Abstract
Objectives
To determine the health literacy levels of persons living with human immunodeficiency virus (HIV) (PLWH) at a health clinic in the Dominican Republic (DR) and assess associations between health literacy, HIV-related knowledge, and health information behavior (how patients need, seek, receive, and use information).
Design
Cross-sectional, descriptive.
Sample
Participants were 107 PLWH attending the Clinic.
Measurements
A theoretically based, 64-item survey assessing information behavior and HIV-related knowledge was administered in Spanish through individual interviews. Health literacy was assessed using the Short Assessment of Health Literacy – Spanish and English.
Results
On average, participants were 40.8 years old and had lived with HIV for 7.7 years. The majority (69.2%) had low health literacy. HIV-related knowledge and information behavior varied by health literacy level and uncertainty regarding a main indicator of disease progression, viral load, was demonstrated regardless of health literacy level. Participants with low health literacy were less likely to answer questions or answer questions correctly and many participants (39.2%) indicated viral transmission can occur through supernatural means.
Conclusions
Findings demonstrate unmet information need and that information received may not always be understood. Methods to improve health education are needed to ensure patients receive health information in an understandable way.
Keywords: Health Literacy, HIV/AIDS, Global Health, Patient Education
INTRODUCTION
The Caribbean has the highest prevalence of human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) outside of sub-Saharan Africa (De Boni, Veloso, & Grinsztejn, 2014). Approximately 75% of individuals living with HIV in this region reside on the island of Hispaniola, shared by the Dominican Republic (DR) and Haiti (Rojas, Malow, Ruffin, Rothe, & Rosenberg, 2011). Although incidence of HIV in the Caribbean, including the DR, has declined (Figueroa, 2014), an estimated 68,000 people in the country are still living with HIV (Joint United Nations Programme on HIV/AIDS, 2015). This decrease in incidence is attributed to improved antiretroviral therapies and large national and international responses to upscale prevention and treatment (Figueroa, 2014). These responses have led to the sustained reduction of new cases and long-term management of existing infections, both of which require persons living with HIV (PLWH) to acquire, comprehend, and use large amounts of information, such as how to manage treatment regimens. Unfortunately, obtaining and understanding required information may be particularly challenging in limited resource settings such as in the DR, where educational infrastructure, economic constraints, and literacy related barriers may complicate the provision and receipt of health information (Aboud & Singla, 2012). Nurses and health educators working with patients in these settings must be aware of these, and other, barriers that patients face when seeking health information in order to ensure that pertinent information gets to the people who need it the most (Person et al., 2006; Shedlin & Shulman, 2004).
Similarly, low levels of educational attainment and high levels of poverty, prevalent in limited resource settings, can lead to low health literacy, a widely discussed phenomenon that refers to the skills required to function in health care settings (Berkman, Sheridan, Donahue, Halpern, & Crotty, 2011). Low health literacy has been linked to worse health outcomes among PLWH, including lower treatment adherence, lower knowledge of illness, and can make it more difficult for individuals to acquire health information (Wawrzyniak, Ownby, McCoy, & Waldrop-Valverde, 2013; Zhang, Terry, & McHorney, 2014). The concept of “information behavior” is similar to health literacy but is more expansive in that it includes how people may need, seek, manage, and use information (Fisher, Erdelez, & McKechnie, 2005). Studies that include assessments of both health literacy and information behavior can generate a more comprehensive picture of how populations interact with health information. This familiarity, combined with an understanding of the HIV-related knowledge patients already have, can enable organizations and providers to more effectively tailor health education to meet patients’ specific needs. Therefore, this study aimed to determine the health literacy levels of PLWH attending a health care clinic in the DR and to explore potential associations between health literacy, HIV-related knowledge, and the health information behavior of this population.
METHODS
Design
Data for this cross-sectional study were collected during individual interviews, conducted in Spanish and guided by an information behavior survey, between August and October 2015.
Ethical Approval
All study procedures were approved by both Columbia University Medical Center’s Institutional Review Board (IRB) and by the Consejo Nacional de Bioética en Salud (CONABIOS), the ethical review committee in the DR.
Study Setting
All research took place at Clínica de Familia La Romana, a comprehensive primary care clinic in the southeast DR. Founded in 2004 by Columbia University’s International Family AIDS Program (IFAP Global Health Program); the Clinic later established independent Dominican governance and is now a non-profit organization licensed by the Dominican Ministry of Health. Free HIV testing and treatment are provided to over 1,600 patients annually, making it the third largest HIV care center in the country (Clínica de Familia, 2014). At the Clinic, health education is routinely provided to patients, either through written materials or verbally, in waiting rooms, during various types of clinical visits, and in monthly support groups.
Sample and Recruitment
Patients were eligible for participation if they were adult (>18 years of age), HIV positive (verified by their provider), and Spanish-speaking. Recruitment consisted of non-probability, consecutive sampling where providers introduced the study to eligible patients who presented at the Clinic during the study period. Interested individuals were referred to the on-site researcher who further explained the study and obtained verbal informed consent prior to interview administration. Interviews took place in a private space to ensure confidentiality.
Measures
Health Information Behavior Survey
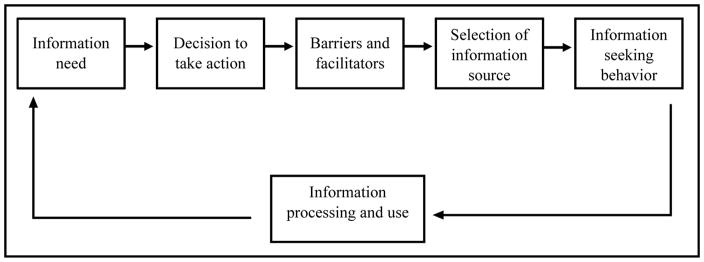
Development of an information behavior survey was guided by an adapted version of Wilson’s model of information behavior (Wilson, 1997). This macro-behavior model generates a comprehensive picture of information flow within a system, emphasizes that information behavior is context specific, and may guide research across fields. The model was adapted to be relevant in the health care context and to show the components represented in this study. Included constructs were re-named to more adequately describe the adapted model as is demonstrated in Figure 1.
Figure 1. Adapted Theoretical Framework.
Context of information need: La Romana, Dominican Republic
Two focus groups, conducted with eight PLWH meeting the same eligibility criteria (Stonbraker et al., 2016b), informed survey development by elucidating the words and phrases that PLWH use to discuss health information and by exploring perceptions of health information in this context. A paper-based survey was then designed for administration during face to face interviews to increase response rates and avoid problems associated with literacy limitations (Ojeda, Flores, Meza, & Morales, 2011). Multiple choice and open-ended questions were developed in Spanish, thus translation was not required. Five techniques to address sensitive topics and elicit complete responses were utilized: indirect questioning, forced responses, motivational language, question formatting, and question order (Fowler, 2014; Ojeda et al., 2011).
The final survey had 64 items: 21 demographic, 13 HIV-related knowledge questions that were part of the 2013 Demographic and Health Survey (DHS) administered in the DR (DHS Program, 2013), and 30 information behavior questions (see supplement for complete list of demographic and knowledge questions). To elucidate information behavior, questions pertaining to the following six components of the theoretical model were developed: (1) information need, defined as the information an individual needs for effective health management; (2) decision to take action, or what initially made participants decide to seek information; (3) barriers and facilitators to information seeking; (4) selection of information source or where individuals prefer to find health information; (5) information seeking behavior such as active or passive information searches; and (6) information processing and use, or an individuals’ ability to articulate understanding and proper utilization of information received. Prior to administration, the survey was pre-tested by three bilingual Dominican experts in health literacy and community health to verify wording and cultural relevance (Polit & Beck, 2012). The survey was pre-tested with the first three study participants and questions that were excessively time consuming or not well understood were modified prior to subsequent administration. Test-retest reliability of this newly developed survey was examined with five participants who agreed to complete the interview a second time. The length of time between the first and second administration ranged from 1.6 to 7.4 (median of 3.4) weeks. Of 64 items, 32 items likely to be stable over time were included. Percent agreement in item responses between the initial and repeat surveys ranged from 84.4 to 96.9%.
Health Literacy Assessment
During interviews, health literacy was measured using the Short Assessment of Health Literacy – Spanish and English (SAHL S&E). This assessment was selected as it has been shown to be correlated with other instruments such as the Short Assessment of Health Literacy for Spanish-speaking Adults (r = 0.88, p<0.05) (Lee, Stucky, Lee, Rozier, & Bender, 2010), has been validated among Spanish-speaking adults (Lee et al., 2010), and can be quickly administered within an interview setting (Stonbraker, Schnall, & Larson, 2015). In the SAHL S&E assessment, participants are asked to pronounce 18 medical words and choose the word most closely associated with each of two alternatives provided. For each word that is correctly pronounced and the appropriate, associated word identified, one point is earned. Scores range from 0 to 18. A participant with a score ≥ 15 is considered to have adequate health literacy and those with ≤ 14 are likely to have low health literacy (Lee et al., 2010). To prevent participant discomfort, the SAHL S&E was not administered to participants who stated they were unable to read and was terminated early if a participant was unable to successfully pronounce and/or associate words in the first three attempts. In both of those cases, the participant was categorized as having low health literacy.
Analytic Strategy
Survey responses were entered into REDCap, an electronic database hosted at Columbia University (Harris et al., 2009). Health literacy was determined based on the SAHL S&E scores and all responses were stratified by health literacy level (adequate or low). Descriptive statistics were calculated and associations between health literacy and responses to HIV-related knowledge questions were assessed using Chi-square or Fisher’s exact tests as appropriate based on cell sizes. These analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC). Responses to open-ended survey questions were categorized by topic and conceptual framework category, and frequencies were generated. Some survey items allowed more than one answer, e.g., “What barriers do people living with HIV face when looking for health information?” In these cases, frequencies were calculated based on the number of expected responses rather than the number of participants.
RESULTS
Participant Characteristics
Of 107 participants, the majority was female (59.8%), Dominican (74.8%), lived in La Romana (57.9%), and had a primary school education or less (68.2%) (Table 1). The average age of participants was 40.8 years (SD=11.2, range=19–75) and the average per person income (total household income divided by the number of people residing there) was 2,592 Dominican Pesos (approximately 60 U.S. Dollars) per month (SD=3,171.2, range=0–17,500). Seven participants indicated there was zero income in their household in the past month and reported living day to day on handouts from their family or by begging. On average, participants had lived with HIV for 7.7 years (SD=5.0, range=0.17–20) and had attended the Clinic for 6.3 years (SD=4.3, range=0.04–16). The sample was reflective of PLWH at the Clinic (Stonbraker, Befus, Lerebours Nadal, Halpern, & Larson, 2016a).
Table 1.
Participant characteristics stratified by health literacy level
| Characteristic | Health Literacy | |
|---|---|---|
| Adequate (N=33) | Low (N=74) | |
|
| ||
| n (%) | n (%) | |
| Gender | ||
| Male | 9 (27.3) | 32 (43.2) |
| Female | 24 (72.7) | 40 (54.1) |
| Transgender | 0 (0.0) | 2 (2.7) |
| Age (Years), Mean (Range) | 38.3 (19 – 70) | 41.9 (20 – 75) |
| Years Living with HIV Diagnosis, Mean (Range) | 8.6 (0.6 – 20) | 7.3 (0.2 – 20) |
| Nationality | ||
| Dominican | 31 (93.9) | 49 (66.2) |
| Haitian | 0 (0.0) | 16 (21.6) |
| Both Dominican and Haitian | 2 (6.1) | 8 (10.8) |
| Other | 0 (0.0) | 1 (1.4) |
| Resides | ||
| La Romana | 25 (75.8) | 37 (50.0) |
| Another City | 7 (21.2) | 26 (35.1) |
| Other Place | 1 (3.0) | 11 (14.9) |
| Highest Level of Education | ||
| No formal education | 0 (0.0) | 12 (16.2) |
| Primary school or less | 8 (24.2) | 53 (71.6) |
| High school or less | 19 (57.6) | 9 (12.2) |
| All or some university | 6 (18.2) | 0 (0.0) |
| Married or in a Serious Relationship | ||
| Yes | 17 (51.5) | 35 (47.3) |
| No | 15 (45.5) | 39 (52.7) |
| Not sure | 1 (3.0) | 0 (0.0) |
| Currently Works Outside the Household | ||
| Yes | 16 (48.5) | 34 (46.0) |
| No | 17 (51.5) | 40 (54.0) |
| Monthly Income (Dominican Pesos), Mean (Range) | 3,619 (0 – 17,500) | 2,133 (0 – 11,700) |
| Time Attending the Clinic (Years), Mean (Range) | 6.9 (0.25 – 15) | 6.0 (0.04 – 16) |
Note: Health literacy was assessed using the Short Assessment of Health Literacy – Spanish and English (SAHL S&E), a tool to measure health literacy that has been validated in Spanish. Scores range from 0 to 18 and a score of 15 or more indicates that a person is likely to have adequate health literacy.
Health Literacy Assessment Scores
The majority of participants (n=74, 69.2%) was identified as having low health literacy (SAHL S&E ≤ 14 [n=23, 21.5%], unable to complete SAHL S&E [n=32, 29.9%], or self-identified as unable to read [n=19, 17.8%]).
HIV-related Knowledge
The proportion of correct responses on HIV-related knowledge questions varied by topic and by participants’ health literacy level. Most participants, regardless of literacy level, knew consistent condom use can prevent transmission of AIDS and that it was possible to get more than one sexually transmitted infection at the same time. However, a significantly higher proportion of those with low health literacy compared to those with adequate health literacy reported HIV could be transmitted via mosquitos (39.2% versus 15.2%, p=0.01) or through witchcraft or other supernatural means (39.2% versus 6.1%, p <0.001) (Table 2). While the proportion of correct responses regarding CD4 count was similar across groups (75.8% and 79.7%), a higher proportion of participants with adequate health literacy compared to low health literacy correctly identified that a low viral load is desirable (45.5% versus 16.2%, p=0.001).
Table 2.
Responses to HIV-related knowledge questions stratified by participants’ health literacy level
| HIV Knowledge Questions | Health Literacy | ||
|---|---|---|---|
|
| |||
| Adequate N=33 |
Low N=74 |
P value | |
|
| |||
| n (%) | n (%) | ||
| A person can get the virus that causes AIDS through mosquito bites. | |||
| No | 28 (84.8) | 45 (60.8) | |
| Yes/Not Sure | 5 (15.2) | 29 (39.2) | 0.01 |
| A person can protect himself from the virus that causes AIDS using a condom every time they have sexual relations.* | |||
| Yes | 31 (94.0) | 71 (96.0) | |
| No/Not Sure | 1 (3.0) | 3 (4.0) | 1.00 |
| A person can get the virus that causes AIDS through witchcraft or other supernatural means. | |||
| No | 31 (93.9) | 45 (60.8) | |
| Yes/Not Sure | 2 (6.1) | 29 (39.2) | <0.001 |
| The virus that causes AIDS can be transmitted from a mother to her baby… | |||
| a. During pregnancy. | |||
| No | 8 (24.2) | 18 (24.3) | |
| Yes/Not Sure | 25 (75.8) | 56 (75.7) | 0.99 |
|
| |||
| b. During birth. | |||
| Yes | 30 (90.9) | 59 (79.7) | |
| No/Not Sure | 3 (9.1) | 15 (20.3) | 0.18 |
|
| |||
| c. During Lactation. | |||
| Yes | 31 (93.9) | 62 (83.8) | |
| No/Not Sure | 2 (6.1) | 12 (16.2) | 0.22 |
|
| |||
| A person can get more than one sexually transmitted infection at the same time. | |||
| Yes | 32 (97.0) | 65 (87.8) | |
| No/Not Sure | 1 (3.0) | 9 (12.2) | 0.17 |
| A person with HIV wants a high number of CD4 cells. | |||
| Yes | 25 (75.8) | 59 (79.7) | |
| No/Not Sure | 8 (24.2) | 15 (20.3) | 0.64 |
| A person with HIV wants a high level of viral load. | |||
| No | 15 (45.5) | 12 (16.2) | |
| Yes/Not Sure | 18 (54.5) | 62 (83.8) | 0.001 |
Note:
1 missing value for this question. Correct answers to questions indicated in bold.
Health Information Behavior
Information need
When asked, “If you could ask one question about your health, what would that question be?”, approximately one third (31.8%) and one half (49.3%) of participants with adequate and low health literacy respectively did not provide a question (Table 3). Of those who responded, more participants with adequate health literacy had questions about the state of the science (progress with vaccine development, pre-exposure prophylaxis, etc.). Participants with low health literacy more commonly asked about transmission (8.8% of responses). A similar percentage of both those with adequate and low health literacy (9.1% and 8.1% of responses respectively) wanted to know more about HIV in general. Participants also wanted to know more about problems not related to HIV, such as about their eyesight or knee pain, how to improve their general health, how to find and manage romantic relationships, and about antiretroviral medications.
Table 3.
Participant responses to health information behavior questions arranged by model construct
| Model Construct | Survey Question and Common Reponses | Health Literacy | |
|---|---|---|---|
| Adequate N=33 |
Low N=74 |
||
| Information need | If you could ask two questions about your health, what would those questions be?* | ||
| No health question identified** | 21 (31.8) | 73 (49.3) | |
| Most frequent topics of health questions | |||
| State of the science (progress on vaccine or cure) | 12 (18.2) | 7 (4.7) | |
| Other health problems not related to HIV | 7 (10.6) | 12 (8.1) | |
| About HIV in general | 6 (9.1) | 10 (6.7) | |
| Transmission (modes, level of risk) | 4 (6.1) | 13 (8.8) | |
| Current health status | 3 (4.5) | 8 (5.4) | |
| How to improve health | 5 (7.6) | 8 (5.4) | |
| About antiretroviral medications | 5 (7.6) | 6 (4.1) | |
| How to find/manage romantic relationships | 0 (0.0) | 5 (3.4) | |
| Other | 3 (4.5) | 6 (4.1) | |
| Decision to take action | What was the main reason you decided to seek healthcare services? | ||
| Experiencing physical symptoms | 11 (23.4) | 36 (48.7) | |
| To verify results obtained in other location | 6 (18.2) | 11 (14.9) | |
| Encouraged by others to seek care | 1 (3.0) | 10 (13.5) | |
| Found out they had been exposed to HIV | 7 (21.2) | 5 (6.8) | |
| To get medical attention/services | 1 (3.0) | 6 (8.1) | |
| To check HIV status | 2 (6.1) | 3 (4.1) | |
| Was pregnant | 2 (6.1) | 2 (2.7) | |
| Other | 3 (9.0) | 1 (1.4) | |
| Barriers and facilitators | When you come to the clinic or take medications, how much support do you feel from your family? | ||
| Has support from ≥ 1 family member(s) | 27 (81.8) | 63 (85.1) | |
| When you come to the clinic or take medications, how much support do you feel from your friends? | |||
| Has support from ≥ 1 friend(s) | 16 (48.5) | 30 (40.5) | |
| Can you please provide two barriers that people living with HIV face when looking for health information?* | |||
| No barrier to access to health information identified** | 9 (13.6) | 58 (39.2) | |
| Barriers commonly mentioned | |||
| Emotional reaction to information | 10 (15.2) | 23 (15.5) | |
| Denial and avoidance of condition | 8 (12.1) | 17 (11.5) | |
| Stigma (rejection and discrimination) | 13 (19.7) | 9 (6.1) | |
| Lack of knowledge | 4 (6.1) | 18 (12.2) | |
| Shyness or embarrassment | 6 (9.1) | 9 (6.1) | |
| Personal traits (general disposition) | 7 (10.6) | 3 (2.0) | |
| Suicidal thoughts | 4 (6.1) | 6 (4.1) | |
| Financial constraint | 2 (3.0) | 1 (0.7) | |
| Other | 5 (7.6) | 5 (3.4) | |
| Selection of information source | What are the best sources or places where participants had learned the most about HIV? | ||
| Identified one source of information | 33 (100.0) | 74 (100.0) | |
| Most commonly identified first source | |||
| Clínica de Familia | 22 (66.7) | 51 (68.9) | |
| Medical professionals | 2 (6.1) | 5 (6.8) | |
| Television | 2 (6.1) | 5 (6.8) | |
| School | 3 (9.1) | 2 (2.7) | |
| Church | 1 (3.03) | 4 (5.4) | |
| Other | 4 (12.1) | 7 (9.5) | |
| Identified a second source of information | 27 (81.8) | 37 (50.0) | |
| Most commonly identified second source | |||
| Clínica de Familia | 7 (25.9) | 8 (21.6) | |
| Internet | 9 (33.3) | 1 (2.7) | |
| Friends or family members | 1 (3.7) | 9 (24.3) | |
| Books/magazines or other print materials | 4 (14.8) | 0 (0.0) | |
| School | 0 (0.0) | 5 (13.5) | |
| Other healthcare center | 3 (11.1) | 5 (13.5) | |
| Radio | 0 (0.0) | 2 (5.4) | |
| Other | 3 (11.1) | 7 (18.9) | |
| Information seeking behavior | When you have a question about your health, how often do you look for the information to answer your question? | ||
| Almost always | 23 (69.7) | 52 (70.3) | |
| Sometimes | 6 (18.2) | 9 (12.2) | |
| Almost never | 4 (12.1) | 12 (16.2) | |
| No response | 0 (0.0) | 1 (1.3) | |
| In the last year, how often did you come to your scheduled appointments? | |||
| Almost always | 30 (90.9) | 67 (90.5) | |
| Sometimes | 3 (9.1) | 7 (9.5) | |
| Information processing and use | How often do you use the information at the clinic to manage your health? | ||
| Almost always | 27 (81.8) | 57 (77.0) | |
| Sometimes | 6 (18.2) | 12 (16.2) | |
| Almost never | 0 (0.0) | 5 (6.8) | |
| How would you rate your ability to use the information provided at the clinic to manage your health? | |||
| Very able | 30 (90.9) | 60 (81.1) | |
| More or less able | 3 (9.1) | 8 (10.8) | |
| Not very able | 0 (0.0) | 6 (8.1) | |
| How many doses of your antiretroviral medications did you miss in the past week? | |||
| 0 | 25 (75.8) | 53 (71.6) | |
| 1–2 | 6 (18.2) | 15 (20.3) | |
| 3 or more | 2 (6.1) | 5 (6.8) | |
| Not prescribed ART or no response | 0 (0.0) | 1 (1.4) | |
| Did you use a condom the last time that you had sexual relations? | |||
| Yes | 24 (72.7) | 54 (73.0) | |
| No | 9 (27.3) | 20 (27.0) | |
Note:
When question encouraged more than one response, data presented as proportion of total responses;
A participant who provided either no response or only one response to the question
Decision to take action
Participants most commonly decided to seek health information when they experienced physical symptoms (23.4% of those with adequate health literacy and 48.7% of those with low health literacy) or because they had received a positive result from another health care center (18.2% and 14.9% depending on health literacy level). Seeking care because of encouragement by others (3% versus 13.5%) or because a participant found out that they had been exposed to HIV (21.2% versus 6.8% depending on health literacy level).
Barriers and facilitators
Compared to those with adequate health literacy, more participants with low health literacy were unable to identify barriers to information seeking (39.2% versus 13.6%). For those who did identify barriers, emotional reactions to a positive diagnosis such as “people go crazy at the beginning” or expressions that the diagnosis “broke them” were commonly identified. Stigma of HIV, including feelings of rejection and discrimination, was the most frequently mentioned barrier by participants with adequate health literacy (19.7%) whereas those with low health literacy more frequently indicated lack of knowledge as a barrier (12.2%). Regardless of health literacy level, denial and avoidance of condition was frequently identified as a barrier to information seeking. Most participants reported feeling supported by at least one family member (over 80% of all participants) when seeking health information whereas 48.5% of those with adequate health literacy and 40.5% of those with low health literacy indicated feeling support from one or more friend(s).
Selection of information source
All participants were able to identify at least one information source; the first source identified by over 65% of participants, regardless of health literacy level, was the Clinic. Only 50% of those with low health literacy identified a second source of information whereas 81.8% of those with adequate health literacy did. Besides the Clinic, other sources of information were the Internet, television, books/magazines and other print materials, other health care centers, school, and friends or family members.
Information seeking behavior
When asked how often participants looked for information to answer their health questions, 69.7% of those with adequate health literacy and 70.3% of those with low health literacy reported that they “almost always” sought the information that they needed. Over 90% of participants also reported that in the previous year, they “almost always” came to the Clinic for their scheduled appointments.
Information processing and use
Over three-fourths of participants said they “almost always” used the information they received in the Clinic to manage their health and indicated feeling “very able” to use the information. Additionally, over 70% of participants, regardless of their health literacy level, indicated that they had not missed a single dose of their prescribed antiretroviral therapy in the previous week. Similarly, more than 70% of participants indicated that they had used a condom during their last sexual encounter. Participants reported their use of information at the Clinic as taking medications as prescribed, getting enough sleep, eating healthily, and using protection during sexual relations.
DISCUSSION
This study aimed to assess the health literacy levels of PLWH in the DR and to explore how health literacy was associated with HIV-related knowledge and influenced overall health information behavior. By SAHL S&E health literacy measurement, less than one third of participants were identified as having adequate health literacy. Furthermore, by adding the proportion of participants who self-identified as not being able to read with the proportion of those who could not complete the first few words on the health literacy assessment, we estimate that almost half (48%) lacked even general literacy. Throughout the literature, methods to assess health literacy are reported to have varying levels of validity and reliability and may not correspond well with other measures of patients’ ability such as educational background or actual knowledge levels (Jordan, Osborne, & Buchbinder, 2011). In our study, participants’ health literacy levels did correspond with other measures that we would have expected, namely, level of education and correct answers on knowledge questions. However, health literacy levels also corresponded to less obvious measures of patient’s ability, such as preferred sources of information (print materials vs. auditory sources) as well as to barriers to information seeking. These findings add to the literature suggesting the SAHL S&E is a valid instrument to quickly measure health literacy among Spanish-speakers in clinical or research settings (Lee et al., 2010).
In knowledge questions, a higher proportion of those with adequate health literacy provided correct answers to all questions except for the question related to CD4 count. This may demonstrate that factors beyond health literacy play a role in patients’ ability to obtain and assimilate health information. For example, more than half of participants with adequate health literacy and over 80% of those with low health literacy were unclear about the interpretation of HIV viral load, a main indicator of disease progression. This indicates that, regardless of health literacy level, complex health information can be difficult to comprehend, especially in stressful situations such as those which arise with management of chronic conditions (Brashers et al., 2000).
Participants in this study demonstrated greater HIV-related knowledge compared to those interviewed in a 2013 national survey of 12,002 households in the DR (DHS Program, 2013). For example, in our sample over 94% of participants regardless of health literacy status indicated that use of condoms can prevent transmission of AIDS compared to 69% to 88% of the 2013 national sample depending on level of education. This suggests that the education offered at the Clinic is helping to improve patients’ overall understanding of HIV. However, the misunderstanding of viral load and methods of transmission indicates that improvement in patient education is still needed.
In this study participants with low health literacy more frequently were either not able, or chose not to, answer questions, reported they were “not sure” of answers, or answered questions incorrectly when compared to participants with adequate health literacy. This may indicate that patients with low health literacy need additional time, more thorough explanations, or visual representations of key ideas in order to grasp intended concepts. These findings are consistent with another study that showed that patients with low health literacy are less likely to ask questions in medical encounters (Katz, Jacobson, Veledar, & Kripalani, 2007). Nurses and other health educators must consider that it may be difficult for patients with low literacy to provide solicited information or formulate necessary questions. Further training for providers working with these patients is warranted so that they can more effectively meet the information needs of their patients (Schiavo, 2014).
The most commonly mentioned barriers to information seeking were emotional responses to information received and stigma, especially around the initial diagnosis. This implies that if there is insufficient support for patients at initial diagnosis, PLWH may avoid seeking further information. Thus, mental health services during all phases of disease progression are critical to enhance wellbeing. This is a new contribution to the literature as existing reports indicate that financial constraints (Bamgbose, Oyesola, & Ogunmodede, 2014), information being too difficult to understand (Hogan & Palmer, 2005), cultural factors (Shedlin & Shulman, 2004), or disease related stigmas (Patel & Dowse, 2013) are the predominant barriers to information seeking. Interestingly, financial constraint was only reported as a barrier to information seeking by a few participants. This could be because HIV services are provided free of charge at the Clinic. It is critical to further elucidate barriers to seeking care and methods to help patients overcome them, as many participants waited to experience physical symptoms before seeking clinical services, a finding that is consistent with the literature (Koenig et al., 2012). Developing and refining community outreach activities that encourage early testing and treatment, provide social and mental health support, and work to reduce stigma at a societal level may help mitigate these challenges.
Cultural or spiritual perceptions of illness may also influence the way individuals seek, obtain, and use health information. Fewer of our sample (60% and 84% depending on health literacy level) indicated that AIDS cannot be transmitted through witchcraft or other supernatural means compared to the 2013 national sample (68% to 96% depending on education level) (DHS Program, 2013), but rates were still high. One possible explanation is the geographic proximity of La Romana to numerous bateyes (settlements of sugar cane workers) where strong spiritual influences may be encountered (Rojas et al., 2011). Regardless of the reason, such cultural or spiritual beliefs may influence a person’s perception of illness and create discordant views of health between patients and providers. These disparate opinions may lead to mistrust in providers, and may lessen motivation to seek services (Person et al., 2006). If health care providers and the wider organization do not consider their patients’ beliefs and provide information from only a biologic standpoint, the information may not be meaningful to patients or patients may simply not be receptive (Lettenmaier, Kraft, Raisanen, & Serlemitsos, 2014).
There are limitations to this study. All participants were recruited at a single health clinic and, therefore, already seeking care in an environment where health information was readily available. Responses were self-reported during interviews and despite attempts to minimize social desirability bias, negative responses may have been under-reported while positive responses, such as optimal treatment adherence, could have been over-reported. Additionally, health information needs may vary between high risk groups such as men who have sex with men and female sex workers (Stonbraker & Larson, 2016) but that was outside the scope of this study. Lastly, we limited recruitment to Spanish speaking participants so our findings do not include the approximately 6% of the patient population at the Clinic who predominantly speak Haitian Creole. Future studies may assess the information behavior of those who speak Haitian Creole and consider how to more effectively provide health information to this population.
Despite limitations, findings of this study demonstrate that even among individuals actively engaged in an environment where health information was regularly provided, who may have been under-reporting negative responses, there were unmet information needs, and the information that was received was not always well understood. The first step to address this issue is to determine what specific information needs to be included in health education as few studies have explored HIV-related information needs (Stonbraker & Larson, 2016) and the relevance of certain educational topics, such as the importance of understanding laboratory results, is unclear (Laws, Danielewicz, Rana, Kogelman, & Wilson, 2015). The second step is to explore methods that may improve health communication. One emerging strategy to improve information exchange between health care providers and their patients is to use information visualizations to facilitate communication (Garcia-Retamero, Okan, & Cokely, 2012; Houts, Doak, Doak, & Loscalzo, 2006). Other communication techniques that may be used among similar populations are the “teach-back” method, speaking more slowly, presenting only a few concepts then verifying understanding, and using simpler language (Dickens, Utley-Smith, Stott, & Relf, 2013).
The most salient point from this research is that existing health education is not penetrating and as a result, it is the collective responsibility of nurses, researchers, and other health care providers to design and evaluate methods to more effectively provide health information to patients. Additionally, participants indicated varying cultural or spiritual perceptions of illness, which may influence how they view information received in a clinical setting, a factor that must be considered if health communication is to be effective. These findings are relevant in limited resource settings globally, as other vulnerable populations may experience similar barriers to acquiring health information. Determining what information patients need and exploring evidence-based, culturally appropriate methods to communicate that information to patients with low health literacy are crucial next steps to ensure individuals can obtain and understand the information they need to manage their health.
Supplementary Material
Acknowledgments
During this research, the authors SS and HC were funded as pre-doctoral fellows on the Training in Interdisciplinary Research to Prevent Infections grant (T32NR013454), funded by National Institute of Nursing Research, National Institutes of Health. During the writing and subsequent revisions, the author SS was supported by the Reducing Health Disparities through Informatics (RHeaDI) training grant (T32NR007969) also funded by the National Institute of Nursing Research, National Institutes of Health. The authors would like to thank Dr. Robert Lucero for his help in conceptualizing this research design and Emelin Martinez, Kristy Medina, and Nayrobi Rivera for their valuable contributions to the language and cultural relevance of this health information behavior assessment. Also, thank you to Niurka Suero-Tejeda for her help with coding open-ended responses.
References
- Aboud FE, Singla DR. Challenges to changing health behaviours in developing countries: a critical overview. Social Science and Medicine. 2012;75(4):589–594. doi: 10.1016/j.socscimed.2012.04.009. [DOI] [PubMed] [Google Scholar]
- Bamgbose O, Oyesola O, Ogunmodede T. Information Needs of People Living with HIV/AIDS in Ibadan Metropolis. Journal of Education and Practice. 2014;5(37):198–203. [Google Scholar]
- Berkman N, Sheridan S, Donahue K, Halpern D, Crotty K. Low health literacy and health outcomes: an updated systematic review. Annals of Internal Medicine. 2011;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- Brashers DE, Neidig JL, Haas SM, Dobbs LK, Cardillo LW, Russell JA. Communication in the management of uncertainty: The case of persons living with HIV or AIDS. Communications Monographs. 2000;67(1):63–84. [Google Scholar]
- Clínica de Familia. [Date Accessed: May 2017];Reporte Anual. 2014 Retrieved from http://www.clinicadefamilia.org.do/wordpress/wp-content/uploads/2012/07/Reporte-Anual-2014_Cl%C3%ADnica-de-Familia-La-Romana.pdf.
- De Boni R, Veloso V, Grinsztejn B. Epidemiology of HIV in Latin America and the Caribbean. Current Opinion in HIV and AIDS. 2014;9(2):192–198. doi: 10.1097/COH.0000000000000031. [DOI] [PubMed] [Google Scholar]
- DHS Program. [Date Accessed: May 2017];Dominican Republic: Standard DHS, 2013. 2013 Retrieved from http://dhsprogram.com/what-we-do/survey/survey-display-439.cfm.
- Dickens A, Utley-Smith Q, Stott G, Relf M. Evaluation of communication techniques used by HIV specialty providers caring for patients with low health literary in an outpatient HIV clinical setting. Journal of Nursing Education & Practice. 2013;3(7) [Google Scholar]
- Figueroa J. Review of HIV in the Caribbean: significant progress and outstanding challenges. Current HIV/AIDS Reports. 2014;11(2):158–167. doi: 10.1007/s11904-014-0199-7. [DOI] [PubMed] [Google Scholar]
- Fisher K, Erdelez S, McKechnie L. Theories of Information Behavior. Medford, New Jersey: Information Today, Inc; 2005. [Google Scholar]
- Fowler F. Survey Research Methods. 5. Boston, MA: Sage Publications, Inc; 2014. [Google Scholar]
- Garcia-Retamero R, Okan Y, Cokely ET. Using visual aids to improve communication of risks about health: a review. The Scientific World Journal. 2012;2012 doi: 10.1100/2012/562637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris P, Taylor R, Thielke R, Payne J, Gonzalez N, Conde J. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogan T, Palmer C. Information preferences and practices among people living with HIV/AIDS: results from a nationwide survey. Journal of the Medical Library Association. 2005;93(4):431. [PMC free article] [PubMed] [Google Scholar]
- Houts P, Doak C, Doak L, Loscalzo M. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Education and Counseling. 2006;61:173–190. doi: 10.1016/j.pec.2005.05.004. [DOI] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. [Date Accessed: May 2017];HIV and AIDS estimates from the Dominican Republic. 2015 Retrieved from http://www.unaids.org/en/regionscountries/countries/dominicanrepublic.
- Jordan J, Osborne R, Buchbinder R. Critical appraisal of health literacy indices revealed variable underlying constructs, narrow content and psychometric weaknesses. J Clin Epidemiol. 2011;64:366–379. doi: 10.1016/j.jclinepi.2010.04.005. [DOI] [PubMed] [Google Scholar]
- Katz MG, Jacobson TA, Veledar E, Kripalani S. Patient literacy and question-asking behavior during the medical encounter: a mixed-methods analysis. Journal of General Internal Medicine. 2007;22(6):782–786. doi: 10.1007/s11606-007-0184-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig S, Rodriguez L, Bartholomew C, Edwards A, Carmichael T, Barrow G, … Quava-Jones A. Long-term antiretroviral treatment outcomes in seven countries in the Caribbean. Journal of Acquired Immune Deficiency Syndromes. 2012;59(4) doi: 10.1097/QAI.0b013e318245d3c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laws MB, Danielewicz M, Rana A, Kogelman L, Wilson IB. Health literacy in Hiv treatment: accurate understanding of key biological treatment principles is not required for good Art adherence. AIDS and Behavior. 2015;19(4):635–644. doi: 10.1007/s10461-014-0931-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Stucky B, Lee J, Rozier R, Bender D. Short assessment of health literacy-spanish and english: a comparable test of health literacy for Spanish and English speakers. Health Services Research. 2010;45:1105–1120. doi: 10.1111/j.1475-6773.2010.01119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lettenmaier C, Kraft JM, Raisanen K, Serlemitsos E. HIV communication capacity strengthening: a critical review. JAIDS, Journal of Acquired Immune Deficiency Syndromes. 2014;66:S300–S305. doi: 10.1097/QAI.0000000000000238. [DOI] [PubMed] [Google Scholar]
- Ojeda L, Flores L, Meza R, Morales A. Culturally competent qualitative research with Latino immigrants. Hispanic Journal of Behavioral Sciences. 2011;33(2):1–20. [Google Scholar]
- Patel S, Dowse R. Understanding the medicines information-seeking behaviour and information needs of South African long-term patients with limited literacy skills. Health Expectations. 2013;18(5):1494–1507. doi: 10.1111/hex.12131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Person B, Addiss D, Bartholomew L, Meijer C, Pou V, Van den Borne B. Health-seeking behaviors and self-care practices of Dominican women with lymphoedema of the leg: implications for lymphoedema management programs. Filaria Journal. 2006;5(1):13. doi: 10.1186/1475-2883-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polit D, Beck C. Nursing Research: Generating and Assessing Evidence for Nursing Practice. 9. Philadelphia PA: Wolters Kluwer Health | Lippincott WIlliams & Wilkins; 2012. [Google Scholar]
- Rojas P, Malow R, Ruffin B, Rothe E, Rosenberg R. The HIV/AIDS epidemic in the Dominican Republic: Key contributing factors. Journal of the International Association of Providers of AIDS Care. 2011;10(5):306–315. doi: 10.1177/1545109710397770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiavo R. Health communication in health disparities settings. Journal of Communication in Healthcare. 2014;7(2):71–73. [Google Scholar]
- Shedlin M, Shulman L. Qualitative needs assessment of HIV services among Dominican, Mexican and Central American immigrant populations living in the New York City area. AIDS Care. 2004;16(4):434–445. doi: 10.1080/09540120410001683376. [DOI] [PubMed] [Google Scholar]
- Stonbraker S, Befus M, Lerebours Nadal L, Halpern M, Larson E. Evaluating the utility of provider-recorded clinical status in the medical records of HIV positive adults in a limited-resource setting. International Journal of STD and AIDS. 2016a;28(7) doi: 10.1177/0956462416663990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stonbraker S, Castillo H, Halpern M, Lerebours Nadal L, Cushman LF, Smaldone A, Larson E. The health information behavior of HIV positive adults in La Romana, Dominican Republic. Paper presented at the Eastern Nursing Research Society Annual Conference; Pittsburgh, PA. 2016b. [Google Scholar]
- Stonbraker S, Larson E. Health-information needs of HIV-positive adults in Latin America and the Caribbean: an integrative review of the literature. AIDS Care. 2016;28(10):1223–1229. doi: 10.1080/09540121.2016.1173645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stonbraker S, Schnall R, Larson E. Tools to measure health literacy among Spanish speakers: An integrative review of the literature. Patient Education and Counseling. 2015;98(12):1513–1523. doi: 10.1016/j.pec.2015.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wawrzyniak AJ, Ownby RL, McCoy K, Waldrop-Valverde D. Health literacy: impact on the health of HIV-infected individuals. Current HIV/AIDS Reports. 2013;10(4):295–304. doi: 10.1007/s11904-013-0178-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson T. Information behaviour: an interdisciplinary perspective. Information Processing & Management. 1997;33(4):551–572. [Google Scholar]
- Zhang N, Terry A, McHorney C. Impact of Health Literacy on Medication Adherence A Systematic Review and Meta-analysis. Annals of Pharmacotherapy. 2014;48(6):741–751. doi: 10.1177/1060028014526562. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.