Abstract
Background
Heart failure (HF) is associated with a high rate of readmissions within 30 days post-discharge and in the following year, especially in frail elderly patients. Biomarker data are scarce in this high-risk population. This study assessed the value of early post-discharge circulating levels of ST2, NT-proBNP, CA125, and hs-TnI for predicting 30-day and 1-year outcomes in comorbid frail elderly patients with HF with mainly preserved ejection fraction (HFpEF).
Methods
Blood samples were obtained at the first visit shortly after discharge (4.9 ± 2 days). The primary endpoint was the composite of all-cause mortality or HF-related rehospitalization at 30 days and at 1 year. All-cause mortality alone at one year was also a major endpoint. HF-related rehospitalizations alone were secondary end-points.
Results
From February 2014 to November 2016, 522 consecutive patients attending the STOP-HF Clinic were included (57.1% women, age 82 ± 8.7 years, mean Barthel index 70 ± 25, mean Charlson comorbidity index 5.6 ± 2.2). The composite endpoint occurred in 8.6% patients at 30 days and in 38.5% at 1 year. In multivariable analysis, ST2 [hazard ratio (HR) 1.53; 95% CI 1.19–1.97; p = 0.001] was the only predictive biomarker at 30 days; at 1 year, both ST2 (HR 1.34; 95% CI 1.15–1.56; p < 0.001) and NT-proBNP (HR 1.19; 95% CI 1.02–1.40; p = 0.03) remained significant. The addition of ST2 and NT-proBNP into a clinical predictive model increased the AUC from 0.70 to 0.75 at 30 days (p = 0.02) and from 0.71 to 0.74 at 1 year (p < 0.05). For all-cause death at 1 year, ST2 (HR 1.50; 95% CI 1.26–1.80; p < 0.001), and CA125 (HR 1.41; 95% CI 1.21–1.63; p < 0.001) remained independent predictors in multivariable analysis. The addition of ST2 and CA125 into a clinical predictive model increased the AUC from 0.74 to 0.78 (p = 0.03). For HF-related hospitalizations, ST2 was the only predictive biomarker in multivariable analyses, both at 30 days and at 1 year.
Conclusions
In a comorbid frail elderly population with HFpEF, ST2 outperformed NT-proBNP for predicting the risk of all-cause mortality or HF-related rehospitalization. ST2, a surrogate marker of inflammation and fibrosis, may be a better predictive marker in high-risk HFpEF.
Electronic supplementary material
The online version of this article (10.1186/s12877-018-0807-2) contains supplementary material, which is available to authorized users.
Background
Heart failure (HF) is associated with a high rate of readmission within 30 days after discharge [1, 2]. The rehospitalization rates are as high as 20–30% in the first month and increase further during the following year [3–6]. This represents a health, social, and economic burden [7–9], especially for elderly patients, as the prevalence of HF is higher in those over 80 years old [10, 11]. Elderly HF patients differ from younger patients in terms of etiology, comorbidities [12], and phenotype, and elderly patients have a higher prevalence of heart failure with preserved ejection fraction (HFpEF) [13, 14]. This clinical difference impacts short- and mid-term outcomes, and readmissions can be due to exacerbations of the underlying disease [15] as well as to other medical problems [16].
Developing risk prediction models to help in clinical decision making is a major challenge in this elderly HFpEF population [17]. Notably, identifying individuals who are at the highest risk of readmission could lay the groundwork for precision medicine to develop customized preventive measures [18]. Indeed, risk stratification may be refined by the use of biomarkers of different pathophysiologic processes that are not necessarily reflected by established clinical risk factors [19]. Predictive biomarker data in such special populations are scarce and the role of biomarkers in elderly subjects with HF is challenged by the presence of comorbidities [20].
Accordingly, our aim was to assess the value of a panel of 4 biomarkers for predicting 30-day and 1-year outcomes in a population of fragile elderly patients with comorbidities and mainly HFpEF. We analyzed the following biomarkers: N-terminal pro-brain natriuretic peptide (NT-proBNP; a marker of myocardial stretch and neurohormonal activation), interleukin-1 receptor-like 1 (ST2; a marker of inflammation and stretch and extracellular matrix remodeling), high-sensitivity troponin I (hs-TnI; a surrogate marker of myocardial injury), and cancer antigen 125 (CA125; a marker of systemic congestion in HF).
Methods
Study population
This prospective single-center investigation was performed as part of the STructured multidisciplinary outpatient clinic for Old and frail Post-discharge patients hospitalized for HF (STOP-HF-Clinic) study, which aimed to reduce readmission rates and facilitate the transition to primary care [21]. The STOP-HF-Clinic study included the most vulnerable patients with a primary hospital diagnosis of HF who were admitted for acutely decompensated HF to internal medicine and geriatric wards [22]. The interventions performed in the STOP-HF-Clinic study and at routine visits were reported previously [20]. At the first visit, a mean of 4.9 ± 2 days after discharge, the following were obtained from each patient: clinical, demographic, and treatment data; Charlson comorbidity index and Barthel functional score; and a blood sample.
Analytical assays
ST2 assay
ST2 was measured using a high-sensitivity sandwich monoclonal immunoassay (Presage® ST2 assay, Critical Diagnostics, San Diego, CA, USA). The hs-ST2 assay had a within-run coefficient of < 2.5% and a total coefficient of variation of 4%.
NT-proBNP assay
NT-proBNP was quantified using the AQT90 FLEX immunoassay (Radiometer Medical). According to the manufacturer, there is no detectable cross-reactivity with ANP, BNP, or CNP, and the within-day CV is < 10% in samples with NT-pro-BNP concentrations higher than 73 pg/mL.
CA125 assay
Ca125 was measured in an Architect i2000 platform (Abbott Diagnostics). The CV of the ARCHITECT CA 125 II assay has a CV < 10%. Samples with concentrations higher than 1000 U/mL were diluted 1:10 using the automated dilution protocol recommended by the manufacturer.
Hs-TnI assay
hs-TnI was measured using an Architect i2000 platform (Abbott Diagnostics). There was ≤0.1% cross-reactivity with skeletal troponin I and ≤ 1% cross-reactivity with cardiac troponin T and troponin C.
Follow-up and endpoints
All patients had visits scheduled at regular intervals for 1 to 3 months, with additional visits as required in cases of decompensation or when need of treatment up-titration20. Clinical follow-up was subsequently performed by the patient’s general practitioner. The composite endpoints, i.e. all-cause mortality or HF-related rehospitalization at 30 days and at 1 year, were the primary endpoints. HF-related rehospitalization was also assessed as a secondary endpoint for both study periods. All-cause death at one year was analyzed as well. Death and hospital admissions were prospectively reviewed using electronic medical records (CP and MD).
Statistical analysis
Categorical variables were expressed as percentages. Continuous variables were expressed as means (standard deviations [SDs]) or medians [25–75 percentiles] according to their distribution (normal or non-normal). Normal distribution was assessed with normal Q-Q plots. Correlation between the different studied biomarkers was performed using Pearson correlation test of log-transformed values of each biomarker. Kaplan-Meier survival curves were plotted for the biomarkers statistically independently associated with the one-year composite end-point and one-year all-cause death and the groups were compared using the Log-Rank test. Univariate Cox regression analyses were performed for all of the endpoints for the four studied biomarkers and also for relevant clinical covariates: age; sex; New York Heart Association functional class; diabetes mellitus; Charlson comorbidity index; Barthel index; and urea, creatinine, hemoglobin, and sodium levels. For HF-related re-hospitalization, a competing risk strategy using the Gray method was adopted, considering death as the competing risk. The four studied biomarkers were log-transformed and analyzed per 1 SD. Multivariable analyses were also performed using the backward step method, with age, sex, and the variables with statistical significance in the univariate analyses as covariates. Predictive “X*Beta” models were created from Cox regression analysis for the composite endpoint, both at 30 days and at 1 year. The best clinical predictive models without biomarkers were constructed, including age and sex and the variables with statistical significance in the univariate analyses. This approach was used because with such strategy we obtained the better AUC with clinical variables. The area under the curve (AUC) of these “X*Beta” models was then obtained. Next, the biomarkers with statistical significance in univariate analyses were added into the models, and new AUCs were calculated for the predictive biomarkers. AUC were compared by chi-squared test. Statistical analyses were performed with SPSS 15 (SPSS Inc., Chicago, IL, USA) and STATA V.13.0 (College Station, Texas, USA). A two-sided p < 0.05 was considered significant.
Results
From February 2014 to November 2016, 522 consecutive patients at the STOP-HF Clinic (57.1% women, mean age 82 ± 8.7 years, 25% older than 88 years; mean LVEF 58.8% ±14) were included in the STOP-HF-Clinic study. Their clinical characteristics are shown in Table 1. The main etiologies were hypertension (39.7%), ischemia (28.7%), and valvular heart disease (13.2%). Diabetes, anemia, and renal failure were highly prevalent. The mean Barthel index was 70.5 ± 25.4, and the mean Charlson comorbidity index was 5.6 ± 2.2. Correlations between biomarkers were modest (Additional file 1: Table S1).
Table 1.
Clinical characteristics of patients
| Total | End-pointa | No end-pointa | p-value | |
|---|---|---|---|---|
| N = 522 | N = 201 | N = 321 | ||
| Age, years | 82.1 ± 8.7 | 84.2 ± 7.4 | 80.8 ± 9.2 | < 0.001 |
| Female sex | 298 (57.1%) | 123 (61.2%) | 175 (54.5%) | 0.1 |
| Etiology | 0.3 | |||
| IHD | 150 (28.7%) | 45 (22.4%) | 105 (32.7%) | |
| Dilated CM | 9 (1.7%) | 3 (1.5%) | 6 (1.9%) | |
| Hypertensive CM | 207 (39.7%) | 85 (42.3%) | 122 (38.0%) | |
| Alcoholic CM | 7 (1.3%) | 2 (1.0%) | 5 (1.6%) | |
| Valvular disease | 69 (13.2%) | 31 (15.4%) | 38 (11.8%) | |
| Other | 80 (15.4%) | 35 (17.4%) | 45 (20.0%) | |
| LVEFa | 55.8% ± 14 | 56.6% ± 14.2 | 55.4% ± 13.9 | 0.4 |
| NYHA functional class | 0.002 | |||
| I | 8 (1.5%) | 1 (0.5%) | 7 (2.2%) | |
| II | 198 (37.9%) | 63 (31.3%) | 136 (42.4%) | |
| III | 306 (58.6%) | 134 (66.7%) | 175 (54.5%) | |
| IV | 6 (1.1%) | 3 (1.5%) | 3 (0.9%) | |
| Diabetes | 274 (52.4%) | 114 (56.7%) | 160 (49.8%) | 0.1 |
| non insulin-dependent | 157 (30.1%) | 64 (31.8%) | 93 (29.0%) | |
| insulin-dependent | 117 (22.4%) | 50 (24.9%) | 67 (20.9%) | |
| Hypertension | 468 (89.7%) | 184 (91.5%) | 284 (88.5%) | 0.3 |
| COPD | 126 (24.1%) | 54 (26.9%) | 72 (22.4%) | 0.3 |
| Renal failure | 411 (78.7%) | 173 (86.1%) | 238 (74.1%) | 0.001 |
| Anaemia | 341 (65.3%) | 141 (70.1%) | 200 (62.3%) | 0.07 |
| Charlson comorbidity index | 5.6 ± 2.2 | 6.1 ± 2.2 | 5.3 ± 2.1 | < 0.001 |
| Barthel index | 70.5 ± 25.4 | 63.6 ± 26.5 | 74.7 ± 23.7 | < 0.001 |
| Core Readmission risk | 26.3% ± 5.2 | 27.0% ± 5.1 | 25.8% ± 5.2 | 0.009 |
| Urea, mg/dL | 90.8 ± 49.4 | 107.2 ± 56.2 | 80.5 ± 41.8 | < 0.001 |
| Creatinine, mg/dL | 1.4 (1.1–2.0) | 1.5 (1.2–2.1) | 1.8 (1.0–1.79) | < 0.001 |
| Hemoglobin, g/dL | 11.7 ± 1.6 | 11.5 ± 1.6 | 11.9 ± 1.7 | 0.01 |
| Sodium, mmol/L | 137.3 ± 3.8 | 136.9 ± 4.3 | 137.5 ± 3.5 | 0.08 |
| NTproBNP, ng/L | 2770 (1245–5843) | 3900 (1695–7160) | 2170 (1025–4635) | < 0.001 |
| ST2, ng/mL | 42.7 (30.9–63.8) | 54.6 (36.7–79.3) | 37.6 (29.1–52.3) | < 0.001 |
| CA125b, U/ml | 47 (22.4–101.1) | 57.4 (26.7–131.4) | 39.2 (20.2–90.2) | 0.001 |
| Hs-TnIb, ng/L | 23.6 (12.2–61-2) | 28.5 (14.8–67.5) | 21.9 (10.4–57.8) | 0.007 |
aComposite end-point all-cause death or heart failure hospitalization at one year
bAvailable in 466 patients
CM cardiomyopathy, IHD ischemic heart disease, LVEF left ventricular ejection fraction, NYHA New York Heart Association, COPD Chronic obstructive pulmonary disease, CA125 Cancer antigen 125, NTproBNP N-terminal pro-brain natriuretic peptide; hs-TnI high sensitivity troponin I, ST2 Interleukin-1 receptor-like 1
Endpoints
HF-related rehospitalization occurred in 36 patients (6.9%) at 30 days and in 137 (26.2%) at 1 year. Death occurred in 13 patients (2.5%) at 30 days and in 121 (23.2%) at 1 year. Finally, the composite endpoint occurred in 45 patients (8.6%) at 30 days and in 201 (38.5%) at 1 year.
At 30 days, diabetes (p = 0.01), urea (p < 0.05), Barthel index (p = 0.008), Charlson comorbidity index (p < 0.001), NT-proBNP (p = 0.001), and ST2 (p < 0.001) were all associated with the primary composite endpoint in the univariate analyses (Table 2). Diabetes (p = 0.007), Charlson comorbidity index (p = 0.001), NT-proBNP (p = 0.04), and ST2 (p < 0.001) were associated with HF-related rehospitalization (Additional file 2: Table S2). In multivariable analysis, female sex (p = 0.01), Charlson comorbidity index (p < 0.001), and ST2 (p = 0.001) were the only independent variables associated with the primary composite endpoint (Table 2) and also with HF-related rehospitalization [female sex (p = 0.04), Charlson comorbidity index (p = 0.003), and ST2 (p = 0.008)] (Additional file 2: Table S2).
Table 2.
Cox regression analyses for the 30-day primary endpoint (all-cause death or HF-related rehospitalization)
| 30-day composite endpoint | ||||||
|---|---|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | |||||
| HR | 95%CI | p-value | HR | 95%CI | p-value | |
| Age | 1.03 | 0.99–1.07 | 0.2 | – | – | – |
| Female sex | 1.54 | 0.83–2.87 | 0.2 | 2.28 | 1.19–4.37 | 0.01 |
| NYHA | 1.08 | 0.63–1.87 | 0.8 | |||
| Diabetes | 1.59 | 1.11–2.56 | 0.01 | – | – | – |
| Charlson comorbidity index | 1.28 | 1.14–1.44 | < 0.001 | 1.26 | 1.11–1.43 | < 0.001 |
| Barthel index | 0.99 | 0.98–1.00 | 0.008 | – | – | – |
| Urea | 1.01 | 1.00–1.01 | < 0.05 | – | – | – |
| Creatinine | 0.99 | 0.93–1.06 | 0.7 | |||
| Hb | 0.93 | 0.77–1.11 | 0.4 | |||
| Na | 1.05 | 0.97–1.14 | 0.2 | |||
| NT-proBNPa | 1.63 | 1.21–2.19 | 0.001 | – | – | – |
| ST2a | 1.67 | 1.33–2.11 | < 0.001 | 1.53 | 1.19–1.97 | 0.001 |
| CA125a | 1.12 | 0.83–1.51 | 0.5 | |||
| Hs-TnIa | 1.23 | 0.92–1.63 | 0.2 | |||
aLog-transformed and per 1 SD
CA125 cancer antigen 125, NT-proBNP N-terminal pro-brain natriuretic peptide, hs-TnI high-sensitivity troponin I, ST2 Interleukin-1 receptor-like 1
Table 3 and Additional file 3: Table S3 show the results of the univariable and multivariable analyses for the composite endpoint and HF-related rehospitalization at one year, respectively. In multivariate analysis, age (p = 0.003), female sex (p = 0.002), urea (p < 0.001), Charlson comorbidity index (p = 0.008), NT-proBNP (p = 0.04), and ST2 (p < 0.001) remained significantly associated with the composite endpoint (Table 3); only female sex (p = 0.01), urea (p < 0.001), and ST2 (p = 0.001) remained significantly associated with HF-related rehospitalization (Additional file 3: Table S3). Figure 1 shows Kaplan-Meier event-free survival curves for the composite end-point relative to circulating levels of ST2 and NTproBNP. Table 4 shows Cox regression analysis results for all-cause death at 1 year. Age (p < 0.001), female sex (p = 0.008), Charlson comorbidity index (p = 0.001), Barthel index (p = 0.008), ST2 (p < 0.001), and CA125 (p = 0.003) remained independent predictors for all-cause death at 1 year. Figure 2 shows Kaplan-Meier survival curves for all-cause death relative to circulating levels of ST2 and CA125.
Table 3.
Cox regression analyses for the 1-year composite endpoint (all-cause death or HF related rehospitalization)
| 1-year composite endpoint | ||||||
|---|---|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | |||||
| HR | 95%CI | p-value | HR | 95%CI | p-value | |
| Age | 1.04 | 1.02–1.06 | < 0.001 | 1.03 | 1.01–1.06 | 0.003 |
| Female sex | 1.28 | 0.96–1.70 | 0.09 | 1.64 | 1.20–2.23 | 0.002 |
| NYHA | 1.54 | 1.18–2.01 | 0.002 | – | – | – |
| Diabetes | 1.16 | 0.98–1.38 | 0.09 | |||
| Charlson comorbidity index | 1.15 | 1.08–1.22 | < 0.001 | 1.10 | 1.03–1.18 | 0.008 |
| Barthel index | 0.99 | 0.98–0.99 | < 0.001 | – | – | – |
| Urea | 1.01 | 1.01–1.01 | < 0.001 | 1.01 | 1.00–1.01 | < 0.001 |
| Creatinine | 1.00 | 1.00–1.01 | 0.3 | – | – | – |
| Hb | 0.90 | 0.82–0.98 | 0.01 | – | – | – |
| Na | 0.97 | 0.93–1.00 | 0.07 | |||
| NT-proBNPa | 1.43 | 1.25–1.65 | < 0.001 | 1.18 | 1.00–1.38 | 0.04 |
| ST2a | 1.63 | 1.44–1.85 | < 0.001 | 1.41 | 1.21–1.63 | < 0.001 |
| CA125a | 1.32 | 1.15–1.52 | < 0.001 | – | – | – |
| Hs-TnIa | 1.21 | 1.05–1.39 | 0.007 | – | – | – |
aLog-transformed and per 1 SD
CA125 cancer antigen 125, NT-proBNP N-terminal pro-brain natriuretic peptide, hs-TnI high-sensitivity troponin I, ST2 Interleukin-1 receptor-like 1
Fig. 1.

Kaplan-Meier event-free survival curves for the composite end-point relative to serum levels of ST2 (a) and NTproBNP (b) above or below the median
Table 4.
Cox regression analyses for 1-year all-cause death
| 1-year all-cause death | ||||||
|---|---|---|---|---|---|---|
| Univariate | Multivariate | |||||
| HR | 95%CI | p-value | HR | 95%CI | p-value | |
| Age | 1.08 | 1.05–1.11 | < 0.001 | 1.08 | 1.05–1.12 | < 0.001 |
| Female Sex | 1.28 | 0.89–1.85 | 0.2 | 1.73 | 1.16–2.59 | 0.008 |
| NYHA | 2.01 | 1.40–2.90 | < 0.001 | – | – | – |
| Diabetes | 1.03 | 0.83–1.29 | 0.8 | |||
| Charlson comorbidity index | 1.15 | 1.05–1.26 | 0.002 | 1.17 | 1.06–1.28 | 0.001 |
| Barthel index | 0.98 | 0.97–0.99 | < 0.001 | 0.99 | 0.98–1.00 | 0.008 |
| Urea | 1.01 | 1.00–1.01 | < 0.001 | – | – | – |
| Creatinine | 1.00 | 1.00–1.01 | 0.4 | |||
| Hb | 0.87 | 0.77–0.97 | 0.02 | – | – | – |
| Na | 0.97 | 0.93–1.02 | 0.2 | |||
| NT-proBNPa | 1.65 | 1.37–1.98 | < 0.001 | – | – | – |
| ST2a | 1.86 | 1.59–2.18 | < 0.001 | 1.45 | 1.21–1.74 | < 0.001 |
| CA125a | 1.58 | 1.33–1.89 | < 0.001 | 1.35 | 1.11–1.65 | 0.003 |
| Hs-TnIa | 1.29 | 1.09–1.52 | 0.003 | – | – | – |
aLog-transformed and per 1 SD
CA125 cancer antigen 125, NT-proBNP N-terminal pro-brain natriuretic peptide, hs-TnI high-sensitivity troponin I, ST2 Interleukin-1 receptor-like 1
Fig. 2.

Kaplan-Meier survival curves for all-cause death relative to serum levels of ST2 (a) and CA125 (b) above or below the median
Risk prediction
Risk prediction of the composite endpoint at 30 days for the clinical model, including age, sex, diabetes, urea, Charlson comorbidity index, and Barthel index, revealed an AUC of 0.696 [0.609–0.783]. The addition of NT-proBNP and ST2 to the clinical model increased the AUC to 0.750 [0.673–0.827] (p = 0.02) (Fig. 3). Further, reclassification significantly improved [NRI 0.40 (0.08–0.80), IDI 0.02 (− 0.002–0.06)].
Fig. 3.
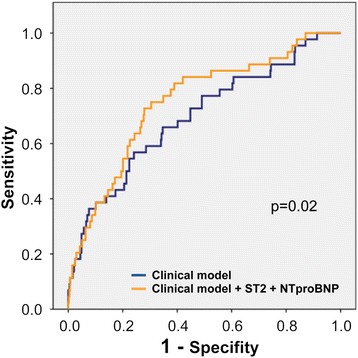
The area under the curve (AUC) for the primary composite endpoint at 30 days for the clinical model and the model with ST2 and NT-proBNP. The clinical model included age, sex, diabetes, urea, Charlson comorbidity index, and Barthel index
Risk prediction of the composite endpoint at 1 year for the clinical model that included age, sex, NYHA class, urea, hemoglobin, Charlson comorbidity index, and Barthel index revealed an AUC of 0.711 [0.665–0.757]. Addition of the 4 studied biomarkers increased the AUC to 0.736 [0.689–0.783] (p = 0.05), and provided significantly better patient reclassification [NRI 0.40 (0.21–0.58), IDI 0.04 (0.01–0.08)]. However, if only NT-proBNP and ST2 (the two biomarkers that were statistically significant in the multivariable analysis) were added to the clinical model, the AUC was virtually the same (0.735 [0.690–0.780]) (p < 0.05 relative to clinical model), and reclassification improvement remained significant as well [NRI 0.38 (0.19–0.55), IDI 0.04 (0.01–0.07)].
Risk prediction for all-cause death at 1 year for the clinical model that included the same covariables revealed an AUC of 0.746 [0.697–0.795]. Addition of the 4 studied biomarkers increased the AUC to 0.789 [0.739–0.838] (p = 0.01). Again, reclassification significantly improved [NRI 0.56 (0.36–0.78), IDI 0.06 (0.02–0.12]. However, if only ST2 and CA125 (the two biomarkers that were statistically significant in the multivariable analysis) were added to the clinical model, the AUC was practically the same (0.786 [0.736–0.836]) (p = 0.02 relative to clinical model), as well as reclassification [NRI 0.60 (0.36–0.80), IDI 0.06 (0.02–0.11)].
Discussion
This study comprehensively analyzed clinical variables and predictive biomarkers to determine their association with 30-day and 1-year adverse events in comorbid frail elderly patients with mainly HFpEF. In terms of clinical prediction, higher multimorbidity is associated with higher risk of all-cause death and readmission both at 30 days [16, 23] and at 1 year [24] despite high-quality multidisciplinary management, especially in the elderly [24, 25]. In our cohort, the Charlson Index as a measure of comorbidity was associated with both composite endpoints at 30 days and 1 year and also with HF-related rehospitalization at 30 days. The prognostic role of the Charlson comorbidity index has been described previously [5, 26], but in our study, it remained independently associated with outcome despite the inclusion of strong predictive biomarker variables. Remarkably, both the primary composite endpoint and the secondary endpoint of 30-day HF rehospitalization were only associated with female sex, Charlson comorbidity index, and ST2.
Notably, predictive biomarkers showed value beyond that of clinical risk factors, since circulating biomarkers have the potential to predict the risk of recurrent hospitalization or death [27, 28]. In our elderly cohort, ST2 emerged as the strongest predictor in both univariate and multivariate analysis for all of the endpoints, which is in line with recent reports [29]. In our study, NT-proBNP, hs-TnI, and CA-125 lost their statistical significance when ST2 and clinical variables were included in the model.
The addiction of circulating ST2 to our model was based on its value as a surrogate of inflammation, stretch, and extracellular matrix status as well as on the observation that the ST2 concentration is not affected by age, renal function [30], or body mass index [31]. These characteristics are highly desirable in a marker that will be used in an elderly population with much comorbidity. Our current data is in line with the notion that ST2 reflects systemic inflammatory disease involving multiple organ systems [32] and that it is related to HFpEF development and to the proinflammatory and profibrotic state [33]. Indeed, it was recently postulated that ST2 is the new “gold standard” for HF prognostication and monitoring [29].
NT-proBNP, a marker of myocardial stretch and neurohormonal activation, is the only biomarker that is currently included in HF guidelines [34] and it has shown incremental diagnostic and prognostic value in HFrEF and HFpEF [35, 36]. However, certain conditions, which are highly prevalent in our patient population, can make it difficult to interpret this versatile biomarker. These conditions include the presence of underlying structural cardiopulmonary diseases (chronic obstructive disease, pulmonary hypertension), anemia, advanced age, atrial fibrillation, female sex, and renal failure, all of which result in high levels of NT-proBNP. By contrast, obesity is well recognized as a condition that reduces circulating NT-proBNP levels. In the current study, NT-proBNP lost its discriminative value: it showed a significant association with the composite endpoint at 1 year, but no significant association with HF-related rehospitalization or 30-day outcomes.
Hs-TnI was included in our analysis because it is generally accepted that troponins offer valuable information for risk stratification during acute decompensation in patients with HFpEF [37]. High levels of hs-TnI have been associated with worse in-hospital, 30-day, and 1-year survival and with longer length of stay and more readmission risk within 30 days [37]. Nevertheless, our data showed that when a multi-biomarker panel was included in the multivariable analysis, hs-TnI lost its predictive value in this high-risk population. Further, as is the case for natriuretic peptides, troponins are strongly influenced by age, history of diabetes mellitus, and lower estimated glomerular filtration rate [38].
CA125 is an interesting biomarker. It has traditionally been linked to ovarian neoplasm, but more recently it has been associated with tissue congestion. Núñez et al. [39] found that CA125 as measured during acute HF hospitalization is an independent predictor of mortality [39]. In our cohort, CA125 also emerged as an independent prognosticator of all-cause death at 1 year, but it did not provide additional value to the primary endpoint at the 30-day or 1-year follow-up. In the STOP-HF Clinic [20] special attention has been paid to treatment of heart congestion; indeed, 100% of the patients were on diuretic therapy, and more than 300 infusions of IV furosemide were administered during the first month of follow-up. The neutral effect of CA125 regarding the composite endpoints may partly be explained by the fact that its assessment was not performed during the acute phase of HF decompensation, where prior works pointed out its value as marker of fluid overload. However, it is remarkable that CA125 remained independently associated with 1-year all-cause mortality regardless it was not measured during the maximum wet phase. Further studies are needed to better understand the value of CA125 in HF.
Historically, it has been much more difficult to estimate the risk of HF hospitalization than to estimate the risk of death [40]. The high rate of readmissions within 30 days post-discharge and during the following year in ageing and comorbid patients highlights the urgency of establishing predictive models with acceptable performance in such patients to guide clinical management and decision making. To our knowledge, the predictive models based on biomarkers that were developed in this study are the first that can be used in this comorbid fragile elderly population with HF. The BIOSTAT-CHF study recently developed and validated three risk models that included biomarkers (natriuretic peptides) to predict all-cause mortality, HF-related hospitalization, and the composite endpoint in a cohort of patients with worsening HF. The patients included in their cohort were a mixture of in-hospital and ambulatory patients with a mean age of 69 years, 27% female, and mean LVEF of 31% [41]; in other words, theirs was a relatively young and mainly male HFrEF population that was quite different from our study cohort. These researchers obtained C-statistic values of 0.73, 0.69, and 0.71 for all-cause mortality, HF-related hospitalization, and the composite endpoint, respectively; these were lower than those reported in the present study, and their follow-up time was 21 months. No short-term predictions were performed.
Limitations
Our study was an observational single-center study with a cohort of elderly patients with comorbidities that mainly had HF of hypertensive etiology and preserved ejection fraction. As such, our results cannot be extrapolated to a global HF population. In fact, the absence of predictive models in such patients may be a strength rather than a limitation given the growing number of HF patients with this phenotype.
The biomarker selection was based on previously described predictive value of the biomarkers, on other information about HF pathways, and on its availability for use in routine clinical practice. The optimal panel of biomarkers remains debatable. One major limitation of this study is the absence of a validation cohort. However, we have not been able to identify a post-discharge cohort with similar clinical characteristics with available multi-biomarker data.
Conclusions
In a comorbid fragile elderly population with mainly HFpEF, ST2 outperformed NT-proBNP for risk prediction of the composite primary endpoint (all-cause mortality or HF-related rehospitalization). Regarding 1-year all-cause mortality, ST2 together with CA125 were independently associated with higher risk and the addition of both biomarkers improved the discriminative accuracy of clinical data. ST2 is a three-in-one biomarker as a surrogate of inflammation, stretch, and extracellular matrix remodeling, and it may be the preferred biomarker for short- and long-term prediction in a high-risk HF population like ours. Comorbidities, as represented by the Charlson comorbidity index, also strongly impacted these patients’ outcomes. Further studies in similar populations are needed to confirm our results.
Additional files
Table S1. Correlations between studied biomarkers. Correlation between the different studied biomarkers was performed using Pearson correlation test of log-transformed values of each biomarker. (DOCX 25 kb)
Table S2. Cox regression analyses for 30-day rehospitalization. A competing risk strategy using the Gray method was adopted, considering death as the competing risk in both univariate and multivariate Cox regression analyses. (DOCX 27 kb)
Table S3. Cox regression analyses for 1-year HF-related hospitalization. A competing risk strategy using the Gray method was adopted, considering death as the competing risk in both univariate and multivariate Cox regression analyses. (DOCX 27 kb)
Acknowledgements
We thank Beatriz González, Roser Cabanes, Margarita Rodríguez, and Carmen Rivas, all of whom are nurses in the HF Unit, for expert help with data collection and for their invaluable work in the unit.
Funding
AB-G was supported by grants from the Ministerio de Educación y Ciencia (SAF2014–59892), Fundació La MARATÓ de TV3 (201502, 201516), CIBER Cardiovascular (CB16/11/00403), and AdvanceCat 2014–2020. JL and SR by grant from Fondo de Investigación Sanitaria, Instituto de Salud Carlos III (FIS PI14/01682).
JN was supported by grants from CIBER Cardiovascular (CB16/11/00420) and PIE15/00013.
Any of these entities had a role in the design, methods, subject recruitment, data collections, analysis and preparation of paper.
Availability of data and materials
Data and material of the study are available from the corresponding author on reasonable request.
Abbreviations
- CA125
Cancer antigen 125
- HF
Heart failure
- HFpEF
Heart failure with preserved ejection fraction
- Hs-TnI
High-sensitivity troponin I
- NT-proBNP
N-terminal pro-brain natriuretic peptide
- ST2
Interleukin-1 receptor-like 1
- STOP-HF-Clinic
STructured multidisciplinary outpatient clinic for Old and frail Post-discharge patients hospitalized for HF
Authors’ contributions
CP: acquisition of subjects and/or data, drafting the manuscript, revision for important intellectual content and approval of the final manuscript. MD: acquisition of subjects and/or data, revision for important intellectual content and approval of the final manuscript. RN: acquisition of subjects and/or data, revision for important intellectual content and approval of the final manuscript. JL: study concept and design, statistical analyses, analysis and interpretation of data, drafting the manuscript, revision for important intellectual content and approval of the final manuscript. JN: analysis and interpretation of data, drafting the manuscript, revision for important intellectual content and approval of the final manuscript. JB: acquisition of subjects and/or data, revision for important intellectual content and approval of the final manuscript. PM: acquisition of subjects and/or data, revision for important intellectual content and approval of the final manuscript. MA: acquisition of subjects and/or data, revision for important intellectual content and approval of the final manuscript. JS: acquisition of subjects and/or data, revision for important intellectual content and approval of the final manuscript. GC: statistical analyses and interpretation of data, revision for important intellectual content and approval of the final manuscript. MCP: acquisition of subjects and/or data, revision for important intellectual content and approval of the final manuscript. SR: analysis and interpretation of data, revision for important intellectual content and approval of the final manuscript. JT: analysis and interpretation of data, revision for important intellectual content and approval of the final manuscript. AB-G: study concept and design, analysis and interpretation of data, drafting the manuscript, revision for important intellectual content and approval of the final manuscript.
Ethics approval and consent to participate
All participants provided written informed consent, and the study was approved by the local ethics committee (Comité Ètic de la Investigació de l’Hospital Universitari Germans Trias i Pujol; EO-10-076). All study procedures were performed in accordance with the ethical standards outlined in the Helsinki Declaration of 1975 as revised in 2013.
Competing interests
JL received lecture honoraria from Roche Diagnostics and reports a relationship with Critical Diagnostics.
JN received board membership fees and travel expenses from Novartis, Roche Diagnostics, Abbott, Rovi, and Vifor.
AB-G received board membership fees and travel expenses from Novartis and Roche Diagnostics and reports a relationship with Critical Diagnostics.
The rest of the authors have no disclosures to mention.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12877-018-0807-2) contains supplementary material, which is available to authorized users.
Contributor Information
Cristina Pacho, Email: cristina.pacho@gmail.com.
Mar Domingo, Email: madote@gmail.com.
Raquel Núñez, Email: rnunez.germanstrias@gencat.cat.
Josep Lupón, Email: jlupon.germanstrias@gencat.cat.
Julio Núñez, Email: yulnunez@gmail.com.
Jaume Barallat, Email: jbarallat@gmail.com.
Pedro Moliner, Email: pmolinerborja@gmail.com.
Marta de Antonio, Email: mdeantonio@hotmail.com.
Javier Santesmases, Email: jsantesmases.germanstrias@gencat.cat.
Germán Cediel, Email: gecediel@yahoo.com.
Santiago Roura, Email: sroura@gmail.com.
M. Cruz Pastor, Email: mcpastor.germanstrias@gencat.cat.
Jordi Tor, Email: jtor.germanstrias@gencat.cat.
Antoni Bayes-Genis, Phone: +34 934978915, Email: abayesgenis@gmail.com.
References
- 1.Fonarow GC. Epidemiology and risk stratification in acute heart failure. Am Heart J. 2008;155:200–207. doi: 10.1016/j.ahj.2006.10.043. [DOI] [PubMed] [Google Scholar]
- 2.Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dharmarajan K, Krumholz HM. Strategies to reduce 30-day readmissions in older patients hospitalized with heart failure and acute myocardial infarction. Curr Geriatr Rep. 2014;3:306–315. doi: 10.1007/s13670-014-0103-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Desai AS, Stevenson LW. Rehospitalization for heart failure: predict or prevent? Circulation. 2012;126:501–506. doi: 10.1161/CIRCULATIONAHA.112.125435. [DOI] [PubMed] [Google Scholar]
- 5.Arora S, Lahewala S, Hassan Virk HU, Setareh-Shenas S, Patel P, Kumar V, et al. Etiologies, trends, and predictors of 30-day readmissions in patients with diastolic heart failure. Am J Cardiol. 2017;120:616–24. doi: 10.1016/j.amjcard.2017.05.028. [DOI] [PubMed] [Google Scholar]
- 6.Chioncel O, Mebazaa A, Harjola VP, Coats AJ, Piepoli MF, Crespo-Leiro MG, et al. Clinical phenotypes and outcome of patients hospitalized for acute heart failure: the ESC heart failure long-term registry. Eur J Heart Fail. 2017;19:1242–54. doi: 10.1002/ejhf.890. [DOI] [PubMed] [Google Scholar]
- 7.Writing Group Members, Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. American Heart Association Statistics Committee; Stroke Statistics Subcommittee. Heart disease and and stroke statistics--2016 update: a report from the American Heart Association. Circulation 2016;133:447–54. [DOI] [PubMed]
- 8.Farré N, Vela E, Clèries M, Bustins M, Cainzos-Achirica M, Enjuanes C, et al. Medical resource use and expenditure in patients with chronic heart failure: a population-based analysis of 88 195 patients. Eur J Heart Fail. 2016;18:1132–1140. doi: 10.1002/ejhf.549. [DOI] [PubMed] [Google Scholar]
- 9.Ambrosy AP, Fonarow GC, Butler J, Chioncel O, Greene SJ, Vaduganathan M, Nodari S, et al. The global hearth and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol. 2014;63:1123–1133. doi: 10.1016/j.jacc.2013.11.053. [DOI] [PubMed] [Google Scholar]
- 10.McMurray JJ, Pfeffer MA. Heart failure. Lancet. 2005;365:1877–1889. doi: 10.1016/S0140-6736(05)66621-4. [DOI] [PubMed] [Google Scholar]
- 11.Curtis LH, Whellan DJ, Hammill BG, Hernandez AF, Anstrom KJ, Shea AM, et al. Incidence and prevalence of heart failure in elderly persons, 1994–2003. Arch Intern Med. 2008;168:418–424. doi: 10.1001/archinternmed.2007.80. [DOI] [PubMed] [Google Scholar]
- 12.Wong CY, Chaudhry SI, Desai MM, Krumholz HM. Trends in comorbidity, disability, and polypharmacy in heart failure. Am J Med. 2011;124:136–43. doi: 10.1016/j.amjmed.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van Riet EE, Hoes AW, Wagenaar KP, Limburg A, Landman MA, Rutten FH. Epidemiology of heart failure: the prevalence of heart failure and ventricular dysfunction in older adults over time. A systematic review. Eur J Heart Fail. 2016;18:242–252. doi: 10.1002/ejhf.483. [DOI] [PubMed] [Google Scholar]
- 14.Lazzarini V, Mentz RJ, Fiuzat M, Metra M, O'Connor CM. Heart failure in elderly patients: distinctive features and unresolved issues. Eur J Heart Fail. 2013;15:717–723. doi: 10.1093/eurjhf/hft028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Comin–colet J, Verdu-Rotellar JM, Vela E, Clèries M, Bustins M, Mendoza L, et al. working group of the Integrated Program for Heart Failure Management of the Barcelona Litoral Mar Integrated Health Care Area, Spain. Efficacy of an integrated hospital-primary care program for heart failure: a population-based analysis of 56,742 patients. Rev Esp Cardiol. 2014;67:283–93. [DOI] [PubMed]
- 16.Davis JD, Olsen MA, Bommarito K, LaRue SJ, Saeed M, Rich MW, et al. All-payer analysis of heart failure hospitalization 30-day readmission: comorbidities matter. Am J Med. 2017;130:93.e9–93.e28. doi: 10.1016/j.amjmed.2016.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steyerberg EW. Clinical prediction models: a practical approach to Develeopment validation and updating. 1. New York: Springer; 2009. Applications of prediction models. [Google Scholar]
- 18.Dunbar-Yaffe R, Stitt A, Lee JJ, Mohamed S, Lee DS. Assessing risk and preventing 30-day readmissions in decompensated heart failure: opportunity to intervene? Curr Heart Fail Rep. 2015;12:309–317. doi: 10.1007/s11897-015-0266-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lupón J, de Antonio M, Galán A, Vila J, Zamora E, Urrutia A, et al. Combined use of the novel biomarkers high-sensitivity troponin T and ST2 for heart failure risk stratification vs conventional assessment. Mayo Clin Proc. 2013;88:234–243. doi: 10.1016/j.mayocp.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 20.Correale M, Monaco I, Brunetti ND, Di Biase M, Metra M, Nodari S, et al. Master Program Students on Drug Development for Heart Failure. Redefining biomarkers in heart failure. Heart Fail Rev. 2018;23:237–53. doi: 10.1007/s10741-018-9683-2. [DOI] [PubMed] [Google Scholar]
- 21.Pacho C, Domingo M, Nuñez R, Lupón J, Moliner P, de Antonio M, González B, et al. Early Postdischarge STOP-HF-Clinic reduces 30-day readmissions in old and frail patients with heart failure. Rev Esp Cardiol (Engl Ed) 2017;70:631–638. doi: 10.1016/j.recesp.2016.12.026. [DOI] [PubMed] [Google Scholar]
- 22.Ho KK, Anderson JM, Kannel WB, Grossman W, Levy D. Survival after the onset of congestive heart failure in Framingham HEart study subjects. Circulation. 1993;88:107–115. doi: 10.1161/01.CIR.88.1.107. [DOI] [PubMed] [Google Scholar]
- 23.Wiley JF, Chan YK, Ahamed Y, Ball J, Carrington MJ, Riegel B, et al. Multimorbidity and the risk of all-cause 30-day readmission in the setting of multidisciplinary Management of Chronic Heart Failure: a retrospective analysis of 830 hospitalized patients in Australia. J Cardiovasc Nurs. 2017; 10.1097/JCN.0000000000000391. [Epub ahead of print] [DOI] [PubMed]
- 24.Rosamond W, Flegal K, Furie K, Go A, Greenlund K, Haase N, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics – 2008 an update: a report from the American Heart Association statistics Commitee and stroke statistics Subcommitee. Circulation 2008;117:e25-e146. [DOI] [PubMed]
- 25.Giamouzis G, Kalogeropoulos A, Georgiopoulou V, Laskar S, Smith AL, Dunbar S, et al. Hospitalization epidemic in patients with heart failure: risk factors, risk prediction, knowledge gaps, and future directions. J Card Fail. 2011;17:54–75. doi: 10.1016/j.cardfail.2010.08.010. [DOI] [PubMed] [Google Scholar]
- 26.Au AG, McAlister FA, Bakal JA, Ezekowitz J, Kaul P, van Walraven C. Predicting the risk of unplanned readmission or death within 30 days of discharge after a heart failure hospitalization. Am Heart J. 2012;164:365–372. doi: 10.1016/j.ahj.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 27.Demissei BG, Postmus D, Cleland JG, O'Connor CM, Metra M, Ponikowski P, et al. Plasma biomarkers to predict or rule out early post-discharge events after hospitalization for acute heart failure. Eur J Heart Fail. 2017;19:728–738. doi: 10.1002/ejhf.766. [DOI] [PubMed] [Google Scholar]
- 28.Bayes-Genis A, Núñez J, Núñez E, Martínez JB, Ferrer MP, de Antonio M, et al. Multi-biomarker profiling and recurrent hospitalizations in heart failure. Front Cardiovasc Med. 2016;3:37. doi: 10.3389/fcvm.2016.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bayes-Genis A, Núñez J, Lupón J. Soluble ST2 for prognosis and monitoring in heart failure: the new gold standard? J Am Coll Cardiol. 2017;70:2389–2392. doi: 10.1016/j.jacc.2017.09.031. [DOI] [PubMed] [Google Scholar]
- 30.Maisel AS, Richards M, Pascual-Figal D, Mueller C. Serial ST2 testing in hospitalized patients with acute heart failure. Am J Cardiol. 2015;115(7 Suppl):32B–37B. doi: 10.1016/j.amjcard.2015.01.038. [DOI] [PubMed] [Google Scholar]
- 31.Chow SL, Maisel AS, Anand I, Bozkurt B, de Boer RA, Felker GM, et al; American Heart Association Clinical Pharmacology Committee of the Council on Clinical Cardiology; Council on Basic Cardiovascular Sciences; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; Council on Epidemiology and Prevention; Council on Functional Genomics and Translational Biology; and Council on Quality of Care and Outcomes Research. Research role of biomarkers for the prevention, assessment, and Management of Heart Failure: a scientific statement from the American Heart Association. Circulation 2017;135:e1054-e1091. [DOI] [PubMed]
- 32.Bayes-Genis A, Januzzi JL, Gaggin HK, de Antonio M, Motiwala SR, Zamora E, et al. ST2 pathogenetic profile in ambulatory heart failure patients. J Card Fail. 2015;21:355–361. doi: 10.1016/j.cardfail.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 33.Zile MR, Baicu CF, Ikonomidis JS, Stroud RE, Nietert PJ, Bradshaw AD, et al. Myocardial stiffness in patients with heart failure and a preserved ejection fraction: contributions of collagen and titin. Circulation. 2015;131:1247–1259. doi: 10.1161/CIRCULATIONAHA.114.013215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Colvin MM, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the Management of Heart Failure: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2017;70:776–803. doi: 10.1016/j.jacc.2017.04.025. [DOI] [PubMed] [Google Scholar]
- 35.Mallick A, Januzzi JL., Jr Biomarkers in acute heart failure. Rev Esp Cardiol. 2015;68:514–525. doi: 10.1016/j.recesp.2015.02.009. [DOI] [PubMed] [Google Scholar]
- 36.Kang S, Park JJ, Choi D, Yoon CH, Oh IY, Kang SM, et al. KorHF Registry. Prognostic value of NT-proBNP in heart failure with preserved versus reduced EF. Heart. 2015;101:1881–8. doi: 10.1136/heartjnl-2015-307782. [DOI] [PubMed] [Google Scholar]
- 37.Pandey A, Golwala H, Sheng S, DeVore AD, Hernandez AF, Bhatt DL, et al. Factors associated with and prognostic implications of cardiac troponin elevation in decompensated heart failure with preserved ejection fraction: findings from the American Heart Association get with the guidelines–heart failure program. JAMA Cardiol. 2017;2:136–45. doi: 10.1001/jamacardio.2016.4726. [DOI] [PubMed] [Google Scholar]
- 38.Jhund PS, Claggett BL, Voors AA, Zile MR, Packer M, Pieske BM, et al. PARAMOUNT Investigators. Elevation in high-sensitivity troponin T in heart failure and preserved ejection fraction and influence of treatment with the angiotensin receptor Neprilysin inhibitor LCZ696. Circ Heart Fail. 2014;7:953–9. doi: 10.1161/CIRCHEARTFAILURE.114.001427. [DOI] [PubMed] [Google Scholar]
- 39.Núñez J, Núñez E, Consuegra L, Sanchis J, Bodí V, Martínez-Brotons A, et al. Carbohydrate antigen 125: an emerging prognostic risk factor in acute heart failure? Heart. 2007;93:716–721. doi: 10.1136/hrt.2006.096016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ouwerkerk W, Voors AA, Zwinderman AH. Factors influencing the predictive power of models for predicting mortality and/or heart failure hospitalization inpatients with heart failure. JACC Heart Fail. 2014;2:429–436. doi: 10.1016/j.jchf.2014.04.006. [DOI] [PubMed] [Google Scholar]
- 41.Voors AA, Ouwerkerk W, Zannad F, van Veldhuisen DJ, Samani NJ, Ponikowski P, et al. Development and validation of multivariable models to predict mortality and hospitalization in patients with heart failure. Eur J Heart Fail. 2017;19:627–634. doi: 10.1002/ejhf.785. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Correlations between studied biomarkers. Correlation between the different studied biomarkers was performed using Pearson correlation test of log-transformed values of each biomarker. (DOCX 25 kb)
Table S2. Cox regression analyses for 30-day rehospitalization. A competing risk strategy using the Gray method was adopted, considering death as the competing risk in both univariate and multivariate Cox regression analyses. (DOCX 27 kb)
Table S3. Cox regression analyses for 1-year HF-related hospitalization. A competing risk strategy using the Gray method was adopted, considering death as the competing risk in both univariate and multivariate Cox regression analyses. (DOCX 27 kb)
Data Availability Statement
Data and material of the study are available from the corresponding author on reasonable request.


