Abstract
Objective
Disinhibited social engagement disorder (DSED) is poorly understood beyond early childhood. In a sample of children who experienced severe, early deprivation, we examined the course of DSED signs from early childhood to early adolescence using variable-centered (linear mixed modeling) and person-centered (growth mixture modeling) approaches.
Method
124 children with a history of institutional care from a randomized controlled trial of foster care as an alternative to institutional care, as well as 69 community comparison children matched on age and sex were included in the study. DSED signs were assessed at baseline (mean age of 22 months), age 30, 42, and 54 months, and age 8 and 12 years using a validated caregiver report of disturbed attachment behavior.
Results
Variable-centered analyses based on intent-to-treat groups indicated that signs of DSED decreased sharply for children randomized to foster care and decreased slightly but remained elevated for children randomized to care as usual. Person-centered analyses revealed four profiles (i.e., elevated, persistent modest, early decreasing, and minimal). Elevated and persistent modest courses were associated with greater placement disruptions (F[3,99]=4.29, p=.007 partial η2=.12), later age of placement into foster care (F[3,56]=3.41, p<.05, partial η2=.16), and more time in institutional care (F[3,115]=11.91, p<.001, partial η2=.24) compared to decreasing and minimal courses.
Conclusion
Early and sustained placement into families following deprivation is associated with minimal or decreasing signs of DSED across development. Reducing the amount of time children spend in institutions and preserving placements may help reduce signs of DSED into early adolescence among previously institutionalized children.
Keywords: Disinhibited social engagement disorder, institutional care, deprivation, disinhibited attachment disorder, indiscriminate behavior
Introduction
Disinhibited social engagement disorder (DSED) is one of the most pervasive clinical sequelae of severe neglect. In young children, it is characterized by overly familiar verbal or physical behavior, willingness to depart with an unfamiliar adult without hesitation, and a tendency to fail to track or check back with a caregiver in unfamiliar settings.1,2 DSED is also referred to as “indiscriminant friendliness,” “indiscriminant sociability,” or “disinhibited social behavior” because affected children exhibit overly familiar behavior or seek comfort and support from relatively unfamiliar adults even in the presence of a familiar caregiver.3–5
Indiscriminant behavior in early childhood has been studied extensively. Signs of DSED in early childhood have been consistently identified in samples of children living in foster care and in samples of children living in or previously removed from institutions.6–12 However, despite a strong association with early psychosocial deprivation, past research indicates that removal of children from institutional care does not reduce signs of DSED for all children.6,9,13,14 Children with signs of DSED in early life are at increased risk for psychopathology and difficulties with peers.15–18
In middle childhood and adolescence, signs of DSED are also associated with a history of psychosocial deprivation,19–22 however, more work is needed to explore how manifestations of DSED in middle childhood and adolescence relate to the well-studied early childhood phenotype. A longitudinal perspective can be especially valuable to examine the course of signs of DSED from early childhood to adolescence among children who experienced deprivation.
Only a few studies have examined the course of DSED across development. Previously, we demonstrated that signs of DSED decreased significantly from baseline (average age=22 months) to 8 years among children in Romania exposed to institutional care.23 Lawler and colleagues14 reported on physical (e.g., overly familiar physical behavior) and nonphysical (e.g., overly familiar verbal behavior) disinhibited social behavior from age 26 to 48 months in a sample of internationally adopted children residing in the United States. In general, signs of DSED remained high over time, however, the study followed children through age 4 years.
The most extensive examination of the course of DSED beyond early childhood was in the English and Romanian Adoptees Study (ERAS).9,21,22 They examined DSED signs from age 4 to early adulthood in sample of children raised in Romanian institutions and later adopted by families in the United Kingdom. Signs of DSED for these previously institutionalized children were stable following adoption from age 4 to 6 years (62% had no change in DSED signs)9 and persisted but slightly decreased in frequency from age 6 to 11 years (54% had persistent mild to marked DSED signs).20 Signs of DSED in a subset of children in the ERAS who spent more than 6 months in the institution were examined in a follow-up that extended into early adulthood (22–25 years).22 The proportion of children demonstrating at least mild signs of DSED appeared to plateau at approximately 15% following age 11 years and remain around 15% into early adulthood. Taken together, past work has demonstrated that signs of DSED may persist following early childhood, however, all such approaches have focused on group level changes, rather than allowing for potential variability in the developmental course of DSED.
Change over time can be characterized using variable-centered (e.g., linear mixed modeling) or person-centered (e.g., growth mixture modeling) approaches. Each approach provides different yet complimentary information about growth trajectories over time.24 Variable-centered approaches identify across-sample, fixed group trends examining mean change and relationships between variables for an entire sample or pre-identified groups within a sample.25 With variable-centered approaches, all research participants in a given sample or group are assumed to be drawn from a single population, and thus expected to change in similar and predictable ways over time. In contrast, person-centered analyses allow for a nuanced examination of individual differences outside of predetermined groups of interest by examining the presence of meaningful, data-derived subgroups defined by unique profiles or trajectories within a sample.26 A combination of both variable-centered and person-centered techniques offers the most comprehensive analysis of the longitudinal course of signs of DSED over time. The variable-centered analyses provide a context within which to review and critique findings from person-centered analyses since person-centered analyses are inherently exploratory, and therefore, susceptible to misinterpretation and over-extension.27
We examined data from the Bucharest Early Intervention Project (BEIP), the only RCT of foster care as an alternative to care as usual. This allows us to examine signs of DSED from early childhood to early adolescence in children exposed to severe, early deprivation, along with age and sex matched comparison children who were never institutionalized.28 Previously, we have shown that signs of DSED are more often identified among young children raised in institutions than those never institutionalized.8,23 Further, we have shown that removal from institutions and placement in foster care leads to reductions in signs of DSED in early childhood6,23 and early adolescence.19 What is not clear from previous analyses are the group- as well as individual-level patterns of change in DSED, or the variables associated with different patterns of DSED signs across development.
Based on previous findings about DSED from the BEIP,6,19,23 we predicted that, from early childhood to early adolescence, children who did not experience early deprivation would not have meaningfully elevated levels of DSED signs, that children randomized to foster care would demonstrate a rapid decline in DSED signs, and that children randomized to the care as usual would demonstrate a slow, but more modest, decline in signs of DSED. We predicted that a person-centered analyses would reveal patterns similar to variable-centered analyses, recognizing the potential for the emergence of additional profiles that could not be predicted a priori given that person-centered analyses are exploratory in nature. Finally, we predicted person-centered analyses would demonstrate that persistent signs of DSED are associated with longer time spent in institutional care and a later age of placement into families.
Method
Participants
Research participants included 193 children with usable data from the BEIP and community comparison children. The original sample consisted of 136 infants and toddlers recruited from institutions in Bucharest and randomized after a baseline assessment (M age=22.49 months, SD=5.63) into either a care as usual group (CAUG; n=68) or a foster care group (FCG; n=68).28 The never institutionalized group (NIG; n=72) comprised an additional group of community comparison children recruited at baseline. Community comparison children were recruited from the hospitals in which the ever-institutionalized children were born and matched on age and sex. Participation varied across data collection; analyses in this report included 61 CAUG children, 63 FCG children, and 69 NIG children (see Figure S1, available online). In addition to a baseline assessment, research participants were assessed at age 30, 42, and 54 months, at which time the RCT intervention ended, and oversight of the foster care network was transferred to local governmental control. Follow-up assessments were conducted at age 8 and 12 years. Details about the original sample are available in Supplement 1, available online.
The BEIP was conducted in collaboration with the Institute of Maternal and Child Health of the Romanian Ministry of Health. Protocols were reviewed and approved by the local Commissions on Child Protection in Bucharest as well as institutional review boards of the three principal investigators (BLINDED). All assessments at the 8- and 12-year follow-ups were reviewed by a standing data safety monitoring board in Bucharest. The 12- year follow-up was also reviewed by an Ethics Committee at Bucharest University. As required by Romanian law, each child’s legal guardian provided consent to participate. Assent was obtained from the children at age 8 and 12 years for each procedure. Discussions of ethical considerations of the study by us and by others are available elsewhere.29–33
Procedure
Children were randomly assigned to the CAUG or FCG following baseline assessment. These groups were indistinguishable on demographic and caregiving quality features.34 All placement decisions following randomization were made by Romanian child protection officials. Analyses were based on original RCT placement (i.e., using an intent-to-treat [ITT] design).
Measures
Disturbances of Attachment Interview
Signs of DSED were assessed using a semi-structured interview of caregivers about signs of disordered attachment that has been widely used and validated at younger ages.8,12,13,23,35 The Disturbances of Attachment Interview was translated into Romanian, back-translated into English, and assessed for meaning at each step by bilingual research staff. The mother reported on children living with biological or foster parents and an institutional caregiver who knew the child well reported on children living in the institution. Caregivers responded to probes about their child’s attachment behavior and the behaviors were rated as rarely or never present, somewhat or sometimes present, or clearly present. The disinhibited social behavior scale was comprised 3 items (lack of shyness around strangers; getting too close physically; asking overly personal or intrusive questions). The use of only three items to assess DSED was necessary as these items were identical across assessment waves, which allowed for consistency of measurement. Additional items added to identify signs of DSED in older children were included at later waves and were not included in the present study. The range for possible scores on the disinhibited social behavior scale was 0 to 6, with higher scores indicating more signs of DSED.
Intervention
The BEIP team recruited and trained 56 foster parents to care for 68 children.28,36 The foster parents were supported by social workers in Bucharest who received regular consultation from clinicians in the U.S. Parents were explicitly encouraged to care for their foster children as if they were their own children and to make full and lasting commitments to them.
Data Analysis
Signs of DSED were assessed longitudinally using variable- and person-centered approaches. The first approach, linear mixed modeling, used a variable-centered method to examine the effect of group assignment and institutional care history on trajectories of DSED signs. LMM accounts for the non-independence of repeated measures within individuals, and handles data from research participants with differing numbers of observations and intervals between assessment waves. Restricted maximum likelihood estimation in Mixed Models in SPSS37 (version 23) was used. Degrees of freedom were calculated using the Satterthwaite method38, in order to reduce type I error rates, which can result in fractional degrees of freedom. Linear, quadratic, and cubic terms for child age in months (i.e., age, age-squared, and age-cubed) as well as age by group interactions were tested to examine developmental changes in DSED. Fixed slope and random intercept terms were included. Given that greater changes were observed earlier in development, a natural log transformation was applied to the age values after subtracting a constant from each value so that the earliest age was represented by a value of 0. The actual age represented by the transformed age variables are presented in Figure 1. Main effects and interaction terms with group were tested for the linear, quadric, and cubic metrics for age. Additional predictors were retained in the model if the terms were at least trend level (p<.10) in the prediction of DSED signs.
Figure 1.
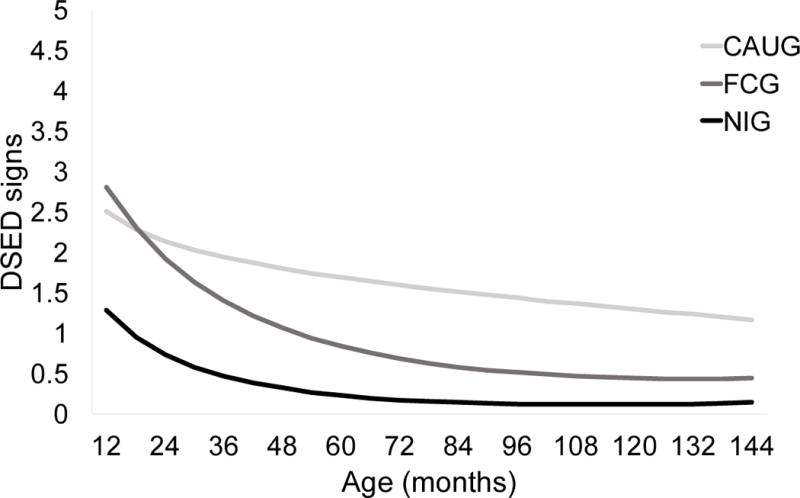
Estimated disinhibited social engagement disorder (DSED) signs as a function of group across development.
Note: CAUG=care as usual group. FCG=foster care group. NIG=never institutionalized group
Growth mixture modeling, is a person-centered, data-driven approach that identifies latent subgroups within the larger sample with similar growth trajectories across assessment waves.27 Probabilities of membership to each identified profile (trajectory) are used to classify research participants into profiles. Data were analyzed using Mplus version 739; missing data were addressed using Maximum Likelihood Ratio, a type of full-information maximum likelihood estimation. Models for a 2-, 3-, 4-, and 5-profile solution were tested to determine the optimal number of profiles for the data. Each model was evaluated based on fit statistics and considerations of theory. Fit indices examined included the Bayesian information criteria statistic value, Lo, Mendell, and Rubin likelihood ratio test40 and bootstrap likelihood ratio test. The model with the lowest Bayesian information criteria statistic value is considered to be the best-fitting model.41 The Lo, Mendell, and Rubin likelihood ratio test40 and bootstrap likelihood ratio test determine whether the addition of each class improves upon the previous model. For example, the indices test whether a 3-profile model fits the data better than a 2-profile model.
Results
Linear Mixed Modeling Analysis of DSED Signs
DSED scores were examined as a function of age using linear mixed modeling. Group status (i.e., CAUG, FCG, and NIG) was examined in relation to the intercept and slope across development. Three age models were examined (linear, quadratic, and cubic age), and given that the cubic age term interacted with group status (p=.051), this model was retained (see Table S1, available online). As can be observed in Figure 1, both the FCG and CAUG groups, on average, had more DSED signs in early life (e.g., until approximately age 20 months) compared to the NIG and did not differ from one another. Further, as predicted, the ITT effects became more apparent as time in foster placement continued to the end of the formal intervention (age 54 months), at which age the FCG had significantly fewer DSED signs than the CAUG. The FCG, on average, had low levels of signs of DSED from age 54 months until early adolescence, whereas the CAUG, declined in DSED signs from early childhood, on average had relatively elevated signs throughout childhood and into early adolescence.
Growth Mixture Modeling of DSED Signs
Latent profiles of DSED signs from baseline to 12 years of age were examined using growth mixture modeling. Given model fit parameters, models were specified using a Poisson error distribution. Models for 2 through 5 profile solutions were tested to arrive at the optimal number of profiles. Fit indices are presented in Table S2 (available online). The Bayesian information criteria and Lo-Mendel-Rubin likelihood ratio test values suggested that the 3-profile model provided the best fit, however, the BIC value for the 4-profile model was similar, and the bootstrap likelihood ratio test indicated that a 4-profile model improved upon a 3-profile model. Furthermore, the bootstrap likelihood ratio test has been shown to have better performance compared to the Lo-Mendel-Rubin likelihood ratio test in identifying the most appropriate number of profiles.42 Therefore, the 4-profile model was chosen as the final model based on fit indices as well as empirical considerations.
Trajectories for the 4-profile solution are presented in Figure 2. One profile, labeled “elevated” contains children who had high levels of DSED signs early in life and continued to be elevated across assessment waves with a gradual decrease into adolescence. Another, labeled “early decreasing” contains children who initially had high scores in early life followed by a pronounced decrease in DSED signs across waves. The remaining two profiles depict relatively stable courses of signs over time. One profile, labeled “persistent modest” contains children who consistently were rated in the low to moderate range across assessment waves. The third profile, labeled “minimal” contains children who consistently demonstrated few to no signs of DSED across waves.
Figure 2.
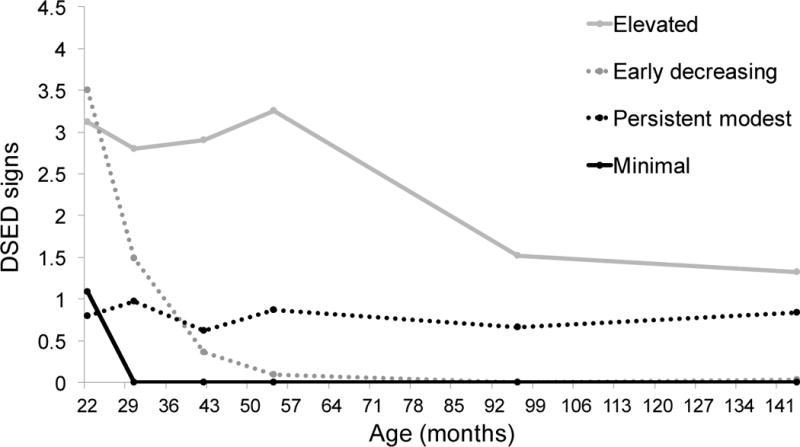
Observed disinhibited social engagement disorder (DSED) signs over time for each profile.
Associations with Group and Sex
A significant relation between group and profile was revealed indicating that the profiles contain different distributions of children across groups (χ2[6]=72.60, p<.001; see Table 1 for the distribution of the number of children in each DSED symptom profile by group membership). The elevated and persistent modest profiles comprised mostly children from the CAUG and FCG. The early decreasing profile contained mostly children from the FCG and NIG, and only a small number of children from the CAUG (n=5). Finally, the minimal profile contained the largest proportion of NIG children. There was no relationship between sex and DSED profile (χ2[3]=4.29, p=.232).
Table 1.
Group Membership and Sex by disinhibited social engagement disorder (DSED). Symptom Profile
| Elevated (n=63) |
Early decreasing (n=36) |
Persistent modest (n=39) |
Minimal (n=55) |
|
|---|---|---|---|---|
| CAUG (n=61) | 35 (55.5%) | 5 (14%) | 20 (51%) | 1 (2%) |
| FCG (n=63) | 20 (32%) | 18 (50%) | 11 (28%) | 14 (25%) |
| NIG (n=69) | 8 (12.5%) | 13 (36%) | 8 (21%) | 40 (73%) |
|
| ||||
| Female (n=101) | 27 (43%) | 19 (53%) | 21 (54%) | 34 (62%) |
| Male (n=92) | 36 (57%) | 17 (47%) | 18 (46%) | 21 (38%) |
Note:. CAUG=care as usual. FCG=foster care group. NIG=never institutionalized group.
Associations with Age of Placement and Institutional Care History
DSED profiles were compared in terms of age of placement into foster care (among the FCG only [n=63]), and age of first placement into a family (for the FCG and CAUG children ever placed in family care [n=124]).
Among all ever-institutionalized children (EIG), placement disruptions and percent time spent in the institution through age 54 months and from 54 months to 12 years was also compared between profiles. We found a significant association between age at placement into foster care and DSED profile (F[3,56]=3.41, p<.05, partial η2=.16; see Table S3, available online). FCG children in the elevated (M=25.99, SD=6.00) and early decreasing (M=23.98, SD=7.16) profiles were, on average, placed into foster care at significantly older ages than children in the minimal profile (M=18.61, SD=7.27).
Age placed into a family for children in the FCG and CAUG also was associated with DSED profile (F[3,114]=7.24, p<.001, partial η2=.16). Children in the elevated (M=35.59, SD=15.76) and persistent modest (M=35.83, SD=17.93) profiles were, on average, first placed into families at significantly older ages than children in the early decreasing (M=25.35, SD=13.11) and minimal (M=18.18, SD=6.97) profiles. Therefore, placement into families at an older age was associated with elevated and modest levels of DSED signs across development.
Placement disruptions through age 54 months did not differ significantly by DSED profile (F[3,111]=1.05, p=.374 partial η2=.03), however, placement disruptions through age 12 years, controlling for disruptions through age 54 months, did differ significantly by profile (F[3,99]=4.29, p=.007 partial η2=.12). Children in the elevated profile, on average, experienced more disruptions during childhood and early adolescence (M=3.49, SD=1.65) than children in the minimal group (M=2.42, SD=0.90). Children in the persistent modest profile, on average, experienced more disruptions in placement during childhood and early adolescence (M=4.45, SD=1.77) compared to all other profiles.
Percent time in institutional care through age 54 months differed significantly between DSED profiles (F[3,115]=11.91, p<.001, partial η2=.24). Children in both the elevated (M=62.63, SD=23.05) and persistent modest (M=61.48, SD=27.62) profiles, on average, spent greater percent time in institutional care through age 54 months compared to children in the early decreasing (M=39.18, SD=19.22) and minimal (M=29.60, SD=12.65) profiles. Therefore, a greater percentage of time spent in institutional care was associated with elevated and modest persistent signs of DSED across development. Percent time in institutional care through age 12, controlling for through age 54 months, did not differ significantly by profile (F[3,99]=0.41, p=.749, partial η2=.01).
Discussion
The present study examined the course of DSED from early childhood to early adolescence in 124 children with a history of institutional rearing and 69 community comparison children. Patterns of DSED signs across development were identified using both variable- and person-centered statistical approaches. Signs of DSED persisted from early childhood to early adolescence for children with a history of institutional rearing, especially if they were placed in families at older ages, had more placement disruptions, and spent more time in institutional care. Trajectories of minimal and early decreasing signs of DSED were common among children with and without institutional care histories. For those with a history of institutional care, minimal or decreasing signs of DSED were associated with earlier and sustained placement in families and less time in institutional care.
The use of variable- and person-centered analyses provided different perspectives on the longitudinal course of DSED from early childhood to early adolescence. Variable-centered analyses examined patterns of change within each intervention group (assigned at baseline) and demonstrated that signs of DSED for children with a history of institutional placement decreased from baseline to age 54 months, with the sharpest decrease observed in the FCG, reflecting a robust effect of the RCT intervention and consistency with prior work from this sample.23 These findings extend upon prior work from this sample by showing that DSED signs remain stable or slightly decrease into adolescence, as suggested by the decline in DSED signs from age 54 months to 8 years in a previous report on this sample.23 Particularly given the long-term persistence of signs of DSED in some children following early deprivation, reducing exposure to institutional care through family placements should be a priority for abandoned infants and young children.
Our findings differ from Lawler and colleagues14 who reported high, sustained levels of DSED signs through 48 months among internationally adopted children, all placed in families in the United States. The fact that not all children in the BEIP exhibited high, sustained levels if indiscriminate behavior may be due to the fact that a greater proportion of children in the BEIP were placed earlier in life compared to children in the Lawler and colleagues study. After 54 months, the age in which support for the foster care intervention was transferred to local Romanian authorities, DSED signs appeared to plateau for both the CAUG and FCG, indicating that at least on the group level, there was stability of DSED levels into adolescence. These findings are consistent with Sonuga-Barke and colleagues22 who reported a sustained plateau of symptoms across middle childhood and adolescence in their sample of post-institutionalized Romanian children adopted into the United Kingdom. Therefore, we provide evidence that signs of DSED may emerge early in life and that elevated levels in early life may persist into early adolescence and adulthood.
Person-centered analyses identified common patterns of change in the data. The elevated, minimal, and early decreasing profiles were similar to those observed in the variable-centered analyses and contained expected proportions of children from the NIG, FCG, and CAUG. There were some, albeit few, children in the minimal profile from both FCG and CAUG, highlighting that a small subset of severely deprived children develop no signs of DSED. A study by Minnis and colleagues43 revealed a strong genetic component for signs of attachment disorders such as DSED, offering one possible explanation of why some children in the FCG and CAUG groups, despite experiencing deprivation, did not show signs of DSED, but this remains to be further explored. The persistent modest profile, comprising children who exhibit persistently mild elevations of DSED signs over time, is a previously unidentified pattern of DSED signs not hypothesized a priori, highlighting the wide variability in signs of DSED as well as the advantage of using multiple statistical approaches. Persistence of signs of DSED may or may not be worrisome depending upon functional impairment. Future work is needed to further explore potential outcomes associated with persistently modest levels of DSED.
Examining profiles identified from growth mixture modeling contributed insight about the specific factors associated with individual variability in DSED signs over time. Consistent with previous work examining patterns of DSED following institutional care, no sex differences were found.14,22 The most important predictors of variability in signs of DSED over time included age of placement into foster care (FCG children), age first placed into a family (EIG children), disruptions in placement, and percent time spent in the institution.
Age of placement into foster care emerged as a potential predictor of outcomes, which has been a common finding in the BEIP.31 Such findings highlight the importance of early intervention, as earlier placement into families has been linked to not only fewer signs of DSED, but a better course of DSED across development. We have previously reported that children placed before the age of 24 months show fewer DSED signs than children placed after 24 months.23 In two separate reports from the same research group, Rutter and colleagues21 and Sonuga-Barke and colleagues22 reported that placement before 6 months was associated with fewer DSED signs throughout childhood and adolescence. In the present study, children with persistently elevated or modest signs of DSED who were from the FCG were placed into foster care at significantly older ages than children with few or no signs of DSED. Over the course of the study, most children in the CAUG were placed eventually into families (e.g., government foster care, adopted within Romania, or returned to biological parents/extended families). Children in the elevated and persistent modest profiles were found to be placed into families at significant older ages than children in the early decreasing and minimal profiles. Therefore, age of placement may not only reduce the occurrence of signs of DSED signs but may also protect against the persistence of signs into early adolescence. These findings underscore the importance of placing children into families at an early age and suggest that early placement may lead to reductions in DSED signs and prevent persistence into early adolescence. Furthermore, they point to a potential sensitive period in early childhood for the impact of adequate caregiving on the development and sustained course of signs of DSED into early adolescence.
Beyond early placement into families, consistency of placement also has implications for the course of DSED across development. Previous work by Pears and colleagues11 demonstrated associations between placement disruptions and signs of DSED among preschool-aged maltreated foster care children. In the present study, more placement disruptions, particularly during childhood and early adolescence, were associated with more signs of DSED. The difference in findings could be due to different samples or age of assessments. Interestingly, children in the persistent modest profile had the highest number of placement disruptions indicating that frequent disruptions, particularly after 54 months of age, may contribute to steady, albeit modest, levels of DSED signs into early adolescence. Despite a clear association with age placed into a family and placement disruption for the persistent modest profile, it is presently unclear how meaningful modest levels of DSED signs are. One study examined the persistence of signs of DSED into adulthood and found little impairment related to DSED in the absence of comorbidity.22 However, additional work is needed to replicate these findings and further examine potential outcomes of this pattern coupled with comorbidity and functional impairment.
Differences among profiles were also found for percent time in institutional care through age 54 months. Spending a greater percentage of time in institutional care early in life was associated with elevated and persistently modest courses of DSED signs across development whereas spending less time in care was associated with minimal or decreasing DSED signs over time. After controlling for percent time in institutional care through age 54 months, percent time in institutional care through age 12 years did not independently contributed to a different course of DSED signs. Taken together, results indicate that early deprivation has a more robust association with the course of DSED signs across development than later deprivation in institutional care. The less time young children spend in institutional care the greater the reduction in the persistence of DSED. Furthermore, preventing disruptions and sustaining placements in families into middle childhood and adolescence also may have a positive impact on signs of DSED across development.
Importantly, the course of DSED following severe deprivation is influenced by earlier placement of children into families and maintaining stable placements. Previous research on family placement reducing signs of DSED has been mixed, with many studies reporting that signs of DSED were not significantly reduced following placement into non-neglecting families—at least in some children.6,9,14,23 Nevertheless, in the present study, we found that placing children into families at an early age may be crucial for improving the course of DSED across development. Another important consideration is the stability of foster care placement. Interventions aimed at reducing signs of DSED following deprivation should focus on finding family placements for children early in life. Once placed in a family, disruptions throughout childhood and adolescence should be minimized. Preserving placements may involve ongoing support to the family and the provision of services such as psychoeducation about the effects of early deprivation. In persistent cases, treatment may be necessary44, however, the evidence base for the treatment of DSED signs is limited and in need of further study.
There were some limitations of this work that are important to note. The signs used to assess DSED were consistent across all waves of assessment, which allows consistency in the scale of measurement and items used to assess DSED longitudinally, but this necessarily reduces developmental sensitivity to the clinical phenotype at different ages. As with most studies of DSED, caregiver report was used, and this introduces possible reporter bias. Because of placement changes, caregivers who reported on children with a history of institutional rearing changed over time, introducing variability. Finally, due to missing data, models were fitted provide approximations of the pattern of DSED signs across available assessment ages, and thus data was not available for each year in age. A larger sample assessed with greater frequency would increase confidence in the findings reported.
Although previous work has identified patterns of DSED across early childhood14 and from childhood into young adulthood22, this is the first report on the longitudinal course of the same signs of DSED from early childhood into early adolescence. Our longitudinal analyses suggest that signs of DSED vary significantly over time, and that both decreasing and stable patterns were apparent from early childhood to early adolescence. Variation was associated with response to a high-quality foster care intervention, length of time children spent in institutional care, and stability of placement once children were placed with families. Further research on DSED beyond early adolescence is needed to better understand the presentation and impact of DSED across development and will be beneficial in identifying ways to improve and sustain the well-being of children into adolescence and adulthood who have been exposed to insufficient care.
Supplementary Material
Table S1. Mixed Modeling Fixed Effect Estimates of Group by Age on disinhibited social engagement disorder (DSED) Signs
Table S2. Fit Indices for Growth Mixture Models
Note: The 5-profile model did not converge and is not a viable model. BIC = Bayesian Information Criteria. LMR-LRT = Lo-Mendel-Rubin likelihood ratio test.
Table S3. Mean Differences in Age Entered Foster Care (FCG only) and Age First Placed into a Family (FCG and CAUG only).
Note: CAUG = care as usual group. E = Elevated. ED = Early decreasing. FCG = foster care group. M = Minimal. PL = Persistent low.
Figure S1. Consolidated Standards of Reporting Trials (CONSORT) figure.
Acknowledgments
This research was supported by the John D. and Catherine T. MacArthur Foundation Research Network on “Early Experience and Brain Development” (Charles A. Nelson, PhD, Chair), the National Institute of Mental Health (NIMH) (1R01MH091363; Nelson) (F32MH107129; Humphreys), the Brain and Behavior Research Foundation (formerly NARSAD) Young Investigator Award 23819 (Humphreys), and the Klingenstein Third Generation Foundation Fellowship (Humphreys).
The authors thank the Bucharest Early Intervention Project staff in Romania and the children and caregivers who participated in this study.
Disclosure: Dr. Humphreys has received grant support from NIMH and the Brain and Behavior Research Foundation. She has received honoraria for lectures to professional audiences. She has served as a paid consultant to ZERO TO THREE. Dr. Fox has received grant support from NIMH and the National Institute of Child Health and Human Development. He has served on the National Scientific Council on the Developing Child. He has received royalties from Taylor and Francis Press and Harvard University Press. He has received honoraria for lectures to professional audiences. Dr. Nelson has received grant support from NIMH, the John D. and Catherine T. MacArthur Foundation, the Sinneave Foundation, and the Binder Family Foundation. He has served on the scientific advisory board of the Merck Foundation, the National Scientific Council on the Developing Child, and has served as a paid consultant to the US Department of Justice. He has received royalties from Harvard University Press, Massachusetts Institute of Technology Press, and Wiley and Sons. He has received honoraria for lectures to professional audiences. Dr. Zeanah has received grant support from NIMH, the Palix Foundation, the Irving Harris Foundation, the Substance Abuse and Mental Health Services Administration, the Lumos Foundation, and the Institute for Mental Hygiene. He has received royalties from Guilford Press and Harvard University Press. He has received honoraria for lectures to professional audiences.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Dr. Guyon-Harris reports no biomedical financial interests or potential conflicts of interest.
Contributor Information
Katherine L. Guyon-Harris, Tulane University School of Medicine, New Orleans, LA.
Kathryn L. Humphreys, Tulane University School of Medicine, New Orleans, LA, Stanford University, Stanford, CA.
Nathan A. Fox, University of Maryland, College Park, MD.
Charles A. Nelson, Boston Children’s Hospital/Harvard Medical School, Boston, MA; The Harvard Graduate School of Education, Cambridge, MA.
Charles H. Zeanah, Tulane University School of Medicine, New Orleans, LA.
References
- 1.American Psychiatric Association. DSM-5: Diagnostic and Statistical Manual of Mental Disorders. 5th. Arlington, VA: American Psychiatric Publishing; 2013. https://books.google.com/books?hl=de&lr=&id=-JivBAAAQBAJ&pgis=1. [Google Scholar]
- 2.ZERO TO THREE. DC:0-5TM: Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood. Washington, DC: Author; 2016. [Google Scholar]
- 3.Chisholm K, Carter MC, Ames EW, Morison SJ. Attachment Security and Indiscriminately Friendly Behavior in Children Adopted from Romanian Orphanages. 1995;7 doi: 10.1017/S0954579400006507. [DOI] [Google Scholar]
- 4.Albus KE, Dozier M. Indiscriminate friendliness and terror of strangers in infancy: Contributions from the study of infants in foster care. Infant Ment Health J. 1999;20(1):30–41. doi: 10.1002/(SICI)1097-0355(199921)20:1<30::AID-IMHJ3>3.0.CO;2-J. [DOI] [Google Scholar]
- 5.Zeanah CH. Disturbances of attachment in young children adopted from institutions. J Dev Behav Pediatr. 2000;21(3):230–236. https://www.researchgate.net/profile/Charles_Zeanah/publication/12434999_Disturbances_of_attachment_in_young_children_adopted_from_institutions/links/54c11e290cf25b4b8071b6b4.pdf. Accessed August 21, 2017. [PubMed] [Google Scholar]
- 6.Gleason MM, Fox NA, Drury SS, Smyke AT, Nelson CA, Zeanah CH. Indiscriminate behaviors in previously institutionalized young children. Pediatrics. 2014;133(3):e657–65. doi: 10.1542/peds.2013-0212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeanah CH, Scheeringa M, Boris NW, Heller SS, Smyke AT, Trapani J. Reactive attachment disorder in maltreated toddlers. Child Abus Negl. 2004;28(8):877–888. doi: 10.1016/j.chiabu.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 8.Zeanah CH, Smyke AT, Koga SF, Carlson E. Attachment in institutionalized and community children in Romania. Child Dev. 2005;76(5):1015–1028. doi: 10.1111/j.1467-8624.2005.00894.x. [DOI] [PubMed] [Google Scholar]
- 9.O’Connor TG, Rutter M. Attachment Disorder Behavior Following Early Severe Deprivation: Extension and Longitudinal Follow-up. J Am Acad Child Adolesc Psychiatry. 2000;39(6):703–712. doi: 10.1097/00004583-200006000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Bruce J, Tarullo AR, Gunnar MR. Disinhibited social behavior among internationally adopted children. Dev Psychopathol. 2009;21(1):157–171. doi: 10.1017/S0954579409000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pears KC, Bruce J, Fisher PA, Kim HK. Indiscriminate friendliness in maltreated foster children. Child Maltreat. 2010;15(1):64–75. doi: 10.1177/1077559509337891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zeanah CH, Smyke AT, Dumitrescu A. Attachment disturbances in young children. II: Indiscriminate behavior and institutional care. J Am Acad Child Adolesc Psychiatry. 2002;41(8):983–989. doi: 10.1097/00004583-200208000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Gleason MM, Fox NA, Drury S, et al. Validity of evidence-derived criteria for reactive attachment disorder: Indiscriminately social/disinhibited and emotionally withdrawn/inhibited types. J Am Acad Child Adolesc Psychiatry. 2011;50(3):216–231. doi: 10.1016/j.jaac.2010.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lawler JM, Koss KJ, Doyle CM, Gunnar MR. The course of early disinhibited social engagement among post-institutionalized adopted children. J Child Psychol Psychiatry Allied Discip. 2016;57(10):1126–1134. doi: 10.1111/jcpp.12606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lehmann S, Breivik K, Heiervang ER, Havik T, Havik OE. Reactive Attachment Disorder and Disinhibited Social Engagement Disorder in School-Aged Foster Children - A Confirmatory Approach to Dimensional Measures. J Abnorm Child Psychol. 2016;44(3):445–457. doi: 10.1007/s10802-015-0045-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jonkman CS, Oosterman M, Schuengel C, Bolle EA, Boer F, Lindauer RJ. Disturbances in attachment: inhibited and disinhibited symptoms in foster children. Child Adolesc Psychiatry Ment Health. 2014;8(1):21. doi: 10.1186/1753-2000-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tizard B, Hodges J. The effect of early institutional rearing on the development of eight year old children. J Child Psychol Psychiatry. 1978;19(2):99–118. doi: 10.1111/j.1469-7610.1978.tb00453.x. [DOI] [PubMed] [Google Scholar]
- 18.Sonuga-Barke EJ, Schlotz W, Kreppner J. Differentiating developmental trajectories for conduct, emotion, and peer problems following early deprivation. Monogr Soc Res Child Dev. 2010;75(1):102–124. doi: 10.1111/j.1540-5834.2010.00552.x. [DOI] [PubMed] [Google Scholar]
- 19.Humphreys KL, Nelson CA, Fox NA, Zeanah CH. Signs of reactive attachment disorder and disinhibited social engagement disorder at age 12 years: Effects of institutional care history and high-quality foster care. Dev Psychopathol. 2017;29(2):675–684. doi: 10.1017/S0954579417000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kay C, Green J, Sharma K. Disinhibited Attachment Disorder in UK Adopted Children During Middle Childhood: Prevalence, Validity and Possible Developmental Origin. J Abnorm Child Psychol. 2016;44(7):1375–1386. doi: 10.1007/s10802-016-0131-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rutter M, Colvert E, Kreppner J, et al. Early adolescent outcomes for institutionally-deprived and non-deprived adoptees. I: Disinhibited attachment. J Child Psychol Psychiatry Allied Discip. 2007;48(1):17–30. doi: 10.1111/j.1469-7610.2006.01688.x. [DOI] [PubMed] [Google Scholar]
- 22.Sonuga-Barke EJS, Kennedy M, Kumsta R, et al. Child-to-adult neurodevelopmental and mental health trajectories after early life deprivation: the young adult follow-up of the longitudinal English and Romanian Adoptees study. Lancet. 2017;389(10078):1539–1548. doi: 10.1016/S0140-6736(17)30045-4. [DOI] [PubMed] [Google Scholar]
- 23.Smyke AT, Zeanah CH, Gleason MM, et al. A randomized controlled trial comparing foster care and institutional care for children with signs of reactive attachment disorder. Am J Psychiatry. 2012;169(5):508–514. doi: 10.1176/appi.ajp.2011.11050748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guyon-Harris KL, Humphreys KL, Degnan KA, Fox NA, Nelson CA, Zeanah CH. A prospective study of reactive attachment disorder following early institutional care: Considering variable- and person-centered approaches. Manuscr under Rev. 2017 doi: 10.1080/14616734.2018.1499208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bergman LR, Magnusson D. A person-oriented approach in research on developmental psychopathology. Dev Psychopathol. 1997;9(2):291–319. doi: 10.1017/S095457949700206X. [DOI] [PubMed] [Google Scholar]
- 26.Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res. 2000;24(6):882–891. doi: 10.1111/j.1530-0277.2000.tb02070.x. [DOI] [PubMed] [Google Scholar]
- 27.Grimm KJ, Ram N, Estabrook R. Growth Modeling : Structural Equation and Multilevel Modeling Approaches. New York, NY: Guilford Press; 2016. https://www.guilford.com/books/Growth-Modeling/Grimm-Ram-Estabrook/9781462526062/summary. Accessed July 20, 2017. [Google Scholar]
- 28.Zeanah CH, Nelson CA, Fox NA, et al. Designing research to study the effects of institutionalization on brain and behavioral development: The Bucharest Early Intervention Project. Dev Psychopathol. 2003;15(4):885–907. doi: 10.1017/S0954579403000452. [DOI] [PubMed] [Google Scholar]
- 29.Miller FG. The randomized controlled trial as a demonstration project: An ethical perspective. Am J Psychiatry. 2009;166(7):743–745. doi: 10.1176/appi.ajp.2009.09040538. [DOI] [PubMed] [Google Scholar]
- 30.Millum J, Emanuel EJ. The ethics of international research with abandoned children. Science (80-) 2007;318(5858):1874–1875. doi: 10.1126/science.1153822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nelson CA, Fox NA, Zeanah CH. Romania’s Abandoned Children: Deprivation, Brain Development, and the Struggle for Recovery. Cambridge, MA: Harvard University Press; 2014. [Google Scholar]
- 32.Rid A. When is research socially valuable? Lessons from the Bucharest Early Intervention Project: Commentary on a case study in the ethics of mental health research. J Nerv Ment Dis. 2012;200(3):248–249. doi: 10.1097/NMD.0b013e318247d124. [DOI] [PubMed] [Google Scholar]
- 33.Zeanah CH, Fox NA, Nelson CA. The Bucharest Early Intervention Project: case study in the ethics of mental health research. J Nerv Ment Dis. 2012;200(3):243–247. doi: 10.1097/NMD.0b013e318247d275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smyke AT, Koga SF, Johnson DE, et al. The caregiving context in institution-reared and family-reared infants and toddlers in Romania. J Child Psychol Psychiatry Allied Discip. 2007;48(2):210–218. doi: 10.1111/j.1469-7610.2006.01694.x. [DOI] [PubMed] [Google Scholar]
- 35.Smyke AT, Dumitrescu A, Zeanah CH. Attachment disturbances in young children. I: The continuum of caretaking casualty. J Am Acad Child Adolesc Psychiatry. 2002;41(8):972–982. doi: 10.1097/00004583-200208000-00016. [DOI] [PubMed] [Google Scholar]
- 36.Smyke AT, Zeanah CH, Fox NA, Nelson CA. A new model of foster care for young children: the Bucharest early intervention project. Child Adolesc Psychiatr Clin N Am. 2009;18:721–734. doi: 10.1016/j.chc.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 37.IBM Corp. SPSS Statistics for Macintosh. 2015 [Google Scholar]
- 38.Satterthwaite F. International Biometric Society. Biometrics Bull. 1946;2:110–114. [Google Scholar]
- 39.Muthén LK, Muthén BO. Mplus User’s Guide. Sixth. Los Angeles, CA: Muthen & Muthen; 1998–2010. [Google Scholar]
- 40.Lo Y, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88(3):767–778. doi: 10.1093/biomet/88.3.767. [DOI] [Google Scholar]
- 41.D’Unger A, Land K, McCall P, Nagin D. How many latent classes of delinquent/criminal careers? Results from mixed poisson regression analyses. Am J Sociol. 1998;103:1593–1630. doi: https://doi.org/10.1086/231402. [Google Scholar]
- 42.Nylund KL, Asparouhov T, Muthén BO. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Struct Equ Model. 2007;14(4):535–569. doi: 10.1080/10705510701575396. [DOI] [Google Scholar]
- 43.Minnis H, Reekie J, Young D, et al. Genetic, environmental and gender influences on attachment disorder behaviours. Br J Psychiatry. 2007;190(6):490–495. doi: 10.1192/bjp.bp.105.019745. [DOI] [PubMed] [Google Scholar]
- 44.Zeanah CH, Chesher T, Boris NW, et al. Practice Parameter for the Assessment and Treatment of Children and Adolescents With Reactive Attachment Disorder and Disinhibited Social Engagement Disorder. J Am Acad Child Adolesc Psychiatry. 2016;55(11):990–1003. doi: 10.1016/j.jaac.2016.08.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Mixed Modeling Fixed Effect Estimates of Group by Age on disinhibited social engagement disorder (DSED) Signs
Table S2. Fit Indices for Growth Mixture Models
Note: The 5-profile model did not converge and is not a viable model. BIC = Bayesian Information Criteria. LMR-LRT = Lo-Mendel-Rubin likelihood ratio test.
Table S3. Mean Differences in Age Entered Foster Care (FCG only) and Age First Placed into a Family (FCG and CAUG only).
Note: CAUG = care as usual group. E = Elevated. ED = Early decreasing. FCG = foster care group. M = Minimal. PL = Persistent low.
Figure S1. Consolidated Standards of Reporting Trials (CONSORT) figure.


