Abstract
Rationale:
Primary pulmonary meningiomas are extremely rare, and only a few cases have been reported in the medical literature. Imaging findings of primary pulmonary meningiomas have been reported even more rarely.
Patient concerns:
We present the case of a 54-year-old male patient with cough and sputum lasting for 20 years. This was a case of primary pulmonary meningioma with initial suspicion of a chest wall intercostal neurinoma.
Diagnoses:
A lung lesion was detected on chest computed tomography (CT) imaging 4 years ago. This case appeared as a solitary well-defined round nodule close to the left chest wall, with heterogeneous enhancement on CT, which inaccurately led to the suspicion of a chest wall intercostal neurinoma.
Interventions:
A thoracoscopic wedge resection was performed.
Outcomes:
The postoperative histological diagnosis was primary pulmonary meningioma. After 2 years of follow-up, the patient is still alive without evidence of metastasis or recurrence.
Lessons:
Increased awareness of the CT characteristics of this rare tumor may broaden the radiologist's knowledge base.
Keywords: computed tomography, lung, primary pulmonary meningioma
1. Introduction
Primary pulmonary meningioma is a very rare tumor. The first case was reported in 1952 by Weiss et al,[1] and <50 cases have been described in the English medical literature.[2–4] Most cases of primary pulmonary meningioma are benign in nature; <5 cases have been reported to be malignant.[5–7] Many benign primary pulmonary meningiomas are misdiagnosed and overtreated with major pulmonary resection or chemotherapy because of the lack of specificity in clinical and laboratory examinations.[8] Therefore, radiological evaluation of a solitary pulmonary nodule can be necessary and challenging.
2. Case report
A 54-year-old man visited our hospital complaining of cough and sputum lasting for 20 years. He had a history of a lung lesion, a solitary pulmonary nodule located in the left upper lobe that was detected on chest computed tomography (CT) imaging 4 years ago. Chest contrast-enhanced CT was performed at our hospital, revealing a 2.0-cm nodule in the left upper lobe, next to the left chest wall, and the broad basement of the nodule was in proximity to the chest wall (Fig. 1A). In the mediastinal window, the lesion showed a well-circumscribed margin and a heterogeneous enhancement pattern; additionally, some pulmonary small arteries were observed at the lesion's edge (Fig. 1B). The lesion showed signs of being benign, as it lacked pleural thickening and adjacent bony destruction and had a well-circumscribed margin. Because the nodule was close to the chest wall and showed heterogeneous enhancement, we first suspected chest wall intercostal neurinoma. The results of the laboratory tests were within normal limits. The central nervous system (CNS) was normal on magnetic resonance imaging (MRI).
Figure 1.
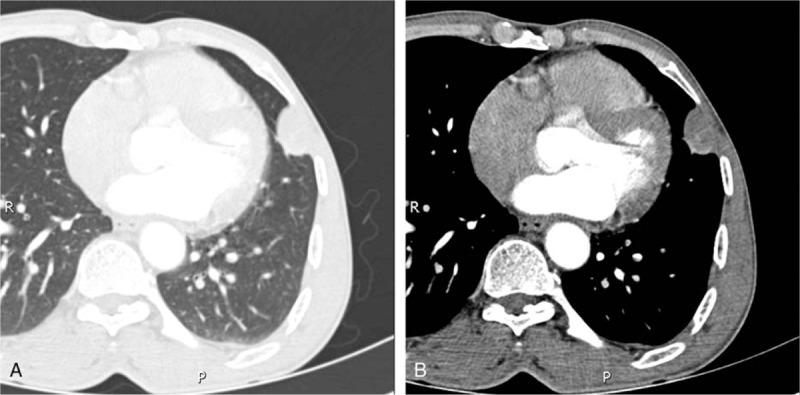
Chest computed tomography-enhanced images of the (A) lung window and (B) mediastinal window. A nodule with a well-circumscribed margin and a heterogeneous enhancement pattern was observed in the left upper lobe in proximity to the left chest wall. Some pulmonary small arteries were observed at the edge of the nodule (B).
A thoracoscopic wedge resection of the lung nodule was performed with an intraoperative frozen section, revealing a spindle-cell tumor that was negative for malignancy. The tumor was a well-demarcated, brown-gray subpleural nodule 1.6 cm in diameter and was located on the upper surface of the left lung. Microscopically, the tumor was composed of bundles of ovoid cells and spindle cells arranged in whorls, and mitotic figures and atypia were absent (Fig. 2A). Immunohistochemical staining demonstrated consistent expression of epithelial membrane antigen vimentin (Vim) (Fig. 2B), and Ki-67 staining was negative. Finally, a histological diagnosis of pulmonary meningioma without characteristics of malignancy was made according to the above-described morphological and immunohistochemical features. After 2 years of follow-up, the patient is still alive without evidence of metastasis or recurrence.
Figure 2.
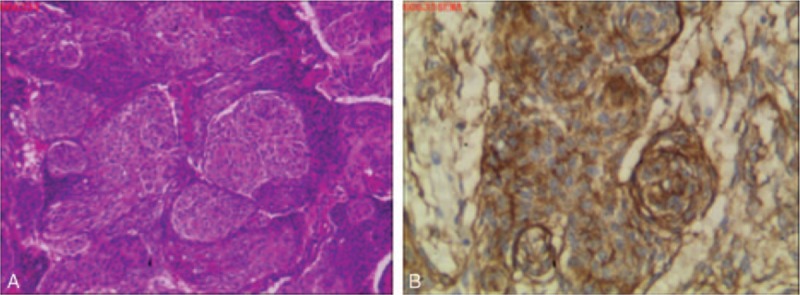
Histological features of the case. (A) Microscopic examination revealed that the tumor was composed of bundles of ovoid cells and spindle cells arranged in whorls (hematoxylin and eosin, 100×). (B) Immunohistochemistry analysis showed tumor cells with positive staining for epithelial membrane antigen (100×).
The patient agreed to authorize us to share the figures and the experiences during his treatment procedure in our department. Informed consent was obtained.
3. Discussion
Primary pulmonary meningioma is a very rare disease, and most cases are detected incidentally on chest plain film or chest CT. There are several controversial hypotheses regarding the pathogenesis of primary pulmonary meningioma. For instance, some authors have proposed that the tumor develops from minute pulmonary meningothelial-like nodules,[9] whereas others suggest that the tumor may arise from pluripotent subpleural mesenchyme.[10]
Meningioma is the most common primary intracranial tumor.[11] Meningioma of the CNS grows slowly without early clinical symptoms, and the typical imaging findings of intracranial meningiomas are easy to diagnose. By contrast, primary pulmonary meningiomas present most often as asymptomatic solitary pulmonary nodules. Moreover, this condition has no characteristic imaging finding, and primary lung cancer or metastasis is commonly suspected on imaging; benign primary pulmonary meningioma is generally well circumscribed in radiological studies.[8] Previous reports of primary pulmonary meningioma with contrast-enhanced CT images showed various enhancement patterns, such as heterogeneous or nodular enhancement,[12,13] poor enhancement,[14,15] or homogeneous enhancement.[2,16,17]
Our case is unique because the solitary nodule was located close to the chest wall with heterogeneous enhancement. Thus, this type of tumor should be included in the differential diagnosis of some extrapulmonary lesions, such as chest wall intercostal neurinoma and pleural mesothelioma. In our case, some small pulmonary arteries were observed at the edge of the nodule. Because the evidence points to a lung lesion, other differential diagnoses include pulmonary carcinoid tumors, sclerosing hemangioma, and pulmonary hamartoma. However, these tumors are usually well-circumscribed. Moreover, sclerosing hemangioma is a rare benign or low-grade tumor that shows marked and rapid enhancement, whereas pulmonary hamartoma, a common benign tumor, generally contains ≥3 histologic components with different degrees of fat, and calcification is commonly observed.
In conclusion, it is necessary to note the imaging features of primary pulmonary meningioma, presenting as a solitary, well-defined nodule in the lung; this rare tumor should be considered in differential diagnoses.
Footnotes
Abbreviations: CNS = central nervous system, CT = computed tomography, MRI = magnetic resonance imaging.
The authors report no conflicts of interest.
References
- [1].Weiss A, Philippides D, Montrieul B, et al. Primary pulmonary meningioma: a rare, slow-growing tumor. J Radiol Electrol Arch Electr Medicale 1952;4:701–3. [PubMed] [Google Scholar]
- [2].Kim YY, Hong YK, Kie JH, et al. Primary pulmonary meningioma: an unusual cause of a nodule with strong and homogeneous enhancement. Clin Imag 2015;40:170–3. [DOI] [PubMed] [Google Scholar]
- [3].Satoh Y, Ishikawa Y. Multiple primary pulmonary meningiomas: 20-year follow-up findings for a first reported case confirming a benign biological nature. Int J Surg Case Rep 2017;31:58–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Drlicek M, Grisold W, Lorber J, et al. Pulmonary meningioma. Immunohistochemical and ultrastructural features. Am J Surg Pathol 1991;15:455–9. [PubMed] [Google Scholar]
- [5].Meij JJCVD, Boomars KA, Bosch JMMVD, et al. Primary pulmonary malignant meningioma. Ann Thorac Surg 2005;80:1523–5. [DOI] [PubMed] [Google Scholar]
- [6].Prayson RA, Farver CF. Primary pulmonary malignant meningioma. Am J Surg Pathol 1999;23:722–6. [DOI] [PubMed] [Google Scholar]
- [7].Weber C, Pautex S, Zulian GB, et al. Primary pulmonary malignant meningioma with lymph node and liver metastasis in a centenary woman, an autopsy case. Virchows Archiv 2013;462:481–5. [DOI] [PubMed] [Google Scholar]
- [8].Matteo I, Giovanni LC, Luca DT, et al. Primary pulmonary meningioma. Report of a case and review of the literature. Lung Cancer 2008;62:401–7. [DOI] [PubMed] [Google Scholar]
- [9].Gomezaracil V, Mayayo E, Alvira R, et al. Fine needle aspiration cytology of primary pulmonary meningioma associated with minute meningotheliallike nodules. Report of a case with histologic, immunohistochemical and ultrastructural studies. Acta Cytol 2002;46:899–903. [DOI] [PubMed] [Google Scholar]
- [10].Lockett L, Chiang V, Scully N. Primary pulmonary meningioma. Am J Surg Pathol 1997;21:453–60. [DOI] [PubMed] [Google Scholar]
- [11].Claus EB, Bondy ML, Schildkraut JM, et al. Epidemiology of intracranial meningioma. Neurosurgery 2005;57:1088. [DOI] [PubMed] [Google Scholar]
- [12].Petscavage JM, Richardson ML, Nett M, et al. Primary chordoid meningioma of the lung. J Thorac Imag 2011;26:W14–6. [DOI] [PubMed] [Google Scholar]
- [13].Incarbone M, Ceresoli GL, Tommaso LD, et al. Primary pulmonary meningioma. Surg Neurol 2008;29:410–3. [Google Scholar]
- [14].Meirelles GS, Ravizzini G, Moreira AL, et al. Primary pulmonary meningioma manifesting as a solitary pulmonary nodule with a false-positive PET scan. J Thorac Imag 2006;21:225–7. [DOI] [PubMed] [Google Scholar]
- [15].Izumi N, Nishiyama N, Iwata T, et al. Primary pulmonary meningioma presenting with hemoptysis on exertion. Ann Thorac Surg 2009;88:647–8. [DOI] [PubMed] [Google Scholar]
- [16].Cura M, Smoak W, Dala R. Pulmonary meningioma: false-positive positron emission tomography for malignant pulmonary nodules. Clin Nucl Med 2002;27:701–4. [DOI] [PubMed] [Google Scholar]
- [17].Masago K, Hosada W, Sasaki E, et al. Is primary pulmonary meningioma a giant form of a meningothelial-like nodule? A case report and review of the literature. Case Rep Oncol 2012;5:471–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


