Abstract
Stroke creates a complex interplay of multiple signaing pathways including excitotoxicity, ionic imbalance, inflammation, oxidative stress and apoptosis. There are very few treatments that have been shown to be beneficial in acute stroke. Recent findings have provided insights into the pathophysiology and mechanisms of ischemic stroke, complementing the traditional glutamate hypothesis: the molecular interaction between PSD95 and GluN2B has been identified as a culprit in stroke-mediated excitotoxicity, leading to the discovery of NA-1, a peptide that disrupts that interaction, as a potent neuroprotective agent for the treatment of acute stroke. In this review we describe its signaling cascade, the target of its therapeutic intervention and its translation from bench to clinical trial.
Keywords: ischemic stroke, PSD-95, GluN2B, protein-protein interaction, NA-1, Tat-NR2B9c
Introduction
According to the World Health Organization stroke is the leading and growing cause of acquired neurological disability and second cause of death worldwide. Stroke mortality is in decline in the Western world, having slipped from the third leading cause of death to the fifth1. This decline in mortality has been primarily due to implementation of new stroke guidelines and improved acute care in hospital settings. Even though stroke death rates are in decline, its prevalence is increasing and recent epidemiological studies have identified that stroke continues to be among the most chronically disabling diseases2. Thus, the reduction in stroke mortality is balanced by an increased burden of disability3.
The majority of strokes are ischemic (87%), occurring as the result of a transient or permanent occlusion of a brain artery that causes a reduction in blood flow in that arterial territory4. Hemorrhagic strokes account for the remaining 13% of cases and are characterized by bleeding into or around the brain. In all those conditions, a consistent decrease in circulating blood flow is enough to deprive neurons of their necessary substrates (oxygen and glucose), eventually leading irrevocably to cell death. Although different brain regions may have different vulnerabilities to ischemic cell damage, neuronal populations seem to be the most sensitive cells when compared with glial cells and vascular cells4.
Ischemic cell death is often a very rapid process that occurs within minutes to hours after blood flow is decreased5. The evolution of ischemic injury, affecting cells adjacent to the originally ischemic area continues for several hours, leading to further neuronal death that may accentuate the severity of the resulting clinical disability or even death6. The extent of tissue death due to lack of oxygen (the infarct) can vary depending on the degree as well as the duration of the reduction in blood flow during the ischemic insult. In the core area of the stroke, in which blood flow is most affected, the lack of oxygen and glucose results in loss of ion homeostasis and metabolic failure. This leads to the overactivation of various damaging processes that culminate in lipolysis, proteolysis and membrane breakdown. By contrast, neurons located within the region that surrounds the ischemic core, may experience a more moderate blood flow reduction, mostly due to residual perfusion from collateral blood vessels. Neuronal tissue in this better perfused area may be able to maintain its structural integrity but lose its function. This is what makes up the “ischemic penumbra”, which is the area of the infarct that may be salvaged if an appropriate treatment is given. As time progresses, the penumbra shrinks and is replaced with irretrievably damaged tissue7. Since the penumbra is the target of acute stroke therapy, significant research is being conducted on targeting cell death mechanisms within this area. It is generally believed that the stroke core territory cannot be salvaged.
Currently, the main treatment for acute stroke is thrombolysis, which is indicated within approximately, within 4.5 h from stroke symptom onset. Thrombolysis is typically accomplished by the administration of tissue plasminogen activator (tPA), the only approved stroke drug in the USA8. However, not all patients with a stroke are candidates for thrombolysis. In fact, due to the risk of hemorrhagic stroke (and bleeding in general), there are strict eligibility criteria for tPA administration. Therefore, because of the rapidly progressive nature of acute stroke, the lack of early pharmacological interventions (besides tPA) and the absence of treatments to promote recovery leave many patients with long-term disabilities. Thus, there is a significant unmet medical need to develop additional treatments for stroke, such as neuroprotectants: drugs that reduce the vulnerability of the brain to ischemia.
Ideally, the purpose of a neuroprotectant would be 1) to salvage the ischemic penumbra; 2) to limit the extent of the secondary damage occurring due to mechanisms such as spreading depolarization and post-ischemic inflammation; and 3) to be useful as a monotherapy that could be administered to the majority of stroke victims in a simple and effective manner.
Pathophysiology of acute stroke
Stroke pathophysiology comprises a variety of mechanisms including excitotoxicity, inflammation, necrosis and apoptosis, which are triggered by hypoxia of the affected tissue. The so-called “ischemic core” corresponds to the irreversibly damaged tissue that is localized in the area in closest proximity to the occluded artery9. Without a supply of glucose and oxygen, neurons in the ischemic core are unable to produce energy in the form of ATP that is necessary to maintain basic cell functions and homeostasis. This results in excessive neuronal depolarization and consequently the release of excitatory neurotransmitters into the synaptic cleft, which fail to be removed from the cleft by re-uptake mechanisms. The dramatically increased concentration of excitatory amino acids leads to overt stimulation of receptors on post-synaptic neurons. Since these receptors are largely permeable to calcium, the intracellular Ca2+ concentration in postsynaptic neurons rises, reaching critical levels that lead to the overactivation of several Ca2+-dependent enzyme systems including phospholipases and proteases that in turn affect cell integrity10. Additionally, the influx of Na+ causes intracellular edema and swelling11. Unless blood flow is quickly restored, cell necrosis ensues within minutes to hours.
In the penumbra region, there may also be mechanisms that cause delayed cell death, a phenomenon that can last for several days from the initial event. Whereas the early cell death is caused largely by a glutamate-induced intracellular Ca2+ rise12, delayed death occurs via apoptotic mechanisms, such as those triggered by the mitochondrial release of cytochrome c13. The main hallmarks of apoptosis are internucleosomal DNA cleavage, somal shrinkage and neuronal condensation, nuclear membrane breakdown, externalization of phosphatidylserine and formation of apoptotic bodies14.
Glutamate is the main excitatory neurotransmitter in the brain. Its role in mediating cell death has been known since the pioneering experiments of Lucas and Newhouse in which L-glutamate was injected into mice retinas, destroying the inner cell layer15. Further work by Olney confirmed this retinal toxicity and also showed the involvement of kainate receptors in producing brain lesions. Olney coined the term “excitotoxicity” to describe the process by which glutamate promotes cell toxicity16. Excitotoxicity describes the well-established process whereby glutamate receptor activation leads to a rise in the intracellular concentration of Ca2+ and Na+ and to cell death17. It is now believed that glutamate toxicity depends mainly on extracellular Ca2+ influx, whereas the influx of extracellular Na+ can cause acute neuronal swelling that has been shown to be reversible18.
Even though the role of Ca2+ in inducing cytotoxicity has been long recognized, the exact mechanisms that mediate its toxic effects remain controversial. It was initially believed that excitotoxicity occurred simply due to “the calcium overload hypothesis”, which suggested that neurotoxicity occurred when intracellular calcium concentration reached a certain threshold19,20. Calcium overload is known to trigger many downstream neurotoxic cascades. For instance, nitric oxide (NO) is synthesized by neuronal nitric oxide synthase (nNOS) which is dependent on the binding of the Ca2+-sensitive enzyme calmodulin. NO reacts with superoxide anions to form a ONOO-, a highly reactive oxidant that promotes tissue damage. This is just one example of the role played by reactive oxygen and nitrogen species (ROS) in cell damage following the activation of enzymes like calpains, proteases, NOS and calcineurins. The damage caused by the production of ROS includes abnormal changes in the organization of the cytoskeleton, mitochondrial dysfunction, the formation of inflammatory molecules and the triggering of signaling pathways that can lead to cell death by apoptosis. Therefore, stroke treatments in the form of free radical scavengers have been proposed for salvaging brain tissue in experimental models of focal ischemia.
Following the calcium overload hypothesis, it became evident that the quantity of Ca2+ influx into the cell was not the sole determinant of cell survival or death. Rather, the source of Ca2+ entry was also important. This was known as the “source specificity hypothesis”21,22. Neurotoxicity is triggered by Ca2+ influx through glutamate receptors23, but similar loads of intracellular Ca2+ permeating through L-type voltage sensitive channels appear innocuous. Thus, the source of Ca2+ entry was assumed to be physically or physiologically linked to downstream pathways that lead to cell death21.
Irrespective of the quantities of calcium required to cause neurotoxicity, glutamate receptors were the key mediators of calcium entry. Therefore, it is not surprising that neuroprotective approaches have been focused on antagonizing these receptors in an attempt to block pathological elevations of Ca2+. Unfortunately, although this approach was intuitive and initially promising, the strategy of glutamate receptor antagonism turned out to be impractical due to deleterious side effects24.
NMDAR-dependent cell death and neuroprotective signaling
The excessive activation of the NMDA receptors and the resulting calcium influx promoted cell death, rendering this receptor a key mediator of excitotoxicity. NMDARs are heterotetramers typically composed of three major subunit types, including an obligatory GluN1, two regulatory GluN2 subunits and less commonly GluN3 members25,26. These subunits have an extracellular amino terminal domain and a C-terminal intracellular tail. The majority of functional NMDARs found in the forebrain contain two GluN1 and two GluN2 (Glun2a-d) subunits. The GluN2 subunits are a determinant of the biophysical and pharmacological properties of the receptors, also governing distinct protein-protein interactions and downstream signaling pathways through their C-terminus tails27,28. When the NMDAR is at resting membrane potential, the channel pore is blocked by magnesium (Mg2+), preventing ions from flowing through the channel. Upon membrane depolarization, the magnesium block is released, opening the ion pore to allow the passage of ions.
NMDARs are highly permeable to exogenous Ca2+ and Na2+ that contribute to membrane depolarization29. Studies supporting the source-specificity hypothesis have shown that Ca2+-dependent neurotoxicity results in greater cell death when Ca2+ influx occurs through NMDARs as opposed to other types of voltage-gated calcium channels (VSCCs) or non-NMDA receptors. This suggests the presence of a direct pathway for neurotoxicity activated by the NMDARs itself. Specifically, the C-terminal cytoplasmic tail of GluN2B subunits can directly interact with multiple intracellular synaptic and cytoskeletal proteins in the NMDAR-associated multiprotein complex within the postsynaptic density (PSD). The main role of the PSD protein is to participate in the regulation of synaptic adhesion, transmitter receptor clustering and modulation of receptor sensitivity. Among these are the membrane-associated guanylate-kinase (MAGUK) family of scaffolding proteins, many of which interact with NMDARs through unique protein-protein interactions. MAGUKs play a role in governing cell-to-cell adhesion, regulation of receptor clustering and modulation of receptor functioning30. It is common for a surface receptor like NMDAR to bind via its C-terminus to a PDZ-domain (named after PSD-95; Disc-large; Zonula-occludens) of a MAGUK protein. For instance, PSD-95 (also known as SAP90), an abundant scaffolding protein within the PSD believed to be responsible for synaptic organization, can bind to GluN2B subunits of the NMDAR through the first and second PDZ domains of PSD-9531. Additionally, the PSD-95 PDZ-2 binds directly to the N-terminus of neuronal nitric oxide synthase (nNOS), thereby connecting NMDARS to nNOS through PSD-95. This molecular arrangement brings NMDAR in close proximity to nNOS, and provides the mechanism by which NMDAR activity triggers NO production by nNOS and excitotoxicity32.
The dual role of NMDARs in acute stroke
NMDARs are known to play a critical role during normal brain function and also in neurological disorders. NMDARs have dual roles as they are capable of promoting both neuronal death and cell survival. It is believed that this is dependent, in part, on the subunit composition of the specific receptors, and their location within the cell27. NMDARs at the plasma membrane are localized both within synaptic and extrasynaptic regions, and it is believed that these locations represent different roles for NMDARs in physiological and pathophysiological events. Although it is likely that NMDARS can mediate excitotoxicity irrespective of location33,34, some studies in cultured cortical and hippocampal neurons show that stimulation of synaptic NMDARs promotes cell survival, whereas extrasynaptic activation promotes neuronal death27,35. This evidence for a dual role of NMDARs activation associates the receptor, depending on its location, with distinct intracellular signaling pathways. For instance, pro-survival factors such as cyclic AMP response element-binding protein (CREB) seem to be activated by synaptic NMDARs to promote cell survival by inducing the expression of genes like brain-derived neurotrophic factor (BDNF), and suppressing apoptotic gene expression. By contrast, extrasynaptic NMDARs mediate cell death by blocking CREB, suppressing BDNF expression and promoting mitochondrial dysfunction and cell death36,37. This might explain why the agent memantine, a weak NMDARs antagonist that supposedly preferentially blocks extrasynaptic NDMARs may hold some promise for certain pathological conditions and appears to exhibit a clinically tolerable activity38,39.
The synaptic versus extrasynaptic localization of NMDARs is not the sole factor mediating their pro-death or pro-survival roles. NMDAR subunit composition holds a key role in regulating the downstream signaling pathways. For example, PSD-95 has been identified as an important synaptic protein involved in pro-death signaling through NMDARs. PSD-95 preferentially associates with GluN2B-containing receptors40. In the adult forebrain, GluN2A-containing NMDARs are preferentially localized at synaptic sites and appear to mediate pro-survival signals, whereas GluN2B-containing NMDARs are preferentially expressed at extrasynaptic sites41,34 and are thought to mediate cell death signaling42,43. Hence, subunit modulation may be one of the mechanisms underlying the effect of receptor localization in NMDAR behavior. However, these rules are neither absolute nor completely understood. Death-promoting GluN2B can also be found in certain synapses and is associated with PSD9544,45. In summary, both the subunit composition and synaptic localization of NMDARs determine which downstream signals occur. Neuronal death seems to be activated by either synaptic or extrasynaptic GluN2B-containing receptor, while synaptic GluN2A-containing NMDARs appear to promote pro-survival signaling34.
GluN2B dependent pro-death signaling in acute stroke
Many pathways downstream of NMDARs have been identified to play a role in excitotoxic signaling besides nNOS. For instance, death-associated protein kinase 1 (also known as DAPK1) is recruited during cerebral ischemia by the GluN2B subunit46. When DAPK1 directly binds and phosphorylates GluN2B, it enhances NMDAR channel conductance resulting in an increase in excitotoxic signaling. Treatment of experimental animals with interfering peptides that impede the interaction between DAPK1 and NMDAR results in reduced brain infarction and improved neurological function. Furthermore, impeding DAPK1 binding automatically promotes other signaling molecules known to be pro-survival, such as ERK 1/247.
A significant signaling molecule downstream from NMDAR that is involved in cell death is PTEN (phosphatase and tensin homolog deleted on chromosome 10). This molecule also binds to the GluN2B subunit48. PTEN plays a role in potentiating the neurotoxic effect of NMDAR activation during ischemia by inhibiting PI3K (phosphatidylinositol 3-kinase) signaling, known for its pro-survival effect. Interestingly, PTEN-induced kinase 1 (PINK1) is thought to function in cell survival-promoting pathways49. When GluN2B-containing NMDARs are overactivated, PINK1-dependent survival signaling is suppressed, thus making PTEN a mediator of neurotoxic cascade50. Another death-promoting protein downstream from NMDAR is SREBP-1 (sterol regulatory element-binding protein-1), which typically functions as a lipid biosynthesis regulator, but during NMDAR-mediated excitotoxicity is involved in promoting cell death51. The discovery of these pathways downstream of NMDARs has provided potential targets for various therapies to treat neurological diseases. However, these pathways are also involved in other physiological processes that occur in parallel to NMDAR-mediated excitotoxicity52. This has stymied the translation of such therapies to the clinic.
An example of non-excitotoxic mechanism of neuronal cell death are those mediated by completely distinct ion channels or receptors. Among these are two members of the transient receptor potential (TRP) channel superfamily53, TRPM2 and TRPM7. Both have been implicated in triggering cell death independently of NMDARs. It is possible that both TRPM2 and TRPM7, which are non-selective cation channels that are activated by oxidative stress play a significant role in ischemic deaths54,55,56. They may represent an additional calcium influx pathway other than NMDARs during ischemia. Thus, following NMDARs overactivation production of reactive oxygen species may in turn activate TRPM2 and TRPM7 channels, creating a feedback loop that perpetuates ischemic cell death.
The discovery of NA-1/Tat-NR2B9c
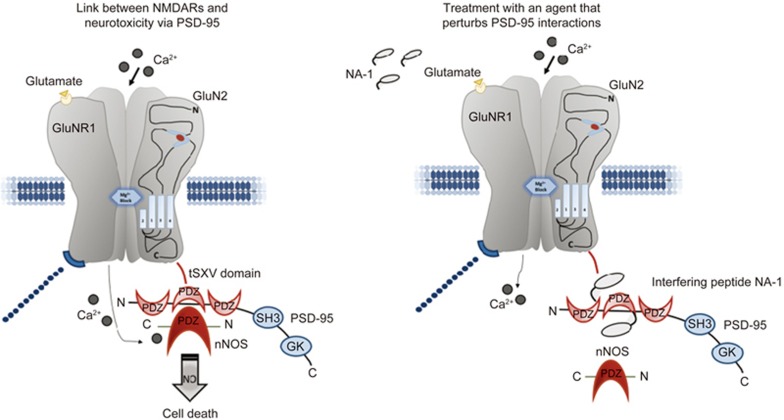
Since PSD-95 has been shown to connect the N-terminal of nNOS with the GluN2B-subunit of the NMDAR, research efforts turned to interfering with this deleterious signaling pathway. Studies in cultured cortical neurons have shown that suppressing PSD-95 expression uncoupled NO production by nNOS from NMDAR-overactivity. This attenuated NMDAR-mediated excitotoxicity, without affecting NMDAR expression or function40. Therefore, suppressing PSD-95 selectively blocks Ca2+-activated nitric oxide production by NMDARs. Since suppressing PSD-95 acutely in stroke is an impractical treatment approach, an alternative strategy to disrupt the NMDAR-PSD-95-nNOS signaling complex was the creation of a drug capable of blocking the protein-protein interaction within this complex. This drug compound is now known as NA-1. It consists of 20 residues including the last nine C-terminal residues of GluN2B (KLSSIESDV) fused to the 11 residue protein transduction domain of the human immunodeficiency virus type 1 (HIV-1) Tat protein that makes the drug cell permeant57,58. This interfering peptide permeates through cell membranes and efficiently disrupts the intracellular interaction of NMDAR with PSD-95, thus disrupting its downstream neurotoxic signaling. Most importantly, unlike NMDAR antagonists, the peptide works within the cell, without directly blocking the synaptic activity of NMDAR or calcium influx (Figure 1). This approach was shown to not only successfully protect cultured cortical neurons from excitotoxicity but to also effectively protect neurons during in vivo stroke experiments after transient middle cerebral artery occlusion (MCAO)58,59,60. Most importantly for the clinical setting, Tat-NR2B9c was successful in protecting the rat brain from MCAO-mediated ischemic damage (both permanent or transient model) even when it was administered 3 h after the insult, conferring significantly reduced infarct volumes in rats and improving their long-term neurobehavioral outcome, including sensorimotor functions, emotionality and cognition59. These studies underlined the potential clinical usefulness of TAT-NR2B9c and its wider therapeutic window.
Figure 1.
Uncoupling of the NMDARs from its downstream effectors using the NA-1 interfering peptide. PSD-95 links NMDARs to toxic downstream cascades including NO production by nitric oxide synthase (nNOS). PSD-95 forms a complex binding to both the tSXV domain of NMDAR GluN2 subunit and with the PDZ domain of nNOS. Disrupting NMDAR-PSD-95 complexes reduce the efficiency by which calcium ions (Ca2+) activate excitotoxic NO production via nNOS. NA-1, also known as Tat-NR2B9c, disrupts the NMDAR-PSD95-nNOS complex, dissociating NMDARs from downstream neurotoxic signaling, without blocking normal synaptic function of NMDARs or calcium influx.
Various groups have shown benefits from the administration of Tat-NR2B9c, such as amelioration of excitotoxic neuronal loss after ischemic damage in vivo, by impairing the pro-death p38 signaling without affecting NMDAR-mediated pro-survival pathways that involved CREB or Akt signaling61,62. Likewise, other research groups have proposed different compounds with a similar mechanism of action to Tat-NR2B9c that also target the NMDAR-PSD-95 interaction and have the same neuroprotective effect. This corroborates the pivotal role of this interaction in mediating excitotoxicity. One of them uses a small molecule inhibitor known as ZL006, that disrupts the PSD-95-nNOS signaling and results in a similar neuroprotective effect during ischemic conditions in vivo63. Another group created a dimeric inhibitor called Tat-NPEG4 (IETDV)2 (also known as Tat-N-dimer), which binds to the PDZ1-1 domain of PSD-95 also reducing the infarct volume in mice subjected to cerebral ischemia64.
The protective effect of Tat-NR2B9c in treating stroke has been tested in cynomolgus macaques, which are higher-order gyrencephalic nonhuman primates that bear significant anatomical and behavioral similarities to humans65. Macaques treated with Tat-NR2B9c 3 h after MCAO onset showed a significant reduction in infarct size, as measured by magnetic resonance imaging (MRI) and confirmed by histology. In addition, animals treated with Tat-NR2B9c performed better at the neurobehavioral assessment as shown by the nonhuman primate stroke scale (NHPSS). Furthermore, gene transcriptome analysis in the ischemic brain tissue confirmed the upregulation of neuroprotective genes that preserve cellular functionality, corroborating the original hypothesis of Tat-NR2B9c as a potent neuroprotectant.
The use of NA-1/Tat-NR2B9c in clinical trials
In 2006, an interesting article was published entitled “1026 experimental treatments in acute stroke”66. The ironic title referred to a Pubmed search of all the pre-clinical studies conducted in the field of stroke that fostered high expectation in developing a therapeutic treatment. In other words, the article was questioning the validity of the animal studies and the experimental procedure as a reliable indicator for clinical outcome in the discovery of a treatment for stroke. This article also highlighted a need for greater rigor in conducting, reporting and analyzing animal data to improve transition of scientific advances from bench to bedside. Using the experimental rigor to compensate for the limitations of animal models. Having in mind the goal of improving preclinical stroke therapy assessment and increasing translational potential, the stroke community decided to provide a series of guidelines called STAIR (stroke therapy academic industry roundtable)67,68. Since the promise of experimental stroke treatments continued to fail in human clinical trials, the hope of STAIR was to improve the validity of the pre-clinical experimental condition to increase the likelihood of translational research against stroke.
Tat-NR2B9c successfully completed a phase 2 clinical trial called ENACT (Evaluating Neuroprotection in Aneurysm Coiling Therapy) in 2012 (ClinicalTrials.gov number, NCT00728182). The goal was to determine the safety and efficacy of Tat-NR2B9c in reducing embolic stroke in patients that undertook an endovascular procedure against brain aneurysms69. Interestingly, the setting in which Tat-NR2B9c was tested was key in this clinical trial, since a major issue for a clinical trial is patient variability. The clinical setting provided for the ENACT allowed the investigators to safely test Tat-NR2B9c in the context of neuroprotection during the removal of a brain aneurysm. This procedure is known to produce micro-strokes, or covert strokes, usually detected though MRI after the procedure. Since stroke is considered to be a variable disease because it is impossible to know when one will occur, this clinical condition offered the best opportunity to study the efficacy of a neuroprotectant at a predictable time from the onset of stroke. The Tat-NR2B9c-treated group, from a single intravenous infusion, experienced a fewer number of lesions. Furthermore, the Tat-NR2B9c-treated group also exhibited improved radiological and clinical outcomes, providing evidence that neuroprotection in humans is achievable. ENACT concluded with positive and encouraging results that warranted further investigation of Tat-NR2B9c in a clinical treatment of acute stroke at a larger scale. Currently, a phase III clinical trial is being conducted in more than 25 cities around the world, to evaluate the clinical benefits of Tat-NR2B9c for neuroprotection after stroke.
Conclusion and future development for use of Tat-NR2B9c
Despite its detrimental effects and its increasing prevalence in the developed world, no novel treatments for stroke have been developed in the last 40 years. The identification of the molecular interaction between PSD95 and GluN2B as a culprit in stroke-mediated excitotoxicity led to the development of Tat-NR2B9c, a peptide that disrupts that interaction. After demonstrating efficacy in vitro, in vivo and in a large primate model of stroke, Tat-NR2B9c is currently being investigated in the clinic. This is the first treatment for stroke in over 20 years to reach Phase III clinical trials. Since the initial application of Tat-NR2B9c to block PSD-95 in acute stroke58, subsequent work has been carried out to investigate its effect on recovery from chronic stroke, as well as other excitotoxicity-mediated neurological diseases, such as stoke recovery70, Alzheimer Disease (AD)71, epilepsy72,73, and neuropathic pain74. The results have been promising. This suggests that the GluN2B-PSD95 interaction plays a central role in neuronal death beyond the confines of stroke. Future research will elucidate the specific mechanisms that play in these different disease settings, and may expand the spectrum of clinical scenarios that would benefit from Tat-NR2B9c.
References
- Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics-2017 Update: a report from the American Heart Association. Circulation 2017; 135: e146–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koton S, Schneider ALC, Rosamond WD, Shahar E, Sang Y, Gottesman RF, et al. Stroke incidence and mortality trends in US communities, 1987 to 2011. JAMA 2014; 312: 259–68. [DOI] [PubMed] [Google Scholar]
- Guha D, Davidson B, Nadi M, Alotaibi NM, Fehlings MG, Gentili F, et al. Management of peripheral nerve sheath tumors: 17 years of experience at Toronto Western Hospital. J Neurosurg 2017: 1–9. doi: 10.3171/2017.1.JNS162292. [DOI] [PubMed]
- Woodruff TM, Thundyil J, Tang SC, Sobey CG, Taylor SM, Arumugam TV. Pathophysiology, treatment, and animal and cellular models of human ischemic stroke. Mol Neurodegener 2011; 6: 11. doi: 10.1186/1750-1326-6-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hossmann KA. The two pathophysiologies of focal brain ischemia: implications for translational stroke research. J Cereb Blood Flow Metab Off J Int Soc Cereb Blood Flow Metab 2012; 32: 1310–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz MA, Lo EH, Iadecola C. The science of stroke: mechanisms in search of treatments. Neuron 2010; 67: 181–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsberg MD, Belayev L, Zhao W, Huh PW, Busto R. The acute ischemic penumbra: topography, life span, and therapeutic response. Acta Neurochir Suppl 1999; 73: 45–50. [DOI] [PubMed] [Google Scholar]
- National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 1995; 333: 1581–7. [DOI] [PubMed] [Google Scholar]
- Yuan J. Neuroprotective strategies targeting apoptotic and necrotic cell death for stroke. Apoptosis Int J Program Cell Death 2009; 14: 469–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon RP, Griffiths T, Evans MC, Swan JH, Meldrum BS. Calcium overload in selectively vulnerable neurons of the hippocampus during and after ischemia: an electron microscopy study in the rat. J Cereb Blood Flow Metab Off J Int Soc Cereb Blood Flow Metab 1984; 4: 350–61. [DOI] [PubMed] [Google Scholar]
- Iadecola C, Anrather J. Stroke research at a crossroad: asking the brain for directions. Nat Neurosci 2011; 14: 1363–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beilharz EJ, Williams CE, Dragunow M, Sirimanne ES, Gluckman PD. Mechanisms of delayed cell death following hypoxic-ischemic injury in the immature rat: evidence for apoptosis during selective neuronal loss. Brain Res Mol Brain Res 1995; 29: 1–14. [DOI] [PubMed] [Google Scholar]
- Liu X, Kim CN, Yang J, Jemmerson R, Wang X. Induction of apoptotic program in cell-free extracts: requirement for dATP and cytochrome c. Cell 1996; 86: 147–57. [DOI] [PubMed] [Google Scholar]
- Lucas DR, Newhouse JP. The toxic effect of sodium L-glutamate on the inner layers of the retina. AMA Arch Ophthalmol 1957; 58: 193–201. [DOI] [PubMed] [Google Scholar]
- Raghupathi R, Graham DI, McIntosh TK. Apoptosis after traumatic brain injury. J Neurotrauma 2000; 17: 927–38. [DOI] [PubMed] [Google Scholar]
- Blood FR, Oser BL, White PL, Olney JW. Monosodium glutamate. Science 1969; 165: 1028–9. [DOI] [PubMed] [Google Scholar]
- Rothman SM. Synaptic activity mediates death of hypoxic neurons. Science 1983; 220: 536–7. [DOI] [PubMed] [Google Scholar]
- Choi DW, Maulucci-Gedde M, Kriegstein AR. Glutamate neurotoxicity in cortical cell culture. J Neurosci Off J Soc Neurosci 1987; 7: 357–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manev H, Favaron M, Guidotti A, Costa E. Delayed increase of Ca2+ influx elicited by glutamate: role in neuronal death. Mol Pharmacol 1989; 36: 106–12. [PubMed] [Google Scholar]
- Marcoux FW, Probert AW, Weber ML. Hypoxic neuronal injury in tissue culture is associated with delayed calcium accumulation. Stroke 1990; 21: III71–4. [PubMed] [Google Scholar]
- Tymianski M, Charlton MP, Carlen PL, Tator CH. Source specificity of early calcium neurotoxicity in cultured embryonic spinal neurons. J Neurosci Off J Soc Neurosci 1993; 13: 2085–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sattler R, Charlton MP, Hafner M, Tymianski M. Distinct influx pathways, not calcium load, determine neuronal vulnerability to calcium neurotoxicity. J Neurochem 1998; 71: 2349–64. [DOI] [PubMed] [Google Scholar]
- Ghosh A, Greenberg ME. Calcium signaling in neurons: molecular mechanisms and cellular consequences. Science 1995; 268: 239–47. [DOI] [PubMed] [Google Scholar]
- Lees KR. Does neuroprotection improve stroke outcome? Lancet Lond Engl 1998; 351: 1447–8. [DOI] [PubMed] [Google Scholar]
- Hollmann M, Heinemann S. Cloned glutamate receptors. Annu Rev Neurosci 1994; 17: 31–108. [DOI] [PubMed] [Google Scholar]
- Paoletti P, Neyton J. NMDA receptor subunits: function and pharmacology. Curr Opin Pharmacol 2007; 7: 39–47. [DOI] [PubMed] [Google Scholar]
- Hardingham GE, Bading H. Synaptic versus extrasynaptic NMDA receptor signalling: implications for neurodegenerative disorders. Nat Rev Neurosci 2010; 11: 682–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan TJ, Emes RD, Grant SG, Komiyama NH. Evolution of NMDA receptor cytoplasmic interaction domains: implications for organisation of synaptic signalling complexes. BMC Neurosci 2008; 9: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monyer H, Burnashev N, Laurie DJ, Sakmann B, Seeburg PH. Developmental and regional expression in the rat brain and functional properties of four NMDA receptors. Neuron 1994; 12: 529–40. [DOI] [PubMed] [Google Scholar]
- Feng W, Zhang M. Organization and dynamics of PDZ-domain-related supramodules in the postsynaptic density. Nat Rev Neurosci 2009; 10: 87–99. [DOI] [PubMed] [Google Scholar]
- Kornau HC, Schenker LT, Kennedy MB, Seeburg PH. Domain interaction between NMDA receptor subunits and the postsynaptic density protein PSD-95. Science 1995; 269: 1737–40. [DOI] [PubMed] [Google Scholar]
- Dawson VL, Dawson TM, Bartley DA, Uhl GR, Snyder SH. Mechanisms of nitric oxide-mediated neurotoxicity in primary brain cultures. J Neurosci Off J Soc Neurosci 1993; 13: 2651–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sattler R, Xiong Z, Lu WY, MacDonald JF, Tymianski M. Distinct roles of synaptic and extrasynaptic NMDA receptors in excitotoxicity. J Neurosci Off J Soc Neurosci 2000; 20: 22–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Wong TP, Aarts M, Rooyakkers A, Liu L, Lai TW, et al. NMDA receptor subunits have differential roles in mediating excitotoxic neuronal death both in vitro and in vivo. J Neurosci Off J Soc Neurosci 2007; 27: 2846–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soriano FX, Hardingham GE. Compartmentalized NMDA receptor signalling to survival and death. J Physiol 2007; 584: 381–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardingham GE, Fukunaga Y, Bading H. Extrasynaptic NMDARs oppose synaptic NMDARs by triggering CREB shut-off and cell death pathways. Nat Neurosci 2002; 5: 405–14. [DOI] [PubMed] [Google Scholar]
- Gouix E, Léveillé F, Nicole O, Melon C, Had-Aissouni L, Buisson A. Reverse glial glutamate uptake triggers neuronal cell death through extrasynaptic NMDA receptor activation. Mol Cell Neurosci 2009; 40: 463–73. [DOI] [PubMed] [Google Scholar]
- Xia P, Chen HV, Zhang D, Lipton SA. Memantine preferentially blocks extrasynaptic over synaptic NMDA receptor currents in hippocampal autapses. J Neurosci Off J Soc Neurosci 2010; 30: 11246–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons CG, Danysz W, Quack G. Memantine is a clinically well tolerated N-methyl-D-aspartate (NMDA) receptor antagonist--a review of preclinical data. Neuropharmacology 1999; 38: 735–67. [DOI] [PubMed] [Google Scholar]
- Sattler R, Xiong Z, Lu WY, Hafner M, MacDonald JF, Tymianski M. Specific coupling of NMDA receptor activation to nitric oxide neurotoxicity by PSD-95 protein. Science 1999; 284: 1845–8. [DOI] [PubMed] [Google Scholar]
- Groc L, Bard L, Choquet D. Surface trafficking of N-methyl-D-aspartate receptors: physiological and pathological perspectives. Neuroscience 2009; 158: 4–18. [DOI] [PubMed] [Google Scholar]
- Chen M, Lu TJ, Chen XJ, Zhou Y, Chen Q, Feng XY, et al. Differential roles of NMDA receptor subtypes in ischemic neuronal cell death and ischemic tolerance. Stroke 2008; 39: 3042–8. [DOI] [PubMed] [Google Scholar]
- Zhou M, Baudry M. Developmental changes in NMDA neurotoxicity reflect developmental changes in subunit composition of NMDA receptors. J Neurosci Off J Soc Neurosci 2006; 26: 2956–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris AZ, Pettit DL. Extrasynaptic and synaptic NMDA receptors form stable and uniform pools in rat hippocampal slices. J Physiol 2007; 584: 509–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas CG, Miller AJ, Westbrook GL. Synaptic and extrasynaptic NMDA receptor NR2 subunits in cultured hippocampal neurons. J Neurophysiol 2006; 95: 1727–34. [DOI] [PubMed] [Google Scholar]
- Tu W, Xu X, Peng L, Zhong X, Zhang W, Soundarapandian MM, et al. DAPK1 interaction with NMDA receptor NR2B subunits mediates brain damage in stroke. Cell 2010; 140: 222–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S, Zhang N, Guo Y, Zhao R, Shi T, Feng S, et al. G-protein-coupled receptor 30 mediates rapid neuroprotective effects of estrogen via depression of NR2B-containing NMDA receptors. J Neurosci Off J Soc Neurosci 2012; 32: 4887–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ning K, Pei L, Liao M, Liu B, Zhang Y, Jiang W, et al. Dual neuroprotective signaling mediated by downregulating two distinct phosphatase activities of PTEN. J Neurosci Off J Soc Neurosci 2004; 24: 4052–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilhelmus MMM, Nijland PG, Drukarch B, de Vries HE, van Horssen J. Involvement and interplay of Parkin, PINK1, and DJ1 in neurodegenerative and neuroinflammatory disorders. Free Radic Biol Med 2012; 53: 983–92. [DOI] [PubMed] [Google Scholar]
- Shan Y, Liu B, Li L, Chang N, Li L, Wang H, et al. Regulation of PINK1 by NR2B-containing NMDA receptors in ischemic neuronal injury. J Neurochem 2009; 111: 1149–60. [DOI] [PubMed] [Google Scholar]
- Taghibiglou C, Martin HGS, Lai TW, Cho T, Prasad S, Kojic L, et al. Role of NMDA receptor-dependent activation of SREBP1 in excitotoxic and ischemic neuronal injuries. Nat Med 2009; 15: 1399–406. [DOI] [PubMed] [Google Scholar]
- Tymianski M. Emerging mechanisms of disrupted cellular signaling in brain ischemia. Nat Neurosci 2011; 14: 1369–73. [DOI] [PubMed] [Google Scholar]
- Nilius B, Owsianik G. The transient receptor potential family of ion channels. Genome Biol 2011; 12: 218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald JF, Xiong ZG, Jackson MF. Paradox of Ca2+ signaling, cell death and stroke. Trends Neurosci 2006; 29: 75–81. [DOI] [PubMed] [Google Scholar]
- Sun HS, Jackson MF, Martin LJ, Jansen K, Teves L, Cui H, et al. Suppression of hippocampal TRPM7 protein prevents delayed neuronal death in brain ischemia. Nat Neurosci 2009; 12: 1300–7. [DOI] [PubMed] [Google Scholar]
- Xie YF, Macdonald JF, Jackson MF. TRPM2, calcium and neurodegenerative diseases. Int J Physiol Pathophysiol Pharmacol 2010; 2: 95–103. [PMC free article] [PubMed] [Google Scholar]
- Schwarze SR, Ho A, Vocero-Akbani A, Dowdy SF. In vivo protein transduction: delivery of a biologically active protein into the mouse. Science 1999; 285: 1569–72. [DOI] [PubMed] [Google Scholar]
- Aarts M, Liu Y, Liu L, Besshoh S, Arundine M, Gurd JW, et al. Treatment of ischemic brain damage by perturbing NMDA receptor- PSD-95 protein interactions. Science 2002; 298: 846–50. [DOI] [PubMed] [Google Scholar]
- Sun H-S, Doucette TA, Liu Y, Fang Y, Teves L, Aarts M, et al. Effectiveness of PSD95 inhibitors in permanent and transient focal ischemia in the rat. Stroke J Cereb Circ 2008; 39: 2544–53. [DOI] [PubMed] [Google Scholar]
- Cui H, Hayashi A, Sun HS, Belmares MP, Cobey C, Phan T, et al. PDZ protein interactions underlying NMDA receptor-mediated excitotoxicity and neuroprotection by PSD-95 inhibitors. J Neurosci Off J Soc Neurosci 2007; 27: 9901–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soriano FX, Martel MA, Papadia S, Vaslin A, Baxter P, Rickman C, et al. Specific targeting of pro-death NMDA receptor signals with differing reliance on the NR2B PDZ ligand. J Neurosci Off J Soc Neurosci 2008; 28: 10696–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MA, Soriano FX, Baxter P, Rickman C, Duncan R, Wyllie DJA, et al. Inhibiting pro-death NMDA receptor signaling dependent on the NR2 PDZ ligand may not affect synaptic function or synaptic NMDA receptor signaling to gene expression. Channels Austin Tex 2009; 3: 12–5. [DOI] [PubMed] [Google Scholar]
- Zhou L, Li F, Xu HB, Luo CX, Wu HY, Zhu MM, et al. Treatment of cerebral ischemia by disrupting ischemia-induced interaction of nNOS with PSD-95. Nat Med 2010; 16: 1439–43. [DOI] [PubMed] [Google Scholar]
- Bach A, Clausen BH, Møller M, Vestergaard B, Chi CN, Round A, et al. A high-affinity, dimeric inhibitor of PSD-95 bivalently interacts with PDZ1-2 and protects against ischemic brain damage. Proc Natl Acad Sci U S A 2012; 109: 3317–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook DJ, Teves L, Tymianski M. Treatment of stroke with a PSD-95 inhibitor in the gyrencephalic primate brain. Nature 2012; 483: 213–7. [DOI] [PubMed] [Google Scholar]
- O'Collins VE, Macleod MR, Donnan GA, Horky LL, van der Worp BH, Howells DW. 1,026 experimental treatments in acute stroke. Ann Neurol 2006; 59: 467–77. [DOI] [PubMed] [Google Scholar]
- Saver JL, Albers GW, Dunn B, Johnston KC, Fisher M. STAIR VI Consortium. Stroke Therapy Academic Industry Roundtable (STAIR) recommendations for extended window acute stroke therapy trials. Stroke 2009; 40: 2594–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher M, Feuerstein G, Howells DW, Hurn PD, Kent TA, Savitz SI, et al. Update of the stroke therapy academic industry roundtable preclinical recommendations. Stroke J Cereb Circ 2009; 40: 2244–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill MD, Martin RH, Mikulis D, Wong JH, Silver FL, Terbrugge KG, et al. Safety and efficacy of NA-1 in patients with iatrogenic stroke after endovascular aneurysm repair (ENACT): a phase 2, randomised, double-blind, placebo-controlled trial. Lancet Neurol 2012; 11: 942–50. [DOI] [PubMed] [Google Scholar]
- Zhou HH, Tang Y, Zhang XY, Luo CX, Gao LY, Wu HY, et al. Delayed administration of Tat-HA-NR2B9c promotes recovery after stroke in rats. Stroke J Cereb Circ 2015; 46: 1352–8. [DOI] [PubMed] [Google Scholar]
- Ittner LM, Ke YD, Delerue F, Bi M, Gladbach A, van Eersel J, et al. Dendritic function of tau mediates amyloid-beta toxicity in Alzheimer's disease mouse models. Cell 2010; 142: 387–97. [DOI] [PubMed] [Google Scholar]
- Florio SK, Loh C, Huang SM, Iwamaye AE, Kitto KF, Fowler KW, et al. Disruption of nNOS-PSD95 protein-protein interaction inhibits acute thermal hyperalgesia and chronic mechanical allodynia in rodents. Br J Pharmacol 2009; 158: 494–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dykstra CM, Ratnam M, Gurd JW. Neuroprotection after status epilepticus by targeting protein interactions with postsynaptic density protein 95. J Neuropathol Exp Neurol 2009; 68: 823–31. [DOI] [PubMed] [Google Scholar]
- Tao F, Tao YX, Mao P, Johns RA. Role of postsynaptic density protein-95 in the maintenance of peripheral nerve injury-induced neuropathic pain in rats. Neuroscience 2003; 117: 731–9. [DOI] [PubMed] [Google Scholar]