Abstract
Purpose
To determine whether an advance care planning (ACP) decision aid for could improve communication about end-of-life treatment wishes between patients with amyotrophic lateral sclerosis (ALS) and their clinicians.
Methods
Fourty-four patients with ALS (≥21, English-speaking, without dementia) engaged in ACP using an interactive computer-based decision aid. Before participants completed the intervention, and again 3 months after, their clinicians reviewed 3 clinical vignettes, and made treatment decisions (n=18) for patients. After patients indicated their agreement with the team’s decisions, concordance was calculated.
Results
The mean concordance between patient wishes and the clinical team decisions was significantly higher post-intervention (post=91.9%, 95% CI=87.8, 96.1, vs. pre=52.4%, 95% CI=41.9, 62.9; p <.001). Clinical team members reported greater confidence that their decisions accurately represented each patient’s wishes post-intervention (mean=6.5) compared to pre-intervention (mean=3.3, 1=low, 10=high, p<.001). Patients reported high satisfaction (mean=26.4, SD=3.2; 6=low, 30=high) and low decisional conflict (mean=28.8, SD=8.2; 20=low, 80=high) with decisions about end-of-life care, and high satisfaction with the decision aid (mean=52.7, SD=5.7, 20=low, 60=high,). Patient knowledge regarding ACP increased post-intervention (pre=47.8% correct responses vs. post=66.3%; p <.001) without adversely effecting patient anxiety or self-determination.
Conclusion
A computer-based ACP decision aid can significantly improve clinicians’ understanding of ALS patients’ wishes regarding end-of-life medical care.
Keywords: Advance Care Planning, Advance Directive, Living Will, Decision Aid, Surrogate Decision Making
Introduction
Amyotrophic lateral sclerosis (ALS) is a progressive, degenerative neurological disorder that inevitably results in functional decline and death, typically preceded by some form of surrogate decision-making at the end of life. Patients with ALS survive an average of 27–43 months after the onset of symptoms (1, 2), and though only a minority of these patients undergo tracheostomy and mechanical ventilation, such interventions commonly occur under emergency conditions in the absence of advance directives (3). As with other medical conditions, when patients with ALS fail to communicate their wishes for future medical treatment, the consequence is often sub-optimal medical decision-making during a crisis (4, 5), unwanted treatment and associated financial burden to patients, families, and society (6, 7), as well as moral distress for those who must make surrogate healthcare decisions (8–10).
Though patients most often rely on their families and physicians to speak on their behalf during a crisis, studies have shown that neither group accurately predict patients’ wishes for life-sustaining treatments (11–15). Furthermore, fewer than 30% of American adults create advance directives to document their wishes (16–20); and even among patients with ALS fewer than 40% have recorded their attitudes and wishes regarding life-sustaining ventilation, resuscitation, artificial nutrition, and hydration (21, 22). In response to the need for better communication, the American Academy of Neurology and the European Federation of Neurological Societies have published guidelines emphasizing the importance of having planning discussions about end-of-life issues (23).
Improving communication between patients with ALS and their healthcare providers is an important way to help respect ALS patients’ wishes. Individuals with ALS want to be involved in end-of-life decisions, particularly those involving tracheostomy and mechanical ventilation (24, 25). Importantly, ALS patients who receive such interventions often become unable to communicate effectively (26), and studies have shown that most would want these life-sustaining measures discontinued under certain conditions (27). Organizations such as the ALS Association (28) and the Muscular Dystrophy Association (29) have developed educational materials to facilitate decisions about living with ALS. And it has been proposed that an ALS-specific advance care planning (ACP) instrument could help facilitate discussion of ACP for these patients (30).
Despite these important steps, a central challenge to the goal of effective ACP is being able to ensure that people have ready access to high quality materials and/or facilitation. The intervention used in the present study (Making Your Wishes Known: Planning Your Medical Future, or MYWK) is an online decision aid created in large part to address this need. It provides a standardized, facilitated process that prepares patients for end-of-life decision-making, and generates an advance directive document that can then be shared and discussed with family members and healthcare providers.
The present study assesses the impact of MYWK on communication between patients with ALS and clinicians who treat them with regard to end-of-life treatment wishes. We hypothesized that the ALS team’s understanding of patients’ wishes would significantly improve after patients used this decision aid.
Materials and Methods
The broad study design involved asking the ALS team to consider several clinical vignettes, and then make hypothetical end-of-life decisions about them. This was done at baseline, and again after patients completed MYWK and shared with the team the advance directive document generated by this decision aid. Patients were then shown the ALS team’s decisions, and asked to indicate whether they agreed or disagreed with each decision. A concordance score was then calculated as described below.
Patient Recruitment, Screening, and Eligibility
Following approval from the institutional Human Subjects Protection Office, patients were recruited from an interdisciplinary ALS clinic at Penn State Hershey Medical Center. Over an 18 month period, letters were sent to all patients scheduled for appointments, and follow-up phone calls were made to all patients who did not return an opt-out form. Interested patients 21 years or older then met with the study coordinator at their next scheduled visit and were asked to provide informed consent. Consenting individuals were screened to ensure they 1) were English speaking; 2) could read at 8th grade level (greater than 25 on the WRAT-3 (31)); 3) did not have evidence of dementia (greater than 23 on Folstein Mini-Mental Status Examination (32)); 4) had at least one previous visit to the ALS Clinic; and (as determined by the patient’s ALS physician) 5) could communicate effectively either verbally or through the use of an alternative/augmentative communication device; 6) had sufficient physical stamina to tolerate the study protocol; and 7) had an estimated life expectancy at enrollment of at least 3 months. Patients were sequentially recruited until the target number of 50 enrollees was reached. Patients who were ineligible for the study but still wished to use the decision-aid were permitted to do so, but no data were collected. Eligible patients who declined participation (n=33) were asked to complete a brief non-participant questionnaire.
ALS Health Care Team Recruitment, Screening and Eligibility
The ALS healthcare team was recruited from the interdisciplinary ALS clinic at Penn State Hershey Medical Center. This 15 member team consisted of physicians, nurses, physical and occupational therapists, as well as a speech therapist, dietician, mental health counselor, social worker, and pastoral counselor. All ALS team members provided informed consent for their participation in this study, and no member of the ALS team declined to participate.
Decision Aid Intervention
Making Your Wishes Known (MYWK) was developed to educate individuals about advance care planning, help them clarify and articulate their values, and then (using an algorithm based on multi-attribute utility theory) (33, 34) translate their wishes and goals into an actionable medical plan (35, 36). MYWK is intended to facilitate, not replace, discussions between patients and healthcare providers, and previous studies with non-ALS patients demonstrated that people who used the program reported high levels of satisfaction, demonstrated improved knowledge about ACP, rated the advance directive generated by MWYK as an accurate and reliable representation of their wishes, and experienced no adverse effect on either hope or anxiety (37–39). A prior pilot study of 17 patients with ALS yielded similar results (40).
MYWK uses an interactive, multi-media format to: 1) provide tailored education about common medical conditions that can result in decisional incapacity, as well as medical treatments often introduced in life-or-death situations; 2) guide individuals to choose a spokesperson, prioritize values and goals, and match treatment options with priorities; and 3) translate individual values and preferences into a detailed advance directive document. Participants used a laptop computer to access MYWK. Individuals with insufficient upper extremity strength and/or coordination communicated their responses to the research assistant (or loved one, if such a person had accompanied them), who operated the computer mouse for them. Upon completing the program, participants received a printed copy of their personalized advance directive.
Patient Measures
Baseline measures included: 1) Demographics and Health Assessment (22 items); 2) Self-Determination (8 items, adapted from Pellino (41), assessing individuals’ sense of control over future treatments); 3) Advance Care Planning Knowledge (27 items, previously described (42), assessing knowledge of the advance care planning process and the clinical decisions patients often face at the end of life); 4) Anxiety (State Trait Anxiety Inventory (43)); 5) Functional Status (ALS Functional Rating Scale-Revised ALSFRS-R (44)); and 6) Quality of Life (ALS-Specific QoL Scale (45)).
Post-intervention patient measures included: 1) Self-Determination and ACP Knowledge (same as pre-intervention); 2) Satisfaction with Advance Care Planning (15 items, assessing comprehensibility, length, pace, amount of information, balance, and overall satisfaction); 3) Decisional Conflict (6 items, assessing discomfort/uncertainty about decisions (46)); 4) Satisfaction with Decision (6 items (47)); and 5) Time and Effort (3 items).
ALS Team Measures
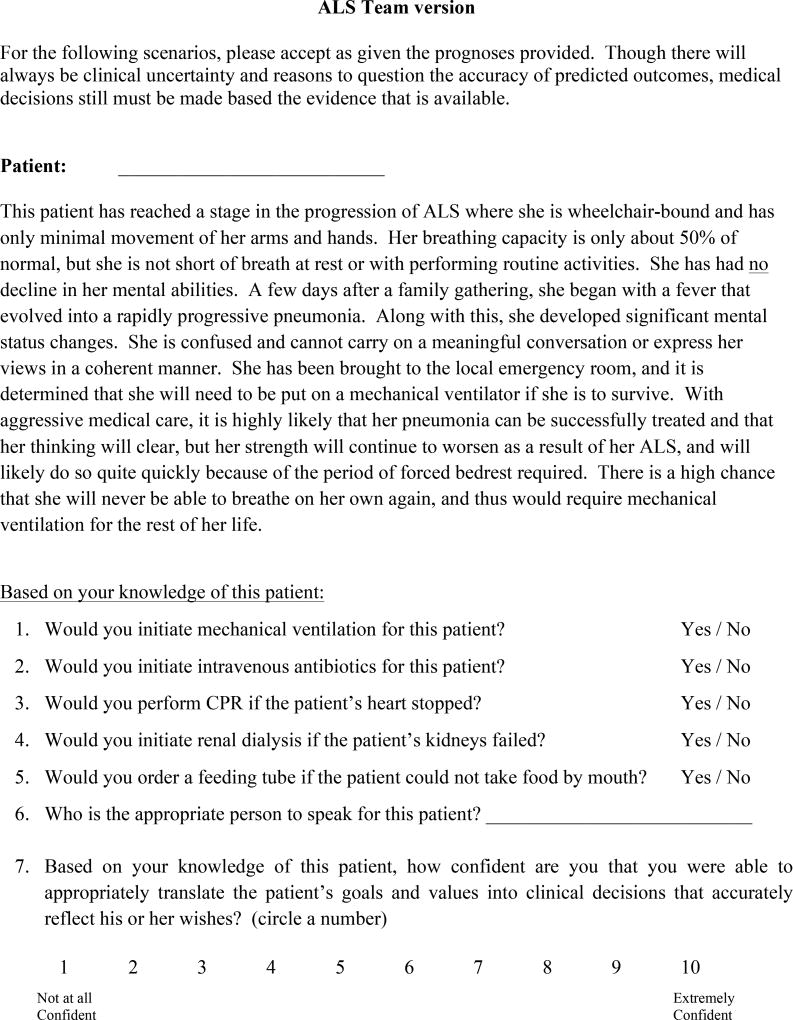
Every 3 months ALS patients undergo a half-day clinical evaluation, after which the ALS team convenes an interdisciplinary meeting. At these meetings ALS team members were asked to discuss three clinical vignettes describing events that would prompt the need for surrogate decision making. For each patient, the ALS team discussed the three scenarios until consensus was reached about what hypothetical medical decisions would be appropriate for that patient (see Figure 1). This was done twice: prior to the patient having used MYWK, and at the patient’s next clinic visit after they had completed MYWK and a copy of their advance directive had been shared with the ALS team. Following each discussion, the ALS team rated their confidence that their decisions accurately reflected the patient’s wishes (10-point Likert-style scale, where 1=low, and 10=high confidence).
Figure 1.
Patient-ALS Team Concordance Calculation
In the weeks following their post-intervention ALS clinic appointment, patient participants were sent the 3 clinical vignettes that had been shared with the ALS team. The patient and physician versions were worded slightly differently. For example, patients were asked “…which of the following would you want and not want? Mechanical ventilation if your breathing worsens (Yes or No), while physicians were asked “Based on your knowledge of this patient, would you initiate mechanical ventilation?” In subsequent phone interviews, the ALS team’s post-intervention decisions were shared with the patients, who were then asked whether they agreed with each decision. Each question-item counted for one point –however, to avoid falsely inflating the concordance score, decisions about who should serve as the patient’s surrogate decision-maker were counted just once (rather than once for each vignette). A concordance score was calculated (using patients’ responses during these telephone interviews) by summing the number of treatment decisions for which patient and ALS team responses were identical, dividing by the total number of treatment decisions, and multiplying by 100 (score range = 0–100%).. The rationale for asking patients whether they agreed or disagreed with the ALS team’s responses (rather than asking them to respond to the vignettes by themselves, i.e., without knowing the clinical team’s opinion) was that this was felt to more closely resemble typical patient involvement in clinical decision making.
Statistical analysis
All analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC), and statistical significance was set at p<0.05. All variables were summarized with frequencies and percentages or means, medians, standard deviations, and quartiles prior to comparisons being made. The distribution of continuous variables was assessed using histograms and box plots. A comparison of pre-intervention to post-intervention mean knowledge was made using a paired t-test. Mean concordance percentage for total and for individual vignettes as well as for procedures, average confidence overall and for the individual vignettes, self-determination, and anxiety were compared using a Wilcoxon signed-rank test due to their distributions being skewed or ordinal in nature.
Results
Completion Rates and Time Spent
Of the 130 eligible patients followed by the ALS team, 17 returned “opt-out” cards, and 33 declined in person. The remaining individuals were approached sequentially until we met our enrollment goal of 50 participants. For these, demographics were calculated for 44 participants (because 6 patients were too ill to attend the research study visit), team confidence was calculated for 43 participants (because 1 patient completed the intervention but never returned for a subsequent ALS clinic appointment), and concordance was calculated for 42 participants (because 1 patient could not be reached after their subsequent clinic visit).
Patient Demographics and Experience with Advance Care Planning
Participants’ mean age was 57.7 years (range=34–78) and the majority were white, married, and had at least a high school education, and moderate physical impairment (See Table 1 for Demographics). The only difference identified among patients who opted out or declined participation (n=50) was that non-participants were more likely to be female (56%) compared to study participants (34%).
Table 1.
Participant Demographic Characteristics (n=44)
| Characteristic | Percent (unless otherwise noted) |
|---|---|
| Age in years, mean (range) | 57.7 ± 11.3 (34–78) |
| Gender | |
| Female | 34.1 |
| Male | 65.9 |
| Race | |
| White | 100.0 |
| Duration of disease (months) | |
| Mean (SD) | 28.9 ± 25.2 |
| ALSFRS-R score* | |
| Mean (SD) | 36.3 ± 7.9 |
| ALSSQOL-R score** | |
| Mean, (SD) | 7.5 ± 1.0 |
| Highest education | |
| Some high school | 6.8 |
| High school graduate or GED | 25.0 |
| Some college or technical school | 25.0 |
| College graduate | 25.0 |
| Graduate or professional school | 18.2 |
| Religion | |
| Catholic | 18.2 |
| Protestant | 59.1 |
| Other | 11.4 |
| No formal religion | 11.4 |
| Marital status | |
| Never married | 6.8 |
| Married or Domestic partnership | 81.8 |
| Divorced or Legally separated | 2.3 |
| Widowed | 9.1 |
| Employment status | |
| Retired | 50.0 |
| Employed full-time | 27.3 |
| Not currently employed | 13.6 |
| Disabled | 9.1 |
ALS Functional Rating scale ranges from 0–48, with higher scores indicating greater function.
ALS-Specific Quality of Life scale ranges from 1–10, with higher scores indicating better quality of life (n=39).
Approximately half of participants reported having read or heard “a lot” (25%) or “a fair amount” (27%) about advance care planning or living wills, while 16% reported having heard almost nothing about them. Half of participants had prepared some form of advance directive prior to enrolling in the study, and half had also formally assigned someone as their spokesperson. All but four participants reported owning a computer (average weekly use=20 hours, range 0–56), and the majority of participants (91%) reported feeling comfortable using a computer.
Participants spent an average of 16 minutes to complete pre-intervention questionnaires, 77 minutes to complete the computer intervention, and 21 minutes for post-intervention questionnaires, with none reporting that completion of the study activities was burdensome.
ALS Team Decisions
Pre-intervention ALS team decisions were recorded for all 50 patient-participants, and post-intervention decisions were recorded for 43 (6 were too ill to attend the research study visit, and 1 completed the intervention but never returned for a subsequent ALS clinic appointment).
Decision Concordance and Confidence
Pre-intervention, patients agreed with 52.4% of the ALS team’s decisions for the clinical vignettes (18 total decisions). Post-intervention, concordance increased to 91.9% (p<.001) (Table 2). Additionally, the ALS team’s confidence that their decisions accurately represented patients’ wishes was significantly higher post-intervention, after they had reviewed the patients’ MYWK-generated advance directive (pre-intervention mean confidence=3.3 vs. post-intervention=6.5, where 1=low and 7=high confidence, see Table 2).
Table 2.
Patient-Provider Decision Concordance and Provider Decisional Confidence
| Concordance (%)* | N | Baseline | Post-Intervention | P-value |
|---|---|---|---|---|
| Mean (95% CI) | Mean (95% CI) | |||
| Total concordance | 42 | 52.4 (41.9, 62.9) | 91.9 (87.8, 96.1) | <0.001 |
| Vignette #1 | 42 | 51.6 (40.8, 62.4) | 96.4 (94.0, 98.9) | <0.001 |
| Vignette #2 | 42 | 55.2 (43.6, 66.7) | 94.8 (91.3, 98.4) | <0.001 |
| Vignette #3 | 42 | 50.4 (38.1, 62.7) | 89.3 (83.0, 95.6) | <0.001 |
| Mechanical ventilation | 42 | 54.8 (43.1, 66.5) | 81.4 (74.4, 88.5) | <0.001 |
| Dialysis | 42 | 48.4 (34.6, 62.2) | 79.4 (69.1, 89.6) | <0.001 |
| Feeding Tube | 42 | 53.2 (40.6, 65.8) | 70.6 (60.3, 81.0) | <0.001 |
| CPR | 42 | 47.6 (33.1, 62.2) | 88.9 (80.7, 97.1) | <0.001 |
| Antibiotics | 42 | 57.9 (44.4, 71.5) | 71.4 (60.1, 82.8) | 0.073 |
| Confidence (1=low, 10=high) * | ||||
| Mean confidence | 43 | 3.3 (2.5, 4.1) | 6.5 (5.7, 7.2) | <0.001 |
| Vignette #1 confidence | 43 | 3.4 (2.6, 4.3) | 6.6 (5.8, 7.4) | <0.001 |
| Vignette #2 confidence | 43 | 3.4 (2.5, 4.8) | 6.5 (5.7, 7.3) | <0.001 |
| Vignette #3 confidence | 43 | 3.1 (2.3, 3.8) | 6.3 (5.4, 7.1) | <0.001 |
Wilcoxon Signed Rank test
Because 1 participant could not be reached after the ALS team made decisions, a discrepancy exists between the numbers used to calculate Concordance (n=42) vs. Confidence (n=43) scores.
Satisfaction with Advance Care Planning
Patients reported high overall satisfaction with the ACP decision aid (mean=9.1 ± 0.9, 1=low and 10=high), as well as for 12 specific tasks (mean=52.7 ± 5.7, 12=low and 60=high), such as providing information about medical conditions and treatments, clarifying values, choosing a spokesperson, and preparing to discuss one’s wishes with others. Patients also reported that the decision aid-generated advance directive was highly accurate in reflecting their wishes (mean=9.4 ± 0.8, 1=low and 10=high).
Impact on Advance Care Planning Knowledge
Participants’ ACP knowledge increased significantly (p<0.001) from a mean of 47.8% (CI=42.8, 52.9) correct answers at baseline to 66.3% (CI=62.8, 69.7) post-intervention.
Impact on Self-Determination, Anxiety, and Decisional Conflict
Participants had a strong sense of self-determination at baseline (mean=35.0, CI= 33.8, 36.2; 8=low, 40=high), which increased significantly (p=0.034), albeit modestly, following the intervention (mean=36.1, CI=34.9, 37.3). Participants’ anxiety was low at baseline (mean=30.5, CI=27.8, 33.1;, 20=low, 80=high), and decreased slightly post-intervention, though not significantly (mean=28.7, CI=26.0, 31.4; p=0.075). Participants reported low levels of decisional conflict for the treatment decision made for the clinical vignettes (mean 28.8 ± 8.2, 16=low, 80=high).
Discussion
This study found that clinicians’ decisions about future end-of-life care were better aligned with patients’ actual wishes after patients completed an online decision aid and shared the advance directive document that it generated. After the intervention, the medical team also reported significantly greater confidence in the accuracy of their treatment decisions.
These findings are noteworthy given the inevitable clinical course faced by patients with ALS, and the observation that physicians are not accurate at predicting patients’ preferences for end-of-life care (48). Hence, a tool that assists healthcare providers to better understand patients’ wishes can help them both engage patients in ACP discussions, and make treatment decisions that are consistent with patients’ wishes.
We do not have detailed information about what happened in the time interval between the intervention and the final discussion, so it is difficult to know with certainty what accounts for this large increase in patient-ALS team agreement. Some of the improvement in concordance may have resulted from direct discussions that improved communication between the patient and the clinical team, which itself is a central goal of MYWK. However, it does not appear that the increased concordance was simply a result of improvement over time (e.g. the clinical team becoming more sensitized and skilled as the study progressed, and hence interacting differently with patients recruited later in the study). Specifically, we found that the 52% concordance at baseline was no different at the end of the 18-month study, nor were there significant differences between early versus end-of-study post-intervention concordance scores.
Before deciding how best to respect a patient’s wishes, clinicians must first determine which treatment options are medically appropriate. The treatment options in this study were limited to interventions that typically would qualify as “medically indicated.” Accordingly our findings may not be generalizable to situations in which patients desire interventions that are medically inappropriate. To the extent that an ACP decision aid can help patients better appreciate which interventions are and are not medically warranted, this too is a benefit.
Consistent with previous studies involving other patient populations, we found that after using the decision aid, patients’ knowledge of ACP increased, and patients expressed high levels of satisfaction with MYWK (37, 40, 42, 49, 50). So too, there were no adverse effects on anxiety, which should help allay concerns some clinicians have about discussing end-of-life issues with patients.
Taken together, these findings suggest that MYWK can be a valuable tool for busy clinicians whose multiple competing obligations make it is increasingly challenging to find sufficient time to educate patients about end-of-life decisions, help them clarify values, and explain the clinical implications of ACP decisions. Preparing patients to have more informed conversations with members of their healthcare team not only can help patients deal with this sensitive topic, but can help clinicians adhere to professional guidelines about ACP.
Limitations
Like all studies, this one has certain limitations. First, the study design did not include a control group, so it is difficult to know with certainty that the improvement in concordance is not attributed to factors other than the decision aid. Second, the main outcome was concordance with decisions made in response to clinical vignettes, not actual decisions. What people decide in real life may differ from decisions involving hypothetical vignettes. Third, the study was conducted at a single institution with low ethnic diversity, and this could affect generalization to other populations. However, the age, male predominance, and ALS-Specific QOL scores of the subjects reflect those in other, larger studies of ALS patients (45). Fourth, the concordance was based on patients’ post-intervention views (rather than comparing patients’ ‘pre-intervention agreement with the ALS team’s pre-intervention decisions’ to their ‘post-intervention agreement with the ALS team’s post-intervention decisions’). The rationale for this approach was that introducing the vignettes prior to the intervention risked introducing bias insofar as the vignettes themselves could constitute an ACP intervention. Additionally, prior research (51) has shown stability in patients’ overall preferences, suggesting that patients’ wishes would not change dramatically over the 3 months of their involvement in the study. Finally, asking patients to agree or disagree with the clinical team’s treatment decisions may have introduced social desirability bias. That said, the clinical reality is that patients make decisions in response to the options and recommendations given to them by clinicians. Additionally, the vignettes and accompanying questions actually sent to patients were framed for patients (Which of the following medical treatments would you want in the circumstances described?), not physicians; and the questions themselves were unanswered (i.e., the ALS team’s responses were not recorded on the materials sent to patients).
Conclusions
The present study suggests that an online decision aid is an effective approach for helping patients with ALS engage in advance care planning, and for helping ALS team members have a better understanding of patients’ wishes regarding end-of-life care. Tools that can help patients and clinicians agree on treatment decisions that are consistent with patients’ values and goals are particularly valuable for patients with progressive, degenerative diseases such as ALS.
Acknowledgments
This research was supported by a grant from the Emily Davie and Joseph S. Kornfeld Foundation, administered by the Greenwall Foundation.
Footnotes
Author Disclosure Statement
Two of the authors (BHL & MJG) have intellectual property and copyright interests for the decision aid used in this study, Making Your Wishes Known: Planning Your Medical Future (MYWK), which is available online free of charge. A version of MYWK that can be widely distributed is currently under development in partnership with a private commercial enterprise.
“This is an Accepted Manuscript of an article published by Taylor & Francis in Amyotrophic lateral sclerosis & frontotemporal degeneration on March 5, 2017, available online: http://www.tandfonline.com/10.1080/21678421.2017.1285317.
References
- 1.Ganzini L, Johnston WS, Silveira MJ. The final month of life in patients with ALS. Neurology. 2002;59(3):428–31. doi: 10.1212/wnl.59.3.428. [DOI] [PubMed] [Google Scholar]
- 2.Lechtzin N, Wiener CM, Clawson L, Chaudhry V, Diette GB. Hospitalization in amyotrophic lateral sclerosis - Causes, costs, and outcomes. Neurology. 2001;56(6):753–7. doi: 10.1212/wnl.56.6.753. [DOI] [PubMed] [Google Scholar]
- 3.Heritier B, Adler D, Iancu F, Ricou B, Gasche Y, Leuchter I, et al. Is tracheostomy still an option in amyotrophic lateral sclerosis? Reflections of a multidisciplinary work group. Swiss medical weekly. 2012;143:w13830-w. doi: 10.4414/smw.2013.13830. [DOI] [PubMed] [Google Scholar]
- 4.Chochinov HM, Tataryn D, Clinch JJ, Dudgeon D. Will to live in the terminally ill. Lancet. 1999;354(9181):816–9. doi: 10.1016/S0140-6736(99)80011-7. [DOI] [PubMed] [Google Scholar]
- 5.Upadya A, Muralidharan V, Thorevska N, Amoateng-Adjepong Y, Manthous CA. Patient, physician, and family member understanding of living wills. Am J Respir Crit Care Med. 2002;166(11):1430–5. doi: 10.1164/rccm.200206-503OC. [DOI] [PubMed] [Google Scholar]
- 6.Emanuel EJ, Emanuel LL. The economics of dying. The illusion of cost savings at the end of life. N Engl J Med. 1994;330(8):540–4. doi: 10.1056/NEJM199402243300806. [DOI] [PubMed] [Google Scholar]
- 7.Teno J, Lynn J, Phillips R, et al. Do advance directives save resources? Clin Res. 1993;41(2):551A. [PubMed] [Google Scholar]
- 8.Curtis JR, Patrick DL, Caldwell ES, Collier AC. Why don't patients and physicians talk about end-of-life care? Barriers to communication for patients with acquired immunodeficiency syndrome and their primary care clinicians. Arch Intern Med. 2000;160(11):1690–6. doi: 10.1001/archinte.160.11.1690. [DOI] [PubMed] [Google Scholar]
- 9.Hawkins NA, Ditto PH, Danks JH, Smucker WD. Micromanaging death: process preferences, values, and goals in end-of-life medical decision making. Gerontologist. 2005;45(1):107–17. doi: 10.1093/geront/45.1.107. [DOI] [PubMed] [Google Scholar]
- 10.Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, Grambow S, Parker J, et al. Preparing for the end of life: preferences of patients, families, physicians, and other care providers. J Pain Symptom Manage. 2001;22(3):727–37. doi: 10.1016/s0885-3924(01)00334-7. [DOI] [PubMed] [Google Scholar]
- 11.Coppola KM, Ditto PH, Danks JH, Smucker WD. Accuracy of primary care and hospital-based physicians' predictions of elderly outpatients' treatment preferences with and without advance directives. Arch Intern Med. 2001;161(3):431–40. doi: 10.1001/archinte.161.3.431. [DOI] [PubMed] [Google Scholar]
- 12.Miura Y, Asai A, Matsushima M, Nagata S, Onishi M, Shimbo T, et al. Families' and physicians' predictions of dialysis patients' preferences regarding life-sustaining treatments in Japan. American Journal of Kidney Diseases. 2006;47(1):122–30. doi: 10.1053/j.ajkd.2005.09.030. [DOI] [PubMed] [Google Scholar]
- 13.Pruchno RA, Lemay EP, Jr, Feild L, Levinsky NG. Predictors of patient treatment preferences and spouse substituted judgments: the case of dialysis continuation. Med Decis Making. 2006;26(2):112–21. doi: 10.1177/0272989X06286482. [DOI] [PubMed] [Google Scholar]
- 14.Shalowitz DI, Garrett-Mayer E, Wendler D. The accuracy of surrogate decision makers: a systematic review. Arch Intern Med. 2006;166(5):493–7. doi: 10.1001/archinte.166.5.493. [DOI] [PubMed] [Google Scholar]
- 15.Zettel-Watson L, Ditto PH, Danks JH, Smucker WD. Actual and perceived gender differences in the accuracy of surrogate decisions about life-sustaining medical treatment among older spouses. Death Studies. 2008;32(3):273–90. doi: 10.1080/07481180701881230. [DOI] [PubMed] [Google Scholar]
- 16.Salmond SW, David E. Attitudes toward advance directives and advance directive completion rates. Orthopaedic Nursing. 2005;24(2):117–27. doi: 10.1097/00006416-200503000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Sessanna L, Jezewski MA. Advance directive decision making among independent community-dwelling older adults - A systematic review of health science literature. Journal of Applied Gerontology. 2008;27(4):486–510. [Google Scholar]
- 18.Jezewski MA, Meeker MA, Sessanna L, Finnell DS. The effectiveness of interventions to increase advance directive completion rates. Journal of Aging and Health. 2007;19(3):519–36. doi: 10.1177/0898264307300198. [DOI] [PubMed] [Google Scholar]
- 19.McAuley WJ, Buchanan RJ, Travis SS, Wang S, Kim M. Recent trends in advance directives at nursing home admission and one year after admission. Gerontologist. 2006;46(3):377–81. doi: 10.1093/geront/46.3.377. [DOI] [PubMed] [Google Scholar]
- 20.Rao JK, Anderson LA, Lin F-C, Laux JP. Completion of advance directives among US consumers. American journal of preventive medicine. 2014;46(1):65–70. doi: 10.1016/j.amepre.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Astrow AB, Sood JR, Nolan MT, Terry PB, Clawson L, Kub J, et al. Decision-making in patients with advanced cancer compared with amyotrophic lateral sclerosis. J Med Ethics. 2008;34(9):664–8. doi: 10.1136/jme.2007.022731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Borasio GD, Shaw PJ, Hardiman O, Ludolph AC, Sales Luis ML, Silani V, et al. Standards of palliative care for patients with amyotrophic lateral sclerosis: results of a European survey. Amyotroph Lateral Scler Other Motor Neuron Disord. 2001;2(3):159–64. doi: 10.1080/146608201753275517. [DOI] [PubMed] [Google Scholar]
- 23.Miller RG, Brooks BR, Swain-Eng RJ, Basner RC, Carter GT, Casey P, et al. Quality improvement in neurology: amyotrophic lateral sclerosis quality measures: report of the quality measurement and reporting subcommittee of the American Academy of Neurology. Neurology. 2013;81(24):2136–40. doi: 10.1212/01.wnl.0000437305.37850.f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Young JM, Marshall CL, Anderson EJ. Amyotrophic lateral sclerosis patients' perspectives on use of mechanical ventilation. Health Soc Work. 1994;19(4):253–60. doi: 10.1093/hsw/19.4.253. [DOI] [PubMed] [Google Scholar]
- 25.Silverstein MD, Stocking CB, Antel JP, Beckwith J, Roos RP, Siegler M. Amyotrophic lateral sclerosis and life-sustaining therapy: patients' desires for information, participation in decision making, and life-sustaining therapy. Mayo Clin Proc. 1991;66(9):906–13. doi: 10.1016/s0025-6196(12)61577-8. [DOI] [PubMed] [Google Scholar]
- 26.Hayashi H, Oppenheimer EA. ALS patients on TPPV: totally locked-in state, neurologic findings and ethical implications. Neurology. 2003;61(1):135–7. doi: 10.1212/01.wnl.0000069925.02052.1f. [DOI] [PubMed] [Google Scholar]
- 27.Moss AH, Oppenheimer EA, Casey P, Cazzolli PA, Roos RP, Stocking CB, et al. Patients with amyotrophic lateral sclerosis receiving long-term mechanical ventilation: Advance care planning and outcomes. Chest. 1996;110(1):249–55. doi: 10.1378/chest.110.1.249. [DOI] [PubMed] [Google Scholar]
- 28.Amyotrophic Lateral Sclerosis Association. http://www.alsa.org/als-care/resources/publications-videos/videos/
- 29.Muscular Dystrophy Association. https://www.mda.org/services/educational-materials.
- 30.Benditt JO, Smith TS, Tonelli MR. Empowering the individual with ALS at the end-of-life: disease-specific advance care planning. Muscle Nerve. 2001;24(12):1706–9. doi: 10.1002/mus.1208. [DOI] [PubMed] [Google Scholar]
- 31.Wilkinson G. WRAT-3: Wide Range Achievement Test, Administration Manual. Wilmington, DE: Wide Range, Inc; 1993. [Google Scholar]
- 32.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 33.Jain NL, Kahn MG. Using knowledge maintenance for preference assessment. Proc Annu Symp Comput Appl Med Care. 1995:263–9. [PMC free article] [PubMed] [Google Scholar]
- 34.Torrance GW, Feeny DH, Furlong WJ, Barr RD, Zhang Y, Wang Q. Multiattribute utility function for a comprehensive health status classification system. Health Utilities Index Mark 2. Med Care. 1996;34(7):702–22. doi: 10.1097/00005650-199607000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Green MJ, Levi BH. Development of an interactive computer program for advance care planning. Health Expectations. 2009;12(1):60–9. doi: 10.1111/j.1369-7625.2008.00517.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Levi BH, Green MJ. Too Soon to give up? Re-examining the value of advance directives. Amer J Bioethics. 2010;10(4):1–14. doi: 10.1080/15265161003599691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Green MJ, Levi BH, Farace E. Acceptability and accuracy of a computer-generated advance directive; Society for Medical Decision Making 29th National Meeting; October 23; Pittsburgh, PA. 2007. [Google Scholar]
- 38.Schubart JR, Levi BH, Camacho F, Whitehead M, Farace E, Green MJ. Reliability of an interactive computer program for advance care planning. J Palliat Med. 2012;15(6):637–42. doi: 10.1089/jpm.2011.0489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Levi BH, Heverley SR, Green MJ. Accuracy of a decision aid for advance care planning: simulated end-of-life decision making. J Clin Ethics. 2011;22(3):223–38. [PMC free article] [PubMed] [Google Scholar]
- 40.Hossler C, Levi BH, Simmons Z, Green MJ. Advance care planning for patients with ALS: Feasibility of an interactive computer program. Amyotroph Lateral Sc. 2011;12(3):172–7. doi: 10.3109/17482968.2010.509865. [DOI] [PubMed] [Google Scholar]
- 41.Pellino T, Tluczek A, Collins M, Trimborn S, Norwick H, Engelke ZK, et al. Increasing self-efficacy through empowerment: preoperative education for orthopaedic patients. Orthop Nurs. 1998;17(4):48–51. 4–9. [PubMed] [Google Scholar]
- 42.Green MJ, Schubart JR, Whitehead MM, Farace E, Lehman E, Levi BH. Advance care planning does not adversely affect hope or anxiety among patients with advanced cancer. J Pain Symptom Manage. 2015;49(6):1088–96. doi: 10.1016/j.jpainsymman.2014.11.293. [DOI] [PubMed] [Google Scholar]
- 43.Spielberger CD, Sydeman SJ, Owen AE, Marsh BJ. Measuring anxiety and anger with the State-Trait Anxiety Inventory (STAI) and the State-Trait Anger Expression Inventory (STAXI) In: Maruish ME, editor. The use of psychological testing for treatment planning and outcomes assessment. 2. Mahwah, NJ: Lawrence Erlbaum Associates, Inc.; 1999. pp. 993–1021. [Google Scholar]
- 44.Cedarbaum JM, Stambler N, Malta E, Fuller C, Hilt D, Thurmond B, et al. The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. Journal of the Neurological Sciences. 1999;169(1–2):13–21. doi: 10.1016/s0022-510x(99)00210-5. [DOI] [PubMed] [Google Scholar]
- 45.Simmons Z, Felgoise SH, Bremer BA, Walsh SM, Hufford DJ, Bromberg MB, et al. The ALSSQOL - Balancing physical and nonphysical factors in assessing quality of life in ALS. Neurology. 2006;67(9):1659–64. doi: 10.1212/01.wnl.0000242887.79115.19. [DOI] [PubMed] [Google Scholar]
- 46.O'Connor AM. Validation of a decisional conflict scale. Medical Decision Making. 1995;15:25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 47.Holmes-Rovner M, Kroll J, Schmitt N, Rovner DR, Breer ML, Rothert ML, et al. Patient satisfaction with health care decisions: The satisfaction with decision scale. Medical Decision Making. 1996;16:58–64. doi: 10.1177/0272989X9601600114. [DOI] [PubMed] [Google Scholar]
- 48.Downey L, Au DH, Curtis JR, Engelberg RA. Life-sustaining treatment preferences: matches and mismatches between patients' preferences and clinicians' perceptions. J Pain Symptom Manage. 2013;46(1):9–19. doi: 10.1016/j.jpainsymman.2012.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Van Scoy LJ, Green MJ, Dimmock AE, Bascom R, Boehmer JP, Hensel JK, et al. High satisfaction and low decisional conflict with advance care planning among chronically ill patients with advanced chronic obstructive pulmonary disease or heart failure using an online decision aid: A pilot study. Chronic Illn. 2016;12(3):227–35. doi: 10.1177/1742395316633511. [DOI] [PubMed] [Google Scholar]
- 50.Markham SA, Levi BH, Green MJ, Schubart JR. Use of a computer program for advance care planning with African-American participants. J Natl Med Assoc. 2015;107(1):26–32. doi: 10.1016/S0027-9684(15)30006-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schubart JR, Camacho F, Green MJ, Rush KA, Levi BH. Assessing the internal consistency and temporal stability of advance directives generated by an interactive, online computer program. BMJ Support Palliat Care. 2015 doi: 10.1136/bmjspcare-2014-000814. [DOI] [PMC free article] [PubMed] [Google Scholar]