, 54.5%), were not currently pregnant (n=1, 0.7% vs. 0, 0.0%) and had given birth in the last year (n=135, 97.8% vs. n=151, 98.1%.). Both groups had given birth a little under four months prior (3.7 months on average vs. 3.9 months on average) and were roughly 18 years of age (18.2 years on average vs. 17.9 years on average,). There were also no significant differences between the groups on rates of depressive symptoms, at baseline. See Table 1.
Table 1.
Demographic variables stratified by control and intervention group. Analysis of Variance (ANOVA) techniques were used to test for differences between groups for continuous variables, while Kruskal-Wallis, Fischer’s Exact Test and Wilcoxon methods were used to test for differences among categorical variables; when and where appropriate.
| Demographic | Control Group N=138 (%) |
Intervention Group N=154 |
p-value |
|---|---|---|---|
|
| |||
| Ethnicity | 0.695 | ||
| White | 11 (7.9%) | 14 (9.1%) | |
| Black | 124 (89.2%) | 133 (86.4%) | |
| Other | 4 (2.9%) | 7 (4.5%) | |
|
| |||
| Education | 0.322 | ||
| < High School | 72 (51.7%) | 84 (54.5%) | |
| High School | 49 (35.3%) | 59 (38.3%) | |
| ➢High School | 17 (12.2%) | 11 (7.2%) | |
|
| |||
| Currently Pregnant | 1 (0.7%) | 0 (0.0%) | 0.281 |
|
| |||
| Depressed | 18 (13.0%) | 19 (12.3%) | 0.856 |
|
| |||
| Given Birth in Last Year | 135 (97.8%) | 151 (98.1%) | 0.892 |
| Mean Months Ago (SD) | 3.7 (3.3) | 3.9 (3.1) | 0.225 |
|
| |||
| Mean Age (SD) | 18.2 (1.9) | 17.9 (2.1) | 0.884 |
|
| |||
| Median Time on Intervention | - | 3.12 minutes (IQR 0.2–28) | - |
From the intervention group, acceptability ratings of the intervention were as follows: The website is easy to use n=124 (80.8%); An internet website is a good place for me to learn about depression n=108 (70.2%); I can relate to one or more of the stories presented on the homepage n=76 (49.2%); I would recommend this website to another teen mom n=110 (71.5%).
Performance on the Instruments
As seen in Table 2, the study instruments had acceptable internal consistency reliability scores. Analysis associated with each research question is described below.
Table 2.
Internal consistency of the instruments overall as well as stratified by group
| Instrument | Cronbach Alpha | Cronbach Alpha | Cronbach Alpha |
|---|---|---|---|
| Overall | Controls | Intervention | |
| Attitudes | 0.78 | 0.76 | 0.79 |
| Subjective Norms | 0.87 | 0.84 | 0.88 |
| Perceived Control | 0.83 | 0.86 | 0.82 |
| Intention | 0.76 | 0.75 | 0.78 |
RQ1: What is the association between exposure to the Internet-based depression intervention and study outcomes (attitude and subjective norms towards mental health treatment, perceived control, intention to seek depression evaluation and treatment and actually receiving treatment), when controlling for baseline measures? Is there a dose response?
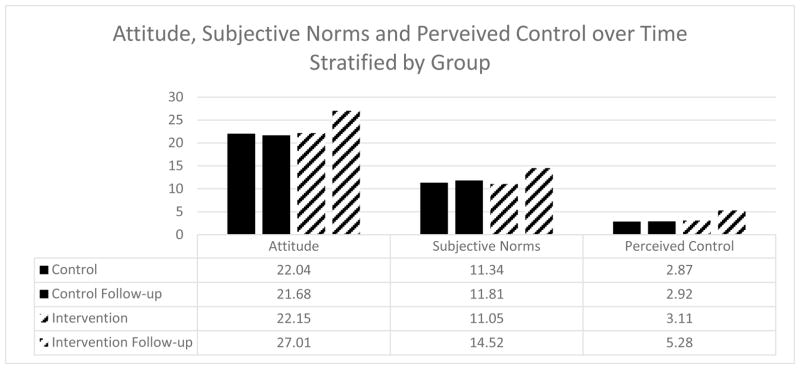
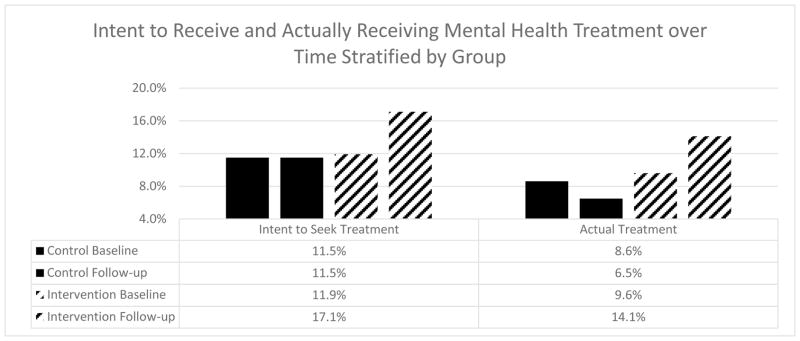
As seen in Table 3 and Figure 1, scores on two of the instruments (attitude p=0.041 and perceived control p=0.007) improved significantly more over time for the intervention group when compared to the control group, but subjective norms did not. In addition, the scores on the instruments remained consistent over time within the control group (attitude, p=0.841; subjective norms, p=0.784; and perceived control, p=0.913), while the scores significantly improved within the intervention group (p=0.018, p=0.040 and p<0.001, respectively). Similarly, as seen in Table 4 and Figure 2, those in the intervention group intend to seek treatment (p=0.003) and actually receive treatment (p=0.009) over time when compared to the control group. Within the control group, intention to seek treatment and actual treatment rates did not change (p=0.999 and p=0.081, respectively). Both rates increased over time within the intervention group (p=0.003 and p<0.001, respectively).
Table 3.
Changes in scores on the instruments as well as outcomes over time both overall and stratified by group
| Outcome | C T1 | C T2 | p-value within | IT1 | I T2 | p-value within | p-value between |
|---|---|---|---|---|---|---|---|
| Attitude | 22.04 | 21.68 | 0.841 | 22.15 | 27.01 | 0.018** | 0.041** |
| Subjective Norms | 11.34 | 11.81 | 0.784 | 11.05 | 14.52 | 0.040** | 0.081 |
| Perceived Control | 2.87 | 2.92 | 0.913 | 3.11 | 5.28 | <0.001** | 0.007** |
| Intend Treatment | 11.50% | 11.50% | 0.999 | 11.90% | 17.10% | 0.013** | 0.003** |
| Actual Treatment | 8.60% | 6.50% | 0.081 | 9.60% | 14.10% | 0.009** | <0.001** |
Note: C=control group; T1=time 1; T2=time 2; I=intervention group
Figure 1.
Attitude, subjective norms, and perceived control over time stratified by group.
Table 4.
GLMM modeling instruments and outcomes over time
| Outcome | Predictors | B | p-value |
|---|---|---|---|
| Attitude | Intervention | 2.92 | 0.018** |
| Time | 1.2 | 0.475 | |
| Age | 0.08 | 0.925 | |
| Ethnicity | 0.05 | 0.961 | |
| Urban | 0.2 | 0.751 | |
| Dose | 2 | 0.029** | |
| Subjective Norms | Intervention | 1.81 | 0.064 |
| Time | 0.52 | 0.587 | |
| Age | 0.06 | 0.958 | |
| Ethnicity | 0.11 | 0.845 | |
| Urban | 0.29 | 0.629 | |
| Dose | 1.38 | 0.291 | |
| Perceived Control | Intervention | 2.06 | 0.021** |
| Time | 0.94 | 0.378 | |
| Age | 0.04 | 0.97 | |
| Ethnicity | 0.14 | 0.824 | |
| Urban | 0.18 | 0.645 | |
| Dose | 0.98 | 0.255 | |
| Intention of Treatment | Intervention | 4.19 | <0.001** |
| Time | 0.54 | 0.583 | |
| Age | 0.03 | 0.982 | |
| Ethnicity | 0.1 | 0.899 | |
| Urban | 0.4 | 0.596 | |
| Dose | 0.79 | 0.524 | |
| Actual Treatment | Intervention | 5.02 | <0.001** |
| Time | 0.47 | 0.59 | |
| Age | 0.06 | 0.906 | |
| Ethnicity | 0.16 | 0.561 | |
| Urban | 0.76 | 0.215 | |
| Dose | 0.65 | 0.33 |
Figure 2.
Seeking information, intent to receive and actually receiving mental health treatment over time stratified by group.
As seen in Table 4, the intervention independently influenced (increased) attitudes (B=2.92, p=0.018), beliefs of perceived control (B=2.06, p=0.021), intention to seek treatment (B=4.19, p<0.001) and actually receiving treatment (B=5.02, p<0.001). Dose of the intervention (measured in time on the intervention) significantly impacted (increased) attitudes (B=2.00, p=0.029). No other predictor impacted any of the outcomes. In addition, no two-way interaction effects existed.
RQ2: What is the association between use of the internet-based depression intervention and actual seeking of depression evaluation and treatment, when controlling for baseline depression symptoms and traditional risk factors
As seen in Table 5, being depressed (OR=2.15, 95% CI 1.15–4.04, p=0.005) and being exposed to the intervention (OR=1.65, 95% CI 1.06–2.32, p=0.012) increased the odds of seeking treatment.
Table 5.
Logistic regression model predicting actually seeking treatment
| Outcome | Predictors | OR (95% CI) | p-value |
|---|---|---|---|
| Actual Treatment | Depressed | 2.15 (1.15–4.04) | 0.005** |
| Intervention | 1.65 (1.06–2.32) | 0.012** | |
| Intention | 17.81 (13.92–28.63) | <0.001** | |
| Time | 1.07 (0.68–1.46) | 0.715 | |
| Age | 1.04 (0.62–1.530 | 0.648 | |
| Ethnicity | 1.09 (0.81–1.41) | 0.659 | |
| Urban | 1.29 (0.70–2.44) | 0.456 | |
| Dose | 1.32 (0.77–2.66) | 0.422 |
RQ3: What is the association between intention to seek depression treatment at baseline and actual seeking of treatment, when controlling for baseline depression symptoms?
Unadjusted, a majority of those who intended to seek treatment (n=26, 17.1%) actually did report receiving treatment (n=22, 84.6%), which is strongly correlated (r=0.86, p<0.001). Similarly, as seen in Table 5, taking an adjusted approach, intention to seek treatment significantly impacts the odds of actually seeking treatment (OR=17.81, 95% CI 13, 92–28.63, p<0.001), (while adjusting for depression, age, ethnicity, urban/rural location, dose, and receiving the intervention).
Discussion and Conclusions
Based upon TPB, this study described the impact of an Internet based depression intervention in successfully changing attitudes, perceived control, intention to seek treatment, and actually seeking treatment in a sample of adolescent mothers. Contrary to expectations, living in a rural area did not impact study results. Receiving a larger dose of the intervention impacted attitude towards mental health treatment, but not the rate of actually seeking treatment.
Subjective norms were not changed by the intervention. As subjective norms reflect “the perceived social pressure to perform or not to perform the behavior” in question (Ajzen, 1991, p. 188), it is likely that the intervention dose was not sufficient to change such a long standing perception.
The rates of depressive symptoms at baseline in both the control and intervention groups were lower than reported in any of our preliminary studies. However, this is the first time that our team has used the PHQ-2 for depression screening; the depression screening instruments for our other studies included the CES-D and/or the EPDS. Researchers, including our research team, should continue to explore the psychometrics of depression screening instruments in adolescent mothers.
Limitations of the study include the use of self-report measures. Medical records were not available to corroborate the adolescent’s report of use of mental health services. In addition, adolescent mothers in the intervention group and comparison group completed measures in different settings (comparison group in home and intervention group online). Although the counties used for recruitment of the adolescent mothers were matched in terms of population and rural/urban location, confidence in study findings would have been enhanced with random assignment of participants to the control or comparison groups.
In terms of recommendations for further research, the vast majority of the adolescent mothers rated the intervention as acceptable. Thus, further Internet interventions should be considered to promote the health of adolescent mothers and their infants.
It is possible that adolescent mothers are not receiving depression evaluation and treatment because of health care system or other barriers that our research team has not previously identified. This information will continue to be collected and will inform any revision of our intervention before we implement the study with a national audience.
Information obtained in this study could enhance the clinical practice of perinatal and public health nurses and other clinicians who play pivotal roles in providing health information, screening, referrals, and support for new mothers with depressive symptoms. An internet based depression intervention can be initiated and monitored at low cost, and it is effective in increasing rates of depression treatment.
Our public health approach of recruiting adolescent mothers from the community may result in different findings compared to a study in which a clinical population of adolescent mothers with a diagnosis of depression constituted the sample. However, we believe our sample is more reflective of the real world and that our findings can more easily be generalizable to a variety of research, practice, and policy settings.
Footnotes
Conflicts of Interest: None to declare.
Ethical Statement
The study was supported by funding from the National Institute of Nursing Research, Award #R15NR013563. The authors report no conflicts of interest. The study was approved by the Human Subjects Protection Program of the University, as well as the research committees of each clinical site. Participants provided informed consent.
Contributor Information
M. Cynthia Logsdon, Associate Chief of Nursing for Research, University of Louisville Hospital/James Brown Cancer Center; Professor, School of Nursing, University of Louisville, 555 S Floyd Street, Louisville KY, 40202.
John Myers, Professor, Department of Pediatrics, Child & Adolescent Research Design & Support (CAHRDS) Unit, University of Louisville School of Medicine, 323 E Chestnut St, Louisville, KY 40202.
Jeff Rushton, Director of Digital Media, University of Louisville, 555 S Floyd Street, Louisville KY, 40202.
Jennifer L. Gregg, Associate Professor and Chair of Communication, University of Massachusetts Boston, 100 Morrissey Blvd., Boston, MA 02125-3393.
Allan M. Josephson, Professor, Division Chief, Child/Adolescent Psychiatry, Department of Pediatrics, Child and Adolescent Psychiatry and Psychology, Louisville, KY.
Deborah Winders Davis, Professor, Department of Pediatrics, Child & Adolescent Research Design & Support (CAHRDS) Unit, University of Louisville School of Medicine, 323 E Chestnut St, Louisville, KY 40202.
Kyle Brothers, Assistant Professor, Department of Pediatrics, School of Medicine, University of Louisville, 323 E Chestnut St, Louisville, KY 40202.
Kristin Baisch, Research Project Coordinator, School of Nursing, University of Louisville, 555 S Floyd Street, Louisville KY, 40202.
Anissa Carabello, Clinical Nurse, University of Louisville Hospital, Louisville, Kentucky 40202.
Krista Vogt, Research Project Assistant, School of Nursing, University of Louisville, 555 S Floyd Street, Louisville KY, 40202.
Kayla Jones, Clinical Nurse, University of Louisville Hospital, Louisville, Kentucky.
Jennifer Angermeier, TAPP Clinic Supervisor, Westport Tapp School, 8800 Westport Rd, Louisville KY, 40242.
References
- Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50:179–211. [Google Scholar]
- Ajzen I. Models of human social behavior and their application to health psychology. Psychology & Health. 1998;13:735–9. [Google Scholar]
- Arroll B, Khin N, Kerse N. Screening for depression in primary care with two verbally asked questions: cross sectional study. British Medical Journal. 2003;327:1144–6. doi: 10.1136/bmj.327.7424.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker R, White KMW. Their Own Words: Why Teenagers Don’t Use Social Networking Sites. Cyberpsychol Behavior Social Network. 2010–2011;14(6):395–398. doi: 10.1089/cyber.2010.0016. [DOI] [PubMed] [Google Scholar]
- Bangor A, Kortum P, Miller J. An empirical evaluation of the system usabiluty scale. International Journal of Human-Computer Interaction. 2008;24(6):574–594. [Google Scholar]
- Beck CT. The effects of postpartum depression on maternal-infant interaction: a meta-analysis. Nurse Researcher. 1995;44:298–304. [PubMed] [Google Scholar]
- Bennett G, Glasgow R. The delivery of public health interventions via the Internet: Actualizing their potential. Annual Review of Public Health. 2009;30:273–92. doi: 10.1146/annurev.publhealth.031308.100235. [DOI] [PubMed] [Google Scholar]
- Bennett G, Herring S, Puleo e, et al. Web based weight loss in primary care: A randomized controlled trial. Intervention and Prevention. 2010;18:308–13. doi: 10.1038/oby.2009.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett GG, Warner ET, Glasgow RE, et al. Obesity Treatment for Socioeconomically Disadvantaged Patients in Primary Care Practice. Archives of Internal Medicine. 2012;172:565–74. doi: 10.1001/archinternmed.2012.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop LM. Abstinence from vaginal intercourse among black adolescent females as a means of pregnancy prevention. Dissertations available from ProQuest Paper, AAI3072973. 2002 http://repositoryupennedu/dissertations/AAI3072973.
- Bleakley A, Berzel C, VanDevanter N, Messeri P. Computer access and Internet use among urban youths. American Journal for Public Health. 2004;94:744–6. doi: 10.2105/ajph.94.5.744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borner I, Braunstein JW, St Victor R, Pollack J. Evaluation of a 2-question screening tool for detecting depression in adolescents in primary care. Clinical Pediatrics, (Phila) 2010;49:947–53. doi: 10.1177/0009922810370203. [DOI] [PubMed] [Google Scholar]
- Brennan PA, Andersen MJ, Hammen C, Bor W. Chronicity, severity, and timing of maternal depressive symptoms: Relationships with child outcomes at age 5. Developmental Psychology. 2000;36(6):759–766. doi: 10.1037//0012-1649.36.6.759. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Matestic P, von Stauffenberg C, Mohan R, Kirchner T. Trajectories of maternal depressive symptoms, maternal sensitivity, and children’s functioning at school entry. Developmental Psychology. 2007:1202–1215. doi: 10.1037/0012-1649.43.5.1202. [DOI] [PubMed] [Google Scholar]
- Chae SY, Chae MH, Tyndall A, Ramirez MR, Winter RO. Can we effectively use the two-item PHQ-2 to screen for postpartum depression? Family Medicine. 2012;44(10):698–703. [PubMed] [Google Scholar]
- Chico E, Gonzalez A, Ali N, Steiner M, Fleming AS. Executive function and mothering: challenges faced by teenage mothers. Developmental Psychobiology. 2014;56(5):1027–1035. doi: 10.1002/dev.21185. [DOI] [PubMed] [Google Scholar]
- Christiansen H, Criffiths K, Jorm A. Delivering interventions for depression by using the internet: randomised controlled trial. British Medical Journal. 2004;328:265. doi: 10.1136/bmj.37945.566632.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox CL, Cowell JM, Marion LN, Miller EH. The Health Self-Determinism Index for Children. Research in Nursing Health. 1990;13:237–46. doi: 10.1002/nur.4770130406. [DOI] [PubMed] [Google Scholar]
- Crutzen R, de Nooijer J, Brouwer W, et al. Internet-delivered interventions aimed at adolescents: a Delphi study on dissemination and exposure. Health Education Research. 2008;23:427–39. doi: 10.1093/her/cym094. [DOI] [PubMed] [Google Scholar]
- Crutzen R, de Nooijer J, Brouwer W, et al. Strategies to facilitate exposure to internet-delivered health behavior change interventions aimed at adolescents or young adults: a systematic review. Health Education Behavior. 2011;38:49–62. doi: 10.1177/1090198110372878. [DOI] [PubMed] [Google Scholar]
- Danaher BG, Boles SM, Akers L, Gordon JS, Severson HH. Defining participant exposure measures in Web-based health behavior change programs. Journal of Medical Internet Research. 2006;8:e15. doi: 10.2196/jmir.8.3.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis CL, Stewart DE. Treatment of postpartum depression, part 1: a critical review of biological interventions. Journal of Clinical Psychiatry. 2004;65:1242–51. doi: 10.4088/jcp.v65n0914. [DOI] [PubMed] [Google Scholar]
- Fishbein M, Von Haeften I, Appleyard J. The role of theory in developing effective interventions: Implications from project SAFER. Psychology Health and Medicine. 2001;6:223–38. [Google Scholar]
- Fisher E, Turner A. Attitudes toward seeking professional psychological help: A shortened form and considerations for research. Journal of College Student Development. 1995;36:368–73. [Google Scholar]
- Fortney J, Rost K, Zhang M. A joint choice model of the decision to seek depression treatment and choice of provider sector. Medical Care. 1998;36:307–20. doi: 10.1097/00005650-199803000-00008. [DOI] [PubMed] [Google Scholar]
- Froman RD, Owen SV. Mothers’ and nurses’ perceptions of infant care skills. Research in Nursing Health. 1990;13:247–53. doi: 10.1002/nur.4770130407. [DOI] [PubMed] [Google Scholar]
- Gaynes BN, Gavin N, Meltzer-Brody S, et al. Perinatal depression: prevalence, screening accuracy, and screening outcomes. Evidence Report Technology Assessment (Summary) 2005;119:1–8. doi: 10.1037/e439372005-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerend M, Lee S, Shepherd J. Predictors of HPV acceptability among underserved women. Sexually Transmitted Diseas. 2007;34:468–71. doi: 10.1097/01.olq.0000245915.38315.bd. [DOI] [PubMed] [Google Scholar]
- Gillmore MR, Archibald ME, Morrison DM, et al. Teen sexual behavior: Applicability of the theory of reasoned action. Journal of Marriage and Family. 2004;64(4):885–97. [Google Scholar]
- Gjerdingen D. The effectiveness of various postpartum depression treatments and the impact of antidepressant drugs on nursing infants. The Journal of the American Board of Family Medicine. 2003;16:372–82. doi: 10.3122/jabfm.16.5.372. [DOI] [PubMed] [Google Scholar]
- Guo S, Fraser M. Propensity Score Analysis: Statistical Methods and Applications. Thousand Oaks: Sage; 2010. [Google Scholar]
- Hauenstein EJ, Petterson S, Rovnyak V, et al. Rurality and mental health treatment. Administration and Policy in Mental Health. 2006;34:225–67. doi: 10.1007/s10488-006-0105-8. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Frank RG, Edlund M, et al. Differences in the use of psychiatric outpatient services between the United States and Ontario. The New England Journal of Medicine. 1997;336:551–7. doi: 10.1056/NEJM199702203360806. [DOI] [PubMed] [Google Scholar]
- Killien MG. Postpartum return to work: mothering stress, anxiety, and gratification. Canadian Journal of Nursing Reasearch. 1998;30:53–66. [PubMed] [Google Scholar]
- Kingston D, Tough S, Whitfield H. Prenatal and postpartum maternal psychological distress and infant development: A systematic review. Child Psychiatry and Human Development. 2012;43(5):683–714. doi: 10.1007/s10578-012-0291-4. [DOI] [PubMed] [Google Scholar]
- Kinsler J, Sneed CD, Morisky DE, Ang A. Evaluation of a school-based intervention for HIV/AIDS prevention among Belizean adolescents. Health Education Research. 2004;19:730–8. doi: 10.1093/her/cyg091. [DOI] [PubMed] [Google Scholar]
- Klnd T, Huang Z, Farr D, Pomerantz K. Internet and computer access and use for health information in an underserved community. Ambulatory Pediatrics. 2005;5:117–21. doi: 10.1367/A04-107R.1. [DOI] [PubMed] [Google Scholar]
- Komiya N, Good GE, Sherrod NB. Emotional openness as a predictor of college students’ attitudes toward seeking psychological help. Journal of Counseling Psychology. 2000;47:138–43. [Google Scholar]
- Koo M, Skinner H. Challenges of internet recruitment: a case study with disappointing results. Journal of Medical Internet Research. 2005;7:e6. doi: 10.2196/jmir.7.1.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leaf PJ, Bruce ML, Tischler GL, et al. Factors affecting the utilization of specialty and general medical mental health services. Medical Care. 1988;26:9–26. doi: 10.1097/00005650-198801000-00002. [DOI] [PubMed] [Google Scholar]
- Lenhart A, Purcell KP, Smith A, Zickuhr K. Social media and mobile internet use among teens and young adults. 2010 http://pewinternet.org/Reports/2010/social-media-and-young-adults.aspx.
- Logsdon MC, Barone M, Lynch T, Robertson A, Myers J, Morrison D, York S, Gregg J. Testing of a protype web based intervention for adolescent mothers on postpartum depression. Applied Nursing Research. 2013;26:143–145. doi: 10.1016/j.apnr.2013.01.005. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Birkimer JC, Simpson T, Looney S. Postpartum depression and social support in adolescents. Journal of Obstetetric Gynecol Neonatal Nursing. 2005;34:46–54. doi: 10.1177/0884217504272802. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Foltz MP, Stein B, Usui W, Josephson A. Adapting and testing telephone-based depression care management intervention for adolescent mothers. Archives of Womens Mental Health. 2010;13:307–17. doi: 10.1007/s00737-009-0125-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logsdon MC, Gohmann S. Challenges and costs related to recruitment of female adolescents for clinical research. Journal of Pediatric Nursing. 2008;23:331–6. doi: 10.1016/j.pedn.2007.10.006. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Hines-Martin V, Rakestraw V. Barriers to depression treatment in low-income, unmarried, adolescent mothers in a southern, urban area of the United States. Issues in Mental Health Nursing. 2009;30:451–5. doi: 10.1080/01612840902722187. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Mittelberg M, Myers J. Use of social media and Internet to obtain health information by rural adolescent mothers. Applied Nursing Research. 2015;28:55–56. doi: 10.1016/j.apnr.2014.04.006. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Usui W, Pinto-Foltz M, Rakestraw VL. Intention to seek depression treatment in adolescent mothers and a comparison group of adolescent girls. Archives of Psychiatric Nursing. 2009;23:41–9. doi: 10.1016/j.apnu.2008.02.013. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Wisner K, Hanusa BH. Does maternal role functioning improve with antidepressant treatment in women with postpartum depression? Journal of Women’s Health. 2009;18:85–90. doi: 10.1089/jwh.2007.0635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logsdon MC, Wisner KL, Pinto-Foltz MD. The impact of postpartum depression on mothering. Journal of Obstetric, Genecologic, and Neonatal Nursing. 2006;35:652–8. doi: 10.1111/j.1552-6909.2006.00087.x. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Ziegler C, Hertweck P, Pinto-Foltz M. Testing a bioecological model to examine social support in postpartum adolescents. Journal of Nursing Scholarship. 2008;40:116–23. doi: 10.1111/j.1547-5069.2008.00215.x. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Bennett G, Crutzen R, Martin L, Eckert D, Robertson A, Myers J, Tomasulo R, Gregg J, Barone M, Lynch T, Flamini L. Preferred health resources and use of social media to obtain health and depression information by adolescent mothers. Journal of Child and Adolescent Psychiatric Nursing. 2014;27:163–8. doi: 10.1111/jcap.12083. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Pinto-Foltz MD, Scheetz J, Myers JA. Self-efficacy and postpartum teaching behaviors of hospital nurses. Journal of Perinatal Education. 2010;19(4):10–16. doi: 10.1624/105812410X530884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maughan A, Cicchetti D, Toth SL, Rogosch FA. Early-occurring maternal depression and maternal negativity in predicting young children’s emotion regulation and socioemotional difficulties. Journal of Abnormal Child Psychology. 2007;35(5):685–703. doi: 10.1007/s10802-007-9129-0. [DOI] [PubMed] [Google Scholar]
- McNeil L, Viswanath K, Bennett GG, Puleo E, Emmons KM. Feasibility of using a web-based nutrition intervention among residents of multiethnic working-class neighborhoods. Preventing chronic disease: Public Health Research, Practice and Policy. 2007;4:1–9. [PMC free article] [PubMed] [Google Scholar]
- McPeak KE, Sandrock D, Spector ND, Pattishall AE. Important determinants of newborn health: postpartum depression, teen parenting, and breast-feeding. Current Opinion in Pediatrics. 2015;27(1):138–144. doi: 10.1097/MOP.0000000000000185. [DOI] [PubMed] [Google Scholar]
- Murry V, Heflinger C, Suiter S, Brody G. Examining perceptions about mental health care and help-seeking among rural African American families of adolescents. Journal of Youth & Adolescence. 2011;40(9):1118–1131. doi: 10.1007/s10964-010-9627-1. [DOI] [PubMed] [Google Scholar]
- National Academy of Sciences. Committee on Adolescent Health Care Services and Models of Care for Treatment, Prevention, and Healthy Development Adolescent Health Services: Missing Opportunities. Washington, DC: National Academies Press; 2009. [Google Scholar]
- NICHD Early Child Care Research Network. Chronicity of maternal depressive symptoms, maternal sensitivity, and child functioning. Developmental Psychology. 1999;35:1297–1310. doi: 10.1037//0012-1649.35.5.1297. [DOI] [PubMed] [Google Scholar]
- Norman CD, Skinner HA. Engaging youth in e-health promotion: lessons learned from a decade of TeenNet research. Adolescent Medicine: State of the Art Reviews. 2007;18:357–69. xii. [PubMed] [Google Scholar]
- O’Hara MW, Stuart S, Gorman LL, Wenzel A. Efficacy of interpersonal psychotherapy for postpartum depression. Archives of General Psychiatry. 2000;57:1039–45. doi: 10.1001/archpsyc.57.11.1039. [DOI] [PubMed] [Google Scholar]
- O’Kearney R, Kang K, Christensen H, Griffiths K. A controlled trial of a school-based Internet program for reducing depressive symptoms in adolescent girls. Depression and Anxiety. 2009;26:65–72. doi: 10.1002/da.20507. [DOI] [PubMed] [Google Scholar]
- Phipps MG, Raker CA, Ware CF, Zlotnick C. Randomized controlled trial to prevent postpartum depression in adolescent mothers. American Journal of Obstetrics and Gynecology. 2013;208:192e1–6. doi: 10.1016/j.ajog.2012.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, O’Keefe Z, Kracker R, Foo HH. Prevention of HIV among adolescents. Prevention Science. 2000;1:15–30. doi: 10.1023/a:1010071932238. [DOI] [PubMed] [Google Scholar]
- Steele RM, Mummery WK, Dwyer T. A comparison of face-to-face or internet-delivered physical activity intervention on targeted determinants. Health Education Behaviors. 2009;36:1051–64. doi: 10.1177/1090198109335802. [DOI] [PubMed] [Google Scholar]
- Stephenson MT, Quick BL, Atkinson J, Tschida DA. Authoritative parenting and drug-prevention practices: implications for antidrug ads for parents. Health Communication Journal. 2005;17:301–21. doi: 10.1207/s15327027hc1703_6. [DOI] [PubMed] [Google Scholar]
- Strecher VJ, Shiffman S, West R. Moderators and mediators of a web-based computer-tailored smoking cessation program among nicotine patch users. Nicotine & Tobacco Research. 2006;1:S95–101. doi: 10.1080/14622200601039444. [DOI] [PubMed] [Google Scholar]
- Swanson V, Power K, Kaur B, Carter H, Shepherd K. The impact of knowledge and social influences on adolescents’ breast-feeding beliefs and intentions. Public Health Nutrition. 2006;9:297–305. doi: 10.1079/phn2006845. [DOI] [PubMed] [Google Scholar]
- Unger JB, Rohrbach LA, Howard-Pitney B, Ritt-Olson A, Mouttapa M. Peer influences and susceptibility to smoking among California adolescents. Substance Use & Misuse. 2001;36:551–71. doi: 10.1081/ja-100103560. [DOI] [PubMed] [Google Scholar]
- Van Voorhees BW, Fogel J, Houston TK, et al. Attitudes and illness factors associated with low perceived need for depression treatment among young adults. Social Psychiatry Psychiatric Epidemiology. 2006;41:746–54. doi: 10.1007/s00127-006-0091-x. [DOI] [PubMed] [Google Scholar]
- Williams SB, O’Connor EA, Eder M, Whitlock EP. Screening for child and adolescent depression in primary care settings: a systematic evidence review for the US Preventive Services Task Force. Pediatrics. 2009;123:e716–35. doi: 10.1542/peds.2008-2415. [DOI] [PubMed] [Google Scholar]
- Wisdom J, Clarke G, Green C. What teens want: barriers to seeking care for depression. Administration and Policy in Mental Health. 2006;33:133–45. doi: 10.1007/s10488-006-0036-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yozwiak JA. Postpartum depression and adolescent mothers: a review of assessment and treatment approaches. Journal of Pediatric Adolescent Gynecology. 2010;23:172–8. doi: 10.1016/j.jpag.2009.09.003. [DOI] [PubMed] [Google Scholar]